Abstract
OBJECTIVE
Self-management of type 2 diabetes including avoidance of hypoglycemia is complex, but the impact of cognition on safe self-management is not well understood. This study aimed to assess the effect of baseline cognitive function and cognitive decline on subsequent risk of severe hypoglycemia and to assess the effect of different glycemic strategies on these relationships.
RESEARCH DESIGN AND METHODS
Prospective cohort analysis of data from the ACCORD trial included 2,956 adults aged ≥55 years with type 2 diabetes and additional cardiovascular risk factors. Cognitive tests (Digit Symbol Substitution Test [DSST], Rey Auditory Verbal Learning Test, Stroop Test, and Mini Mental Status Examination) were conducted at baseline and 20 months. Study outcomes were incident confirmed severe hypoglycemia requiring medical assistance (HMA) and hypoglycemia requiring any assistance (HAA).
RESULTS
After a median 3.25-year follow-up, a 5-point-poorer baseline score on the DSST was predictive of a first episode of HMA (hazard ratio 1.13 [95% CI 1.08–1.18]). Analyses of the other cognitive tests and of HAA were consistent with the DSST results. Cognitive decline over 20 months increased the risk of subsequent hypoglycemia to a greater extent in those with lower baseline cognitive function (Pinteraction = 0.037). Randomization to an intensive versus standard glycemic strategy had no impact on the relationship between cognitive function and the risk of severe hypoglycemia.
CONCLUSIONS
Poor cognitive function increases the risk of severe hypoglycemia in patients with type 2 diabetes. Clinicians should consider cognitive function in assessing and guiding their patients regarding safe diabetes self-management regardless of their glycemic targets.
Type 2 diabetes is an increasingly common disease. Its optimal management requires the active participation of affected patients, who must perform home glucose monitoring and adjust glucose-lowering medication and insulin, in anticipation and avoidance of hypoglycemia (1–3). The complexity of many diabetes treatment regimens requires good cognitive function. Therefore, cognitive function may be an important determinant of the risk for treatment-related adverse events such as severe hypoglycemia. Prospective studies suggest that cognitive status may affect the functional ability of patients with type 2 diabetes (4), and patients with dementia are less likely to be involved in diabetes self-care (5). However, it has not been shown that cognitive impairment leads to a greater risk of severe hypoglycemia. Improved understanding of this relationship may assist providers, caregivers, and patients in developing new treatment and education guidelines for diabetes management for people with cognitive impairment.
The ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial assessed the effects of two different glycemic control strategies among individuals with type 2 diabetes at high risk for cardiovascular disease. ACCORD prospectively and systematically ascertained all severe hypoglycemic episodes. In addition, the ACCORD-MIND (Memory IN Diabetes) study assessed several domains of cognition among a subset of ACCORD participants. Thus, ACCORD-MIND provides a unique opportunity to assess the effect of baseline cognitive function on subsequent risk of severe hypoglycemia, as well as the effect of declines in cognitive function on the ongoing risk for severe hypoglycemia, and whether intensive versus standard glycemic control strategies affect these relationships.
RESEARCH DESIGN AND METHODS
Study design and eligibility
The design of ACCORD has previously been described (6,7). In brief, from 2001 to 2005, participants aged 40–79 years with type 2 diabetes and an A1C ≥7.5% and who had characteristics putting them at high risk of cardiovascular disease were recruited from 77 sites in the U.S. and Canada. Individuals were excluded if they had had frequent or serious hypoglycemia in the previous year or were unwilling to do home glucose monitoring. All 10,251 participants were randomized either to comprehensive intensive glycemic therapy targeting A1C <6.0% or to standard glycemic therapy targeting A1C 7.0–7.9%. In a double 2 × 2 factorial design, 4,733 of the participants were enrolled in a blood pressure–lowering trial, and 5,518 participants were enrolled in a lipid therapy trial. In December 2007, after a mean 3.5 year follow-up, the independent data and safety monitoring board recommended discontinuation of the intensive glycemia intervention due to excess mortality, after which point all participants were managed using the standard glycemic strategy. This report describes events occurring during the active glycemia intervention period.
