Abstract
OBJECTIVE
IGF-I has an almost 50% amino acid sequence homology with insulin and elicits nearly the same hypoglycemic response. Studies showed that low and high IGF-I levels are related to impaired glucose tolerance and to a higher risk of type 2 diabetes. The aim of the current study was to evaluate the association between IGF-I level and insulin resistance in a Danish general population.
RESEARCH DESIGN AND METHODS
Included were 3,354 adults, aged 19–72 years, from the cross-sectional Health2006 study. The homeostasis model assessment of insulin resistance (HOMA-IR) was used as the index to estimate insulin resistance. Serum IGF-I levels were determined by an immunoassay and grouped into quintiles (Q1–Q5). Linear or multinomial logistic regression analyses were performed.
RESULTS
In the study population, 520 subjects (15.5%) had increased HOMA-IR values above 2.5. After adjustment for age, sex, physical activity, and waist-to-height ratio, a U-shaped association between IGF-I and HOMA-IR was found. Low IGF-I (Q1: odds ratio [OR] 1.65 [95% CI 1.16–2.34], P < 0.01) as well as high IGF-I (Q5: 1.96 [1.38–2.79], P < 0.01) levels were related to a higher odds of increased HOMA-IR values compared with subjects with intermediate (Q3) IGF-I levels. These associations remained statistically significant after the exclusion of subjects with type 2 diabetes and by using the updated computer HOMA2-IR model.
CONCLUSIONS
Low- and high-normal IGF-I levels are both related to insulin resistance. The biological mechanism of this complex phenomenon has to be elucidated in more detail for future risk stratification.
IGF-I, predominantly synthesized in the liver upon stimulation by growth hormone (GH), is usually bound to IGF-binding protein 3 (IGFBP-3) in circulation (1). IGF-I has an almost 50% amino acid sequence homology with insulin and elicits nearly the same hypoglycemic response (2). Several studies have investigated the effect of IGF-I on insulin sensitivity and its relation to type 2 diabetes. Large longitudinal studies, including the National Health and Nutrition Examination Survey (NHANES) III, reported a higher risk of insulin resistance, metabolic syndrome (MetS), and type 2 diabetes in subjects with low IGF-I serum concentrations or low IGF-I–to–IGFBP-3 ratios (3,4). A recent German study in 7,665 subjects, however, showed that low and high baseline IGF-I serum concentrations were both related to a higher risk of developing type 2 diabetes within 5 years (5). This U-shaped association seems to be likely in face of a higher prevalence of MetS or type 2 diabetes in patients with GH deficiency (6), a state of low IGF-I levels, as well as with acromegaly (7), a disease characterized by high IGF-I levels, although endogenous GH secretion may confound short-term glucose homeostasis in these patients. On the basis of these findings, we also hypothesize a U-shaped relation between IGF-I levels and insulin sensitivity as precursor to manifest type 2 diabetes.
In general, the effects of IGF-I in the control of glucose homeostasis is well known. Animal models showed that a deletion of hepatic IGF-I production, resulting in 80% reduced IGF-I levels, led to hyperinsulinemia and abnormal glucose clearance (8,9). An epidemiological study reported a negative correlation between IGF-I levels and insulin resistance measured by the homeostasis model assessment of insulin resistance (HOMA-IR) (10). Confirming results were found in an Italian study that investigated subjects with and without type 2 diabetes as well as with impaired glucose tolerance (11). IGF-I levels were positively correlated with insulin sensitivity among all three groups. Unfortunately, both studies did not account for a possible U-shaped association and were relatively small, with study populations of 404 and 506 subjects. Therefore, the aim of the current study was to evaluate the possible U-shaped association between IGF-I serum concentration and insulin resistance assessed by HOMA-IR in a large Danish population of 3,354 adults aged 19–72 years.
