Abstract
Background:
Tuberculosis (TB) of hip constitutes nearly 15% of all cases of osteoarticular tuberculosis. We report a retrospective study carried out on 43 children with hip TB.
Materials and Methods:
Forty-three children of TB hip treated between 1971 and 2000 were analysed. Twenty-four children of the early series were treated with streptomycin (S), isoniazid (H) and PAS (Pa) for 18 months (3HPaS, 15 HPa), while 19 children in the later series were treated with isoniazid (H), rifampicin (R) and ethambutol (E) or pyrazinamide (Z) for 12 months [(12 RHE(Z)]. Five out of 18 children with radiologically normal appearing type hip TB were treated with chemotherapy alone and 38 children were subjected to surgery; simple synovectomy alone in 31 hips, joint debridement in six hips, and proximal femoral varisation osteotomy in one. After surgery hips were immobilized in cast for one to three months according to the severity of the disease and patients pain tolerance, and then were mobilized under leg traction in bed gradually till pain subsided completely.
Results:
TB of hip healed with minimum sequelae in all children. In 18 Type one hip TB, normal hip (synovial form) anatomy was maintained, and in 25 patients with advanced lesions some defect in the femoral head and acetabulum was noticed, though painless good hip motion was maintained. Excellent to good results were obtained in 31 children (73.1%), fair in eight (18.6%), and poor in four (9.3%). In four patients with poor results, there was some residual morphological defect in the hip. None developed ankylosis of hip.
Conclusion:
We achieved good outcome with minimum sequelae in this series. The management goal should be aimed not only to heal the disease but also to maintain a painless mobile hip and anatomical cephalocotyloid relationship until maturity, and retard the development of secondary osteoarthritis.
Keywords: Tuberculosis, hip, osteoarticular, infective arthritis
INTRODUCTION
Tuberculosis (TB) of hip presents significant clinical problems, though undoubtedly it has become rarer than before.1–5 The disease once established in the hip leads to progressive destruction of the joint if untreated at an early stage, and may even proceed to pathological dislocation. The pain, loss of movement, and progressive development of deformity results in loss of function of the affected hip. Subluxated or dislocated hips following infection are difficult to be managed to obtain a stable, mobile, congruous, and concentric joint. Generally, such hips with advanced lesion luxate further and/or finally result in osteoarthritic or ankylosis even after disease healing.6–11
Diagnosis at an early stage and effective chemotherapy are vital to heal the disease and to save the joint.3–10 Antituberculous chemotherapy with or without surgical intervention has been well-documented in the literature,3–7,11–13 but residual anatomic deformity such as flexion abduction or adduction, subluxation or dislocation, and the management for those residuals in children have rarely been documented. No comprehensive treatment protocol has been outlined.14–19 The primary objectives of the management were not only the healing of the disease, but also the preservation of the joint motion till the healing of the disease and thereafter. We report this retrospective study on hip TB in children treated between 1971 and 2000 AD.
MATERIALS AND METHODS
Forty-three children, 25 males, and 18 females age ranged from 3 to 15 years were treated at four different hospitals of Seoul between 1971 and 2000. Twenty-four children of the first series were treated between 1971 to 1975, and 19 children of the second series were treated between 1976 to 2000. The patients’ complaints were night sweat and weight loss, pain in hip at rest and motion, restricted hip motion, limping, flexed and abducted hip attitudes. Sixteen patients had active lung TB. None had history of high fever just before the clinical presentation of the hip symptoms, and had previous history of trauma. The duration of the illness was one to six months. All children had positive Mantoux test. Intraosseous iliac lesions in two cases and femoral neck lesion in one were included as extracapsular type. The hip lesions in 18 children with normal cephocotyloid anatomy on X-ray were diagnosed as an early infection, and the hips in 25 children had advanced disease. Shanmugasundaram's morphological classification was used for radiographic staging [Figure 1A]. Eighteen had TB hip of normal type, 5 with travelling acetabulum, 5 with dislocation type, 7 with Perthes type, 2 with protrusio acetabuli, 4 with atrophic type, and 2 with mortar and pestle type.
Figure 1A.
