If only Mary Poppins was right and all it took was a ‘spoonful of sugar’ to help the medicine go down. But, as most clinicians know, when it comes to persuading patients to take their medicines, do a little more exercise, eat healthily or simply turn up for scheduled appointments, it often takes more than just a spoonful of sugar to sweeten the deal.
This latter problem – patients who do not attend their appointments (DNAs) and who fail to cancel with enough time to offer it to another – is an especially vexing one and a major drain on NHS resources. Up to 6 million appointments are missed each year with direct costs estimated to be in the region of £700 million.1,2
One survey of 683 GPs found that 84% considered DNAs a major problem leading to lengthened waiting times, difficulty in reaching performance targets and greater costs.3 Other studies have cited reduced patient satisfaction, public health issues and increases in inappropriate Accident & Emergency presentations as consequences.4
So why do patients DNA? There are doubtless many reasons. Perhaps they felt better or experienced anxiety about potential bad news. Maybe there were issues with transportation or they experienced difficulty getting through to cancel. Perhaps they couldn't get time off work. A simple fact however, backed up by surveys of patients themselves, is that whilst they do often feel better, experience anxiety or encounter problems with processes and systems, the most common reason why patients DNA is that they simply forget.5
Given this ‘epidemic of forgetfulness’ it shouldn't surprise anyone to learn that many attempts to reduce, or at least manage the impact of DNAs, have been made. Some centres may overbook their clinics in anticipation of experiencing high DNA rates. But approaches like these can have knock-on effects that ultimately disadvantage patients, and however frustrating and unnecessary a waste of clinician time DNAs can be, overbooking does not deal with the problem itself.6 One cannot assume that a DNA is a medical condition resolved. It is the authors' experience (and most likely readers' too) that patients still present, but at less convenient times, in less appropriate care settings, with the additional health and financial implications that frequently accompany a worsened condition.
Perhaps a simpler solution would be to introduce a modest charge for appointments or fines for non-attendance. Given that over half of all appointments are accounted for by patients with long-term conditions such as diabetes and arthritis, this seems unfair – effectively penalizing people for falling ill.7 Fines present difficulties in terms of administration and enforcement.8 They can also backfire. Studies in children's day care centres found that penalizing late or non-attenders actually increased lateness and non-attendance.9
There is some evidence to support the use of reminder systems. Koshy et al. showed SMS reminders to have a modest effect in reducing DNAs at ophthalmology outpatients departments.10 A gastroenterology clinic found a telephone call to patients one week prior to their appointment reduced DNA rates from 23.3% to 5.7%.11 Whilst both approaches have been shown to have an effect in hospital settings, the challenge in primary care can be rather different. Most patients require appointments within a 24–48 hour period and so it may not be practical to put reminder systems in place. Consequently it is the authors' observation that one of the more common approaches is to publish the regrettable number of patients who don't attend presumably in an attempt to highlight the problem, shame non-attenders and appeal to patients' sense of responsibility (See Figure 1 for an example). Some centres might even threaten persistent non-attenders with removal from their lists, but we found it difficult to confirm the extent to which this actually occurs.
Figure 1.
Example of a typical communication highlighting the problem of DNAs
As is sometimes the case when dealing with commonly occurring challenges it can be helpful to look beyond our immediate environment and examine how those outside medicine deal with similar issues. The hospitality industry, for example, has long dealt with the problem of ‘no shows’. Customers call a restaurant to reserve a table and some fail to show. Like the NHS the cost can be considerable. Renowned social psychologist Robert Cialdini cites the example of restaurateur Gorden Sinclair who added two words that his receptionists used when taking customer bookings over the telephone.12 Instead of the usual ‘Please call us if you need to change or cancel your booking’ before hanging up, Sinclair asked staff to instead say ‘Will you please call us if you need to change or cancel your booking?’ and then pause, prompting the customer to make a verbal commitment by answering ‘Yes’.
Such a small change seems unlikely to yield big results, but this verbal commitment led to a notable drop in no-shows for a reason well known to behavioural scientists. People generally prefer to live up to their commitments, especially those that are voluntary and require active involvement. 13
But can behaviourally informed interventions like this be applied as effectively in busy healthcare centres to reduce DNAs?
Over a 4 month period (February – May 2011), we sought an answer to this question by testing three interventions informed from the behavioural sciences (specifically social influence theory) in two health centres in NHS Bedfordshire. The Wheatfield Surgery, Luton is a 7-partner practice providing, on average, 7000 GP and nurse led appointments each month. Toddington Medical Centre is a 4-partner practice averaging 3200 appointments. Like many centres, both experienced frustrating levels of DNAs. In the previous 12-month period, DNAs totalled 4700.
