Abstract
OBJECTIVE
To examine whether quality of diabetes care is equitable for South Asian and Chinese patients in an urban Canadian setting.
RESEARCH DESIGN AND METHODS
Process and intermediate measures of quality of care were compared between 246 South Asians, 170 Chinese, and 431 patients from the general population with type 2 diabetes selected from 45 family physicians’ practices.
RESULTS
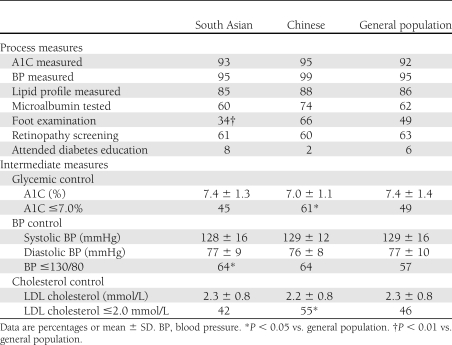
A total of 61% of Chinese achieved A1C ≤7.0% versus 45% of South Asians and 49% of the general population (P < 0.05). They were also more likely to achieve LDL cholesterol ≤2.0 mmol/L, while South Asians were more likely to achieve blood pressure ≤130/80. There was only one significant process of care deficiency: fewer foot examinations among South Asians (34 vs. 49% for the general population, P < 0.01).
CONCLUSIONS
Quality of diabetes care in a Canadian urban setting was equitable, with ethnic minorities somewhat more likely to achieve recommended targets than the general population.
Racial and ethnic minority populations in the U.S. achieve worse health outcomes and have greater mortality than whites (1). The experience of ethnic minorities in Canada is different because of a publicly funded universal health care system that may mitigate some socioeconomic and insurance barriers to care. Canadian minorities also represent different ethnic groups, with the two largest being South Asians (from the Indian subcontinent) and Chinese (2). We examined quality of type 2 diabetes care in an urban family practice setting, comparing South Asians and Chinese with the general population.
RESEARCH DESIGN AND METHODS
Previous research suggests that minority patients see different practitioners than nonminority patients (3), which may confound evaluations of quality of care. Therefore, we recruited all patients from the practices of the same family physicians. We identified neighborhoods in the Toronto area where ≥25% of the population reported either South Asian or Chinese ethnicity in the 2006 Canadian census. Family physicians were enrolled who had been in practice for at least 3 years and who had at least 10 South Asian or Chinese diabetic patients and 10 general population diabetic patients in their practice. The general population could not include South Asians or Chinese but could include whites or people from any other ethnic group. Other ethnic groups, the largest of which were black and Filipino, made up 24% of the population of the selected neighborhoods, similar to their proportion of the Toronto population as a whole (2).
In each participating physician’s office, we randomly selected 10 South Asian or Chinese and 10 general population diabetic patients. Inclusion criteria were age ≥18 years and type 2 diabetes for ≥2 years. Trained abstractors reviewed the selected charts and collected process and intermediate measures of diabetes care. Provincial ophthalmology and optometry billing claims data were searched to determine diabetic retinopathy screening.
Mean values or proportions for each quality measure were compared between both ethnic groups and the general population. To account for patient clustering within physicians, linear and logistic regression models using generalized estimating equations were used to determine statistical significance. Models were not adjusted for age or socioeconomic status because these factors may have formed part of the causal pathway explaining disparities in quality of care. Models adjusting for baseline characteristics were tested and did not materially change the inferences of the results (not shown). All statistical analyses were performed using SAS version 9.2.
RESULTS
We recruited 26 physicians from neighborhoods with large concentrations of South Asians and 19 physicians from neighborhoods with large concentrations of Chinese. From these physicians, 847 eligible patients with type 2 diabetes were identified. Of these patients, 246 were South Asians and 170 were Chinese (Supplementary Table 1). Both minority populations had a greater preponderance of men than the general population. South Asians also were substantially younger (mean age 58 vs. 66 and 64 years) and were more likely to be recent immigrants (26 vs. 10 and 9%) compared with Chinese and general population patients, respectively. Groups did not differ by socioeconomic status or diabetes duration.
Quality of care is shown in Table 1. A greater proportion of Chinese achieved the glycemic control target of A1C ≤7.0% and the lipid control target of LDL cholesterol ≤2.0 mmol/L, whereas a greater proportion of South Asians achieved the blood pressure target of ≤130/80. South Asians were less likely to receive a foot examination than the general population. Otherwise, there were no differences in quality indicators between groups.
Table 1.
Process and intermediate measures of quality of care
CONCLUSIONS
We found virtually no differences in process measures of diabetes care between South Asians, Chinese, and the general population. For intermediate measures, the ethnic minority populations were, if anything, more likely to achieve recommended targets. Indeed, the quality of care achieved by all patients in the study was moderately high, with overall glycemic, blood pressure, and LDL cholesterol control exceeding or close to recommended targets. In contrast, American data show lower performance for virtually all measures, particularly among patients on Medicaid (4).
Most American studies of ethnic disparities in diabetes care focus on blacks and Hispanics (5–7). Several studies including Asians show narrower disparities compared with whites than for other minorities, but these studies do not disaggregate Asian subgroups (6–8). Our findings corroborate recent California data showing similar A1C and lipid levels for South Asians and Chinese versus whites (9). Several studies from the U.K. find marked disparities in glycemic control and other intermediate measures for South Asians (10–13), although these gaps have diminished after years of quality improvement initiatives in British primary care (14). By selecting both minority and general population patients from the same family physicians’ practices, our study eliminated interphysician differences between groups (3), which may have driven some of the inequity found in previous studies.
