Abstract
OBJECTIVE
To investigate the association of lipoprotein-associated phospholipase A2 (LpPLA2) mass and activity with incident cardiovascular disease (CVD) in a population with high prevalences of insulin resistance and diabetes, conditions for which epidemiological data remain sparse.
RESEARCH DESIGN AND METHODS
We conducted a nested, case-control study (n = 1,008) within a population-based cohort of American Indians. Case subjects were defined by incidence of first-ever CVD up to 10 years later. Control subjects comprised participants free of CVD events during the follow-up period who were frequency matched to case subjects by age, sex, and diabetes status. LpPLA2 mass and activity were measured using commercially available assays.
RESULTS
LpPLA2 mass and activity were moderately correlated with each other (r = 0.30), but only LpPLA2 activity exhibited moderate correlations with lipid fractions. After extensive adjustment for covariates, both LpPLA2 measures were significantly associated with incident CVD, but the relationship was inverse for LpPLA2 mass (highest versus lowest tertile, relative risk [RR] 0.55 [95% CI 0.39–0.79]) and positive for LpPLA2 activity (highest versus lowest tertile, 1.65 [1.12–2.42]). These associations were similar when participants with and without diabetes were examined separately.
CONCLUSIONS
In this population-based cohort enriched with dysmetabolic phenotypes, LpPLA2 mass and activity showed divergent associations with CVD. The inverse relationship for LpPLA2 mass is contrary to observations from predominantly nondiabetic populations and will require independent replication. Whether this finding relates to redistribution of LpPLA2 to lipoprotein classes where it is less atherogenic or reflects incomplete measurement of LpPLA2 mass associated with altered lipoprotein composition in insulin resistance warrants further investigation.
Recognition of the seminal role of inflammation in atherogenesis (1) has led to a search for key molecular drivers of the vascular inflammatory response as potential therapeutic targets or markers of prognosis in at-risk individuals. One such candidate is the enzyme lipoprotein-associated phospholipase A2 (LpPLA2), a secretory product of inflammatory cells that binds primarily to apolipoprotein B–containing lipoproteins such as LDL (2). Because excess LDL accumulates within the subendothelial space during atherogenesis, LpPLA2 function may have particular specificity for inflammation within the vascular compartment (3).
LpPLA2 catalyzes the hydrolysis of oxidized phospholipids to lysophosphatidyl choline and oxidized, nonesterified fatty acids, mediators that can trigger inflammatory cell activation and retard clearance of apoptotic cells within the atheroma’s necrotic core (4). Such proinflammatory actions would act to foster progression of atherosclerosis and plaque instability (4). The pathophysiologic role of LpPLA2 in atherosclerosis remains controversial, however, because the enzyme’s removal of proatherogenic oxidized phospholipids can itself have an atheroprotective effect (3). Moreover, in vitro LpPLA2 can also hydrolyze platelet-activating factor (PAF), which is a potent mediator of thrombotic, allergic, and inflammatory responses (3). Although degradation of PAF would serve an anti-inflammatory function, the extent to which LpPLA2 can effect PAF breakdown in vivo remains uncertain (3,4).
Against such experimental observations is a large body of epidemiological studies that have predominantly found a positive association between LpPLA2 mass and activity and cardiovascular outcomes (5). Few studies to date, however, have addressed the link between LpPLA2 and clinical events in populations with high prevalences of insulin resistance and diabetes, disorders where vascular inflammation and oxidative stress are particularly pronounced (6). We examined the relations between LpPLA2 mass and activity and incident cardiovascular disease (CVD) in a population-based cohort of American Indians enriched with dysmetabolic phenotypes.
RESEARCH DESIGN AND METHODS
Study population
The Strong Heart Study (SHS) is a population-based longitudinal survey of CVD in 13 American Indian communities, as detailed previously (7). Herein, we conducted a nested, case-control study of participants without prevalent CVD or dialysis dependence at the second SHS exam (n = 2,941). Prevalent CVD comprised definite coronary heart disease (CHD), definite stroke, congestive heart failure (CHF), and atrial fibrillation. The second SHS exam entailed clinical and laboratory evaluation between 1993 and 1995, as previously described (7). Case subjects consisted of 504 participants who developed CVD during follow-up through December 2003. Control subjects included participants who remained free of clinical CVD during this period and were frequency matched (1:1) to case subjects by age, sex, and diabetes status.
Definition of clinical variables and determination of end points
Hypertension was defined as blood pressure ≥140/90 mmHg or antihypertensive therapy, diabetes as fasting glucose ≥126 mg/dL or glucose-lowering treatment, and BMI as the ratio of weight (kilograms) to the square of height (meters). Metabolic syndrome was defined according to National Cholesterol Education Program criteria (8). Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as fasting insulin (μU/mL) × fasting glucose (mmol/L)/22.5 (9). Insulin resistance was defined according to a previous classification scheme as BMI >28.9 kg/m2 and HOMA-IR >4.65, or BMI >27.5 kg/m2 and HOMA-IR >3.60, among participants without diabetes (10). Glomerular filtration rate was estimated (eGFR) using the modification of diet in renal disease equation (11).