Applying these social influence approaches in two centres allowed us to test the impact of two separate interventions in one and simultaneously test the cumulative effect of the same two interventions plus a third at the Toddington Medical Centre. Prior to testing we held training sessions with reception staff supported by the partners and the practice manager. The training focussed on the rationale for the interventions and the practicalities of applying them. Training was held two weeks prior to starting the interventions allowing staff a period of time to reflect, ask questions and raise any concerns. There were none.
Active commitments
The majority of appointments are booked by telephone. Once a patient is provided with an appointment, the receptionist hangs-up the phone and proceeds to the next patient waiting on the line. Given the largely passive role of patients in these interactions, we believed that increasing patient participation would reduce DNAs or at least increase the chances that those subsequently unable to attend would call and cancel.
For a period of one month, patients were provided with a 4-digit reference number that identified their appointment and which they were asked to write down. Specifically receptionists were instructed to say
“Your appointment with Dr. Smith is on Tuesday at 10.35am. Would you please write down the following appointment identification number – (e.g. 1234).”
We believed this intervention would be effective for two reasons. The unexpectedness of the reference number system should increase appointment salience (novelty) in the eyes of the patient, leading to greater recall. We further predicted that asking patients to write down the number actively involved them in the interaction, which would impact on DNAs. And it did. Comparing DNA rates to the same month in previous years and against an annual average we actually measured a rise in DNAs.
This result was frustrating given that the overwhelming evidence from behavioural science suggested that we should expect a reduction. We quickly convened a meeting with the practice staff to investigate and, over a cup of tea and a packet of custard cream biscuits, we listened to their feedback.
Some raised the issue of patients not having pen and paper to hand when they called. Others claimed that explaining the system to patients led to unnecessarily long calls. However these issues rarely were a significant factor – a fact backed up by reports from the practice manager. The reason the intervention failed was straightforward – staff were not complying with it.
In an attempt to address this non-compliance, in addition to our gift of custard creams, we offered practice staff an alternative intervention. Would they instead be willing to ask patients to verbally repeat back the time and date of their appointment before ending the call? They readily agreed to this concession and implemented it immediately with high levels of compliance. The impact was almost as immediate too. The following month DNAs were 3.5% lower.
Written commitments
In common with other health centres, Wheatfield and Toddington hold regular Nurse clinics. These clinics offered two attractive features for testing a second intervention. Firstly the nurses themselves were responsible for appointment making. Secondly, a high proportion of nurse consultations were attended by patients who would likely make return visits. Blood tests for patients with type II diabetes, immunization boosters and replacement dressings were typical examples.
A common finding from previous persuasion research shows that a commitment to action can be strengthened to the extent that the individual making that commitment writes it down.14 Accordingly, when making follow-up appointments we asked nurses to ensure that patients wrote down the time and date on the appointment card themselves rather than the more common practice of the nurse doing so. This costless intervention led to a reduction in subsequent DNAs of 18% compared to the previous 6 months average (P < 0.05%).
Communicating the right norms
As discussed, in an attempt to reduce DNAs primary and secondary care centres will often publicize the number of patients who DNA via posters on waiting room walls or TV monitors. Whilst understandable, we believed there are reasons why such an approach might increase rather than decrease DNAs. For example, research has shown that drawing attention to the regrettable frequency of unwanted behaviours can have the effect of normalizing those behaviours resulting in an increase in their incidence.15 We further posit that given that these messages will only be viewed by patients who actually attend, they could serve as a rather effective advertisement to the merits of non-attendance.
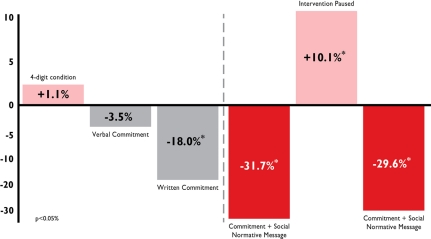
We replaced signs that communicated the number of patients who DNA'd in previous months, with signs that conveyed the much larger number of patients who did turn up. This, in combination with the verbal and written commitment-led interventions described, resulted in a 31.7% reduction in DNAs compared to the past 12 months' average. In an attempt to show that these reductions were a direct result of the interventions and not influenced by other factors, we ceased interventions for one month which led to a rise in DNAs. Activating the same set of interventions the following month, we duly measured a reduction of 29.6% (all P < 0.05%) (Figure 2).
Figure 2.