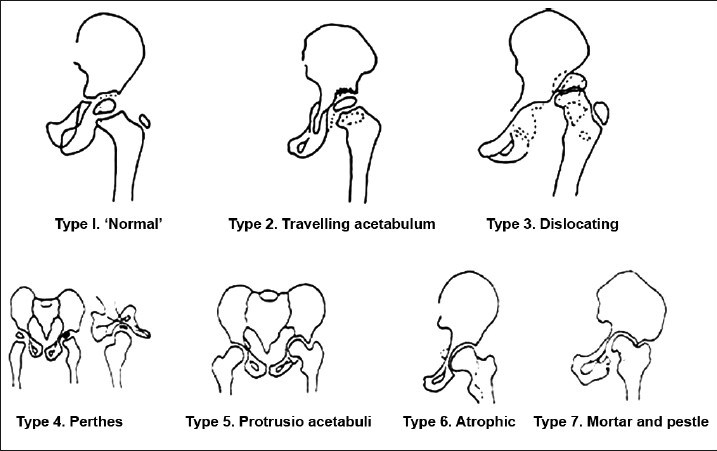
Radiological types of tuberculosis of the hip, redrawn from Shanmugasundaram (1983)3
Provisional diagnosis at initial examination was made on the basis of the clinical, laboratory (complete blood counts, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP)), and radiological findings of the lung and hips. The ESR and CRP were studied to assess the response to chemotherapy. The routine cytological and culture study of aspirates and histological study of the excised synovium and debrided tissues were carried out. Joint aspirates from all patients were routinely subjected to culture and cytological studies. Tuberculosis was strongly suspected if there were no growth of any pyogenic bacteria,8 and if a sheet of lymphocytes and giant cells instead of neutrophils and plasma cells were found in the aspirates.10 Transient synovitis, Legg-Calve-Perthes disease, and pyogenic arthritis was ruled out. Histological diagnosis of excised synovium and debrided materials could be made in 21 patients. Routine culture for M. tuberculosis was not attempted. Polymerase chain reaction (PCR) test of the aspirates and tissue specimens were not performed.
Combined oral nutritious food supply, antituberculous chemotherapy, with or without leg traction in bed were started immediately for all patients, when tentative clinical diagnosis was made even before conclusive bacteriological and histological diagnosis was provided.
First 18 patients (till 1975) were treated by isoniazid (INH; H), streptomycin (S) and PAS (Pa) for 18 months (regimen of INH, PAS, SM for three months and INH, PAS for 15 months) and thereafter (after 1975) INH (H), rifampicin(R), ethambutol (E) or pyrazinamide (Z) were administered for 12 months. Second line and newer drugs were not used for any of the patients. Four-drug regimen (H, R, E, Z) for 12 months was prescribed for the seven patients with relatively advanced lesions who had joint debridement surgery in the second series.
Only five out of 18 patients with normal appearing hip type (early cases) TB were treated conservatively with chemotherapy alone including leg traction in bed for three to four weeks, because the patients’ parents did not accept the surgery.
Our therapeutic plan was to subject the patients to surgery primarily for diagnostic biopsy and secondly to excise the proliferative and thickened diseased synovium and necrotic tissues. Thirty-eight patients were subjected to surgery; 13 patients with normal appearing hips and 25 patients with advanced lesions. Simple synovectomy in 31 hips, joint debridement in six hips, and femoral varisation osteotomy in one subluxated hip was done. The surgical peeling off of the articular cartilage was not carried out during debridement.
After synovectomy and joint debridement, hip spica cast was applied for one to three months in 32 out of 38 hips according to the severity of the disease, and it was followed by skin or skeletal leg traction of two to three weeks in bed, for free active assisted hip mobilization for around 5 min every hour on the basis of the patients’ hip pain tolerance. The remaining six patients with advanced lesions were subjected to leg traction immediate postoperatively, because the patient support groups rejected the cast immobilization. Same postoperative management for 14 patients with unstable hips showing upward subluxation, protrusio acetabuli, and mortar and pestle type hips were given, as it was done for the stable non luxated hips.
All efforts were made to maintain the mobility of the hip even for the casted hips by encouraging the children to do the hip muscle strengthening exercises and the moving exercise of their hip joints inside the cast. Partial weight-bearing ambulation was permitted when the pain was tolerable or had subsided.