The primary end point of major CVD events was defined as definite, nonfatal myocardial infarction (MI), CHD, or stroke and cardiovascular death. Criteria for nonfatal CVD events have been previously described (7). Deaths were identified, verified, and classified as attributable to CVD if caused by MI, sudden death from CHD, stroke, or CHF using standardized procedures (7).
Laboratory methods
LpPLA2 mass and activity were measured at the SHS Core Laboratory in serum samples stored at −80°C. In prior studies (5), determinations of LpPLA2 mass and activity after long-term storage have yielded values whose distributions and correlations to other analytes have been consistent with recently drawn samples. LpPLA2 mass was measured in duplicate from May to September 2008 on never-thawed specimens by ELISA (PLAC III; diaDexus, Inc.). The intra-assay and interassay coefficients of variation (CVs) were both 8%. These were determined by testing four human serum pools with LpPLA2 concentrations distributed throughout the assay’s calibration range. For intra-assay CV, the samples were tested 20 times on one plate. For interassay CV, the samples were tested in duplicate, two separate assays per day, for 5 days. In view of the unexpected association with CVD observed for LpPLA2 mass, additional funding was requested for determination of LpPLA2 activity, which was measured in the same samples previously thawed once for the LpPLA2 mass determinations. LpPLA2 activity was measured in singlicate in January 2011 using a colorimetric assay (diaDexus, Inc.) for hydrolysis of labeled PAF (GlaxoSmithKline, Research Triangle Park, NC). Intra-assay CVs were 1.3 and 0.8%, whereas interassay CVs were 2.0 and 1.0%, for low and high activity standards, respectively.
The concentrations of high-sensitivity C-reactive protein (hsCRP) and fibrinogen were determined by ELISA (12) and a modified Clauss method (13), respectively. HbA1c was assessed by high-pressure liquid chromatography (14). The urine albumin/creatinine ratio (UACR) was obtained from a single spot urine (7). Lipoprotein (a) mass, measured by immunoassay during the first SHS exam, was available in 710 participants (15).
Statistical analysis
Categorical variables were compared by the χ2 test, and continuous variables by the Wilcoxon rank sum test. Correlations were evaluated by Spearman coefficients. Effect modification of LpPLA2’s relations with lipid fractions by diabetes was examined by including cross-product terms in linear regression models. Unconditional logistic regression was used to evaluate multivariable-adjusted associations of sex-specific tertiles of LpPLA2 mass and activity with incident CVD. This involved fitting sequential models that adjusted first for age (continuous), sex, and diabetes (yes/no); and then additionally for hypertension (yes/no), BMI (continuous), LDL and HDL (both continuous), smoking status (current versus ever/never), and serum creatinine, UACR, and hsCRP (all continuous); and subsequently for HbA1c (continuous), diabetes duration (continuous), oral hypoglycemics (yes/no), and insulin therapy (yes/no). Tests for linear trend used an ordinal indicator variable for tertiles. Subsequent models also assessed alcohol use, antihypertensive medication, estrogen therapy, and fibrinogen, as well as exclusion of participants receiving lipid-lowering therapy. Moreover, associations were examined among participants with and without diabetes separately. We also assessed the impact of excluding participants with advanced kidney disease (eGFR <30 mL/min/1.73 m2) and macroalbuminuria (UACR ≥300 mg/g). All analyses were conducted with SPSS version 19.0 (SPSS Inc., Chicago, IL).
RESULTS
Baseline characteristics
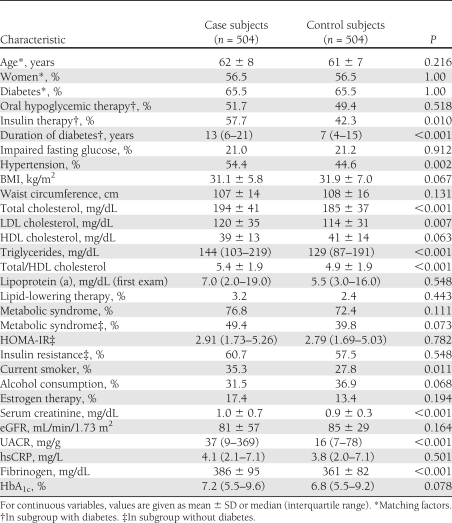
Of the 504 case subjects, 239 had fatal/nonfatal MI, 90 fatal/nonfatal stroke (87 ischemic), and 12 both; 175 had fatal/nonfatal CHD, 4 fatal CHF, and 8 other fatal CVD. Overall, 56.8% of the study cohort was obese; 72.6% had the metabolic syndrome; 21.1 and 65.5% had impaired fasting glucose and diabetes, respectively; 17.2 and 2.7% had eGFR <60 and <30 mL/min/1.73 m2; and 26.7 and 18.3% had micro- and macroalbuminuria. Diabetic participants had median HbA1c of 8.6% and duration of diabetes of 10 years; 33.6% were on insulin therapy. Of those without diabetes, 59.1% were insulin resistant. These and other characteristics are presented in Table 1 according to case/control subject status. Case subjects were similar to control subjects in age, sex, and diabetes as a result of frequency matching, but had greater hypertension, current smoking, insulin use, and duration of diabetes than control subjects. Case subjects also had higher lipids, serum creatinine, UACR, and fibrinogen.