There are some limitations to our study. Important factors that could contribute to quality of care for minority patients, such as language proficiency or degree of acculturation, could not reliably be collected from family physicians’ charts. In addition, patients and physicians in this study were selected from urban neighborhoods with large South Asian or Chinese populations. Physicians practicing in these neighborhoods may have had greater cultural sensitivity than those living in areas with fewer South Asians or Chinese, and minority patients in the selected neighborhoods may have had greater access to familiar ethnic foods and have had greater community social supports to empower behavior change and healthful lifestyles. Thus, the generalizability of study findings to places with smaller minority populations, particularly in smaller cities and rural areas, is uncertain.
In conclusion, the process and intermediate measures of diabetes care in a Canadian urban family practice setting were similar between South Asians and Chinese and the general population. Further research will be required to establish the mechanisms through which equitable care was achieved in this population and how those can be translated into clinical and policy decisions affecting minority populations more broadly. In addition, methods of improving quality of care, particularly for poorly performed process measures such as foot examination or retinopathy screening, must be developed for the whole population with diabetes, regardless of ethnicity.
Acknowledgments
This study was funded by the Heart and Stroke Foundation of Ontario. B.R.S. has received salary support from the Canadian Institutes of Health Research and the Canadian Diabetes Association. The Institute for Clinical Evaluative Sciences has received support from the Ontario Ministry of Health and Long-Term Care.
No potential conflicts of interest relevant to this article were reported.
B.R.S. researched data, contributed to discussion, and drafted, reviewed, and edited the manuscript. K.C.-D. researched data and reviewed and edited the manuscript. S.S.A., P.C.A., D.G.M., and J.E.H. contributed to discussion and reviewed and edited the manuscript. B.R.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in abstract form at the 70th Scientific Sessions of the American Diabetes Association, Orlando, Florida, 25–29 June 2010.
The authors thank Matthew Stanbrook, Don Redelmeier, and Arlene Bierman, all of the University of Toronto, for their comments on an earlier draft of the manuscript.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1845/-/DC1.
References
- 1.Institute of Medicine Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC, National Academies Press, 2002 [PubMed] [Google Scholar]
- 2.Statistics Canada. Ethnocultural Portrait of Canada Highlight Tables, 2006 Census Ottawa, Statistics Canada, 2008 (No. 97-562-XWE2006002) [Google Scholar]
- 3.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med 2004;351:575–584 [DOI] [PubMed] [Google Scholar]
- 4.National Committee for Quality Assurance The State of Health Care Quality. Washington, DC, National Committee for Quality Assurance, 2010 [Google Scholar]
- 5.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care 2003;41:1221–1232 [DOI] [PubMed] [Google Scholar]
- 6.Lanting LC, Joung IMA, Mackenbach JP, Lamberts SW, Bootsma AH. Ethnic differences in mortality, end-stage complications, and quality of care among diabetic patients: a review. Diabetes Care 2005;28:2280–2288 [DOI] [PubMed] [Google Scholar]
- 7.Kirk JK, Bell RA, Bertoni AG, et al. Ethnic disparities: control of glycemia, blood pressure, and LDL cholesterol among US adults with type 2 diabetes. Ann Pharmacother 2005;39:1489–1501 [DOI] [PubMed] [Google Scholar]
- 8.McBean AM, Huang Z, Virnig BA, Lurie N, Musgrave D. Racial variation in the control of diabetes among elderly Medicare managed care beneficiaries. Diabetes Care 2003;26:3250–3256 [DOI] [PubMed] [Google Scholar]
- 9.Kanaya AM, Adler N, Moffet HH, et al. Heterogeneity of diabetes outcomes among Asians and Pacific Islanders in the US: the Diabetes Study of Northern California (DISTANCE). Diabetes Care 2011;34:930–937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mukhopadhyay B, Forouhi NG, Fisher BM, Kesson CM, Sattar N. A comparison of glycaemic and metabolic control over time among South Asian and European patients with type 2 diabetes: results from follow-up in a routine diabetes clinic. Diabet Med 2006;23:94–98 [DOI] [PubMed] [Google Scholar]
- 11.McElduff P, Edwards R, Burns JA, et al. Comparison of processes and intermediate outcomes between South Asian and European patients with diabetes in Blackburn, north-west England. Diabet Med 2005;22:1226–1233 [DOI] [PubMed] [Google Scholar]
- 12.Gray J, Millett C, Saxena S, Netuveli G, Khunti K, Majeed A. Ethnicity and quality of diabetes care in a health system with universal coverage: population-based cross-sectional survey in primary care. J Gen Intern Med 2007;22:1317–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fischbacher CM, Bhopal R, Steiner M, Morris AD, Chalmers J. Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. J Public Health (Oxf) 2009;31:239–249 [DOI] [PubMed] [Google Scholar]
- 14.Verma A, Birger R, Bhatt H, et al. Ethnic disparities in diabetes management: a 10-year population-based repeated cross-sectional study in UK primary care. J Public Health (Oxf) 2010;32:250–258 [DOI] [PubMed] [Google Scholar]