RESEARCH DESIGN AND METHODS
Study population
The Health2006, a population-based cross-sectional study, was initiated at the Research Centre for Prevention and Health (RCPH) in June 2006 and was terminated in May 2008 (12). Participants were recruited through the Danish Civil Registration office as a random sample of men and women aged between 19 and 72 years and living in 11 municipalities of the western part of the Capital Region of Denmark. Of 7,931 invited men and women, 3,471 participated, for a response rate of 43.8%. All participants gave written informed consent before taking part in the study, and the study was approved by the local ethics committee (KA20060011).
Of the 3,471 participants, 50 with missing data for IGF-I, glucose levels, or HOMA-IR were excluded, as were 67 with missing information for used confounders. The final study population comprised 3,354 subjects (1,847 women, 1,507 men).
Measurements
Participants underwent an extensive health examination when visiting the RCPH, including measurement of height, weight, and waist circumference. Waist-to-height ratio and BMI were calculated. Information on sociodemographic variables, physical activity, and functional limitations was measured by self-report questionnaire.
Participants were asked to categorize their usual physical activity level during leisure time as 1) mainly sedentary, 2) lightly active, 3) moderately active, or 4) vigorously active (13). Categories 3 and 4 were combined for the analyses because of few participants in category 4. Smoking status was categorized as never, former, and current smoker. The definition of type 2 diabetes was based on self-reported physician’s diagnosis or self-reported diabetic medication.
Fasting blood samples were drawn from the cubital vein with the subject supine. Plasma glucose concentration was determined by the hexokinase method (Hitachi 912, Roche Diagnostics, Mannheim, Germany). Plasma insulin was measured using an enzyme-linked immunosorbent assay (DAKO Diagnostic Ltd, Ely, Cambs, U.K.). Firstly, the HOMA1-IR was calculated as insulin (µU/mL) × glucose (mmol/L)/22.5 according to Matthews et al. (14), and results were categorized into two groups according to 2.5, as previously used cutoff indicating a high probability of insulin resistance (14), or to the 75th quartile (corresponding to 1.819) based on subjects without self-reported physician’s diagnosis or self-reported diabetic medication. Secondly, we alternatively used the updated computer HOMA2-IR model (http://www.dtu.ox.ac.uk/homacalculator/index.php) with nonlinear solution and categorized into two groups according to 1.4 (15) or to the 75th quartile (corresponding to 1.133) based on subjects without self-reported physician’s diagnosis or self-reported diabetic medication.
In 2009, IGF-I serum concentrations were determined in serum that had been stored at −80°C by an immunoassay (Immulite 2000 IGF-1, Siemens Medical Solutions Diagnostics, Los Angeles, CA) on automated Immulite 2000 (Siemens Medical Solutions Diagnostics). The assay has been extensively validated in our laboratory, and in our hands, intra- and interassay coefficients of variation were less than 4 and 9%, respectively (16).
Statistical analysis
Continuous data are expressed as median (25th; 75th quartile), and nominal data are expressed as percentage. For bivariate analyses, the Kruskal-Wallis test (continuous data) or χ2 test (nominal data) were used to compare women and men. In a first step, linear regression with restricted cubic splines (17) was used to detect a possible nonlinear dependency of HOMA values on IGF-I serum concentration. Three knots were prespecified, located at the 10th, 50th, and 90th percentile, as recommended by Stone and Koo (17), and HOMA values were log-transformed. On the basis of these results, IGF-I serum concentrations were categorized into five groups according to age-adjusted quintiles of distribution (Q1–Q5), and in a second step, ANOVA or logistic regression analyses adjusted for age, sex, physical activity, and waist-to-height ratio were used to assess the association between IGF-I serum concentration and HOMA1-IR or HOMA2-IR values. Adjusted means or odds ratios (ORs) with 95% CI were calculated. Sensitivity analyzes were performed after the exclusion of subjects with type 2 diabetes and separately for men and women with respect to increased HOMA-IR values. All statistical analyses were performed using SAS 9.1 software (SAS Institute Inc., Cary, NC).