For a patient with silent travelling acetabulum, varisation osteotomy was carried out to reposition the femoral head. There were no candidates of joint resection surgery or arthrodesis. Drug responses, and healing of the disease were assessed clinically by improvement in the symptoms, the laboratory data (total blood count, ESR, CRP), and observations on imaging. Outcome was not assessed by the residual anatomical defects in hip morphology and patients’ satisfaction [Table 1], because feed back on the satisfaction by the sick children and their supporters did not coincide each other. The final outcome assessment was done rather on the basis of the hip function.
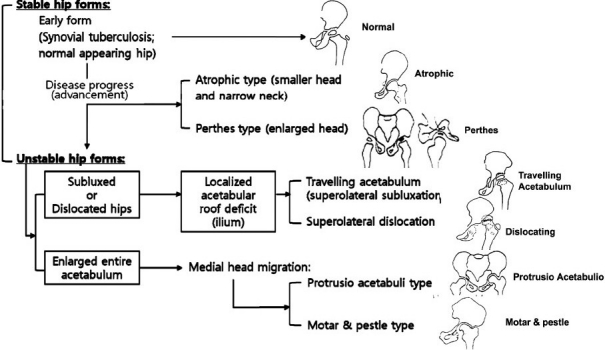
Table 1.
Outcome assessment (Moon, 1984)12
RESULTS
The mean followup was 3 years (range 1.4-13.7 years).
The lesion healed in all with no drug-related complications. The mean ESR before chemotherapy was 57 mm/h (range, 35-57 mm/h), which became normal with mean 12 mm/h (range 9-18 mm/h) within two to three months. CRP values on average before and after treatment at 3, 6, 9, and 12 months were 3.9 mg/dL (range, 3.6-4,4 mg/dL), 0.43 mg/dL (range, 0.22-1.1 mg/dL), 0.08 mg/dL (range, 0.17-0.04 mg/dL), 0.06 mg/dL (range, 0.13-0.03 mg/dL), and 0.04 mg/dL (range. 0.06-0.02 mg/dL), respectively.
No growth of pyogenic bacteria was obtained on joint aspirates of all patients while a sheet of lymphocytes, giant cells and necrotic cells were found in the absence of neutrophils and plasma cells by cytological study. Histological studies of the excised synovium and debrided tissues in 21 of 25 patients showed classic tubercular granuloma. However, M. tuberculosis was found in the tissue specimens of only seven patients.
Regional osteoporosis of the femoral head and neck was observed in most cases regardless of the stages of the disease. The osteoporosis severity related with the disease chronicity.
The results of the non-surgical treatment in five children with normal appearing hips were the same as those of the synovectomy in 13 children with normal appearing tuberculosis of hip. In those18 patients with normal appearing hip TB (Type 1), the normal hip function and anatomy were maintained clinically and radiologically till the end of treatment.
The other 25 surgically treated patients had painless near normal hip motion without visible deformities. In all patients the femoral heads were preserved even in the unstable hips. Avascular necrosis of the femoral head and spontaneous hip fusion were not seen in any patient. The disease arrest began to be observed average at 3.2 months post-chemotherapy (range 2-4 months), and the complete arrest at an average 5.7 months (range 5-7 months). The final healing was observed at an average of 10 months (range 8-11 months) together with the complete subsidence of the disease-related clinical symptoms and signs and normalization of the laboratory data.
Clinically excellent to good results were obtained in 31 children (72.1%), fair in eight (18.6%), and poor in four (9.3%). The four poor results were found in cases of protrusio acetabuli and mortar and pestle type, and they had mild hip pain, some residual limp and/or slight flexion contracture of the hip. On X-rays minor morphological abnormalities in the joints were observed in 22 patients with advanced lesions. But they did not complain of pain in or around the hips at the time of termination of chemotherapy and in up to 5 to 13.5 years’ followup, though they might lead to coxarthrosis in early adult life.
Advanced disease left some limitation of hip motion with flexion contracture, and more residual cepholocotyloid defect. The disease healing and residual pain did not closely correlate with the stages of the disease.
DISCUSSION
Tuberculosis of hip, though undoubtedly rarer in the developed countries,1–9 still presents significant problems in the less privileged countries. Its incidence is next to the TB of spine.
In making a diagnosis the authors depended more on the clinical features, classical laboratory data, study of aspirates, histological and imaging findings, because the conventional culture for tubercle bacilli was a very tedious process, and delayed the treatment. Also, modern molecular diagnostic techniques such as PCR and ex-vivo interferon-γ test were not available till 1990. The accuracy of the clinical diagnosis was confirmed by the chemotherapy results.
