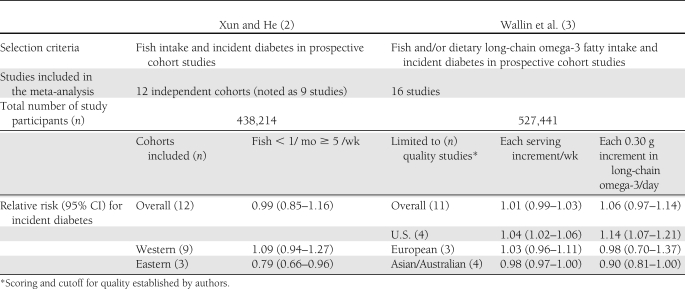
Evidence-based health recommendations are founded on the assumption that quality of research and findings are largely reproducible (1). Prospective cohort studies that have examined how fish and omega-3 fatty acid intake are related to the risk of developing diabetes have yielded inconsistent findings. This issue of Diabetes Care includes articles from two research teams that each conducted a meta-analysis of fish intake and incident diabetes (Table 1) (2,3). Independently both teams found the same explanation for the lack of consistent findings and no overall association between fish intake and incident diabetes. Separating the studies based on geography yielded two distinctly opposing associations. Analysis of studies conducted in Western countries (U.S. and Europe) found that a higher intake of fish was associated with a higher incidence of diabetes, whereas analysis of studies conducted in Eastern countries (Asia and Australia) found that eating more fish was associated with a lower incidence of diabetes (2,3).
Table 1.
These divergent associations raise a number of questions regarding variables that may account for the inconsistencies. Considerations should be given to environmental factors, e.g., wild versus farm raised, mercury content, differences in preparation methods, e.g., frying, and demographic and health characteristic confounding or interaction. A recent study of restaurant food intake and incident diabetes found the relationship between fried fish and diabetes was attenuated by BMI (4). The use of objective biomarkers for omega-3 fatty acid intake in the Cardiovascular Health Study found that the incidence of diabetes was lower with higher levels of omega-3 biomarkers, also when adjusting for BMI (5). Environmental contaminants such as methyl mercury can induce in vitro and in vivo pancreatic β-cell dysfunction via oxidative stress in a mouse model (6). Thus, fluctuating environmental exposures and/or energy densities may account for observed differences in diabetes risk in geographic populations.
Both meta-analysis articles used the term “fish” to refer to intake of fresh water, ocean, and shell fish (2,3), but these items may also be referred categorically as “seafood” as noted in current federal recommendations. The 2010 Dietary Guidelines for Americans definition of “seafood” includes fish, such as salmon, tuna, trout, and tilapia, and shellfish, such as shrimp, crab, and oysters. The Dietary Guidelines suggest increasing seafood intake from the current level of about 3.5 ounces per week to about 8 ounces per week. This would yield a weekly intake of approximately 1,750 mg of long-chain omega-3 fatty acids, specifically from eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Although the concentration of EPA and DHA vary widely, the recommendation is intended to achieve a daily average intake of 250 mg based on evidence that 250 mg of EPA+DHA is associated with reduced cardiac deaths among individuals with and without preexisting cardiovascular disease (CVD). Recommendations from the American Diabetes Association (ADA) and the American Heart Association (AHA) address the general cardiovascular benefits focusing on two fish meals per week (particularly fatty fish) and omega-3 supplements for treating hypertriglyceridemia (7–10).
The ADA 2008 nutrition recommendations addressed potential benefits of omega-3 fatty acid supplements in hypertriglyceridemia (10). Potential concerns included an accompanying small rise in LDL cholesterol that is likely to be offset by an increase in HDL cholesterol. Glucose metabolism was not found to be adversely affected. ADA concluded, “Consumption of omega-3 fatty acids from fish or from supplements has been shown to reduce adverse CVD outcomes, but the evidence for α-linolenic acid is sparse and inconclusive. In addition to providing omega-3 fatty acids, fish frequently displace high–saturated fat–containing foods from the diet. Two or more servings of fish per week (with the exception of commercially fried fish filets) can be recommended” (10).
The ADA's systematic review, “Macronutrients, Food Groups, and Eating Patterns in the Management of Diabetes,” published in February 2012 (7), focuses on metabolic control and preventing CVD complications. The review states: “Overall it appears that supplementation with omega-3 fatty acids does not improve glycemic control but may have beneficial effects on CVD risk biomarkers among individuals with type 2 diabetes by reducing [triglycerides] (in some but not all studies). Other benefits (e.g., increasing HDL cholesterol or decreasing LDL cholesterol) are not clearly defined” (7).