All participants were provided with glucose-lowering medications prescribed by the investigators, glucose-monitoring equipment, educational materials, and counseling regarding diabetes care. Intensive group participants attended visits every month for the first 4 months and then every 1–2 months, and they were asked to conduct home glucose monitoring two to eight times per day. Standard group participants attended visits every 4 months and were asked to conduct home glucose monitoring a few times per week to three times per day. At each visit, glucose logs were reviewed and education regarding hypoglycemia recognition, prevention, and self-treatment was provided. If a participant experienced an episode of severe hypoglycemia, glycemic targets were relaxed for at least 4 weeks and a cohabitant was provided with a glucagon kit and instructions for use. For second episodes (or more) of severe hypoglycemia requiring medical assistance, additional information was sought and reviewed by the study’s central safety officer.
ACCORD-MIND, described elsewhere (8), enrolled a subset of 2,977 participants from 52 ACCORD sites from August 2003 to October 2005. Participants eligible for MIND were >55 years of age and were fluent in English or Spanish. Certified technicians administered and scored a 30-min battery of cognitive tests (English or validated Spanish translations) performed by each participant at baseline (targeted to be performed within 45 days after randomization into ACCORD) and again after 20 months. To ensure that participants were not hypoglycemic at the time of testing, tests were administered only if capillary glucose was ≥60 mg/dL (3.3 mmol/L) and usually after breakfast.
All blood and urine measurements in this report were obtained from baseline samples analyzed in the ACCORD central laboratory. The study protocols were approved by ethics boards at all participating centers, and all participants provided written informed consent.
Definitions of severe hypoglycemia
At every visit, participants were asked about experiences of “low blood sugar” including therapy and consequences. A diagnosis of severe hypoglycemia required documentation of a plasma glucose <50 mg/dL (2.8 mmol/L) or symptoms that promptly resolved with oral carbohydrate, intravenous glucose, or parenteral glucagon. Episodes requiring hospitalization or care in an emergency department or from emergency personnel were identified as “hypoglycemia requiring medical assistance” (HMA). The primary outcome for this report is time from randomization until the first episode of HMA. HMA is a more specific measure of severe hypoglycemia and is more likely to be well documented than episodes of “hypoglycemia requiring any third-party assistance” (HAA) from a medical or any nonmedical person. For assessment of the effect on people who experience recurrent severe hypoglycemia, time to the second episode of HMA was also reported. Time to first and second episodes of HAA was also reported.
Cognitive tests
The ACCORD-MIND battery, described elsewhere (8), was chosen because of its sensitivity to cognitive changes arising from both cerebrovascular and neurodegenerative etiologies.
The primary cognitive measure for this study was the Digit Symbol Substitution Test (DSST), which is a subset of the Wechsler Adult Intelligence Scale (WAIS-III). It assesses a wide variety of executive functions that may be relevant to recognition and rapid treatment of hypoglycemia, including visual motor speed, learning capacity, sustained attention, and working memory. It has been used in cognitively intact individuals, and it has been shown to predict cognitive decline, physical disability (2% over 8.4 years for a one-point-lower score) (9), and mortality (0.2–0.7% per year for a one-point-lower score) (9–11). Scores of 0 (worst) to 133 (best) are possible. Across the range of normal cognition, six points on the DSST is approximately equivalent to one point on the Mini-Mental Status Exam (MMSE), with which clinicians may be more familiar (12). The DSST is the cognitive test of greatest interest in this study, since it provides a broad assessment of cognition (12).
The Rey Auditory Verbal Learning Test (RAVLT), a test of verbal memory, assesses registration and recall of words. It is a sensitive tool for neurologic impairment in a variety of patients and has been used extensively in epidemiological research. Higher scores indicate better performance (13).