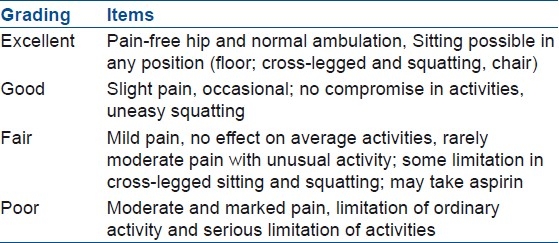
Babhulkar and Pande introduced a classification, based on disease progress.1 However, it was difficult to convert their classification into Shanmugasundaram's which was based on the destructive pattern.3 The current authors introduced their working classification and compared it with Shanmugasundaram's. Tuberculosis of the hips in children, was classified by the current authors based on the joint stability, cephalocotyloid morphology and its anatomical relationship. Also, the relation of the current authors’ and Shanmugasundaram's classifications is illustrated for comparison [Figure 1B].
Figure 1B.
Classification of tuberculosis of hip in children, based on the joint stability, cephalocotyloid morphology and its anatomical relation with Shanmugasundaran's classification (Moon, 1984)12
Early diagnosis and effective chemotherapy are vital to save the joint.3,6,8–14 When the joint proper is not involved, the disease can be treated without residual deformity by chemotherapy alone. Thus, painless, stable and mobile joint can be maintained till the end of treatment and thereafter. For TB limited to the synovium, rest and chemotherapy may be sufficient, and this is more common in children. Most tuberculous hips appearing normal on radiograph usually respond well to chemotherapy. The fact was proven in the current series because the results of the treatment in two different therapeutic groups (non-synovectomy and synovectomy) of children with normal appearing hips were equal. Thus, our conclusion is that synovial TB is purely a medical condition. In the current series the chemotherapy was started without delay when the provisional clinical diagnosis was made. Thus, the golden time to save the joint was not lost. The normalization of the inflammatory markers at three months after chemotherapy was judged as good disease response for the antitubercular drugs. For the early synovial form of TB, regardless of the type of treatment, graduated hip movement was started as soon as possible when the pain was relieved and the muscles’ spasm subsided under chemotherapy.3,6,9,12
In advanced cases with joint destruction, with or without pathological dislocation, surgical management to restore and/or to maintain hip function becomes increasingly difficult.10–12 Fortunately, with the availability of potent antitubercular agents the disease can be successfully controlled, but restoration of normal function of the hip joint is a problem. An ideal result would be one which would achieve a painless, stable and mobile hip joint, particularly in our region, for comfortable floor life at home and religious activities.
In the last three decades there has been a remarkable advances in the diagnosis and management.11–13 All efforts were made to preserve the hip anatomy, joint mobility and growth plates of the femoral head and tri-radiate cartilage until maturity by avoiding the conventional clean radical debridement surgery.1,2,5,7,14 It is known that during the early stage the disease is predominantly synovial, and that adequate treatment could prevent damage to the joint cartilage and underlying bone and thereby preserve joint function, particularly in children.14–19
It was confirmed that total synovectomy was not essential in every patient. During synovectomy around the femoral neck, utmost attention was paid to not damage the feeding vessels to the head, located beneath the hypertrophied synovium, and to not dislocate the femoral head to ease the synovectomy procedure.3–5 The current authors’ view was that the surgery-related early and late complications could be minimized by following the aforementioned surgical guideline.
In the past, the loosened articular cartilages in the lesion were radically excised by surgeons who were very reluctant to preserve the loosened articular cartilage.1–5,14 In osteoarticular TB cartilage destruction is mechanical, and not enzymatic. In all types of hip TB of the current series the femoral epiphyseal, physeal and tri-radiate cartilages were relatively well preserved even in cases of enlarged acetabular sockets. Thus, during debridement, the partly loosened articular cartilage was intentionally preserved. No patient in the current series developed early physeal closure of the proximal femoral physis and tri radiate cartilage. Consequently, almost normal femoral and acetabular growth continued, though there were some residual deformities of the femoral head and acetabulum.