RESULTS
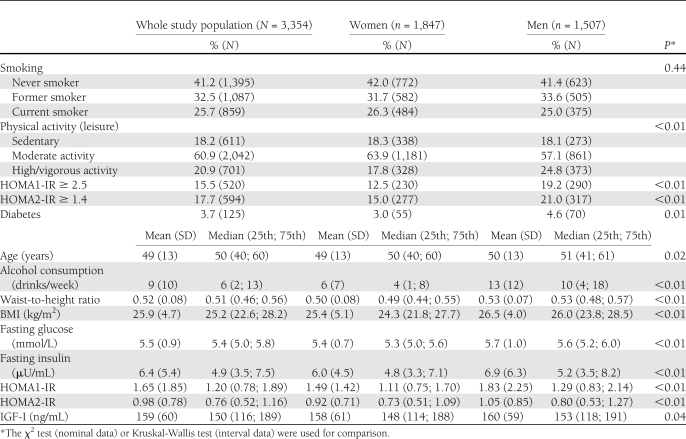
Men were older, consumed more alcohol, had a higher waist-to-height ratio, and were less often “moderately physically active” but were more often “highly physically active” than women (Table 1). Furthermore, men had higher values of HOMA1-IR and HOMA2-IR and were more often affected by type 2 diabetes. IGF-I serum concentrations were slightly but statistically significantly higher in men than in women. Regarding the age-dependency of the IGF-I serum concentrations and the HOMA1-IR values, we observed a strong decline in IGF-I with age (median 20–25 years: 250 ng/mL; 65–70 years: 121 ng/mL), whereas the HOMA1-IR did not change substantially with age (median 20–25 years: 1.26; 65–70 years: 1.28), even if the variance become larger (Supplementary Fig. 1).
Table 1.
General characteristics of the study population
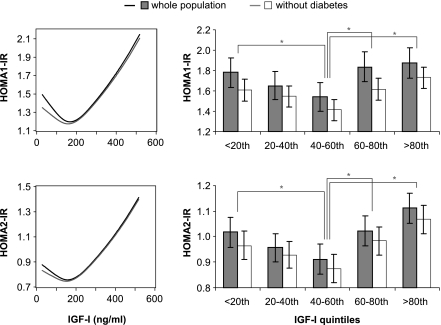
In a first step, crude linear regression with restricted cubic splines detected a U-shaped association between IGF-I serum concentrations and HOMA1-IR or HOMA2-IR, even after the exclusion of subjects with type 2 diabetes (Fig. 1, left). Multivariable ANOVA confirmed these associations and revealed also U-shaped associations between IGF-I quintiles and both HOMA-IR estimates (Fig. 1, right). The estimated mean HOMA1-IR or HOMA2-IR values were up to 0.33 or 0.20 units higher in the 1st and 5th IGF-I quintile compared with the middle IGF-I quintile. The exclusion of 126 subjects with type 2 diabetes led to lower mean levels of HOMA1-IR and HOMA2-IR; however, the U-shaped association did not substantially change (Fig. 1).
Figure 1.
Association between IGF-I serum concentration and level of HOMA1-IR (upper) and updated computer HOMA2-IR (lower) for the whole study population and after exclusion of subjects with diabetes. Left side: Crude linear regression with restricted cubic splines. Right side: Estimated mean level of HOMA-IR with 95% CI by levels of IGF-I. ANOVA was adjusted for age, sex, physical activity, and waist-to-height ratio. Tests for differences between the middle IGF-I quintile (40–60th) and the remaining groups were performed.*P < 0.05. P values were adjusted for multiple comparison.
