Abstract
OBJECTIVE
We evaluated the impact of an automated decision support tool (DST) on clinicians’ ability to identify glycemic abnormalities in structured self-monitoring of blood glucose (SMBG) data and then make appropriate therapeutic changes based on the glycemic patterns observed.
RESEARCH DESIGN AND METHODS
In this prospective, randomized, controlled, multicenter study, 288 clinicians (39.6% family practice physicians, 37.9% general internal medicine physicians, and 22.6% nurse practitioners) were randomized to structured SMBG alone (STG; n = 72); structured SMBG with DST (DST; n = 72); structured SMBG with an educational DVD (DVD; n = 72); and structured SMBG with DST and the educational DVD (DST+DVD; n = 72). Clinicians analyzed 30 patient cases (type 2 diabetes), identified the primary abnormality, and selected the most appropriate therapy.
RESULTS
A total of 222 clinicians completed all 30 patient cases with no major protocol deviations. Significantly more DST, DVD, and DST+DVD clinicians correctly identified the glycemic abnormality and selected the most appropriate therapeutic option compared with STG clinicians: 49, 51, and 55%, respectively, vs. 33% (all P < 0.0001) with no significant differences among DST, DVD, and DST+DVD clinicians.
CONCLUSIONS
Use of structured SMBG, combined with the DST, the educational DVD, or both, enhances clinicians’ ability to correctly identify significant glycemic patterns and make appropriate therapeutic decisions to address those patterns. Structured testing interventions using either the educational DVD or the DST are equally effective in improving data interpretation and utilization. The DST provides a viable alternative when comprehensive education is not feasible, and it may be integrated into medical practices with minimal training.
Use of self-monitoring of blood glucose (SMBG) in type 2 diabetes has been shown to facilitate therapy optimization and promote healthy behavioral changes, leading to improved clinical outcomes (1–5). However, SMBG is only useful when the glucose information is collected in a structured manner, the data are accurately interpreted, and the results prompt appropriate therapeutic action (1–5).
In the Structured Testing Program (STeP) study, a large, cluster-randomized, clinical trial, Polonsky et al. (4) demonstrated significant reductions in HbA1c and more timely therapeutic changes when structured SMBG was combined with comprehensive clinician education regarding data interpretation and use. The study used a standardized seven-point glucose data collection tool (Accu-Chek 360° View blood glucose analysis system; Roche Diagnostics, Indianapolis, IN).
A key component of the study’s intervention was comprehensive physician training in both SMBG data interpretation and appropriate application of lifestyle and pharmacologic therapies to address glycemic abnormalities identified in the SMBG data collection tool. The data collection tool was validated in an earlier pilot study (6).
We developed an automated decision support tool that analyzes SMBG data from the 360° View form (Roche Diagnostics) and generates a printed report that identifies the primary glycemic abnormality and recommends appropriate therapeutic options. The purpose of the study was to assess the impact of the use of decision support tool (DST) reports on clinicians’ ability to correctly interpret structured SMBG data and make appropriate therapeutic decisions.
RESEARCH DESIGN AND METHODS
In this 2-month, multicenter, prospective, randomized study, clinicians in the DST group were compared with clinicians who used structured SMBG, alone, structured SMBG with an SMBG training program (DVD), and structured SMBG with both the SMBG training program and the decision support tool (DST+DVD). The study used 30 prepared patient cases from the STeP trial, which were reviewed by an expert panel of diabetes specialists. Clinicians were asked to analyze each patient case, identify the primary abnormality, and select the most appropriate class of drug to treat the abnormality identified. Clinicians were also asked to complete electronic questionnaires after the complete evaluation of all case studies to obtain feedback on the DST report and educational program, according to study group.
The primary objective of this study was to assess the impact of the use of decision support tool reports on clinicians’ ability to correctly interpret structured SMBG data and make appropriate therapeutic decisions.
Subjects
The study randomized 288 clinicians for the study. Practice specialties included: family practice physicians (39.6%), general internal medicine physicians (37.9%), and nurse practitioners (22.5%), who were identified and recruited using defined clinician selection criteria. Inclusion criteria were: board certification in family practice, general internal medicine or certified nurse practitioner; current licensure to practice in good standing, actively engaged in clinical practice full time (≥30 h per week), currently recommended SMBG to their type 2 diabetes patients, and possessed a valid e-mail address and computer access. Clinicians were excluded from the study if they currently used specialized structured testing data collection forms in their practices, were actively engaged in educating interns, residents, medical students, or other healthcare professionals, or were recognized as a specialist in diabetes care.