Joint space narrowing indirectly indicates the destruction of the articular cartilage. Based on this fact it was reported that the predicted outcome was poor when the joint space was reduced to 3 mm or less.2,7 In the current series the joint space narrowing could be lessened by leg traction which coincided with Tuli's report.7
It was interpreted by the current authors that the hips in Perthes type, atrophic hip, and protrusio acetabuli were stable, while the travelling acetabulum, mortar and pestle, and dislocating hip types were unstable. However, all those unstable hips became stable at the end of the treatment. The issue was how to manage the unstable subluxated or dislocated hips in children, because there were no detailed documentations related to the subluxated and luxated hips in the previous literature. No comprehensive treatment program has been outlined except Choi et al.,'s report on the pyogenic hips.17 Regardless of the stage of the disease, TB healed in all patients [Figures 2–5]. Initial hip traction in bed was very rewarding in relieving the hip pain and muscle spasm, and in maintaining hip motion, and correcting the hip deformity during the mobilizing exercises. Lateral subluxation of the femoral head was considered to be caused by chronic synovitis, and destroyed femoral head and/or acetabular roof.
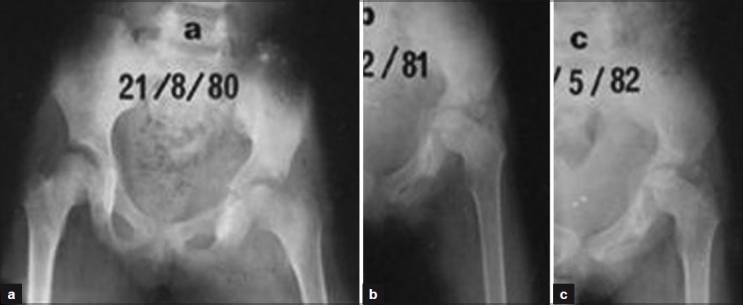
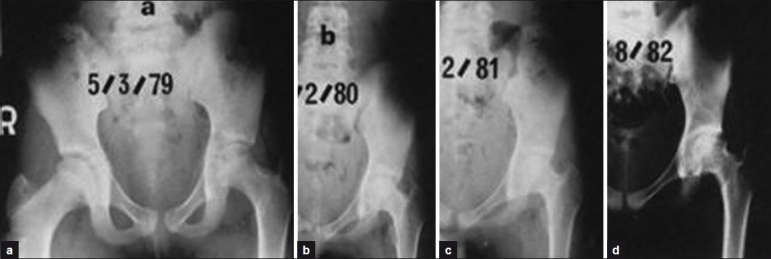
Figure 2.

X-ray pelvis with both hips anteroposterior view (a) and (L) hip joint (b, c) showing an example of normal hip type tuberculosis secondary to iliac acetabular lesion of left hip (a, b). Triple chemotherapy for 12 months and bed rest was given. The tuberculosis lesion had healed without joint damage and sequelae (c)
Figure 5.
X-ray pelvis both hips (a) and (L) hip joint (b, c) anteroposterior view showing an example of relatively advanced tuberculosis of left hip in a 12-year-old boy (a). After joint debridement of left hip, hip was casted for 2 months under the cover of triple chemotherapy (b). However, there was progressive joint destruction. Therefore, chemotherapy was changed to 4 drug regimen. Finally mortar and pestle type of hip was seen (c). However the boy was free from pain, and his hip was clinically stable. He could enjoy almost normal life
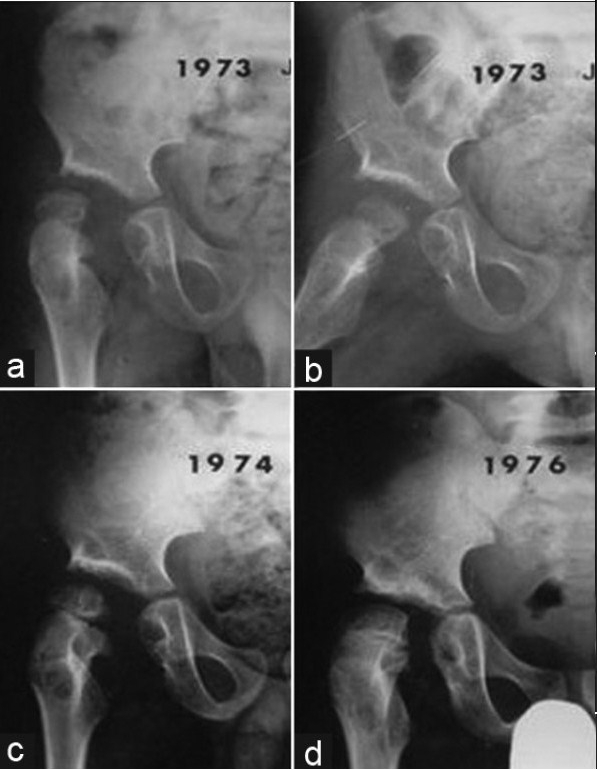
Figure 3.

