Abstract
Although the MHC class II ‘u' haplotype is strongly associated with type 1 diabetes (T1D) in rats, the role of MHC class II in the development of tissue-specific autoimmune diseases including T1D and autoimmune thyroiditis remains unclear. To clarify this, we produced a congenic strain carrying MHC class II ‘a' and ‘u' haplotypes on the Komeda diabetes-prone (KDP) genetic background. The u/u homozygous animals developed T1D similar to the original KDP rat; a/u heterozygous animals did develop T1D but with delayed onset and low frequency. In contrast, none of the a/a homozygous animals developed T1D; about half of the animals with a/u heterozygous or a/a homozygous genotypes showed autoimmune thyroiditis. To investigate the role of genetic background in the development of thyroiditis, we also produced a congenic strain carrying Cblb mutation of the KDP rat on the PVG.R23 genetic background (MHC class II ‘a' haplotype). The congenic rats with homozygous Cblb mutation showed autoimmune thyroiditis without T1D and slight to severe alopecia, a clinical symptom of hypothyroidism such as Hashimoto's thyroiditis. These data indicate that MHC class II is involved in the tissue-specific development of autoimmune diseases, including T1D and thyroiditis.
Keywords: type 1 diabetes, autoimmune thyroiditis, alopecia, MHC class II, haplotype, KDP rat
Introduction
The major histocompatibility complex (MHC), also known as human leukocyte antigen (HLA) in human, is associated with various autoimmune diseases. Especially, MHC class II genes show the strongest association with type 1 diabetes (T1D), in which DRB1*03-DQB1*0201 and DRB1*04-DQB1*0302 haplotypes in Caucasian and DRB1*0405-DQB1*0401, DRB1*0802-DQB1*0302 and DRB1*0901-DQB1*0303 haplotypes in Japanese confer susceptibility to the disease, while DRB1*15-DQB1*0602 haplotype in Caucasian and DRB1*1501-DQB1*0602 and DRB1*1502-DQB1*0601 haplotypes in Japanese confer protection against the disease.1, 2, 3, 4, 5
T1D is frequently accompanied by autoimmune thyroid disease (AITD), such as Graves' disease (GD) and Hashimoto's thyroiditis (HT). The DR3 haplotype in Caucasian and DRB1*0405-DQB1*0401, DRB1*0802-DQB1*0302 and DRB1*0901-DQB1*0303 haplotypes in Japanese confer susceptibility to T1D complicated with AITD.6, 7, 8
AITD alone is also associated with MHC class II genes. The DR3 haplotype confers susceptibility to GD and the DR7 haplotype confers protection against GD,9, 10 in which arginine at position 74 of DR beta chain exhibits a strong association with the disease in Caucasian.11, 12 With less confidence, DR3 and DR4 haplotypes are associated with HT.13, 14, 15
The MHC region shows the strongest susceptibility to T1D in animal models, such as NOD mice, BB rats, KDP rats and LEW.1AR1-iddm rats. Almost every rat model of T1D possesses the same ‘u' haplotype on the MHC class II loci (RT1-B, -D), suggesting that the class II ‘u' haplotype confers susceptibility to T1D in rats. Autoimmune thyroiditis (also known as HT in humans) with no clinical manifestation of hypothyroidism is frequently observed in BB and KDP rats.16, 17, 18, 19 In the analysis of backcross between BB rats (MHC class II ‘u' haplotype) and PVG.R23 rats (‘a' haplotype), u/u homozygous animals showed 88% diabetes and 45% thyroiditis; u/a heterozygous animals showed no diabetes and 64% thyroiditis, suggesting that ‘u' haplotype confers susceptibility to T1D but is susceptible or neutral to thyroiditis while ‘a' haplotype confers susceptibility to thyroiditis but is protective against T1D.20 In another report, analysis of F2 intercross between BB and Fischer rats (‘lv' haplotype) found that u/u, u/lv and lv/lv animals showed 24, 24 and 0% thyroiditis, respectively, and analysis of backcross between BB and Lewis rats (‘l' haplotype) showed that u/u and u/l exhibited 25 and 31% thyroiditis, respectively.21 These data suggest that ‘u' haplotype confers susceptibility to thyroiditis, and acts in a dominant manner against ‘l' and ‘lv' haplotypes. However, these results were based on the mixed genetic backgrounds such as backcross or intercross progeny. There has been no data on replacement of genetic backgrounds through the production of congenic strains. In KDP rats, thyroiditis frequently develops in animals showing no or late onset diabetes.17, 19 Thus, although the ‘u' haplotype is necessary for the development of T1D, the association of ‘u' and other haplotypes with T1D and thyroiditis remains unclear.
To clarify the role of MHC class II in the development of T1D and thyroiditis, we established and investigated a congenic strain carrying MHC class II ‘a' and ‘u' haplotypes on the KDP genetic background. To investigate the role of genetic background in the development of thyroiditis, we produced and investigated a congenic strain carrying Cblb mutation of the KDP rat on the PVG.R23 genetic background (MHC class II ‘a' haplotype).