Randomization
Eligible clinicians were randomized to four groups using a randomization scheme provided by the statistician to ensure balanced representation of family practice physicians, general internal medicine physicians, and nurse practitioners in each group and that clinicians from small and large practice groups and managed care organizations were represented among all study groups. The four study groups were: 1) structured SMBG, alone, using the 360° View tool (STG; n = 72), 2) structured SMBG with the DST (DST; n = 72), 3) structured SMBG with an SMBG training program (DVD; n = 72), and 4) structured SMBG with decision support tool and SMBG training program (DST+DVD; n = 72). Cases were presented to each clinician in random order according to a defined randomization scheme. All clinicians reviewed the same cases.
Materials
Seven-Point SMBG Data Collection Tool (Accu-Chek 360° View).
This validated tool enables patients to record and plot a seven-point SMBG profile (fasting, preprandial/2-h postprandial at each meal, bedtime) on 3 consecutive days (see Supplementary Materials and Methods). The tool allows patients to document meal sizes and energy levels and to comment on their SMBG experiences (6).
DST.
The Accu-Chek 360° Automated DST was developed to produce an automated analysis of a 3-day structured SMBG regimen and provide corresponding medical information (see Supplementary Materials and Methods). The DST is based on the Accu-Chek 360° View tool and supporting information in the video “Making Sense of Your Blood Glucose Monitoring Results.” The DST graphs and tabulates the completed SMBG results and provides an automated analysis of results by identifying patterns and incidences of hypoglycemia, fasting/preprandial hyperglycemia, and 2-h postprandial hyperglycemia. The DST was supported by a brief orientation video that was to be viewed by DST and DST+DVD clinicians.
SMBG training program.
The educational DVD program (Making Informed Therapy Decisions Using Structured SMBG) is a 28-min presentation that provides information about basic SMBG pattern management, identification of glycemic abnormalities, and use of SMBG data to initiate and adjust pharmacologic therapy. Content of the program is based on the live training provided to clinicians in the STeP study intervention group (4).
Case studies.
The Expert Panel determined the primary glycemic feature and best therapeutic course for each case study (see Supplementary Materials and Methods). The case studies included patient HbA1c, age, ethnicity, height, weight, BMI, duration of diabetes, current medications, patient-reported information regarding disease management, and completed 360° View forms. Glycemic abnormalities included patterns of hypoglycemia (≤80 mg/dL), fasting/preprandial hyperglycemia (≥111 mg/dL), and postprandial hyperglycemia (>50 mg/dL excursion above fasting/preprandial level). These glucose cut points mirror the glycemic thresholds used in the STeP study (4). A breakout of the cases evaluated by study clinicians is as follows: 1 euglycemia; 7 hypoglycemia; 15 fasting/preprandial hyperglycemia; 5 2-h postprandial hyperglycemia; 1 falsified data; and 1 insufficient data. Participants reviewed the patient case studies and completed a series of questions for each case regarding the primary glycemic feature and best course of therapeutic action from the choices provided. After completing their evaluation of all the case studies, participants were asked to complete electronic exit questionnaires in order to provide feedback on the DST report, 360° View tool, and the SMBG training DVD, based upon their study group.
Statistical analysis
All statistical analyses were conducted based on the per protocol set (PP). The PP set includes all randomized clinicians who reviewed all 30 of the case studies without any major protocol deviations. Major protocol deviations included: missing ≥5 min of SMBG training DVD; missing ≥1 min of the DST orientation video; or not reviewing any of the resources before answering case study questions for >10% of case studies.
The percentage of clinicians who correctly identified the primary glycemic feature was analyzed using generalized linear mixed model with each group (STG, DST, DVD, and DST+DVD) and type of health care provider as fixed effects; the empirical covariance estimator was computed to account for the dependence of all case study data from each clinician. Multiple comparisons between the four groups were adjusted by a simulation-based approach in the same mixed model procedure. Comparisons of clinicians’ ability to correctly interpret structured SMBG data were conducted based on the same mixed model as the following: 1) STG versus DST, benefit of DST information on ability to correctly interpret structured SMBG data; 2) STG versus DVD, benefit of SMBG training; 3) STG versus DST+DVD, benefit of DST information and SMBG training; 4) DST versus DVD, determine if DST information is more valuable than SMBG training; 5) DST versus DST+DVD, determine if provision of DST information and SMBG training is superior to provision of DST information alone; and 6) DVD versus DST+DVD, determine if provision of DST information combined with SMBG training is superior to provision of SMBG training alone. The percentage of clinicians who correctly identified the appropriate clinical decision and percentage of clinicians who correctly identified both the primary glycemic feature and the appropriate clinical decision were analyzed in the same manner. Data manipulation, tabulations of descriptive statistics, and statistical modeling and inference were performed using SAS Version 9.1.3 (SAS Institute, Cary, NC).