X-ray pelvis both hips (a) and (L) hip joint (b, c) anteroposterior view showing an example of Perthes type hip secondary to epiphysio-metaphyseal tuberculosis of the left proximal femur (a, b). After joint debridement, the child was immobilized with cast for 6 weeks under cover of triple chemotherapy (12 months). Tuberculosis healed without joint destruction, though residual coxa magna deformity was present (c)
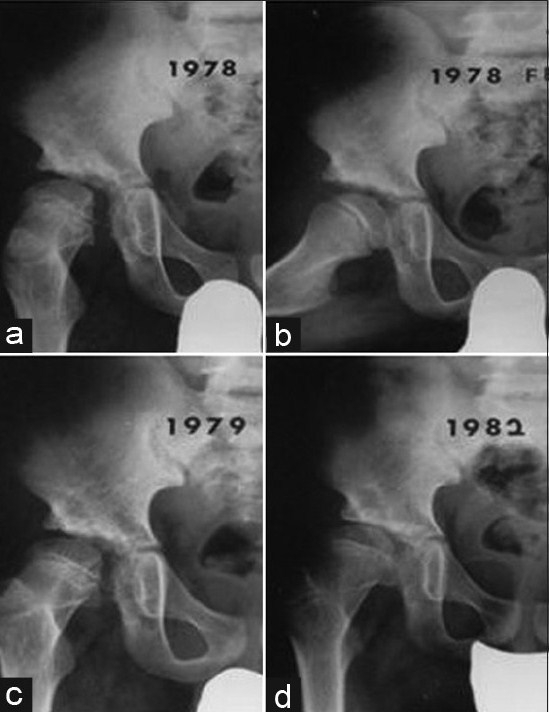
Figure 4.
X-ray pelvis both hips (a) and (L) hip joint (b, c, d) anteroposterior view showing an example of atrophic type hip due to tuberculosis of hip in a 11-year-old girl. There is slight joint space narrowing of left hip with slight pubes varus deformity of left pelvis (a). After synovectomy chemotherapy for 12 months was given (b, c, d). Tuberculosis healed (3 years followup) though atrophic head and neck are seen (d)
For the dislocated hip, non-surgical and surgical reduction and hip cast immobilization should be practiced, while for the subluxated hip such as travelling acetabulum, reposition of the laterally and upwardly displaced femoral head into the acetabulum should be performed by varization osteotomy. The abduction brace or cast is non-effective [Figure 6A–C].
Figure 6A.
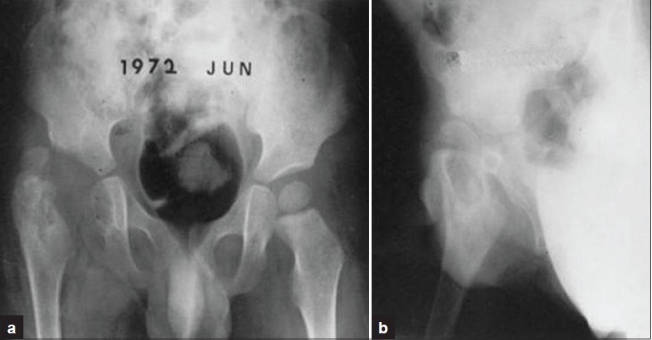
X-ray pelvis both hips (a) and (R) hip joint (b) anteroposterior view showing an example of dislocating type of tuberculosis of hip in a 3-year-old boy. Multiple cystic lesions on epiphysis, metaphysis of the proximal femur, and medial aspect of the ischium, with an enlarged acetabulum (mortar type) destructive change are seen, but triradiate cartilage is well preserved
Figure 6C.