AHA recommends use of a 2–4 g EPA + DHA daily supplement with medical supervision for treating hypertriglyceridemia, noting an approximate 5–10% reduction in triglycerides per gram of EPA/DHA consumed. Although hypertriglyceridemia was noted to be associated with insulin resistance and risk for developing diabetes, the recommendations do not include using omega-3 fatty acids as a diabetes prevention strategy (9). Analysis of data from the Diabetes Prevention Program (DPP) indicates that intake of fish was below two servings per day before and after receiving intensive lifestyle counseling (11). However, Golub et al. (12) “hypothesize that EPA and DHA supplementation … can contribute to the prevention and reduction of obesity” by affecting the endocannabinoid and mesocorticolimbic pathways and is a safe and inexpensive population intervention that the Food and Drug Administration deems as “generally recognized as safe” for dosage up to 3 g/day (12). Although Golub et al. acknowledge the multifactorial causes of obesity, their hypothesis seems to be based on considering fish oils to be a “magic bullet” public health solution (12). Aquaculture and genetically modified fish are proposed strategies to increase the availability of fish/seafood and omega-3 fatty acid supplements; yet more research is needed on the safety and effects of these methods (13). There has also been considerable effort to provide pharmaceutical options for slowing the progression to overt diabetes, noting that thiazolidinediones “have been shown to be as good, if not better, than lifestyle intervention” (14). Weight loss, achieved by reducing caloric intake and increasing physical activity, and thiazolidinedione therapy can reduce the risk of developing diabetes by over 50%. Other proposed options for reducing the increasing prevalence of diabetes include bariatric surgery, incretin-based therapies, and addressing β-cell function using pharmagenomic approaches. The potential effect size of eating fish and of fish oil supplement is far below the risk reduction potential of these options. There is a need for research that addresses the etiology of geographic divergences related to cooking methods, environmental exposures, and demographics in the association between fish intake and risk of developing diabetes. This research may also provide novel insights into mechanisms associated with the development of diabetes. Despite the promise of pharmaceutical and surgical solutions to the diabetes pandemic, such solutions may accrue high costs and unintended consequences.
How applicable are current nutrition recommendations? The 2010 Dietary Guidelines are consistent with earlier ADA and AHA recommendations in advising intake of 8 oz or two “fish/seafood” meals per week to reduce cardiovascular risk, especially sudden death associated with myocardial infarction. Recommendations with regard to omega-3 fatty acid supplements focus on medically supervised usage for the treatment of hypertriglyceridemia. Since adverse health effects are minimal, continuing with these recommendations seems reasonable. However, the best lifestyle recommendations for preventing diabetes remain caloric reduction, increasing physical activity, and promoting healthy food choices and cookery methods to achieve weight loss. In an era of soaring health care costs, we need to be mindful of quick-fix solutions to the diabetes pandemic and consider broken systems associated with increasing availability of energy-dense foods and low levels of physical activity.
Acknowledgments
This work was supported in part by National Institute of Diabetes and Digestive and Kidney Diseases grants (R34DK090695, 5R18DK075981, and NIH-DK 20541).
No potential conflicts of interest relevant to this article were reported.
References
- 1.Spahn JM, Lyon JM, Altman JM, et al. The systematic review methodology used to support the 2010 Dietary Guidelines Advisory Committee. J Am Diet Assoc 2011;111:520–523 [DOI] [PubMed] [Google Scholar]
- 2.Xun P, He K. Fish consumption and incidence of diabetes: a meta-analysis of data from 438,000 individuals in 12 independent prospective cohorts with an average 11-year follow-up. Diabetes Care 2012;35:930–938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wallin A, Di Giuseppe D, Orsini N, Patel PS, Forouhi NG, Wolk A. Fish consumption, dietary long-chain n-3 fatty acids, and risk of type 2 diabetes: systemic review and meta-analysis of prospective studies. Diabetes Care 2012;35:918–929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krishnan S, Coogan PF, Boggs DA, Rosenberg L, Palmer JR. Consumption of restaurant foods and incidence of type 2 diabetes in African American women. Am J Clin Nutr 2010;91:465–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Djoussé L, Biggs ML, Lemaitre RN, et al. Plasma omega-3 fatty acids and incident diabetes in older adults. Am J Clin Nutr 2011;94:527–533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen YW, Huang CF, Tsai KS, et al. The role of phosphoinositide 3-kinase/Akt signaling in low-dose mercury-induced mouse pancreatic beta-cell dysfunction in vitro and in vivo. Diabetes 2006;55:1614–1624 [DOI] [PubMed] [Google Scholar]
- 7.Wheeler ML, Dunbar SA, Jaacks LM, et al. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care 2012;35:434–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lichtenstein AH, Appel LJ, Brands M, et al. ; American Heart Association Nutrition Committee Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation 2006;114:82–96 [DOI] [PubMed] [Google Scholar]
- 9.Miller M, Stone NJ, Ballantyne C, et al. ; American Heart Association Clinical Lipidology, Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2011;123:2292–2333 [DOI] [PubMed] [Google Scholar]
- 10.Bantle JP, Wylie-Rosett J, Albright AL, et al. ; American Diabetes Association Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 2008;31(Suppl. 1):S61–S78 [DOI] [PubMed] [Google Scholar]
- 11.Mayer-Davis EJ, Sparks KC, Hirst K, et al. ; Diabetes Prevention Program Research Group Dietary intake in the diabetes prevention program cohort: baseline and 1-year post randomization. Ann Epidemiol 2004;14:763–772 [DOI] [PubMed] [Google Scholar]
- 12.Golub N, Geba D, Mousa SA, Williams G, Block RC. Greasing the wheels of managing overweight and obesity with omega-3 fatty acids. Med Hypotheses 2011;77:1114–1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Silva SS, Nguyen TT, Turchini GM, Amarasinghe US, Abery NW. Alien species in aquaculture and biodiversity: a paradox in food production. Ambio 2009;38:24–28 [DOI] [PubMed] [Google Scholar]
- 14.Kahn SE, Utzschneider KM. What's next for diabetes prevention? Diabetes Care 2011;34:1678–1680 [DOI] [PMC free article] [PubMed] [Google Scholar]