The Stroop test assesses an executive function largely attributable to frontal lobe function, namely the ability to view complex visual stimuli and to direct attention and respond to one attribute while inhibiting the response to another attribute. This is a timed test for which higher scores indicate worse performance (14).
The MMSE assesses global mental status and is used clinically to screen for possible cognitive impairment, which may require more in-depth evaluation. It is mainly used in elderly populations. Scores of 0 (worst) to 30 (best) are possible (15).
Statistical methods
All analyses were conducted using SAS software, version 9.1 (SAS Institute). Baseline characteristics and 20-month change in cognitive test scores (20-month score minus baseline score) of participants with or without HMA were compared by t tests or χ2 tests. Baseline characteristics of interest were those that have previously been associated with cognitive status and/or hypoglycemia (16,17). Pearson correlations between baseline cognitive test scores were calculated.
Unadjusted annualized incidence rates of hypoglycemia for groups of individuals divided by tertiles of baseline cognitive test score were calculated by dividing the number of individuals with events by the total number of person-years until the time of the first event or last contact. Time to first episode of severe hypoglycemia was compared between these three cognitive groups using Kaplan-Meier curves and log-rank tests. Hazard ratios (HRs) and 95% CIs were calculated by Cox models for each of the upper two groups compared with the group in the lowest third of cognitive test scores after controlling for variables used to stratify randomization.
Cox models were also used to calculate HRs and 95% CIs of a five-point-worse DSST test score for severe hypoglycemia among all participants and separately for intensive and standard group participants. Assumptions of linearity (P = 0.26) and proportional hazards (P = 0.11) were not rejected and therefore were considered valid. The interaction between baseline cognitive scores and the glycemia intervention group was used to determine whether the effect of baseline cognitive status on the risk of hypoglycemia differed in the intensive versus the standard group. Three sets of models were fit: model 1 includes variables used to stratify randomization (second trial assignment [blood pressure or lipid]: randomized group allocation within the blood pressure trial or lipid trial and history of clinical cardiovascular disease). Model 2 includes all model 1 variables plus sex, age, education, language of test administration, and depression. Model 3 includes all model 2 variables plus diabetes duration, prior stroke, baseline A1C, ethnicity, BMI, history of peripheral neuropathy, urine albumin-to-creatinine ratio, and baseline insulin use. Models were not adjusted for other medications including lipid-lowering or antihypertension medications. Because of the large number of covariates involved relative to the number of observed events, model 3 was only fit when both intervention groups were analyzed together.
The effect of worsening cognitive status during the first 20 months of therapy on the subsequent risk of severe hypoglycemia was estimated in model 1. To eliminate the confounding effect of prior hypoglycemia on cognitive function or subsequent hypoglycemia, these analyses were restricted to individuals who had no severe hypoglycemia prior to the 20-month cognitive assessment. Tests of interaction were used to investigate whether baseline cognitive function moderated the effect of 20-month change in cognitive function on hypoglycemic events. Crude incidence of HMA was plotted for nine groups defined by tertiles of change in DSST score and by tertiles of baseline DSST score to illustrate the relationship. In addition, a χ2 test with 3 df (baseline DSST × intervention group, change DSST × intervention group, and baseline DSST × change DSST × intervention group) was performed to determine whether the observed relationships were similar between intensive and standard glycemia intervention groups.
RESULTS
Participant characteristics
ACCORD-MIND enrolled 2,977 participants. We excluded 20 individuals who did not complete baseline cognitive assessments and 1 who experienced severe hypoglycemia between randomization and the baseline cognitive assessment. Of the remaining 2,956 participants followed for a median of 3.25 years, 160 reported one or more HMA episodes, including 36 who reported at least two HMA episodes. Sixty-eight people who had no HMA episodes before the 20-month assessment reported one or more HMA episodes occurring after the 20-month cognitive assessment, nine of whom reported at least two HMA episodes after this time. In total, 238 of the 2,956 participants reported at least one HAA, and 73 reported at least two HAAs. Of those who had no HAAs before 20 months, 99 reported at least two HAAs and 18 reported at least two HAAs after the 20-month assessment.