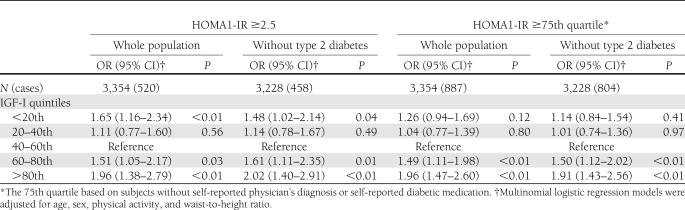
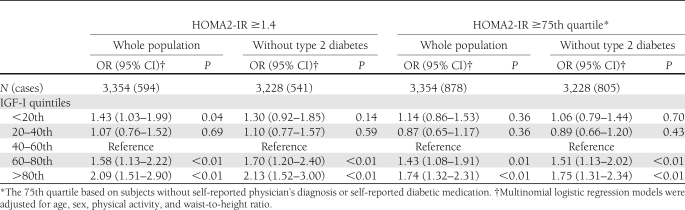
Logistic regression analyses revealed that subjects within the lowest or highest IGF-I quintiles had an up to twofold higher odds of having a HOMA1-IR >2.5 or HOMA2-IR >1.4 compared with subjects in the middle IGF-I quintile (Tables 2 and 3). With respect to HOMA1-IR, the exclusion of individuals with type 2 diabetes did not substantially change the results, with the lowest and highest IGF-I quintiles both related to a higher odds of HOMA1-IR >2.5 (Table 2). With respect to HOMA2-IR, however, only high IGF-I serum concentrations were still related to a higher odds of HOMA1-IR >1.4 (Table 3).
Table 2.
Association between levels of IGF-I and HOMA1-IR
Table 3.
Association between levels of IGF-I and HOMA2-IR
By using the 75th quartile as a cutoff to define high HOMA1-IR or HOMA2-IR values, only high but not low IGF-I levels were related to a higher odds of having high HOMA-IR in the whole population as well as in subjects without type 2 diabetes. A possible explanation might be that the 75th quartile (HOMA1-IR: 1.819; HOMA2-IR: 1.133) is less sensitive than the cutoffs of 2.5 or 1.4. Therefore, the specificity of the cutoffs might be less to detect an association to low IGF-I serum concentrations.
Sensitivity analyses were performed with triglycerides and BMI instead of waist-to-height ratio as confounders to investigate the potential effect of anthropometry or lipid metabolism on the association of IGF-I serum concentration and insulin resistance. These analyses confirmed the main results: no substantial changes in estimates of increased HOMA-IR were found.
Furthermore, linear and logistic regression analyses were repeated separately for men and women. Linear regression with restricted cubic splines still showed a U-shaped association for both sexes (data not shown). Logistic regression analyses revealed differences between men and women for low IGF-I (Supplementary Tables 1 and 2). In women, low and high IGF-I serum concentrations were still related to higher odds of increased HOMA1-IR or HOMA2-IR values. In contrast to the main results, a positive relation between low IGF-I and odds of HOMA2-IR >75th quartile was also found in the entire female population. In contrast to women, only men with high IGF-I serum concentrations had higher odds of increased HOMA-IR for all investigated cutoffs. No associations were found for low IGF-I serum concentrations.
CONCLUSIONS
In the present population-based study of 3,354 Danish subjects, we detected a U-shaped association between IGF-I serum concentrations and insulin resistance. Low and high IGF-I serum concentrations within the normal range were both related to higher odds of being insulin resistant in the whole population without GH-related disorders. A closer view on possible sex-specific difference showed that the relation with low IGF-I serum concentrations was pronounced in women but not in men. These findings implicate sex differences in the association between IGF-I serum concentration and insulin resistance.
In general, few studies have addressed possible sex differences in relation to the GH/IGF system. Yet a sexual dimorphism with respect to GH secretion is widely accepted, with women who are fertile having higher serum GH levels than men (18). GH secretion seems to exerted by the differential effects of androgens and estrogens at the hypothalamic level (19). Moreover, sex-specific effects of GH replacement therapy have been reported and support the sex-related differences (20).