Table 1.
Baseline characteristics of study cohort
Levels and correlations of LpPLA2 mass and activity
Valid measurements were obtained in 491 case subjects and 492 control subjects for LpPLA2 mass, and 494 case subjects and 499 control subjects for LpPLA2 activity. LpPLA2 mass levels were lower in case subjects than control subjects (median 306 [IQR 235–409] vs. 342 [264–452] μg/L, P < 0.001), in women than men (317 [241–408] vs. 332 [245–450] μg/L, P = 0.049), and in participants with diabetes than without (313 [239–422] vs. 342 [264–438] μg/L, P = 0.034), but did not differ among nondiabetic participants with and without insulin resistance (338 [251–443] vs. 352 [267–440] μg/L, P = 0.523). LpPLA2 activity was higher in case subjects than control subjects (228 [194–280] vs. 216 [178–260] μmol/min/L, P < 0.001), lower in women than men (209 [178–249] vs. 246 [199–290] μmol/min/L, P < 0.001), and similar in diabetic and nondiabetic subjects (222 [188–271] vs. 223 [183–270] μmol/min/L, P = 0.676) or in nondiabetic individuals with and without insulin resistance (231 [188–276] vs. 213 [177–265] μmol/min/L, P = 0.156).
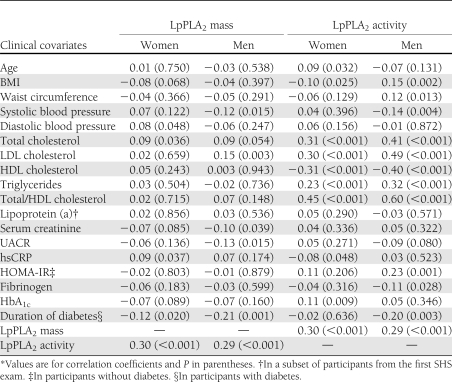
Correlations between LpPLA2 measures and baseline covariates are shown in Table 2. For LpPLA2 mass, there were modest positive correlations with total cholesterol and hsCRP in women, and with LDL in men. Men also exhibited modest negative correlations between LpPLA2 mass and systolic blood pressure, serum creatinine, UACR, and, as did women, diabetes duration. In turn, LpPLA2 activity showed modest positive correlations in women with age and HbA1c, and modest negative correlations with BMI and hsCRP. In men, the correlations of LpPLA2 activity with BMI and waist circumference were instead modestly positive, whereas for systolic blood pressure and fibrinogen, they were modestly negative. Men without diabetes showed a moderate positive correlation for LpPLA2 activity with HOMA-IR, but those with diabetes exhibited a moderately negative correlation with diabetes duration. Moreover, there were moderately strong, positive correlations in both sexes between LpPLA2 activity and total cholesterol, LDL, triglycerides, and total/HDL cholesterol, along with a moderate negative correlation with HDL. These correlations tended to be stronger in men than women. Furthermore, the correlations between LpPLA2 mass and LpPLA2 activity were moderate in both sexes.
Table 2.
Cross-sectional correlates* of LpPLA2 mass and activity
When correlations were examined in subgroups with and without diabetes (Supplementary Table), modest correlations were observed only among diabetic participants for LpPLA2 mass with hsCRP (positive), and with UACR, HbA1c, and diabetes duration (negative). By contrast, LpPLA2 activity showed a modest negative correlation with hsCRP and fibrinogen, though not HbA1c in diabetic subjects, but was again negatively correlated with diabetes duration. LpPLA2 activity was also modestly negatively correlated with UACR in nondiabetic subjects, in whom its correlations with lipid fractions tended to be stronger than among diabetic participants.
We next tested whether the associations of LpPLA2 mass or activity with LDL, HDL, and total/HDL cholesterol, hsCRP, HbA1c, and UACR were modified by diabetes status in age- and sex-adjusted linear models. There was no significant effect modification by diabetes (P ≥ 0.13) except in the case of LpPLA2 activity’s relation to total/HDL cholesterol (P = 0.007), for which the partial coefficient was modestly higher for nondiabetic than diabetic participants (r = 0.59 vs. 0.47). These findings were not influenced by diabetes medications.