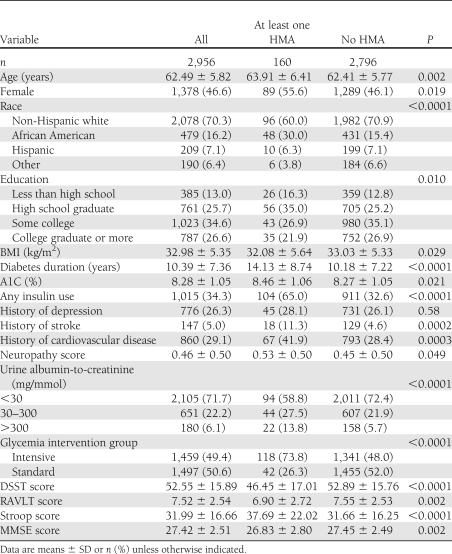
Compared with those who never had an HMA episode, participants who experienced at least one HMA episode were more likely to be female, older, African American, and less educated; more likely to have less-well controlled diabetes of longer duration with more albuminuria, neuropathy, and cardiovascular disease; and more likely to have been randomized to intensive glycemic therapy and also had significantly worse baseline scores on all cognitive tests (Table 1). The absolute value of Pearson correlation coefficients between pairs of the four cognitive tests at baseline ranged from 0.29 to 0.47 (all P values <0.0001).
Table 1.
Baseline characteristics of participants
Effect of baseline cognitive status on risk of hypoglycemia
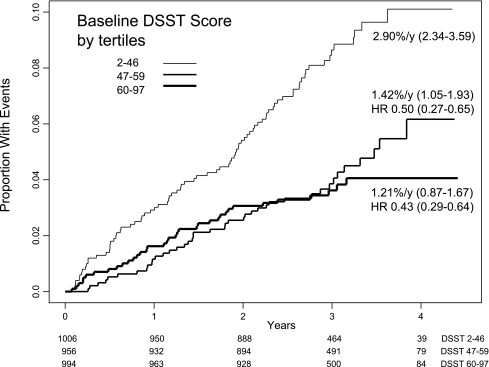
Lower baseline DSST score was associated with an increased risk for first episode of HMA (Fig. 1) (P < 0.0001 by log-rank test). The crude rate of HMA within the lowest third of baseline DSST score was 2.90% per year (95% CI 2.34–3.59), whereas rates were progressively lower within the middle (1.42% per year [95% CI 1.05–1.93]) and upper third (1.21% per year [0.87–1.67]). There was a 50% (95% CI 27–65) lower risk in the middle third compared with the lowest third and a 57% (36–71) lower risk in the highest third compared with the lowest third after adjustment for randomization stratification variables.
Figure 1.
Kaplan-Meier curves for HMA according to baseline thirds of the DSST score. Crude incidence rates and 95% CIs are shown for each group. Log-rank test P < 0.0001. HRs for the middle- and highest-score groups are with reference to the lowest–DSST score group.
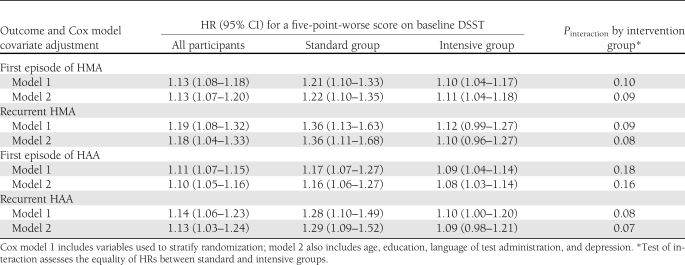
In the setting of model 1, a five-point-lower DSST score increased the risk of HMA by 13% (95% CI 8–18) and HAA by 11% (7–15). Similar results were seen for recurrent hypoglycemia and after adjustment for model 2 variables (Table 2). Even after adjustment for all the variables in model 3, a five-point-lower DSST score increased the risk of HMA by 10% (0–22) and HAA by 7% (2–13). The risk of hypoglycemia due to poor cognition was not statistically different between the two intervention groups (Table 2).