Based on previous data (6), ∼82% of the STG participants were expected to correctly interpret SMBG data on average across all 30 case studies and the correlation coefficient within each participant were estimated to be 0.3. Additionally, we assumed that ∼15% of the participants would not comply with the protocol. A total of 65 participants per group were required to achieve at least 95% power to detect a difference of 15% for each pairwise comparison between the four study groups (per-comparison type I error rate = 0.0085, two-sided test; family-wise type I error rate = 0.05). Recognizing that the assumed 82% accuracy rate for STG clinicians was much higher than the actual results, 51% for identification of primary glycemic feature and 33% for identification of primary glycemic feature and selection of appropriate therapeutic option, we conducted additional power analyses, replacing 82 with 51 and 33%, respectively. Although the poststudy power dropped to 87% for both outcome variables, this was still acceptable.
RESULTS
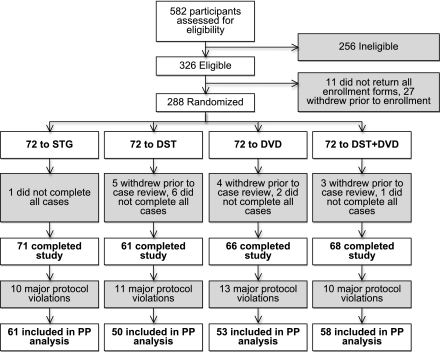
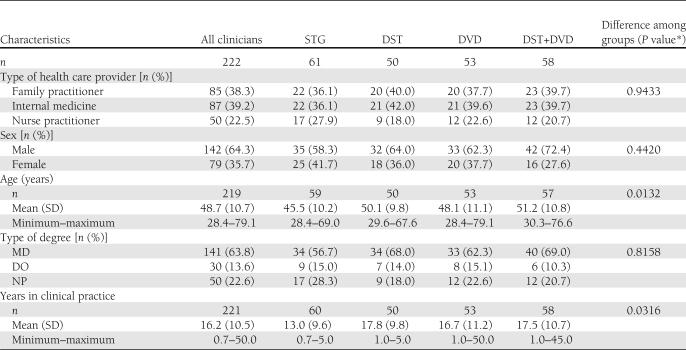
Of 582 clinicians assessed for eligibility, 288 were randomized to the four study groups (Fig. 1). A total of 222 (77%) clinicians completed all 30 patient cases with no major protocol deviations: n = 61, STG; n = 50, DST; n = 53, DVD; and n = 58, DST+DVD. Clinician characteristics among the four groups differed only by age and years in clinical practice; STG clinicians tended to be younger with fewer years in clinical practice than clinicians in the other study groups (Table 1). Age, sex, and years in practice had no significant main effects on clinicians’ ability to identify the primary glycemic patterns or make appropriate clinical decisions. The following results present findings from the PP analysis set.
Figure 1.
Consort diagram.
Table 1.
Subject characteristics
Identification of primary glycemic abnormality and selection of appropriate therapeutic option
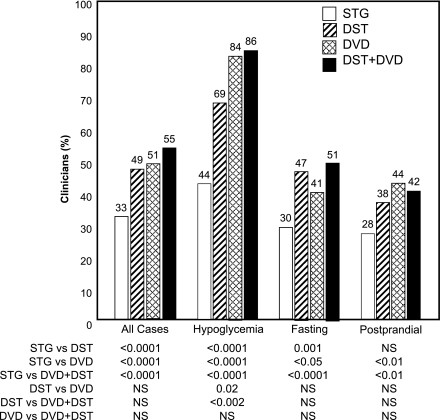
In all cases, significantly more DST (49%), DVD (51%), and DST+DVD (55%) clinicians correctly identified the glycemic abnormality and selected the most appropriate therapeutic option compared with STG (33%) clinicians (all P < 0.0001), with no significant differences among DST, DVD, and DST+DVD clinicians (Fig. 2). Significantly fewer DST clinicians correctly identified and selected appropriate treatment for hypoglycemia compared with DVD and DST+DVD clinicians. There was no significant difference between DST and STG clinicians in identifying and recommending treatment for postprandial hyperglycemia.