Results
Establishment of a KDP.PVG-RT1a/u congenic strain
By crossing the KDP and PVG.R23 rats followed by 11 successive backcrosses to the KDP, we successfully produced a congenic strain carrying the MHC class II ‘a' and ‘u' haplotypes (heterozygous state) on the KDP genetic background. Genome-wide profiling revealed that the region of <14.6 Mb between p-terminus and D20Rat60 on chromosome 20 harboring the MHC class II region of the PVG.R23 rat had been introgressed into the KDP genetic background, and that the PVG.R23 genome was not detected on other chromosomes (Supplementary Table 1). As the Cblb homozygous mutants have poor reproductive ability,17, 22 we have been maintaining the congenic strain having the Cblb region in the heterozygous state.
Incidence of diabetes of the KDP.PVG-RT1a/u congenic strain
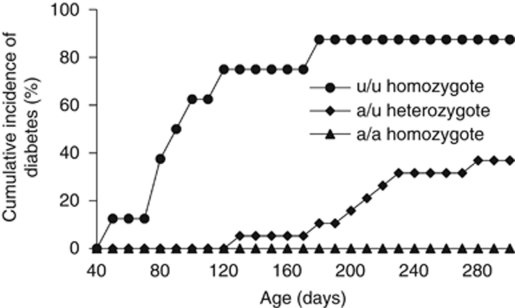
We compared the incidence of T1D among the Cblb homozygous mutant animals with each of the three genotypes at MHC class II region in the congenic strain under the same specific pathogen-free condition (Figure 1). At 300 days of age, 88% (7/8) of u/u homozygous animals developed T1D similar to the original KDP rat,22 and 37% (7/19) of a/u heterozygous animals did develop T1D but with delayed onset and low frequency. In contrast, none (0/11) of the a/a homozygous animals developed T1D. The u/u homozygous animals developed T1D as early as 50 days of age, while the a/u heterozygous animals developed the disease around 120 days of age at the earliest. Despite the low incidence and the delay of onset, it is noteworthy that the a/u heterozygous animals developed T1D.
Figure 1.
Cumulative incidence of diabetes in the KDP.PVG-RT1a/u congenic strain. Under the same specific pathogen-free condition, data of diabetes onset were obtained from the u/u homozygous (n=8), a/u heterozygous (n=19) and a/a homozygous (n=11) animals, all of which harbor the homozygous Cblb mutation. P<0.001 for u/u vs a/u and u/u vs a/a, and P=0.027 for a/u vs a/a by log-rank tests.
Degree of insulitis and thyroiditis of the KDP.PVG-RT1a/u congenic strain
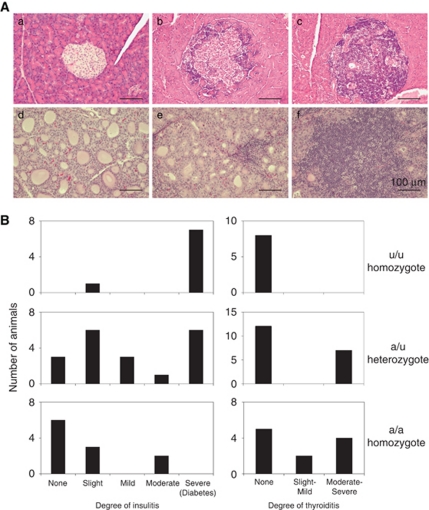
We then investigated the degree of insulitis and thyroiditis shortly after the onset of diabetes in diabetic animals and at 300 days of age in non-diabetic animals (Figure 2). All of the diabetic animals showed severe insulitis, whereas non-diabetic animals showed none to moderate insulitis: 100% (8/8) of u/u homozygous and 84% (16/19) of a/u heterozygous animals developed slight to severe insulitis. Although none of the a/a homozygous animals developed T1D, 45% (5/11) of them exhibited slight to moderate insulitis, suggesting that ‘a' haplotype did not confer complete protection against insulitis. In contrast to the severity of insulitis, thyroiditis was observed in 0% (0/8), 37% (7/19) and 55% (6/11) of u/u homozygous, a/u heterozygous and a/a homozygous animals, respectively (Figure 2). The serum thyroid stimulating hormone (TSH) values seem to be higher in a/a homozygous and a/u heterozygous animals than those of u/u homozygous animals, but there is no significant difference among them (Supplementary Figure 1). Furthermore, all of the TSH values are in normal range, suggesting no clinical manifestation of hypothyroidism.
Figure 2.
Degree of insulitis and thyroiditis in the KDP.PVG-RT1a/u congenic strain at 300 days of age. (A): Representative histology of the pancreas and thyroid glands in the congenic strain. a, normal islet; b, mild insulitis; c, severe insulitis; d, normal thyroid glands; e, mild thyroiditis; f, severe thyroiditis. (B) The degree of insulitis and thyroiditis in the congenic strain shortly after the onset of diabetes or at 300 days of age for non-diabetic animals. Data were obtained from the u/u homozygous (n=8), a/u heterozygous (n=19) and a/a homozygous (n=11) animals, all of which harbor the homozygous Cblb mutation. Insulitis: P=0.017 for u/u vs a/u, P<0.001 for u/u vs a/a and P=0.020 for a/u vs a/a; Thyroiditis: P=0.050 for u/u vs a/u, P=0.016 for u/u vs a/a and P=0.573 for a/u vs a/a by Mann–Whitney U tests.