Table 2.
Baseline DSST score and subsequent risk of severe hypoglycemia
Consistent with the results of the DSST, a one-point difference in the direction of poorer cognitive function in the baseline scores of the other cognitive tests was also predictive of a first episode of HMA after adjustment for stratification variables (model 1): RAVLT HR 1.10 (95% CI 1.03–1.17; P = 0.0023); Stroop 1.01 (1.007–1.02; P < 0.001); and MMSE 1.09 (1.03–1.15; P = 0.0014).
Effect of cognitive decline on risk of hypoglycemia
A total of 2,665 participants completed baseline and 20-month DSST assessments and did not have any hypoglycemia before the 20-month assessment. Among these participants, the changes in cognitive test scores from baseline to the 20-month assessment (20-month score minus baseline score mean ± SD) were not significantly different for those who did (n = 68) versus those who did not (n = 2,597) experience subsequent HMA (DSST −0.84 ± 7.33 vs. −1.39 ± 8.14, P = 0.58; RAVLT −0.03 ± 1.95 vs. 0.36 ± 1.75, P = 0.11; Stroop 0.94 ± 19.83 vs. −1.00 ± 13.52, P = 0.43; and MMSE 0.43 ± 2.49 vs. −0.10 ± 1.97, P = 0.28). However, with use of Cox analysis, cognitive decline over 20 months, assessed by the DSST, was associated with an increased risk of hypoglycemia thereafter among those with lower baseline cognitive status, whereas this relationship was not present for those with better baseline cognitive status (interaction between baseline value and change score treated as continuous variables: Pinteraction = 0.037 for HMA and Pinteraction = 0.029 for HAA) after adjustment for the covariates in model 1. The relationship did not differ between standard and intensive glycemic intervention groups (P = 0.13 for HMA and P = 0.32 for HAA; data not shown). The dependence on baseline cognitive status of the relationship between change in DSST score and HMA incidence is illustrated by arbitrarily dividing participants into thirds of baseline DSST and change in DSST. As noted in Fig. 2, the pattern of increased incidence of HMA being associated with larger declines in cognition is not apparent in the group with the highest baseline scores.
Figure 2.
Effect of 20-month change in DSST score on crude incidence of severe hypoglycemia requiring medical assistance after 20 months, according to baseline thirds of DSST score. Number of individuals in each category is presented above each bar.
CONCLUSIONS
Severe hypoglycemia requiring assistance occurs in 0.4–1.5% of patients treated with standard type 2 diabetes therapy every year (18,19). The association between hypoglycemia and poor cognitive function is well described, but it is most often used to infer that cognitive decline is a consequence of hypoglycemia (20). The current study shows that cognitive function is a significant determinant of hypoglycemia, an important consideration in safe self-management of type 2 diabetes. The risk of developing severe hypoglycemia was significantly higher for patients with deficits in cognitive status. A DSST score in the lowest third increased the rate of HMA twofold. This is considerable, given that antecedent HMA (generally considered a strong risk factor) increased the risk of HMA fourfold. A five-point-lower DSST score increased the risk of HMA by 13% and recurrent HMA to an even greater degree after considering other factors. To put this in context, ~40 g alcohol (3–4 standard drinks) will acutely lower an individual’s DSST score by approximately five points (21–23), and among people in the same age range as those in ACCORD-MIND, a one-point difference in DSST score is consistent with the difference in cognition seen between two people differing in age by 1–2 years (24–28), differing in formal education experience by ~4 years (26) and, among people with type 2 diabetes, differing in A1C by 0.57% (16). Thus, even small differences in cognition can have an impact on hypoglycemia risk.
