Abstract
Background:
The incidence of Tuberculosis (TB) of elbow is 2-5% of all skeletal locations. Most reports of TB elbow have focused attention on the diagnosis. The management options and classification has been missing. We present a retrospective clinicoradiological analysis of 38 cases (40 elbows) of TB of elbow joint.
Materials and Methods:
The patients presented with pain, swelling and loss of motion. Two cases had bilateral involvement. The average delay between onset of symptoms and presentation was 8 months. The elbows were classified according to modified Martini's radiological classification, which distinguishes between osseous lesions close to joint line (e.g. coronoid, condyles) and lesions away from the joint line (e.g. epicondyles, olecranon). We modified the classification to subdivide into para-articular bony lesions that had invaded the joint and those that were threatening to invade joint. All patients received antitubercular chemotherapy and immobilization in above-elbow plaster slab for 4–8 weeks. Twenty patients underwent surgical interventions (synovectomy, intraarticular debridement).
Results:
The average followup period was 5.3 years (range 1.5-14.2 years). The range of movement at final followup averaged 107° for stage 2, 90° for stage 3A, 47° for stage 3B and 32° for stage 4. Range of supination and pronation was less satisfactory as compared to flexion and extension and all elbows with bony involvement had less than 90° arc of supination and pronation.
Conclusion:
Surgical intervention could appreciably alter the outcome especially in patients with extra-articular involvement close to the joint. We have classified this subgroup separately.
Keywords: Elbow, infection, tuberculosis
INTRODUCTION
The elbow joint is the most frequently involved joint in tubercular infections of the upper limb. The reported incidence of elbow TB varies from 2 to 5% of all skeletal locations.1,2 There are few published major reports focusing on TB of the elbow joint.3–8 Wilson (1953),4 managed cases with prolonged immobilization and classified the condition radiologically. Martini et al.5,6 classified the cases into four radiological types and the treatment was based on the severity of radiological involvement.7 In most of the reports of TB elbow has focused attention on the unique diagnosis.3,6,8 The management options and classification has been missing. We present a retrospective analysis of patients of TB elbow. Our study led us to modify the existing radiological classification6,7 and distinguish between osseous lesions present away from and those present close to the joint. This may be helpful in prognosticating the functional end result and defining the management options.
MATERIALS AND METHODS
This retrospective study included thirty-eight patients (40 elbows) with TB of the elbow, treated between July 1992 and July 2006. The data was obtained from the case records of the hospital. The pain, duration of symptoms prior to diagnosis, range of motion (ROM) and deformity were recorded in all the cases. The pre treatment and followup radiographs were available for all the patients. We documented the principal radiological findings, the different sites of bony lesions and extent of bony involvement around the elbow joint at the time of presentation. The clinical parameters at last followup were evaluated.
The diagnosis of elbow TB was confirmed by needle aspirate in six elbows, which was subjected to histopathology, AFB staining, and polymerase chain reaction (PCR), for Mycobacterium complex and by histopathologic examination of open biopsy specimen in 28 elbows. When open surgical procedure was performed (n=28), a formal joint debridement was done for cases undergoing biopsy where joint involvement was already evident, while in other cases as much of the pathological tissue as possible was removed at the time of biopsy without jeopardizing the integrity of the bone. Out of the 28 specimens, 20 did not show the AFB, but the histopathologic findings confirmed TB pattern (epitheloid infiltration, tubercle formation, caseous necrosis and Langhan's gaint cells). Four patients were treated based on the clinicoradiological grounds alone; two patients with bilateral involvement had biopsy done on the side with initial presentation. Two cases had involvement of other skeletal sites; only in four cases was clinically or radiologically evident pulmonary or visceral TB documented. The supratrochlear (n=4) and axillary (n=3) lymph nodes, were enlarged in seven cases.
All patients were treated for a total period of 14–18 months with antitubercular chemotherapy as per the protocol followed at our institute.1 Initial intensive treatment phase [four drugs comprising lsoniazid (INH), Rifampicin, Ethambutol and Pyrazinamide for 2 months] was followed by continuation phase protocol (INH and Rifampicin, plus Ethambutol for two more months) and maintenance phase (INH plus Rifampicin) for another 10–14 months. All the elbows were immobilized initially in an above elbow plaster slab for a period of 4–8 weeks at 90° of elbow flexion and neutral forearm rotation, till the inflammation, swelling and spasm subsided. This was followed by mobilization of elbow and strengthening protocols for 2–6 months. The back slab was continued during night time and rest periods for periods ranging from 3 to 6 months. Surgical debridement was carried out in selected cases (n=28). The indication of surgery was either patients not responding to chemotherapy of 4–6 weeks (n=3), cases where lesions close to joint line were threatening intraarticular spread (n=5), cases which had advanced (n=15) (stage 3B/4) disease but with functional range of movement, or diagnostic dilema (n=5). Debridement was combined with open biopsy for 5 elbows. Followup assessment included clinical parameters like pain, range of movement, deformity and subjective evaluation of functional disability as well as followup radiographs to look for signs of healing. Serial erythrocyte sedimentation rate (ESR) assessment was done to determine the response to antituberculosis treatment (ATT). The final result at followup was classified as excellent, good, fair or poor, depending on the final range of movement. Elbows with >120° ROM were classified as having excellent outcome and elbows with an ROM of about 80°–120°, 50°–80°, or <50° were classified as having good, fair or poor outcome.