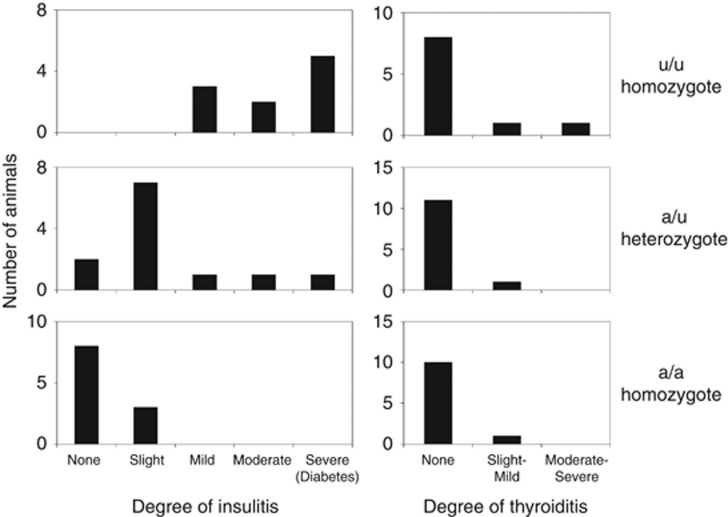
To clarify the development of insulitis and thyroiditis in the congenic strain, we further investigated the degree of insulitis and thyroiditis at 120 days of age (Figure 3), at which 75% of u/u homozygous animals developed T1D while none of the a/u heterozygous animals developed diabetes. Slight to severe insulitis was observed in 100% (10/10), 83% (10/12) and 27% (3/11) of u/u homozygous, a/u heterozygous and a/a homozygous animals, respectively, the severity of which was milder than that at 300 days of age. At the same age, thyroiditis was observed in 20% (2/10), 8% (1/12) and 9% (1/11) of u/u homozygous, a/u heterozygous and a/a homozygous animals, respectively. The degree of thyroiditis was much milder than that of insulitis, suggesting that insulitis develops earlier than thyroiditis in these animals.
Figure 3.
Degree of insulitis and thyroiditis in the KDP.PVG-RT1a/u congenic strain at 120 days of age. The degree of insulitis and thyroiditis in each animal was evaluated shortly after the onset of diabetes or at 120 days of age for non-diabetic animals. Data were obtained from the u/u homozygous (n=10), a/u heterozygous (n=12) and a/a homozygous (n=11) animals, all of which harbor the homozygous Cblb mutation. Insulitis at 300 days vs 120 days: P=0.184 for u/u, P=0.202 for a/u and P=0.280 for a/a; Thyroiditis at 300 days vs 120 days: P=0.193 for u/u, P=0.055 for a/u and P=0.018 for a/a by Mann–Whitney U tests.
Establishment of a PVG.KDP-Cblb congenic strain
By crossing the KDP and PVG.R23 rats followed by seven successive backcrosses to the PVG.R23, we successfully produced a congenic strain carrying the mutated Cblb allele of the KDP rat on the PVG.R23 genetic background (MHC class II ‘a' haplotype). Genome-wide profiling revealed that the region of <42.2 Mb between D11Rat13 and D11Rat37 on chromosome 11 harboring the mutated Cblb allele of the KDP rat had been introgressed into the PVG.R23 genetic background, and that the KDP genome was not detected on other chromosomes (Supplementary Table 1). As the Cblb homozygous mutants have poor reproductive ability,17, 22 we have been maintaining the congenic strain having the Cblb region in the heterozygous state.
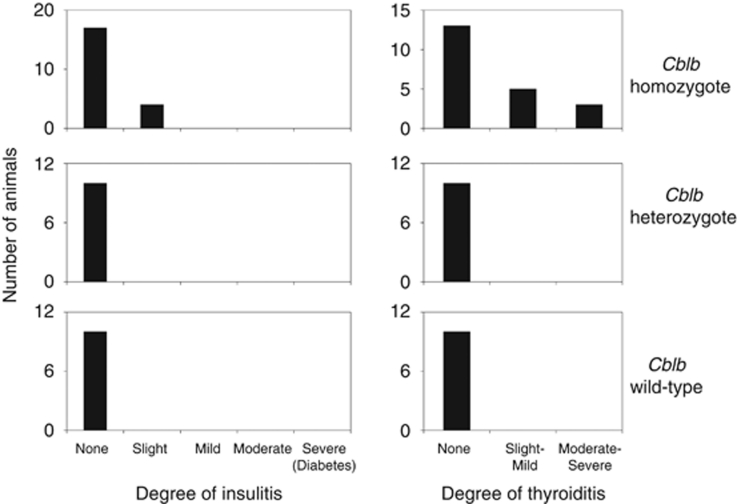
Degree of insulitis and thyroiditis of the PVG.KDP-Cblb congenic strain
As expected, none of the animals in this congenic strain developed T1D before 300 days of age. We investigated the degree of insulitis and thyroiditis at 300 days of age, and found that 19% (4/21) of the Cblb homozygous mutants showed only slight insulitis, whereas heterozygous (n=10) and wild-type (n=10) animals exhibited no insulitis (Figure 4). At the same age, thyroiditis was observed in 38% (8/21) of the Cblb homozygous mutant animals, whereas none of the heterozygous (n=10) or wild-type (n=10) animals showed thyroiditis (Figure 4). The degree of insulitis and thyroiditis of the Cblb homozygous mutant animals is similar to that of a/a homozygous animals in the KDP.PVG-RT1a/u congenic strain. There is no significant difference in the serum TSH values among animals with three genotypes of Cblb (Supplementary Figure 1) and all of the TSH values are in normal range, suggesting no clinical symptom of hypothyroidism. However, there was one Cblb homozygous mutant animal exhibiting an exceptionally high TSH value of more than 200 ngml−1. This animal also showed severe thyroiditis and severe hair loss (alopecia), indicating clinical manifestation of hypothyroidism such as HT.