(a, b, c, d) followup serial roentgenograms taken in February 1978, March 1979 and February 1982 still show some widening of the medial joint space with complete disappearance of the initial multiple cystic lesions on the epiphysis, metaphysis and ischium. Joint space narrowing and subchondral sclerosis of the right acetabular dome indicate the early osteoarthritic changes
Figure 6B.
(a, b, c, d) followup radiograms (R) hip of same patient demonstrate the spontaneous gradual medial head migration and disappearance of the cystic bony lesions, though there is slight femoral head subluxation
Somerville listed postoperative anterior capsular laxity as a cause of redislocation in congenital hip dislocation, but no previous authors found it to be a cause of redislocation in hip TB after anterolateral radical joint debridement [Figures 7A and B]. Somerville stated, “If the postoperative capsular laxity as a cause of congenitally dislocated hip was transitory, any recumbency treatment failed”. Therefore, he believed such a child should be encouraged to mobilize and start weight-bearing as soon as possible, and that this would benefit the laxity and the dislocation.12 If capsular laxity persisted he suggested anterior capsular reefing with the hip held in full medial rotation. The current authors believed that in Case 6 [Figures 6A and 6C], spontaneous reduction of the head to the acetabulum on roentgenograms could be attributed to the early mobilization of the hip.
Figure 7A.
X-ray pelvis with hips (a) and (L) hip joint anteroposterior view showing an example of travelling acetabulum in a 6-year-old boy. Hip was immobilized by cast for 2 months under cover of the triple antitubercular chemotherapy (a). Boy restored painless unlimited hip motion, though subluxation persisted on radiogram. Intertrochanteric femoral osteotomy was performed to treat the subluxed hip (b, c). Radiograms taken at postoperative one year and one year 6 months demonstrate the well seated femoral head in the acetabulum with slightly widened socket dome space (d, e)
Figure 7B.

Radiograms taken on postoperative 9 year (at age of 15 years) pelvis with both hips (a) and (L) hip (b) anteroposterior view demonstrates the good cephalocotyloid relationship, though some enlarged and flattened head with pubes varus deformity are seen
Since the pathologically dislocated hips generally did not become normal spontaneously during growth, every effort should be made to detect the disease early, and take the appropriate remedial measures.7–10 If the abducted femoral head hinged on the acetabular margin, as in most of the subluxated or dislocated hips following infection, spontaneous progressive cephalocotyloid improvement could not be expected without having a non hinging hip by any measure. The senior author (MSM) of the current series recommended early varisation osteotomy to restore a normal cephalocotyloid relation of the travelling acetabulum secondary to hip TB in children. As a condition, he suggested that varus osteotomy was indicated only when the head position was improved in the socket by abduction.13,19 It was right that immobilization of the diseased hips by the leg traction in bed and cast for a short time was helpful, either to relieve pain, to maintain the joint stability and mobility, or to correct deformity before and after surgery.
As regards the ambulation, Tuli recommended very thoughtfully gradual weight-bearing after four to six months of treatment, and permitted unsupported weight-bearing at 18 to 24 months. However, the current authors permitted early ambulation at the time when the pain subsided and was tolerable to bear weight and subsided. Our proposed rehabilitation regimen for ambulation boosted the patients’ confidence and activity level.
It is a noteworthy fact that none of the previous authors provided evidence data in defining the healing of the disease. The final issue is how long will pediatric patients remain pain free after healing of the disease because there is a possibility that the healed hip will show degenerative changes because of the residual cephocotyloid deformity, in early adulthood. Therefore, the management goal should not only to achieve healed status but also maintain normal cephalocotyloid relationship and muscle power around the hip, and prevent and retard the development of secondary osteoarthritis. Thus, a better condition for hip replacement surgery in adulthood can be provided, when the secondary osteoarthritis becomes symptomatic.
The limitations of this study are its retrospective nature, different chemotherapeutic formula in two groups, a small and unequal number of each radiologic type, unequal followup time for each case, different disease stage at the time of management, and different management including surgery.