Reduction in DNAs following interventions
Conclusion
Our studies provide for three simple changes, informed from the behavioural sciences that can be immediately and costlessly implemented to reduce DNAs. To our best knowledge this is the first time these social influence interventions have been formally tested in NHS centres.
In light of the substantial changes currently taking effect in the NHS, it would be remiss not to view these results in a wider context beyond the obvious frustration and waste which DNAs cause. Regardless of the vast array of evidence based policies, protocols and treatments at our disposal to deliver world-class care free at the point of need, success will often be incumbent on patients taking responsibility and playing their part.
When it comes to persuading patients to take their medicines, do more exercise, eat healthily or simply turn up for scheduled appointments, we believe that insights from the behavioural sciences can and will play an increasingly important role in providing the architecture for influencing such change.
DECLARATIONS
Competing interests
Steve Martin is an author, business columnist and Director of INFLUENCE AT WORK a consultancy that advises on influence and behaviour change. He is a member of the Dept. of Health Behaviour Change Responsibility Network and works on patient engagement strategies for several Clinical Commissioning Groups.
Suraj Bassi is an Orthopaedic Surgeon and a Senior Manager in the healthcare advisory practice at professional services firm BDO LLP.
Rupert Dunbar-Rees is a General Practitioner and a Director at BDO LLP leading on clinical commissioning.
Funding and sponsorship
INFLUENCE AT WORK, BDO LLP and NHS Bedfordshire contributed equally towards the funding and sponsorship of this paper.
Guarantor
Dr. Suraj Bassi MRCS FRSA led the day to day management of these studies, has access to the data and accepts responsibility for this work.
Ethical approval
Not applicable
Contributorship
Steve Martin led the study and intervention design, conducted literature reviews and authored this essay; Dr. Suraj Bassi was the study manager, collected and analysed data, conducted literature reviews and contributed to the original and revised versions of this essay; Dr. Rupert Dunbar-Rees acted as GP advisor, reviewed the data and contributed to the original and revised versions of this essay.
Acknowledgements
The data was independently audited and verified by Edmund Tiddeman at NHS Bedfordshire.
We also recognize the help of the partners and staff at Wheatfield Medical Centre, Luton and Toddington Medical Centre, Bedfordshire specifically Debbie Wilkins, Nadia Shaw, Helen Smart and Tony Medwell.
References
- 1.No shows cost the NHS millions. See http://news.bbc.co.uk/1/hi/health/8195255.stm (last accessed date 20 November 2011)
- 2.See http://www.drfosterhealth.co.uk/features/outpatient-appointment-no-shows.aspx#references (last accessed date 20 November 2011)
- 3.2003. DPP 2005. Anon. DPP: Developing Patient Partnerships.
- 4.Karter AJ, Parker MM, Moffet HH, Ahmed AT Missed appointments and poor glycemic control: an opportunity to identify high-risk diabetic patients. Med Care 2004;42: 110–5 [DOI] [PubMed] [Google Scholar]
- 5.Neal RD, Hussain-Gambles M, Allgar V, Lawlor A, Dempsey O Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Family Practice 2005;6:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lacy NL, Paulman A, Reuter M, Lovejoy M Why We Don't Come: Patient Perceptions on No-Shows. Annals of Family Medicine 2 2004;5:541–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones V, Barham L Healthy Work: Challenges and Opportunities to 2030 London: BUPA, 2009 [Google Scholar]
- 8.Fysh T Missed outpatient appointments. J R Soc Med 2002;95:376–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gneezy U, Rustichini A A fine is a price. Journal of Legal Studies 1999;29:1;1–18 [Google Scholar]
- 10.Koshy E, Car J, Majeed A Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments. BMC Ophthalmology 2008;8:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott M, Allen S, Bamford A, Walshe M, Ingham Clark C Influence of a nurse practitioner on non-attendance rate for barium enema. J R Soc Med 2002;95:448–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cialdini RB Influence: Science and Practice (5th ed). Boston: Allyn & Bacon, 2009 [Google Scholar]
- 13.Goldstein NJ, Martin SJ, Cialdini RB Yes 50 Secrets from the Science of Persuasion. London: Profile Books, 2007 [Google Scholar]
- 14.Cioffi D, Garner R On doing the decision: effects of active versus passive commitment and self-perception. Personality and Social Psychology Bulletin 1996;22:133–44 [Google Scholar]
- 15.Schultz PW, Nolan J, Cialdini RB, Goldstein NJ, Griskevicius V The constructive, destructive, and reconstructive power of social norms. Psychological Science, 2007:18:429–34 [DOI] [PubMed] [Google Scholar]