Figure 4.
Degree of insulitis and thyroiditis in the PVG.KDP-Cblb congenic strain at 300 days of age. The degree of insulitis and thyroiditis in each animal was evaluated at 300 days of age. Data were obtained from the animals homozygous (n=21), heterozygous (n=10) and wild type (n=10) for the Cblb mutation. P=0.082 for insulitis and P=0.249 for thyroiditis by Mann–Whitney U tests in comparison between the a/a homozygous animals in the KDP.PVG-RT1a/u congenic strain and the Cblb homozygous mutants in the PVG.KDP-Cblb congenic strain.
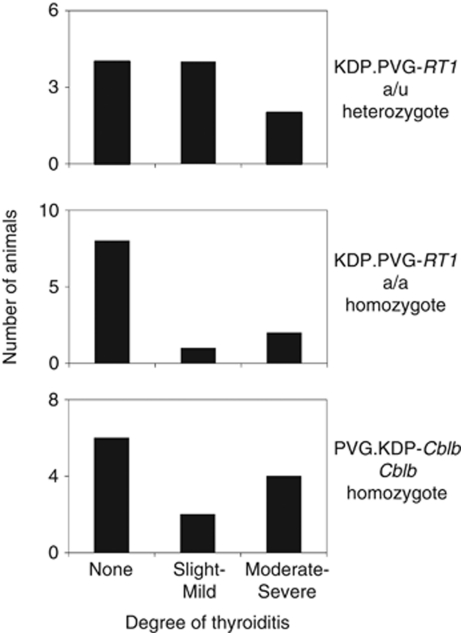
Effect of iodide on the development of thyroiditis in the congenic strains
The NOD-H2h4 mice, which express MHC class II ‘k' haplotype on the NOD background, do not develop T1D but spontaneous autoimmune thyroiditis, which is accelerated by adding iodide in the drinking water.23 To clarify the effect of iodide on the development of thyroiditis in the congenic strains, we supplied animals with 0.15% NaI in the drinking water for 4 weeks around 200 days of age. In the KDP.PVG-RT1a/u congenic strain, thyroiditis was observed in 60% (6/10) and 27% (3/11) of a/u heterozygous and a/a homozygous animals, respectively (Figure 5). In the PVG.KDP-Cblb congenic strain, thyroiditis was observed in 50% (6/12) of the Cblb homozygous mutant animals (Figure 5). As there was no significant acceleration in the development of thyroiditis with iodide treatment for 4 weeks, we did not measure TSH levels in these animals.
Figure 5.
Degree of thyroiditis in the KDP.PVG-RT1a/u and PVG.KDP-Cblb congenic strains with iodide treatment. The degree of thyroiditis in each animal was evaluated after 4 weeks of iodide treatment. Data were obtained from the a/u heterozygous (n=10) and a/a homozygous (n=11) animals in the KDP.PVG-RT1a/u congenic strain, all of which harbor the homozygous Cblb mutation, and from the Cblb homozygous mutant animals (n=12) in the PVG.KDP-Cblb congenic strain. Thyroiditis in NaI treatment vs no treatment: P=0.682 for a/u heterozygous animals in the KDP.PVG-RT1a/u congenic strain, P=0.218 for a/a homozygous animals in the KDP.PVG-RT1a/u congenic strain and P=0.355 for the Cblb homozygous mutants in the PVG.KDP-Cblb congenic strain by Mann–Whitney U tests.