Figure 2.
Percentage of clinicians who correctly identified primary glycemic abnormalities and selected the most appropriate therapeutic option in all cases.
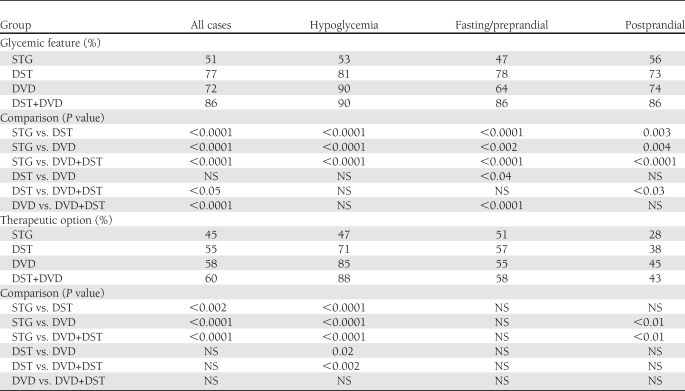
Significant between-group differences were also seen in clinicians’ ability to: 1) identify primary glycemic features; and/or 2) select appropriate therapeutic options associated with the glycemic patterns identified (Table 2).
Table 2.
Percentage of clinicians who correctly identified primary glycemic abnormalities and selected the most appropriate therapeutic option
Time spent with case studies
The mean (SD) time all clinicians spent with all of the cases was 65.6 ± 32.9 min. Significant differences were seen between the STG and DST+DVD groups (63.8 ± 34.9 vs. 72.0 ± 29.6 min; P = 0.03), DST and DVD groups (68.8 ± 34.5 vs. 57.7 ± 31.0 min; P < 0.01), and DVD and DST+DVD groups (57.7 ± 31.0 vs. 72.0 ± 29.6 min; P < 0.001).
Exit surveys
Approximately 94% of all clinicians felt that the information provided in the data collection tool is more accurate than data provided in traditional logbooks; there were no significant between-group differences in this assessment. The majority of clinicians (75.2%) felt that the data collection tool provided more useful information than HbA1c data; however, significantly (P < 0.02) fewer STG clinicians (62.3%) agreed or strongly agreed with this assessment than those in the DVD (83.0%) and DST+DVD (87.9%) groups, with no significant difference between the STG and DST groups.
Overall, >90% of DST and DST+DVD clinicians felt the automated data support tool provided clinically useful information and enhanced interpretation of the SMBG data. After viewing the training DVD, >95% of clinicians felt that they could more accurately identify glycemic patterns presented in the data collection tool and that they could use the SMBG data to adjust patient medications.
CONCLUSIONS
SMBG is most useful when the glucose data are collected in a structured manner, the data are accurately interpreted, and the results prompt appropriate therapeutic actions. Recent studies have demonstrated that structured SMBG has the ability to significantly improve diabetes outcomes (1–5). The STeP study demonstrated the clinical efficacy of structured SMBG when combined with comprehensive clinician education (4). We demonstrated that use of structured SMBG, in combination with a DST, SMBG training, or both, enhances clinicians’ ability to correctly identify significant glycemic patterns and make appropriate therapeutic decisions to address those patterns. Although both the DST report and training DVD were effective in improving ability of clinicians to interpret data, the combination of the two tools was superior. Although both the DST and training DVD were also equally effective in improving clinicians’ ability to select the best therapeutic option, the combination of the DST and training DVD showed no superiority over use of either tool. This was also evidenced when assessing clinicians’ ability to both interpret the data and select the most appropriate therapeutic option.
However, even with the benefit of both the DST and SMBG training, alone or used in combination, many clinicians did not accurately identify and appropriately treat the primary glycemic abnormality, according to the training and support materials provided. Although this could be partially explained by participants choosing to exercise their own clinical judgment in the case assessments, we believe our results underscore the need for further improvement in clinical diabetes management.