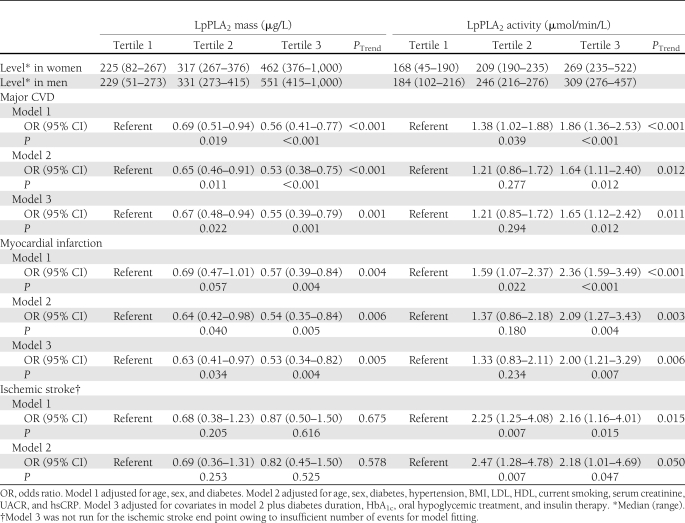
LpPLA2 mass and outcome
Table 3 shows the relationship between tertiles of LpPLA2 mass and major CVD. There was a significant inverse association across increasing tertiles of LpPLA2 mass with incident CVD after adjustment for matching variables, which persisted after controlling for other clinical and laboratory covariates. After full adjustment for potential confounders, there was a 33% lower RR of CVD for the middle versus the lower tertile (P = 0.022), and a 45% lower risk for the upper versus the lower tertile (P = 0.001). Findings were similar when waist circumference replaced BMI, total/HDL cholesterol replaced LDL and HDL, and eGFR replaced serum creatinine. Nor were effect estimates influenced by additional adjustment for antihypertensive medication, alcohol, estrogen therapy, fibrinogen, or lipoprotein (a) (data not shown). Moreover, exclusion of participants with kidney disease did not affect the results.
Table 3.
Associations of tertiles of LpPLA2 mass and activity with CVD
A similar relationship was observed for LpPLA2 mass when the outcome was limited to MI (Table 3). For ischemic stroke, risk estimates were also suggestive of a negative association, but there was lack of precision reflecting fewer events.
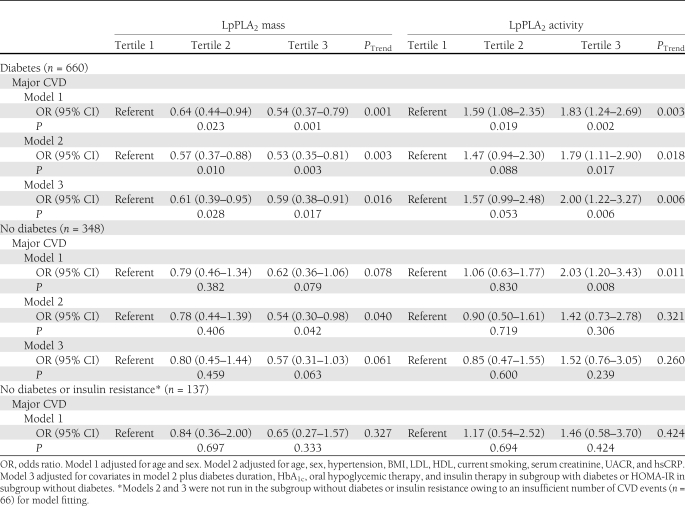
Likewise, when analyses were stratified by diabetes status, there was an inverse association among diabetic participants that was comparable to that seen overall (Table 4). The relationship was similar among participants without diabetes at different levels of adjustment, although it became nonsignificant after inclusion of HOMA-IR. To further assess the influence of dysglycemia on the inverse relationship, we explored the age- and sex-adjusted association among participants without diabetes or insulin resistance. As in nondiabetic participants, risk estimates were attenuated as compared with age- and sex-adjusted values in diabetic subjects, albeit with broad 95% CIs.
Table 4.
Associations of tertiles of LpPLA2 mass and activity with CVD in subgroups with and without diabetes
LpPLA2 activity and outcome
As also shown in Table 3, LpPLA2 activity manifested the opposite association with incident CVD, with a significant graded increase in risk across increasing tertiles. The association was attenuated after adjustment for clinical and laboratory factors, but there was still a 65% higher risk of major CVD for the upper tertile in the fully adjusted model (P = 0.012). These findings were not meaningfully altered with consideration of waist circumference, total/HDL cholesterol, or eGFR as alternative covariates. Nor did adjustment for additional baseline covariates or exclusion of participants with kidney disease materially affect results.