Discussion
In the present study, we investigated the role of MHC class II in the development of tissue-specific autoimmune diseases including T1D and autoimmune thyroiditis by use of newly established congenic strains. The results indicate that, under homozygosity for Cblb mutation, MHC class II ‘u' haplotype confers susceptibility to insulitis and T1D, while ‘a' haplotype confers protection against insulitis and T1D, in which ‘u' haplotype acts in a semidominant manner with respect to ‘a' haplotype. In contrast, under homozygosity for Cblb mutation, MHC class II ‘u' haplotype confers neutral susceptibility to thyroiditis, while ‘a' haplotype confers susceptibility to thyroiditis, in which ‘a' haplotype acts in a dominant or semidominant manner with respect to ‘u' haplotype. It should be noted that it is not T1D but thyroiditis that occurs in congenic rats with homozygosity for both MHC class II ‘a' haplotype and Cblb mutation. These findings support the previous report on the analysis of backcross between BB and PVG.R23 rats20 but further clarifies the mode of inheritance of ‘a' and ‘u' haplotypes on the KDP genetic background. The length of the congenic interval found in each congenic strain varied. The relatively small cohort sizes of these experiments were underpowered to detect small effects caused by the congenic intervals. Larger cohorts are needed to detect more subtle effects of congenic intervals in T1D and thyroiditis.
To our knowledge, this study is the first analysis of the role of rat MHC class II haplotypes in the development of T1D and autoimmune thyroiditis in a genetic background susceptible to T1D using congenic strains. In addition to the BB, KDP and LEW.1AR1-iddm rats, spontaneous T1D also occurs (with a frequency of 2%) in LEW.1WR1 rats.24 Almost all spontaneous or virus-induced T1D models in rat species possess ‘u' haplotype at MHC class II,25 suggesting that the MHC class II ‘u' haplotype is required to develop T1D in rats. In humans, non-aspartic acid at position 57 of HLA-DQ beta chain of MHC class II is associated with T1D.26 At position 57 of rat RT1-B beta, which is orthologous to HLA-DQ beta, the ‘u' allele possesses non-aspartic acid, while ‘a' allele possesses aspartic acid.27 These findings indicate that the MHC class II molecule encoded by ‘u' but not ‘a' haplotype recognizes an unidentified epitope, among which an insulin epitope is the strong candidate,28, 29 and leads to islet-specific autoimmunity, resulting in T1D.
In humans, arginine at position 74 of HLA-DR beta chain of MHC class II has been reported to be strongly associated with GD.11 At position 74 of rat RT1-D beta, which is orthologous to HLA-DR beta, both the ‘u' and ‘a' alleles possess alanine.27 These indicate that both haplotypes are not likely to be susceptible to GD. Although there are no such data for HT, ‘a' but not ‘u' haplotype would be expected to possess amino acid(s) that confer susceptibility to HT. There has been no known spontaneous animal model exhibiting final pathophysiological states of AITD, including GD and HT. Although the BB and KDP rats show spontaneous autoimmune thyroiditis, they do not develop hypothyroidism. In this study, we also investigated whether combination of the thyroiditis-susceptible MHC class II haplotype ‘a' and the autoimmunity-susceptible Cblb mutation could induce hypothyroidism on two different genetic backgrounds such as the KDP and PVG.R23. Although 40–60% of animals in both strains developed thyroiditis, the TSH levels suggested no clinical symptom of hypothyroidism. However, in the PVG.KDP-Cblb congenic strain, 76% (16/21) of the Cblb homozygous mutant animals showed slight to severe alopecia, which is often found to be associated with hypothyroidism in humans. Only 19% (4/21) of these animals developed severe alopecia, while the others exhibited only slight to mild states. Furthermore, regrowth occurred spontaneously in many cases and the hair growth was restored within several months. These findings suggest the use of the PVG.KDP-Cblb congenic strain as a spontaneous animal model of HT. However, the low frequency of incidence of severe pathophysiological states makes practical use of this model difficult; iodide supplement from younger age and longer duration might induce hypothyroidism more frequently.
In conclusion, the roles of rat MHC class II ‘a' and ‘u' haplotype in the development of T1D and autoimmune thyroiditis differ. The congenic strains established in this study will be useful for the investigation of the pathogenesis and pathophysiology of tissue-specific autoimmune diseases, including T1D and thyroiditis.
Materials and methods
KDP and PVG.R23 rats
Both KDP (RT1.AuBuDuCu) and PVG.R23 (RT1.AuBaDaCav1) rats were a kind gift from Dr K Komeda (Tokyo Medical University), and were maintained at the Institute for Experimental Animals, Kobe University School of Medicine. The KDP/Tky strain is available from Japan SLC, Inc. All animals were maintained under specific pathogen-free conditions at 23±2 °C and 55±10% relative humidity with a 12-h light–dark cycle, and were provided with water and a commercial diet CE-2 (CLEA Japan, Inc., Tokyo, Japan) at the Institute for Experimental Animals, Kobe University School of Medicine. All animal experiments were approved by the Committee on Animal Experimentation, Kobe University School of Medicine, and carried out in accordance with the ‘Guidelines for Animal Experimentation at Kobe University'.
KDP.PVG-RT1a/u congenic strain
The KDP and PVG.R23 rats were crossed to produce the F1 progeny. Eleven successive backcrosses (N12) to the KDP rats were needed to obtain animals heterozygous at MHC class II region but homozygous for KDP allele for the other regions. The Cblb region has been maintained in the heterozygous state to overcome the poor reproductive ability of the Cblb homozygous mutants.17, 22 An intercross between the N12 animals was conducted to obtain the congenic strain (N12F1) carrying MHC class II (RT1-B, -D) ‘a' and ‘u' haplotypes on the KDP genetic background. The congenic strain, named KDP.PVG-RT1a/u/Nyo, is available from the National Bio-Resource Project of Rat in Japan (http://www.anim.med.kyoto-u.ac.jp/nbr/).