In conclusion, clinical and radiological diagnosis was the key component in designing the management. Antituberculous drugs are the mainstay of treatment. Early initiation of chemotherapy and judicious surgical intervention can help to promote early healing, minimize residuals, and maintain the hip function until adulthood.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Babhulkar S, Pande S. Tuberculosis of the hip. Clin Orthop Relat Res. 2002;398:93–9. doi: 10.1097/00003086-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Campbell JA, Hoffman EB. Tuberculosis of the hip in children. J Bone Joint Surg Br. 1995;77:319–26. [PubMed] [Google Scholar]
- 3.Shanmugasundaram TK. A clinicoradiological classification of tuberculosis of the hip. In: Shanmugasundaram TK, editor. Current concepts in bone and joint tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Club and the Indian Orthop Assoc; 1983. p. 60. [Google Scholar]
- 4.Vora PH. Role of early surgery in management of tuberculosis of hip. In: Shanmugasundaram TK, editor. Current concept in bone and joint tuberculosis. Madras, India: Proceedings of Combined Congress of International Bone and Joint Tuberculosis Clue and the Indian Orthopedic Association; 1983. p. 60. [Google Scholar]
- 5.Metha MT. Prognosis of tuberculous arthritis. In: Shanmugasundaram TK, editor. ibi-dem. Chennai: 1983. pp. 78–80. [Google Scholar]
- 6.Masood S. Diagnosis of tuberculosis of bone and soft tissue by fine needle aspiration biopsy. Diagn Cytopathol. 1992;8:451–4. doi: 10.1002/dc.2840080505. [DOI] [PubMed] [Google Scholar]
- 7.Tuli SM. Tuberculosis of the skeletal system (Bones, Joints, Spine and Bursal sheaths) 2nd ed. New Delhi: Jaypee Brothers Medical Publishers PVT Ltd; 1997. Tuberculosis of the hip joint; pp. 59–96. [Google Scholar]
- 8.Mousa HA. Evaluation of sinus-tract cultures in chronic bone infection. J Bone Joint Surg. 1997;78:567–9. doi: 10.1302/0301-620x.79b4.7316. [DOI] [PubMed] [Google Scholar]
- 9.Finegold SM, Baron EJ. Baily and Scott's diagnostic microbiology. St Louis: Mosby Co; 1986. [Google Scholar]
- 10.Moon MS, Kim I, Jung TI. Diagnosis of bone lesion by fine needle aspiration biopsy. J Korea Orthop Assoc. 1978;13:7–12. [Google Scholar]
- 11.Moon MS, Kim I, Kim JM, Lee HS, Ahn YP. Synovial biopsy by Franklin-Silverman needle. Clin Orthop Relat Res. 1980;150:224–8. [PubMed] [Google Scholar]
- 12.Moon MS, Rhee SK, Lee KS, Kim SS. A natural course of a dislocated healed tuberculous hip in a child: A case report. Clin Orthop Relat Res. 1984;190:154–7. [PubMed] [Google Scholar]
- 13.Moon MS, Lee KS, Kim YS. Varisation osteotomy in subluxated hip as sequella of healed tuberculosis in children. J Korea Orthop Assoc. 1982;17:203–5. [Google Scholar]
- 14.Moon MS, Choi NY. Treatment of residual dislocation and subluxation of tuberculous hip in children. In: Ueno, Akamatsu, Itami, editors. The Hip Clinical studies and basic research. Amsterdam; New York; Tokyo: Excerpta Medica Internet Series; 1984. p. 634. [Google Scholar]
- 15.Mitchell GP. Management of acquired dislocation of the hip in septic arthritis. Orthop Clin North Am. 1980;11:51–64. [PubMed] [Google Scholar]
- 16.Medical Research Council Working Party on Tuberculosis of Spine: Five-year assessment of controlled trials of ambulant treatment, debridement and anterior spinal fusion in the management of tuberculosis of the spine. Studies in Rhodesia and Hong Kong. J Bone Joint Surg. 1978;60:163–76. doi: 10.1302/0301-620X.60B2.350883. [DOI] [PubMed] [Google Scholar]
- 17.Choi IH, Pizzutillo PD, Bowen JR, Dragann R, Malhis T. Sequellae and reconstruction after septic arthritis of hip in infants. J Bone Joint Surg Am. 1990;72:1150–65. [PubMed] [Google Scholar]
- 18.Somerville EG. Aetiology, management and sequellae. Berlin, Heidleberg: Springer-Verlag; 1982. Displacement of the hip in children; pp. 104–6. [Google Scholar]
- 19.Moon MS, Sun DH, Jung CH. Surgical treatment of pathological dislocation of child hip after acute osteomyelitis of ilium – a case report. J Korea Orthop Assoc. 1994;29:412–14. [Google Scholar]