The association of LpPLA2 activity with MI alone was also positive, with numerically stronger risk estimates than for the composite CVD end point (Table 3). A stronger positive association was also present for ischemic stroke, but precision was again low.
Among diabetic participants, the association between LpPLA2 activity and major CVD was similar to the entire cohort’s. The risk estimates strengthened, however, with further adjustment for diabetes duration, HbA1c, and diabetes medications. Likewise, a significant positive association was observed in the nondiabetic subset after adjustment for matching factors. The relationship was attenuated and ceased to be significant, however, with more extensive adjustment in this smaller subgroup or in its subset without insulin resistance.
CONCLUSIONS
Main findings
In this cohort with high prevalences of glycometabolic abnormalities, we found paradoxical associations between LpPLA2 mass and activity and first-ever CVD. Specifically, LpPLA2 mass and LpPLA2 activity showed directionally opposite relationships with incident CVD, wherein LpPLA2 mass was inversely associated, but LpPLA2 activity was positively associated, with this outcome. These associations did not show significant differences between subgroups with and without diabetes and were, moreover, directionally consistent for the component end points of MI and ischemic stroke.
Previous studies of LpPLA2 and CVD events in diabetes
Although previous population-based studies of LpPLA2 and CVD have included variable proportions of participants with diabetes, few investigations have focused on cohorts composed exclusively or predominantly of individuals with dysglycemia. In a study that combined male and female diabetic participants in the Health Professionals Follow-up Study and the Nurses’ Health Study, there was a significant positive association between LpPLA2 activity and incident CHD, but no significant relationship was detected for LpPLA2 mass (16). Interestingly, the correlation between LpPLA2 mass and activity in that subgroup of white health professionals was identical to the one observed in our cohort, and their adjusted risk estimate for the comparison of extreme tertiles of LpPLA2 activity for nonfatal MI and fatal CHD was of similar, if modestly lower, magnitude to ours for the same outcome (RR 1.75 [95% CI 1.05–2.92] vs. 1.95 [1.22–3.09]). Because the risk estimates of LpPLA2 mass for CHD were not reported (16), however, we are unable to compare the relationship therein with the inverse association observed here.
A second study also examined the prospective association of LpPLA2 mass and activity with CVD specifically in a diabetic subset (17). In this sample of mostly white older adults from the Cardiovascular Health Study, no significant association between LpPLA2 mass or activity and CVD, including CHF, was observed (adjusted RRs of 1.24 [95% CI 0.90–1.71] and 0.95 [0.69–1.32], respectively, for values above versus below the 75th percentile) (17).
Data from the above investigations, however, were included in the LpPLA2 Studies Collaboration, a meta-analysis of prospective studies that also evaluated cohorts with prevalent CVD (5). Pooling of the findings from diabetic participants across studies (n = 8,427 participants; 18% of total) revealed a significant positive association between LpPLA2 mass and CHD (RR 1.16 per SD [95% CI 1.05–1.28]), which was comparable to that observed in the larger sample without diabetes (5).
Potential explanations for findings
The inverse association between LpPLA2 mass and CVD detailed here is unanticipated. Not only is it divergent from the positive relationship documented for LpPLA2 activity in the same cohort, but also runs counter to available epidemiological evidence of positive or null associations (5). Such evidence, however, comes from the predominantly nondiabetic populations of European descent included in the LpPLA2 Studies Collaboration, although subgroup analysis of diabetic participants showed a consistent association (5). Our American Indian population differs from such cohorts in its greater severity and duration of diabetes, and in its predominance of women, rather than men. The current study also excluded prevalent CVD, which did not significantly influence the overall associations of LpPLA2 mass with outcomes in the above meta-analysis but was associated with higher risk estimates, particularly for vascular death (5).
A central consideration in attempting to account for our findings is that, much as LpPLA2 function is closely dependent on the type of lipoprotein to which it is complexed (18,19), the measurable fraction of LpPLA2 mass may vary for different lipoprotein particles (19). Specifically, immunoassay methods for determination of LpPLA2 mass appear not to detect all active enzyme in LDL, as they do for HDL (19). The same problem, however, does not apply to LpPLA2 activity, plasma measurement of which is not influenced by its companion lipoprotein.
Approximately 75% of plasma LpPLA2 circulates bound to apolipoprotein-B–containing particles, principally LDL, with the remainder associating with HDL. Furthermore, the enzyme has particular affinity for smaller LDL particles (20,21), levels of which are increased in the setting of insulin resistance and type 2 diabetes (22). We observed that LpPLA2 mass, but not activity, was lower in participants with diabetes than without in our cohort, consistent with prior findings from the LpPLA2 Studies Collaboration, which also documented lower levels of LpPLA2 mass in diabetic individuals (5). Because redistribution of LpPLA2 to small LDL particles might amplify its proatherogenic effects, yet make enzyme mass less available for detection by immunoassay, such redistribution could provide an explanation for the divergent associations observed for LpPLA2 mass and activity. The higher the absolute level of small LDL particles and the proportion of LpPLA2 complexed with them, the lower the measurable concentration of LpPLA2 mass but the greater the measurable LpPLA2 activity, and with it, the heightened atherogenicity resulting from increased concentrations of LpPLA2–small-LDL complexes. This explanation might seem at odds with the weak correlation between LpPLA2 mass and total LDL observed here in men only, but LpPLA2 mass, unlike activity, has been reported to be a poor measure of smaller LDL particles (19).