A large majority of clinicians in all study groups felt that the information provided by the data collection was more accurate than traditional logbook data and that it was more useful in making therapy decisions than HbA1c values. Interestingly, this sentiment was strongest among clinicians who used both the DST and training DVD, thus reinforcing the idea that structured SMBG should be viewed as a comprehensive approach to diabetes care rather than simply a recipe for testing, an approach that requires a defined algorithm for testing, the ability to understand and interpret the glucose data, and the ability to make appropriate therapeutic decisions based on those data.
A key limitation of the study was absence of a pure control arm (e.g., unstructured glucose data presented in a logbook) that would have assessed the effect of use of the data collection tool compared with use of traditional, random glucose testing, which is normally seen in family practice. Given the findings from the STeP study (4) and other recent trials (1–3,5), our results may overestimate the level of accuracy in SMBG data interpretation and therapy selection found in real-world clinical practices where structured SMBG is seldom used.
Our findings demonstrate that structured SMBG interventions that employ both decision support and education are superior to use of structured SMBG alone. Although use of either the educational DVD or the DST are equally effective in improving data interpretation and utilization, the DST provides a viable alternative when comprehensive education is not feasible, and it may be integrated into medical practices with minimal training. However, given the significant percentage of clinicians who did not identify the primary abnormality, select the most appropriate therapeutic options, or both, additional training (specifically in the area of therapeutic adjustments) may be needed in order to optimize use of structured SMBG in clinical practice.
Acknowledgments
Funding for the study was provided by Roche Diagnostics. H.W.R., O.S., J.U., C.G.P., and Z.J. have provided consulting services to Roche Diagnostics. C.R., L.A., N.W., M.A.-S., and R.S.W. are employees of Roche Diagnostics. No other potential conflicts of interest relevant to this article were reported.
H.W.R., O.S., J.U., C.R., L.A., N.W., M.A.-S., and R.S.W. developed the study concept and protocol. H.W.R., O.S., J.U., C.G.P., and R.S.W. developed the manuscript. H.W.R., O.S., J.U., C.R., L.A., N.W., C.G.P., Z.J., N.W., M.A.-S., and R.S.W. participated in data analysis, contributed to the discussion, and reviewed and edited the manuscript. L.A. served as clinical operations study manager. Z.J. performed statistical analysis. C.G.P. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in poster form at the 71st Scientific Sessions of the American Diabetes Association, San Diego, California, 24–28 June 2011.
The authors thank Drs. Charles Schikman, private medical practice, and David Tetrick, Community Health Network, for assistance in case study development. The authors also thank Lisa Curtis, Roche Diagnostics, for study monitoring and organizational support.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1351/-/DC1.
References
- 1.Durán A, Martín P, Runkle I, et al. Benefits of self-monitoring blood glucose in the management of new-onset Type 2 diabetes mellitus: the St Carlos Study, a prospective randomized clinic-based interventional study with parallel groups. J Diabetes 2010;2:203–211 [DOI] [PubMed] [Google Scholar]
- 2.Kempf K, Kruse J, Martin S. ROSSO-in-praxi: a self-monitoring of blood glucose-structured 12-week lifestyle intervention significantly improves glucometabolic control of patients with type 2 diabetes mellitus. Diabetes Technol Ther 2010;12:547–553 [DOI] [PubMed] [Google Scholar]
- 3.Bonomo K, De Salve A, Fiora E, et al. Evaluation of a simple policy for pre- and post-prandial blood glucose self-monitoring in people with type 2 diabetes not on insulin. Diabetes Res Clin Pract 2010;87:246–251 [DOI] [PubMed] [Google Scholar]
- 4.Polonsky WH, Fisher L, Schikman CH, et al. Structured self-monitoring of blood glucose significantly reduces A1C levels in poorly controlled, noninsulin-treated type 2 diabetes: results from the Structured Testing Program study. Diabetes Care 2011;34:262–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Franciosi M, Lucisano G, Pellegrini F, Cantarello A, Consoli A, Cucco L, et al. ROSES: role of self-monitoring of blood glucose and intensive education in patients with Type 2 diabetes not receiving insulin. A pilot randomized clinical trial. Diabet Med 2011;28:789–796 [DOI] [PubMed] [Google Scholar]
- 6.Polonsky WH, Jelsovsky Z, Panzera S, Parkin CG, Wagner RS. Primary care physicians identify and act upon glycemic abnormalities found in structured, episodic blood glucose monitoring data from non-insulin-treated type 2 diabetes. Diabetes Technol Ther 2009;11:283–291 [DOI] [PubMed] [Google Scholar]