These findings are supported by observations from a study with very similar patients. The ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation) study found an increased risk of severe hypoglycemia among those with worse MMSE scores (29). In addition to corroborating the findings based on the MMSE, our study extends the relationship to a variety of cognitive domains assessed by the DSST, RAVLT, and Stroop test. Given that these tests assess somewhat overlapping but largely distinct domains (|r| = 0.29–0.47), it seems that the risk of severe hypoglycemia is related to a core cognitive construct or an interrelation of several constructs that is not uniquely captured by one cognitive test (processing speed, memory, and the ability to focus on the task at hand), underscoring the complexity of hypoglycemia prevention in diabetes self-management.
Contrary to the results in persons with type 2 diabetes, the results of DCCT (Diabetes Control and Complications Trial) in participants with type 1 diabetes showed no effect of baseline cognitive ability on subsequent risk of severe hypoglycemia (30). One possible reason for this discrepancy could be a difference in how amenable hypoglycemic episodes are to detection and prevention in type 1 versus type 2 diabetes. A more likely explanation, however, lies in the differences between the study populations. In contrast to the study cohort in ACCORD-MIND, participants in the DCCT trial were much younger (13–39 years of age); had to be free of hypertension, hypercholesterolemia, or other severe medical conditions (31); and may have had an insufficient range of cognitive dysfunction to detect an effect on the risk of hypoglycemia. Furthermore, in the current study, those experiencing HMA had longer diabetes duration and more comorbidities than those who never experienced HMA.
Our study is the first to show that decline in cognitive function is also a risk factor for severe hypoglycemia, particularly among those with lower baseline cognitive function. The results suggest that good cognitive function is critical to safely manage diabetes. Moreover, the severity of the deficits in conjunction with a greater rate of decline increases the risk for severe hypoglycemic events. The likeliest explanation for these findings is that prevention of severe hypoglycemia requires sufficient cognitive skills to coordinate a variety of generic and individual factors including adherence to other drugs, adherence to glucose-lowering drugs, activity levels, dietary patterns, recognition and responsiveness to early symptoms of hypoglycemia, anticipation of situations in which hypoglycemia may occur, and initiation of appropriate mitigating actions. This suggests that cognition should be evaluated when managing people with diabetes and that for people in the lower range of cognitive function, health care providers should pay particular attention to address some or all of these possible mechanisms using established techniques like hypoglycemia anticipation and awareness training (32), and adherence promotion tools (33), etc., and may need to individually tailor therapeutic and monitoring approaches.
The relationship between poor cognitive status or cognitive decline and severe hypoglycemia was not different between the intensive versus standard glycemic therapy groups, consistent with the ADVANCE findings (29). These results suggest that clinicians should be alert to the increased risk of hypoglycemia in patients with poor cognitive status regardless of their current glycemic targets.
The strengths of this study are the prospective ascertainment of severe hypoglycemic episodes and longitudinal assessment of cognitive change over time in a large cohort of people with established type 2 diabetes. Furthermore, the analyses were able to eliminate the confounding effects of recent prior hypoglycemic events on subsequent events and were able to demonstrate robustness of the relationships by using several tests of cognitive function and two definitions of severe hypoglycemia and recurrent severe hypoglycemia. It should be noted, however, that subjects with visual acuity, hearing, or dexterity problems may have had some difficulty with the tests, which could underestimate cognitive function. Furthermore, unmeasured confounding variables may have been missed. The relevance of these findings to patients who are younger, are recently diagnosed, have A1C <8.0%, or do not have vascular disease is unknown.
This study highlights the important impact of cognitive status and cognitive decline on the ability of patients with type 2 diabetes to manage their disease safely. In an era when patients with diabetes are living longer, additional studies are needed to assess the effect of strategies to reduce the impact of cognitive impairment on the risk of severe hypoglycemia and other aspects of diabetes self-management.