Lower levels of LpPLA2 mass were also reported in a cross-sectional comparison of patients with diabetes and healthy control subjects who underwent determinations of carotid intima-media thickness (23). Of further relevance to our findings, LpPLA2 mass (activity was not measured) was positively associated with carotid intima-media thickness in control subjects, but not among diabetic patients (23). Previous studies have documented a redistribution of LpPLA2 toward HDL in the setting of diabetes (19,24), and the observation that LpPLA2 mass was lower in diabetic than nondiabetic subjects for any given level of total/HDL cholesterol was deemed consistent with such redistribution as a potential explanation for the findings in that study (23). Redistribution of LpPLA2 to HDL is difficult to invoke as an explanation for our results, however, given the nonexistent correlation documented between LpPLA2 mass and HDL. The lack of correlation between LpPLA2 mass and lipid fractions in our cohort remains puzzling, and suggests the need for future studies to isolate lipoprotein subclasses and determine their respective LpPLA2 content in the context of dysglycemia.
An additional consideration is that determination of LpPLA2 activity is based on the rate of hydrolysis of PAF in vitro, yet several other plasma enzymes, such as lecithin-cholesterol acyltransferase, are capable of hydrolyzing PAF (25). Because such catalytic activity may be upregulated in the setting of heightened oxidative stress (26), a hallmark of insulin resistance and diabetes (6), it is possible that the disjunction between the associations of LpPLA2 mass and activity observed here could reflect contributions of enzymes beyond LpPLA2 itself.
Apart from these possibilities, we considered the potential influence of medications, which have been shown to affect LpPLA2 levels (27), but these had no measurable impact on our findings. Nor did the presence of kidney disease appear to account for our results. Finally, we entertained the possibility that redistribution to lipoprotein (a), a carrier of oxidized phospholipids for which LpPLA2 also has close affinity (28), could explain our findings. Given the low concentration of lipoprotein (a) in American Indians (15), its lack of correlation with LpPLA2 mass or activity, and the absence of a detectable influence on the associations observed, this does not appear likely.
The premise that the inverse association with CVD observed for LpPLA2 mass relates to the dysmetabolic phenotype of our population is partly supported by the negative, if modest, correlations observed for LpPLA2 mass with HbA1c and disease duration among diabetic participants. Although the inverse LpPLA2 mass–CVD relationship was attenuated in the subgroup without diabetes and insulin resistance, the RRs were still <1.0, which does not provide evidence of a strong gradient across categories of dysglycemic severity. Yet even the nondiabetic, noninsulin-resistant subgroup was characterized by considerable prevalences of impaired fasting glucose (43.1%), metabolic syndrome (16.8%), eGFR <60 mL/min/1.73 m2 (13.1%), and albuminuria (12.4%). These observations suggest that not only hyperglycemia per se but also insulin resistance and oxidative stress, or other as yet undefined factors, may be responsible for the findings in this cohort.
Limitations
Several limitations must be acknowledged. First, we did not have determinations of lipoprotein subclasses, or apolipoprotein levels themselves, which could have helped to elucidate the basis for the associations observed. Second, despite a focus on atherosclerotic/thrombotic events, we did include fatal CHF in the primary end point to avoid misclassification of deaths from unrecognized ischemic CHF. This was a minor constituent of the primary outcome, however, and relations with specific atherothrombotic components proved directionally consistent with the main results. Last, our findings derive from a population of American Indians with more pervasive and severe glycometabolic abnormalities than studied heretofore. These results at the upper end of the cardiometabolic risk spectrum are at variance with the preponderance of existing data for LpPLA2 mass and do not necessarily apply to other ethnic groups. Nevertheless, many prior reports from SHS (29–31) have yielded risk factor associations that have been subsequently confirmed in other populations at high cardiometabolic risk.
In this cohort of American Indians with highly prevalent glycometabolic disturbances, LpPLA2 mass and activity exhibited opposite relationships with incident CVD. LpPLA2 mass showed an inverse independent association and LpPLA2 activity a positive independent association with this outcome. The present findings in a cohort enriched with dysmetabolic phenotypes are of particular importance in light of the widening epidemics of obesity and diabetes affecting modern societies (32,33), and will require independent replication in similar populations. In the context of ongoing randomized trials assessing the potential clinical benefits of pharmacologic inhibition of LpPLA2, our findings support measurement of LpPLA2 activity, instead of mass, to guide identification of subjects with increased LpPLA2-associated risk in view of the greater consistency of its relationship with CVD across the spectrum of cardiometabolic risk.