Previous studies have reported controversial results with respect to sex differences and glucose homeostasis (21). In some studies, men had reduced or increased insulin sensitivity than women; whereas, other researchers found comparable insulin sensitivity between the sexes (21). However, data indicate that men exhibit lower postprandial glucose concentrations but are more often affected by impaired fasting glucose. Possible explanations include differences in fat distribution, physical activity, or the use of oral contraceptives. Abdominal obesity is one of the major risk factors of insulin sensitivity, and it is well documented that men more often suffer from visceral fat accumulation. Further, men with higher physical activity were even more often affected by impaired fasting glucose (22). However, the reasons for the sex-specific divergence on insulin secretion, insulin action, and glucose effectiveness are unclear and remain to be investigated.
In concordance with our main results, a recent longitudinal study found a U-shaped association between IGF-I and the 5-year risk of type 2 diabetes (5). Furthermore, our findings regarding low but not high IGF-I serum concentrations were confirmed by previous observational investigations (3,4). A cross-sectional analysis of the NHANES showed twofold higher odds of insulin resistance in subjects with the lowest IGF-I–to–IGFBP-3 ratio (4). A further study found a 50% reduced risk of impaired glucose tolerance (IGT) or type 2 diabetes during a 4.5-year follow-up period in individuals with IGF-I levels above the study-specific median (3). The latter study found no evidence for a nonlinear association between IGF-I and IGT or type 2 diabetes. Nonetheless, the interpretation of these findings is somewhat limited by the small number of incident cases (IGT, n = 44; type 2 diabetes, n = 7). A further reason for the lack of a relation between high IGF-I serum concentrations and the investigated end point might be that both studies (3,4) used age-independent IGF-I categorization and therefore included mainly older subjects with a higher predetermined risk of type 2 diabetes or IGT in the group with low IGF-I serum concentrations.
IGF-I has structural homology with insulin, and several studies supported a positive influence of IGF-I on glucose homeostasis, which strengthened the relation between decreased IGF-I and insulin resistance. IGF-I leads to an increase in peripheral glucose uptake and a decreased production of hepatic glucose causing better insulin sensitivity (2,23). Furthermore, low IGF-I serum concentrations were related to a higher anthropometric status, which in turn is related to insulin resistance. On the other side, adult patients with GH replacement therapy revealed a higher prevalence of insulin resistance and MetS (24,25). However, whether this is an IGF-I effect or rather a free fatty acid–mediated GH effect is questionable. Therefore, some have argued that GH replacement therapy might be associated with the development of MetS or an acceleration of the manifestation of type 2 diabetes in patients at risk (26,27,24).
In contrast, one of the suggested benefits of GH replacement on body composition includes a decrease in abdominal fat mass (28), which should theoretically reduce insulin resistance, the features of MetS, and incident type 2 diabetes. The available data of observational studies regarding this issue showed no clear picture, and controlled end point studies are scarce. A further issue arises because GH is indeed the major stimulus for IGF-I production in the liver, but both hormones can have opposing metabolic effects. As mentioned, IGF-I increases peripheral glucose uptake, whereas GH shows diabetic actions and increases glucose production (23).
Further differences are apparent for free fatty acid homeostasis. Although IGF-I may reduce serum free fatty acid levels, GH promotes lipolysis and ketogenesis (29,23). The effect of IGF-I in reducing serum free fatty acid levels may be important in improving insulin sensitivity related to the “lipotoxic” effects of free fatty acids (30–32). In our study population, sensitivity analyses revealed no effect of triglycerides on the association between IGF-I serum concentration and HOMA-IR. Altogether, the separation of the IGF-I-related and GH-related effects on metabolism is not always possible, and therefore, the complete role of the IGF-I/GH axis in glucose homeostasis is not yet clarified (33). A limitation of the current study is the cross-sectional study design that did not allow us to draw firm conclusions on the chronologic sequence of changes in the GH/IGF axis and alterations in the control of glucose homeostasis.
Insulin resistance is highly correlated to obesity and high insulin levels as insulin stimulates hepatic IGF-I synthesis (34) and increases the fraction of circulating free IGF-I by downregulating hepatic synthesis of IGFBP-1 and, to a lesser extent, hepatic secretion of IGFBP-2 (35,36). Indeed, several studies report that free IGF-I is elevated in obesity (35,37–39), while the total IGF-I concentrations remain within the reference range (39) or are even low-normal, with a normalization upon weight loss (40). A reasonable hypothesis may be that high free IGF-I levels in obese patients may inhibit endogenous GH secretion by negative feedback.