PVG.KDP-Cblb congenic strain
The KDP and PVG.R23 rats were crossed to produce the F1 progeny. Seven successive backcrosses (N8) to the PVG.R23 rats were needed to obtain animals heterozygous at the Cblb region but homozygous for PVG.R23 allele for the other regions. An intercross between the N8 animals was conducted to obtain the congenic strain (N8F1) carrying the mutated Cblb allele of the KDP rat on the PVG.R23 genetic background. The congenic strain, named PVG.KDP-Cblb/Nyo, is available from the National Bio-Resource Project of Rat in Japan (http://www.anim.med.kyoto-u.ac.jp/nbr/).
Genotyping
The simple sequence length polymorphism markers and PCR–RFLP markers used in this study have been described (Rat Genome Database, available at http://rgd.mcw.edu/).17, 22, 30, 31 Genotyping was performed as described in previous investigations.17, 22, 30, 31 Briefly, genomic DNA was extracted from the tail tip of each rat using the automatic DNA Isolation System (Kurabo, Osaka, Japan). PCR amplification was carried out using 200-n sense and antisense primers, 200 μ each dNTP, 12-ng genomic DNA and 0.75 U of LA Taq DNA polymerase (Takara Bio Inc., Shiga, Japan) in a total volume of 15 μl. The PCR product was mixed with loading buffer (0.03% bromphenol blue and 30% glycerol), electrophoresed on 4% NuSieve 3:1 agarose gel (FMC BioProducts, Rockland, ME, USA) and stained with ethidium bromide. For Cblb, genotyping was performed by PCR–RFLP analysis using primers, 5′-TGCCCCTTCTGTCGCTGTGA-3′ and 5′-CCTCGGTTTTGAATCAACAG-3′, and restriction enzyme TaqI. For D20Rwh1 (RT1-Bb), genotyping was performed by PCR–RFLP analysis using primers, 5′-CACCAACGGGACGCAGCGCAT-3′ and 5′-CAAGCCGCCGCAGGGAGGTG-3′, and restriction enzyme BssHII. For RT1-Db, genotyping was performed by PCR–RFLP analysis using primers, 5′-ACGCAGCGCGTGCGGCTTCT-3′ and 5′-GCTCCATGAACTCCTTCTGTTTG-3′, and restriction enzyme DdeI.
Phenotyping of diabetes
Phenotyping was completed using a previously described protocol.30 Diabetes was defined as glycosuria positivity and blood glucose levels ⩾250 mg dl−1 under ad libitum dietary conditions. Data were obtained from two generations (N12F1 to N12F2) of the KDP.PVG-RT1a/u congenic strain and two generations (N8F2 to N8F3) of the PVG.KDP-Cblb congenic strain.
Histological analysis
Histological analysis was performed as described previously17, 30 with some modifications. Briefly, tissues were fixed in 10% formalin, and paraffin sections were stained with hematoxylin and eosin. Serial sections were viewed via light microscopy by an examiner blind to the experimental conditions of the animals. Each animal was rated on the degree of insulitis, which ranged from none to severe (none [0%], slight [0%<and lower than or equal to 5%], mild [5%<and lower than or equal to 20%], moderate [20%<and lower than or equal to 70%], and severe [70%<]) based mainly on the percentage of moderately and severely infiltrated islets. The term ‘slight insulitis' refers to at least one infiltrated islet across the sections and a percentage of infiltrated islets of 5% or less. Animals were also rated on the degree of thyroiditis, which ranged from none to severe (none, slight-mild and moderate-severe) based on the percentage of infiltrated regions in the thyroid sections. Data were obtained from two generations (N12F1 to N12F2) of the KDP.PVG-RT1a/u congenic strain and two generations (N8F2 to N8F3) of the PVG.KDP-Cblb congenic strain, with the exception that the degree of insulitis and thyroiditis at 120 days of age was evaluated in the N12F5 generation of the KDP.PVG-RT1a/u congenic strain.
TSH assay
Serum TSH was measured with an enzyme-linked immunosorbent assay kit (Rat TSH ELISA KIT, Shibayagi, Gunma, Japan).
Iodide administration
The a/u heterozygous and a/a homozygous animals in the KDP.PVG-RT1a/u congenic strain and the Cblb homozygous mutant animals in the PVG.KDP-Cblb congenic strain were supplied with 0.15% NaI in the drinking water for 4 weeks around 200 days of age.