Acknowledgments
This study was supported by grants U01-HL-41642, U01-HL-41652, U01-HL-41654, U01-HL-65521, UL1-RR-031975, and K23-HL-070854 (to J.R.K.) from the National Institutes of Health and by an unrestricted grant from diaDexus, Inc.
J.R.K. and J.G.U. received unrestricted funding from diaDexus, Inc., to support this project. At the time of this study and analysis, R.L.W. was executive vice president and chief scientific officer of diaDexus, Inc. No other potential conflicts of interest relevant to this article were reported.
J.R.K. participated in study conception and design, acquired data, performed statistical analysis, interpreted data, drafted the manuscript, and critically revised the manuscript for important intellectual content. J.G.U. and B.V.H. participated in study conception and design, acquired data, interpreted data, and critically revised the manuscript for important intellectual content. J.Z., R.B.D., and E.T.L. acquired data and critically revised the manuscript for important intellectual content. R.L.W. interpreted data and critically revised the manuscript for important intellectual content. J.R.K. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the SHS participants, staff, and coordinators.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1639/-/DC1.
The views expressed in this article are those of the authors and do not necessarily reflect those of the Indian Health Service.
References
- 1.Hansson GK. Inflammatory mechanisms in atherosclerosis. J Thromb Haemost 2009;7(Suppl. 1):328–331 [DOI] [PubMed] [Google Scholar]
- 2.Packard CJ. Lipoprotein-associated phospholipase A2 as a biomarker of coronary heart disease and a therapeutic target. Curr Opin Cardiol 2009;24:358–363 [DOI] [PubMed] [Google Scholar]
- 3.Mallat Z, Lambeau G, Tedgui A. Lipoprotein-associated and secreted phospholipases A2 in cardiovascular disease: roles as biological effectors and biomarkers. Circulation 2010;122:2183–2200 [DOI] [PubMed] [Google Scholar]
- 4.Zalewski A, Macphee C. Role of lipoprotein-associated phospholipase A2 in atherosclerosis: biology, epidemiology, and possible therapeutic target. Arterioscler Thromb Vasc Biol 2005;25:923–931 [DOI] [PubMed] [Google Scholar]
- 5.Thompson A, Gao P, Orfei L, et al. ; Lp-PLA(2) Studies Collaboration Lipoprotein-associated phospholipase A(2) and risk of coronary disease, stroke, and mortality: collaborative analysis of 32 prospective studies. Lancet 2010;375:1536–1544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meigs JB, Larson MG, Fox CS, Keaney JF, Jr, Vasan RS, Benjamin EJ. Association of oxidative stress, insulin resistance, and diabetes risk phenotypes: the Framingham Offspring Study. Diabetes Care 2007;30:2529–2535 [DOI] [PubMed] [Google Scholar]
- 7.Lee ET, Welty TK, Fabsitz R, et al. The Strong Heart Study. A study of cardiovascular disease in American Indians: design and methods. Am J Epidemiol 1990;132:1141–1155 [DOI] [PubMed] [Google Scholar]
- 8.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Executive summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 9.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419 [DOI] [PubMed] [Google Scholar]
- 10.Stern SE, Williams K, Ferrannini E, DeFronzo RA, Bogardus C, Stern MP. Identification of individuals with insulin resistance using routine clinical measurements. Diabetes 2005;54:333–339 [DOI] [PubMed] [Google Scholar]
- 11.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D; Modification of Diet in Renal Disease Study Group A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999;130:461–470 [DOI] [PubMed] [Google Scholar]
- 12.Best LG, Zhang Y, Lee ET, et al. C-reactive protein as a predictor of cardiovascular risk in a population with a high prevalence of diabetes: the Strong Heart Study. Circulation 2005;112:1289–1295 [DOI] [PubMed] [Google Scholar]
- 13.Palmieri V, Celentano A, Roman MJ, et al. ; Strong Heart Study Relation of fibrinogen to cardiovascular events is independent of preclinical cardiovascular disease: the Strong Heart Study. Am Heart J 2003;145:467–474 [DOI] [PubMed] [Google Scholar]
- 14.Lu WQ, Resnick HE, Jablonski KA, et al. Effects of glycaemic control on cardiovascular disease in diabetic American Indians: the Strong Heart Study. Diabet Med 2004;21:311–317 [DOI] [PubMed] [Google Scholar]