Major strengths of the current study are the large scale of the cohort and the population-based design. Limitations arise from the cross-sectional study design. Furthermore, we have no IGFBP-3 measurements that would add information by investigating the estimated amount of free IGF-I in relation to HOMA-IR values.
In conclusion, in the current study we detected a U-shaped association between IGF-I serum concentrations and increased HOMA values; therefore, deviations of IGF-I regulation in both directions are related to insulin resistance. The biologic mechanism of this complex phenomenon has to be elucidated in more detail for future risk stratification.
Acknowledgments
The project is financially supported by grants from the Velux Foundation; the Danish Medical Research Council, Danish Agency for Science, Technology and Innovation; the Aase and Ejnar Danielsens Foundation; ALK-Abelló A/S, Hørsholm, Denmark; and Research Centre for Prevention and Health, the Capital Region of Denmark. No other potential conflicts of interest relevant to this article were reported.
N.F., H.W., and A.L. contributed to the study design and concept for the data analysis. A.L. and A.J. organized the sample collection and data preparation. N.F. performed statistical analyses, drafted the manuscript, and wrote the final version together with all other coauthors. N.F., B.T., T.J., A.J., C.S., H.W., and A.L. contributed to the interpretation of the results and the discussion. All authors read and approved the final manuscript. N.F. had full access to all data in the study and takes responsibility for the integrity of data and the accuracy of data analysis.
The authors thank the staff at Research Centre for Prevention and Health for carefully performed data collection.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-1833/-/DC1.
References
- 1.Jones JI, Clemmons DR. Insulin-like growth factors and their binding proteins: biological actions. Endocr Rev 1995;16:3–34 [DOI] [PubMed] [Google Scholar]
- 2.Boulware SD, Tamborlane WV, Rennert NJ, Gesundheit N, Sherwin RS. Comparison of the metabolic effects of recombinant human insulin-like growth factor-I and insulin. Dose-response relationships in healthy young and middle-aged adults. J Clin Invest 1994;93:1131–1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sandhu MS, Heald AH, Gibson JM, Cruickshank JK, Dunger DB, Wareham NJ. Circulating concentrations of insulin-like growth factor-I and development of glucose intolerance: a prospective observational study. Lancet 2002;359:1740–1745 [DOI] [PubMed] [Google Scholar]
- 4.Sierra-Johnson J, Romero-Corral A, Somers VK, et al. IGF-I/IGFBP-3 ratio: a mechanistic insight into the metabolic syndrome. Clin Sci (Lond) 2009;116:507–512 [DOI] [PubMed] [Google Scholar]
- 5.Schneider HJ, Friedrich N, Klotsche J, et al. Prediction of incident diabetes mellitus by baseline IGF1 levels. Eur J Endocrinol 2011;164:223–229 [DOI] [PubMed] [Google Scholar]
- 6.van der Klaauw AA, Biermasz NR, Feskens EJ, et al. The prevalence of the metabolic syndrome is increased in patients with GH deficiency, irrespective of long-term substitution with recombinant human GH. Eur J Endocrinol 2007;156:455–462 [DOI] [PubMed] [Google Scholar]
- 7.Melmed S. Medical progress: acromegaly. N Engl J Med 2006;355:2558–2573 [DOI] [PubMed] [Google Scholar]