Acknowledgments
ACCORD was sponsored by the National Heart, Lung, and Blood Institute (NHLBI), and ACCORD-MIND was sponsored by NHLBI, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Eye Institute, the National Institute on Aging (NIA) and the Intramural Research Program at NIA, and the Centers for Disease Control and Prevention.
The funding agencies had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
No potential conflicts of interest relevant to this article were reported.
Z.P., M.E.M., and H.C.G. researched data, contributed to discussion, wrote the manuscript, and reviewed and edited the manuscript. L.J.L., J.D.W., E.R.S., and R.M.B. researched data, contributed to discussion, and reviewed and edited the manuscript. R.M.L. and F.I.-B. contributed to discussion and reviewed and edited the manuscript. T.C.-Y. and M.D.S. researched data and reviewed and edited the manuscript. L.C.L. reviewed and edited the manuscript. Z.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. no. NCT00000620, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1855/-/DC1.
*A complete list of the ACCORD Group of Investigators and the ACCORD-MIND Investigators can be found in the Supplementary Data.
References
- 1.American Diabetes Association Standards of medical care in diabetes—2009. Diabetes Care 2009;32(Suppl. 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee Organization of Diabetes Care. Canadian Journal of Diabetes 2008;32:S20–S24 [Google Scholar]
- 3.International Diabetes Federation Education. In Global Guideline for Type 2 Diabetes. Brussels, International Diabetes Federation, 2005, p. 15–18 [Google Scholar]
- 4.McGuire LC, Ford ES, Ajani UA. The impact of cognitive functioning on mortality and the development of functional disability in older adults with diabetes: the second longitudinal study on aging. BMC Geriatr 2006;6:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinclair AJ, Girling AJ, Bayer AJ. Cognitive dysfunction in older subjects with diabetes mellitus: impact on diabetes self-management and use of care services. All Wales Research into Elderly (AWARE) Study. Diabetes Res Clin Pract 2000;50:203–212 [DOI] [PubMed] [Google Scholar]
- 6.Buse JB, Bigger JT, Byington RP, et al. ; ACCORD Study Group Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol 2007;99(12A):21i–33i [DOI] [PubMed] [Google Scholar]
- 7.Gerstein HC, Riddle MC, Kendall DM, et al. ; ACCORD Study Group Glycemia treatment strategies in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol 2007;99(12A):34i–43i [DOI] [PubMed] [Google Scholar]
- 8.Williamson JD, Miller ME, Bryan RN, et al. ; ACCORD Study Group The Action to Control Cardiovascular Risk in Diabetes Memory in Diabetes Study (ACCORD-MIND): rationale, design, and methods. Am J Cardiol 2007;99(12A):112i–122i [DOI] [PubMed] [Google Scholar]
- 9.Rosano C, Simonsick EM, Harris TB, et al. Association between physical and cognitive function in healthy elderly: the health, aging and body composition study. Neuroepidemiology 2005;24:8–14 [DOI] [PubMed] [Google Scholar]
- 10.Pavlik VN, de Moraes SA, Szklo M, Knopman DS, Mosley TH, Jr, Hyman DJ. Relation between cognitive function and mortality in middle-aged adults: the atherosclerosis risk in communities study. Am J Epidemiol 2003;157:327–334 [DOI] [PubMed] [Google Scholar]
- 11.Swan GE, Carmelli D, LaRue A. Performance on the digit symbol substitution test and 5-year mortality in the Western Collaborative Group Study. Am J Epidemiol 1995;141:32–40 [DOI] [PubMed] [Google Scholar]
- 12.Proust-Lima C, Amieva H, Dartigues JF, Jacqmin-Gadda H. Sensitivity of four psychometric tests to measure cognitive changes in brain aging-population-based studies. Am J Epidemiol 2007;165:344–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lezak MD. Memory I: tests. In Neuropsychological Assessment. New York, Oxford University Press, 1995, p. 429–498 [Google Scholar]