Statistical analysis
Differences in the incidence of diabetes were assessed using log-rank tests. Differences in the degree of insulitis or thyroiditis were assessed using Mann–Whitney U tests. Differences in the TSH values were assessed using Tukey–Kramer method. Statistical analysis was performed by R.32
Acknowledgments
This study was supported by a Core Research for Evolutional Science and Technology grant from the Japan Science and Technology Agency and Grants-in-Aid for Scientific Research, a grant for Biomedical Cluster Kansai and a grant for the Global COE Program ‘Global Center of Excellence for Education and Research on Signal Transduction Medicine in the Coming Generation' from the Ministry of Education, Culture, Sports, Science and Technology of Japan. We thank the late Professor K Komeda (Tokyo Medical University) for his helpful advice during the course of this study.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on Genes and Immunity website (http://www.nature.com/gene)
Supplementary Material
References
- She JX. Susceptibility to type I diabetes: HLA-DQ and DR revisited. Immunol Today. 1996;17:323–329. doi: 10.1016/0167-5699(96)10014-1. [DOI] [PubMed] [Google Scholar]
- Awata T, Kuzuya T, Matsuda A, Iwamoto Y, Kanazawa Y. Genetic analysis of HLA class II alleles and susceptibility to type 1 (insulin-dependent) diabetes mellitus in Japanese subjects. Diabetologia. 1992;35:419–424. doi: 10.1007/BF02342437. [DOI] [PubMed] [Google Scholar]
- Ikegami H, Kawaguchi Y, Yamato E, Kuwata S, Tokunaga K, Noma Y, et al. Analysis by the polymerase chain reaction of histocompatibility leucocyte antigen-DR9-linked susceptibility to insulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1992;75:1381–1385. doi: 10.1210/jcem.75.5.1358911. [DOI] [PubMed] [Google Scholar]
- Yasunaga S, Kimura A, Hamaguchi K, Ronningen KS, Sasazuki T. Different contribution of HLA-DR and -DQ genes in susceptibility and resistance to insulin-dependent diabetes mellitus (IDDM) Tissue Antigens. 1996;47:37–48. doi: 10.1111/j.1399-0039.1996.tb02512.x. [DOI] [PubMed] [Google Scholar]
- Kawabata Y, Ikegami H, Kawaguchi Y, Fujisawa T, Shintani M, Ono M, et al. Asian-specific HLA haplotypes reveal heterogeneity of the contribution of HLA-DR and -DQ haplotypes to susceptibility to type 1 diabetes. Diabetes. 2002;51:545–551. doi: 10.2337/diabetes.51.2.545. [DOI] [PubMed] [Google Scholar]
- Golden B, Levin L, Ban Y, Concepcion E, Greenberg DA, Tomer Y. Genetic analysis of families with autoimmune diabetes and thyroiditis: evidence for common and unique genes. J Clin Endocrinol Metab. 2005;90:4904–4911. doi: 10.1210/jc.2004-2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker JM. Clinical review: type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab. 2006;91:1210–1217. doi: 10.1210/jc.2005-1679. [DOI] [PubMed] [Google Scholar]
- Katahira M, Maeda H, Tosaki T, Segawa S. The human leukocyte antigen class II gene has different contributions to autoimmune type 1 diabetes with or without autoimmune thyroid disease in the Japanese population. Diabetes Res Clin Pract. 2009;85:293–297. doi: 10.1016/j.diabres.2009.06.007. [DOI] [PubMed] [Google Scholar]
- Heward JM, Allahabadia A, Daykin J, Carr-Smith J, Daly A, Armitage M, et al. Linkage disequilibrium between the human leukocyte antigen class II region of the major histocompatibility complex and Graves' disease: replication using a population case control and family-based study. J Clin Endocrinol Metab. 1998;83:3394–3397. doi: 10.1210/jcem.83.10.5137. [DOI] [PubMed] [Google Scholar]
- Chen QY, Huang W, She JX, Baxter F, Volpe R, Maclaren NK. HLA-DRB1*08, DRB1*03/DRB3*0101, and DRB3*0202 are susceptibility genes for Graves' disease in North American Caucasians, whereas DRB1*07 is protective. J Clin Endocrinol Metab. 1999;84:3182–3186. doi: 10.1210/jcem.84.9.5991. [DOI] [PubMed] [Google Scholar]
- Ban Y, Davies TF, Greenberg DA, Concepcion ES, Osman R, Oashi T, et al. Arginine at position 74 of the HLA-DR beta1 chain is associated with Graves' disease. Genes Immun. 2004;5:203–208. doi: 10.1038/sj.gene.6364059. [DOI] [PubMed] [Google Scholar]
- Simmonds MJ, Howson JM, Heward JM, Cordell HJ, Foxall H, Carr-Smith J, et al. Regression mapping of association between the human leukocyte antigen region and Graves disease. Am J Hum Genet. 2005;76:157–163. doi: 10.1086/426947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon N, Zhang L, Weetman AP. HLA associations with Hashimoto's thyroiditis. Clin Endocrinol (Oxf) 1991;34:383–386. doi: 10.1111/j.1365-2265.1991.tb00309.x. [DOI] [PubMed] [Google Scholar]