- 8.Sjögren K, Wallenius K, Liu JL, et al. Liver-derived IGF-I is of importance for normal carbohydrate and lipid metabolism. Diabetes 2001;50:1539–1545 [DOI] [PubMed] [Google Scholar]
- 9.Yakar S, Liu JL, Fernandez AM, et al. Liver-specific igf-1 gene deletion leads to muscle insulin insensitivity. Diabetes 2001;50:1110–1118 [DOI] [PubMed] [Google Scholar]
- 10.Colao A, Di Somma C, Cascella T, et al. Relationships between serum IGF1 levels, blood pressure, and glucose tolerance: an observational, exploratory study in 404 subjects. Eur J Endocrinol 2008;159:389–397 [DOI] [PubMed] [Google Scholar]
- 11.Sesti G, Sciacqua A, Cardellini M, et al. Plasma concentration of IGF-I is independently associated with insulin sensitivity in subjects with different degrees of glucose tolerance. Diabetes Care 2005;28:120–125 [DOI] [PubMed] [Google Scholar]
- 12.Thyssen JP, Linneberg A, Menné T, Nielsen NH, Johansen JD. The prevalence and morbidity of sensitization to fragrance mix I in the general population. Br J Dermatol 2009;161:95–101 [DOI] [PubMed] [Google Scholar]
- 13.Saltin B, Grimby G. Physiological analysis of middle-aged and old former athletes. Comparison with still active athletes of the same ages. Circulation 1968;38:1104–1115 [DOI] [PubMed] [Google Scholar]
- 14.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–419 [DOI] [PubMed] [Google Scholar]
- 15.Geloneze B, Vasques AC, Stabe CF, et al. ; BRAMS Investigators HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS). Arq Bras Endocrinol Metabol 2009;53:281–287 [DOI] [PubMed] [Google Scholar]
- 16.Sørensen K, Aksglaede L, Petersen JH, Leffers H, Juul A. The exon 3 deleted growth hormone receptor gene is associated with small birth size and early pubertal onset in healthy boys. J Clin Endocrinol Metab 2010;95:2819–2826 [DOI] [PubMed] [Google Scholar]
- 17.Stone C, Koo CY. Additive splines in statistics. In Proceedings of the Statistical Computing Section ASA Washington, DC, American Statistical Association, 1985 [Google Scholar]
- 18.Gatford KL, Egan AR, Clarke IJ, Owens PC. Sexual dimorphism of the somatotrophic axis. J Endocrinol 1998;157:373–389 [DOI] [PubMed] [Google Scholar]
- 19.Ohlsson C, Mohan S, Sjögren K, et al. The role of liver-derived insulin-like growth factor-I. Endocr Rev 2009;30:494–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Span JP, Pieters GF, Sweep FG, Hermus AR, Smals AG. Gender differences in rhGH-induced changes in body composition in GH-deficient adults. J Clin Endocrinol Metab 2001;86:4161–4165 [DOI] [PubMed] [Google Scholar]
- 21.Blaak E. Sex differences in the control of glucose homeostasis. Curr Opin Clin Nutr Metab Care 2008;11:500–504 [DOI] [PubMed] [Google Scholar]
- 22.Halldin M, Rosell M, de Faire U, Hellénius ML. The metabolic syndrome: prevalence and association to leisure-time and work-related physical activity in 60-year-old men and women. Nutr Metab Cardiovasc Dis 2007;17:349–357 [DOI] [PubMed] [Google Scholar]
- 23.Møller N, Jørgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr Rev 2009;30:152–177 [DOI] [PubMed] [Google Scholar]
- 24.Jeffcoate W. Growth hormone therapy and its relationship to insulin resistance, glucose intolerance and diabetes mellitus: a review of recent evidence. Drug Saf 2002;25:199–212 [DOI] [PubMed] [Google Scholar]
- 25.Attanasio AF, Mo D, Erfurth EM, et al. ; International Hypopituitary Control Complications Study Advisory Board Prevalence of metabolic syndrome in adult hypopituitary growth hormone (GH)-deficient patients before and after GH replacement. J Clin Endocrinol Metab 2010;95:74–81 [DOI] [PubMed] [Google Scholar]