- 14.Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol 1935;18:643–662 [Google Scholar]
- 15.Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 1992;40:922–935 [DOI] [PubMed] [Google Scholar]
- 16.Cukierman-Yaffe T, Gerstein HC, Williamson JD, et al. ; Action to Control Cardiovascular Risk in Diabetes-Memory in Diabetes (ACCORD-MIND) Investigators Relationship between baseline glycemic control and cognitive function in individuals with type 2 diabetes and other cardiovascular risk factors: the action to control cardiovascular risk in diabetes-memory in diabetes (ACCORD-MIND) trial. Diabetes Care 2009;32:221–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller ME, Bonds DE, Gerstein HC, et al. ; ACCORD Investigators The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ 2010;340:b5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel A, MacMahon S, Chalmers J, et al. ; ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 19.Gerstein HC, Miller ME, Byington RP, et al. ; Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kodl CT, Seaquist ER. Cognitive dysfunction and diabetes mellitus. Endocr Rev 2008;29:494–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brumback T, Cao D, King A. Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug Alcohol Depend 2007;91:10–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lukas SE, Lex BW, Slater JP, Greenwald NE, Mendelson JH. A microanalysis of ethanol-induced disruption of body sway and psychomotor performance in women. Psychopharmacology (Berl) 1989;98:169–175 [DOI] [PubMed] [Google Scholar]
- 23.Heishman SJ, Stitzer ML, Bigelow GE. Alcohol and marijuana: comparative dose effect profiles in humans. Pharmacol Biochem Behav 1988;31:649–655 [DOI] [PubMed] [Google Scholar]
- 24.Beydoun MA, Kaufman JS, Sloane PD, Heiss G, Ibrahim J. n-3 Fatty acids, hypertension and risk of cognitive decline among older adults in the Atherosclerosis Risk in Communities (ARIC) study. Public Health Nutr 2008;11:17–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoyer WJ, Stawski RS, Wasylyshyn C, Verhaeghen P. Adult age and digit symbol substitution performance: a meta-analysis. Psychol Aging 2004;19:211–214 [DOI] [PubMed] [Google Scholar]
- 26.Lee DM, Tajar A, Ulubaev A, et al. ; EMAS study group The association between different cognitive domains and age in a multi-centre study of middle-aged and older European men. Int J Geriatr Psychiatry 2009;24:1257–1266 [DOI] [PubMed] [Google Scholar]
- 27.MacDonald SW, Hultsch DF, Strauss E, Dixon RA. Age-related slowing of digit symbol substitution revisited: what do longitudinal age changes reflect? J Gerontol B Psychol Sci Soc Sci 2003;58:187–194 [DOI] [PubMed] [Google Scholar]
- 28.Wielgos CM, Cunningham WR. Age-related slowing on the Digit Symbol task: longitudinal and cross-sectional analyses. Exp Aging Res 1999;25:109–120 [DOI] [PubMed] [Google Scholar]
- 29.de Galan BE, Zoungas S, Chalmers J, et al. ; ADVANCE Collaborative Group Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial. Diabetologia 2009;52:2328–2336 [DOI] [PubMed] [Google Scholar]
- 30.Austin EJ, Deary IJ. Effects of repeated hypoglycemia on cognitive function: a psychometrically validated reanalysis of the Diabetes Control and Complications Trial data. Diabetes Care 1999;22:1273–1277 [DOI] [PubMed] [Google Scholar]
- 31.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 32.Cox DJ, Kovatchev B, Koev D, et al. Hypoglycemia anticipation, awareness and treatment training (HAATT) reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Int J Behav Med 2004;11:212–218 [DOI] [PubMed] [Google Scholar]
- 33.Misono AS, Cutrona SL, Choudhry NK, et al. Healthcare information technology interventions to improve cardiovascular and diabetes medication adherence. Am J Manag Care 2010;16(Suppl. HIT):SP82–SP92 [PubMed] [Google Scholar]