- 15.Wang W, Hu D, Lee ET, et al. Lipoprotein(a) in American Indians is low and not independently associated with cardiovascular disease. The Strong Heart Study. Ann Epidemiol 2002;12:107–114 [DOI] [PubMed] [Google Scholar]
- 16.Hatoum IJ, Hu FB, Nelson JJ, Rimm EB. Lipoprotein-associated phospholipase A2 activity and incident coronary heart disease among men and women with type 2 diabetes. Diabetes 2010;59:1239–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nelson TL, Kamineni A, Psaty B, et al. Lipoprotein-associated phospholipase A(2) and future risk of subclinical disease and cardiovascular events in individuals with type 2 diabetes: the Cardiovascular Health Study. Diabetologia 2011;54:329–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stafforini DM, Carter ME, Zimmerman GA, McIntyre TM, Prescott SM. Lipoproteins alter the catalytic behavior of the platelet-activating factor acetylhydrolase in human plasma. Proc Natl Acad Sci USA 1989;86:2393–2397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tellis CC, Tselepis AD. The role of lipoprotein-associated phospholipase A2 in atherosclerosis may depend on its lipoprotein carrier in plasma. Biochim Biophys Acta 2009;1791:327–338 [DOI] [PubMed] [Google Scholar]
- 20.Tsimihodimos V, Karabina SA, Tambaki AP, et al. Altered distribution of platelet-activating factor-acetylhydrolase activity between LDL and HDL as a function of the severity of hypercholesterolemia. J Lipid Res 2002;43:256–263 [PubMed] [Google Scholar]
- 21.Gazi I, Lourida ES, Filippatos T, Tsimihodimos V, Elisaf M, Tselepis AD. Lipoprotein-associated phospholipase A2 activity is a marker of small, dense LDL particles in human plasma. Clin Chem 2005;51:2264–2273 [DOI] [PubMed] [Google Scholar]
- 22.Krauss RM. Lipids and lipoproteins in patients with type 2 diabetes. Diabetes Care 2004;27:1496–1504 [DOI] [PubMed] [Google Scholar]
- 23.Constantinides A, van Pelt LJ, van Leeuwen JJ, et al. Carotid intima media thickness is associated with plasma lipoprotein-associated phospholipase A2 mass in nondiabetic subjects but not in patients with type 2 diabetes. Eur J Clin Invest 2011;41:820–827 [DOI] [PubMed] [Google Scholar]
- 24.Kujiraoka T, Iwasaki T, Ishihara M, et al. Altered distribution of plasma PAF-AH between HDLs and other lipoproteins in hyperlipidemia and diabetes mellitus. J Lipid Res 2003;44:2006–2014 [DOI] [PubMed] [Google Scholar]
- 25.Subramanian VS, Goyal J, Miwa M, et al. Role of lecithin-cholesterol acyltransferase in the metabolism of oxidized phospholipids in plasma: studies with platelet-activating factor-acetyl hydrolase-deficient plasma. Biochim Biophys Acta 1999;1439:95–109 [DOI] [PubMed] [Google Scholar]
- 26.Subbaiah PV, Liu M. Disparate effects of oxidation on plasma acyltransferase activities: inhibition of cholesterol esterification but stimulation of transesterification of oxidized phospholipids. Biochim Biophys Acta 1996;1301:115–126 [DOI] [PubMed] [Google Scholar]
- 27.Heart Protection Study Collaborative Group Lipoprotein-associated phospholipase A2 activity and mass in relation to vascular disease and nonvascular mortality. J Intern Med 2010;268:348–358 [DOI] [PubMed] [Google Scholar]
- 28.Tsimikas S, Tsironis LD, Tselepis AD. New insights into the role of lipoprotein(a)-associated lipoprotein-associated phospholipase A2 in atherosclerosis and cardiovascular disease. Arterioscler Thromb Vasc Biol 2007;27:2094–2099 [DOI] [PubMed] [Google Scholar]
- 29.Howard BV, Robbins DC, Sievers ML, et al. LDL cholesterol as a strong predictor of coronary heart disease in diabetic individuals with insulin resistance and low LDL: the Strong Heart Study. Arterioscler Thromb Vasc Biol 2000;20:830–835 [DOI] [PubMed] [Google Scholar]
- 30.Wang W, Lee ET, Fabsitz R, Welty TK, Howard BV. Using HbA(1c) to improve efficacy of the american diabetes association fasting plasma glucose criterion in screening for new type 2 diabetes in American Indians: the Strong Heart Study. Diabetes Care 2002;25:1365–1370 [DOI] [PubMed] [Google Scholar]
- 31.Lindsay RS, Resnick HE, Zhu J, et al. Adiponectin and coronary heart disease: the Strong Heart Study. Arterioscler Thromb Vasc Biol 2005;25:e15–e16 [DOI] [PubMed] [Google Scholar]
- 32.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 2006;295:1549–1555 [DOI] [PubMed] [Google Scholar]
- 33.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047–1053 [DOI] [PubMed] [Google Scholar]