- 26.Hew FL, Koschmann M, Christopher M, et al. Insulin resistance in growth hormone-deficient adults: defects in glucose utilization and glycogen synthase activity. J Clin Endocrinol Metab 1996;81:555–564 [DOI] [PubMed] [Google Scholar]
- 27.Johannsson G, Bengtsson BA. Growth hormone and the metabolic syndrome. J Endocrinol Invest 1999;22(Suppl.):41–46 [PubMed] [Google Scholar]
- 28.Monson JP, Bengtsson BA, Abs R, Feldt-Rasmussen U, Wüster C. Can growth hormone therapy cause diabetes? KIMS Strategic Committee. Lancet 2000;355:1728–1729 [DOI] [PubMed] [Google Scholar]
- 29.Moller N, Gjedsted J, Gormsen L, Fuglsang J, Djurhuus C. Effects of growth hormone on lipid metabolism in humans. Growth Horm IGF Res 2003;13(Suppl. A):S18–S21 [DOI] [PubMed]
- 30.Cousin SP, Hügl SR, Wrede CE, Kajio H, Myers MG, Jr, Rhodes CJ. Free fatty acid-induced inhibition of glucose and insulin-like growth factor I-induced deoxyribonucleic acid synthesis in the pancreatic beta-cell line INS-1. Endocrinology 2001;142:229–240 [DOI] [PubMed] [Google Scholar]
- 31.Poitout V, Robertson RP. Minireview: Secondary beta-cell failure in type 2 diabetes—a convergence of glucotoxicity and lipotoxicity. Endocrinology 2002;143:339–342 [DOI] [PubMed] [Google Scholar]
- 32.Wilding JP. The importance of free fatty acids in the development of Type 2 diabetes. Diabet Med 2007;24:934–945 [DOI] [PubMed] [Google Scholar]
- 33.Clemmons DR. Involvement of insulin-like growth factor-I in the control of glucose homeostasis. Curr Opin Pharmacol 2006;6:620–625 [DOI] [PubMed] [Google Scholar]
- 34.Böni-Schnetzler M, Schmid C, Meier PJ, Froesch ER. Insulin regulates insulin-like growth factor I mRNA in rat hepatocytes. Am J Physiol 1991;260:E846–E851 [DOI] [PubMed] [Google Scholar]
- 35.Conover CA, Lee PD, Kanaley JA, Clarkson JT, Jensen MD. Insulin regulation of insulin-like growth factor binding protein-1 in obese and nonobese humans. J Clin Endocrinol Metab 1992;74:1355–1360 [DOI] [PubMed] [Google Scholar]
- 36.Brismar K, Fernqvist-Forbes E, Wahren J, Hall K. Effect of insulin on the hepatic production of insulin-like growth factor-binding protein-1 (IGFBP-1), IGFBP-3, and IGF-I in insulin-dependent diabetes. J Clin Endocrinol Metab 1994;79:872–878 [DOI] [PubMed] [Google Scholar]
- 37.Rasmussen MH, Frystyk J, Andersen T, Breum L, Christiansen JS, Hilsted J. The impact of obesity, fat distribution, and energy restriction on insulin-like growth factor-1 (IGF-1), IGF-binding protein-3, insulin, and growth hormone. Metabolism 1994;43:315–319 [DOI] [PubMed] [Google Scholar]
- 38.Frystyk J, Vestbo E, Skjaerbaek C, Mogensen CE, Orskov H. Free insulin-like growth factors in human obesity. Metabolism 1995;44(Suppl. 4):37–44 [DOI] [PubMed] [Google Scholar]
- 39.Nam SY, Lee EJ, Kim KR, et al. Effect of obesity on total and free insulin-like growth factor (IGF)-1, and their relationship to IGF-binding protein (BP)-1, IGFBP-2, IGFBP-3, insulin, and growth hormone. Int J Obes Relat Metab Disord 1997;21:355–359 [DOI] [PubMed] [Google Scholar]
- 40.Rasmussen MH, Hvidberg A, Juul A, et al. Massive weight loss restores 24-hour growth hormone release profiles and serum insulin-like growth factor-I levels in obese subjects. J Clin Endocrinol Metab 1995;80:1407–1415 [DOI] [PubMed] [Google Scholar]