- Petrone A, Giorgi G, Mesturino CA, Capizzi M, Cascino I, Nistico L, et al. Association of DRB1*04-DQB1*0301 haplotype and lack of association of two polymorphic sites at CTLA-4 gene with Hashimoto's thyroiditis in an Italian population. Thyroid. 2001;11:171–175. doi: 10.1089/105072501300042901. [DOI] [PubMed] [Google Scholar]
- Zeitlin AA, Heward JM, Newby PR, Carr-Smith JD, Franklyn JA, Gough SC, et al. Analysis of HLA class II genes in Hashimoto's thyroiditis reveals differences compared to Graves' disease. Genes Immun. 2008;9:358–563. doi: 10.1038/gene.2008.26. [DOI] [PubMed] [Google Scholar]
- Sternthal E, Like AA, Sarantis K, Braverman LE. Lymphocytic thyroiditis and diabetes in the BB/W rat. A new model of autoimmune endocrinopathy. Diabetes. 1981;30:1058–1061. doi: 10.2337/diab.30.12.1058. [DOI] [PubMed] [Google Scholar]
- Yokoi N, Komeda K, Wang H-Y, Yano H, Kitada K, Saitoh Y, et al. Cblb is a major susceptibility gene for rat type 1 diabetes mellitus. Nat Genet. 2002;31:391–394. doi: 10.1038/ng927. [DOI] [PubMed] [Google Scholar]
- Saito Y, Komeda K, Kanazawa M.Development of autoimmune thyroiditis in Komeda diabetes-prone rats Journal Tokyo Med University 20036153–58.(Japanese). [Google Scholar]
- Yokoi N, Hayashi C, Fujiwara Y, Wang HY, Seino S. Genetic reconstitution of autoimmune type 1 diabetes with two major susceptibility genes in the rat. Diabetes. 2007;56:506–512. doi: 10.2337/db06-1027. [DOI] [PubMed] [Google Scholar]
- Awata T, Guberski DL, Like AA. Genetics of the BB rat: association of autoimmune disorders (diabetes, insulitis, and thyroiditis) with lymphopenia and major histocompatibility complex class II. Endocrinology. 1995;136:5731–5735. doi: 10.1210/endo.136.12.7588330. [DOI] [PubMed] [Google Scholar]
- Pettersson A, Wilson D, Daniels T, Tobin S, Jacob HJ, Lander ES, et al. Thyroiditis in the BB rat is associated with lymphopenia but occurs independently of diabetes. J Autoimmun. 1995;8:493–505. doi: 10.1016/0896-8411(95)90004-7. [DOI] [PubMed] [Google Scholar]
- Yokoi N, Namae M, Fuse M, Wang HY, Hirata T, Seino S, et al. Establishment and characterization of the Komeda diabetes-prone rat as a segregating inbred strain. Exp Anim. 2003;52:295–301. doi: 10.1538/expanim.52.295. [DOI] [PubMed] [Google Scholar]
- Rasooly L, Burek CL, Rose NR. Iodine-induced autoimmune thyroiditis in NOD-H-2h4 mice. Clin Immunol Immunopathol. 1996;81:287–292. doi: 10.1006/clin.1996.0191. [DOI] [PubMed] [Google Scholar]
- Mordes JP, Guberski DL, Leif JH, Woda BA, Flanagan JF, Greiner DL, et al. LEW.1WR1 rats develop autoimmune diabetes spontaneously and in response to environmental perturbation. Diabetes. 2005;54:2727–2733. doi: 10.2337/diabetes.54.9.2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mordes JP, Bortell R, Blankenhorn EP, Rossini AA, Greiner DL. Rat models of type 1 diabetes: genetics, environment, and autoimmunity. ILAR J. 2004;45:278–291. doi: 10.1093/ilar.45.3.278. [DOI] [PubMed] [Google Scholar]
- Todd JA, Bell JI, McDevitt HO. HLA-DQ beta gene contributes to susceptibility and resistance to insulin-dependent diabetes mellitus. Nature. 1987;329:599–604. doi: 10.1038/329599a0. [DOI] [PubMed] [Google Scholar]
- Ettinger RA, Moustakas AK, Lobaton SD. Open reading frame sequencing and structure-based alignment of polypeptides encoded by RT1-Bb, RT1-Ba, RT1-Db, and RT1-Da alleles. Immunogenetics. 2004;56:585–596. doi: 10.1007/s00251-004-0725-7. [DOI] [PubMed] [Google Scholar]
- Nakayama M, Abiru N, Moriyama H, Babaya N, Liu E, Miao D, et al. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435:220–223. doi: 10.1038/nature03523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent SC, Chen Y, Bregoli L, Clemmings SM, Kenyon NS, Ricordi C, et al. Expanded T cells from pancreatic lymph nodes of type 1 diabetic subjects recognize an insulin epitope. Nature. 2005;435:224–228. doi: 10.1038/nature03625. [DOI] [PubMed] [Google Scholar]
- Yokoi N, Kanazawa M, Kitada K, Tanaka A, Kanazawa Y, Suda S, et al. A non-MHC locus essential for autoimmune type I diabetes in the Komeda diabetes-prone rat. J Clin Invest. 1997;100:2015–2021. doi: 10.1172/JCI119733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuyama T, Ishibiki J, Awata T, Noda M, Kanazawa Y, Sugawara M, et al. An improved genetic linkage map of rat chromosome 20. Comp Med. 2000;50:369–373. [PubMed] [Google Scholar]
- R Development Core Team R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria 2010 . http://www.R-project.org .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.