The patients were classified into four stages using a classification that was modified from Martini's original radiographic classification6,7 [Table 1] and we correlated these retrospectively with the treatment protocols employed. Stage 1 included those without any evident radiological osseous lesions. Stage 2 patients included those with involvement of epicondyles and olecranon (away from the joint line) [Figure 1]. Stage 3 includes lesion of condyles, coronoid process, head of the radius and those of the olecranon, which were potentially threatening to invade the joint. Stage 3 was again divided into stage 3A (pathology not extending into the joint) [Figure 2] and stage 3B (extension into joint) [Figure 3]. Stage 4 included those with gross destruction of the joint, pathological fractures, or dislocations [Figure 4].
Table 1.
Prognostic classification of TB elbow6
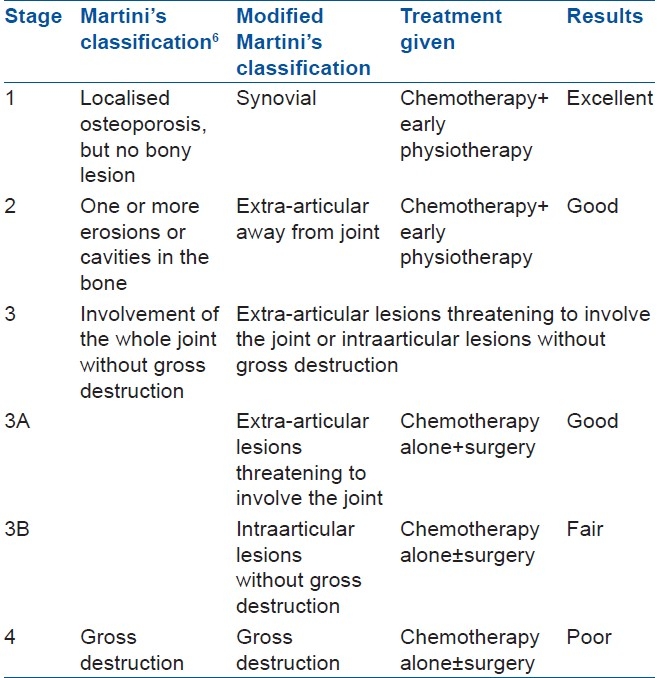
Figure 1.

Anteroposterior view of elbow showing stage 2 lesion involving medial epicondyle only
Figure 2.

Anteroposterior and lateral view of elbow showing stage 3A involvement (limited to coronoid)
Figure 3.
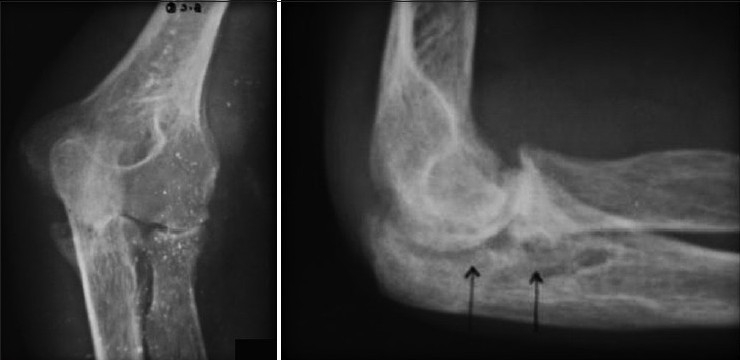
Anteroposterior and lateral view of elbow showing stage 3B involvement (joint involvement without significant destruction)
Figure 4.
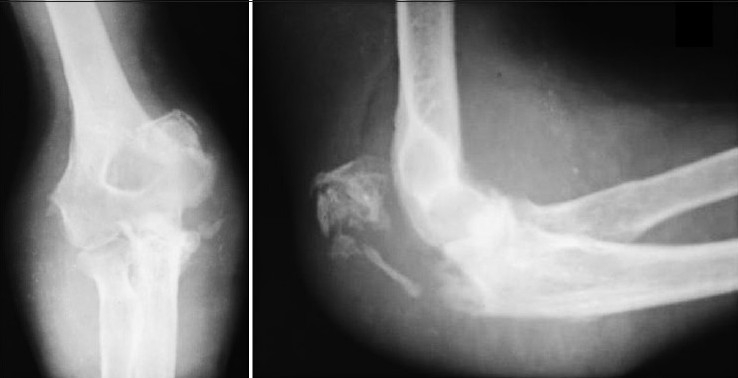
Anteroposterior and lateral view of elbow showing stage 4 involvement (gross joint destruction with pathological fracture)
Retrospective correlation of clinicoradiological types with the management protocols employed was done, and functional end results were correlated with radiology, clinical features, delay in presentation and type of therapeutic measures undertaken.
RESULTS
Out of 38 patients, there were 15 male and 23 female patients. Right side was involved in 21 and left side in 19 elbows (2 bilateral). Age ranged from 6 to 70 years (mean 33 years). Delay between onset of symptoms and presentation to hospital averaged 8 months (range 3–15 months).
On the basis of radiological picture at presentation, patients were retrospectively classified according to our modification of Martini classification. One patient in stage 1 (synovitis only) was treated with chemotherapy and physical therapy alone, and regained full functional motion range with no disability.
The detailed site wise distribution of elbow TB is given in Figure 5. 10 elbows were classified as stage 2. The average range of movement in stage 2 cases at presentation was 91° (range 65°–115°). All stage 2 patients were treated with chemotherapy and physiotherapy alone.
Figure 5.
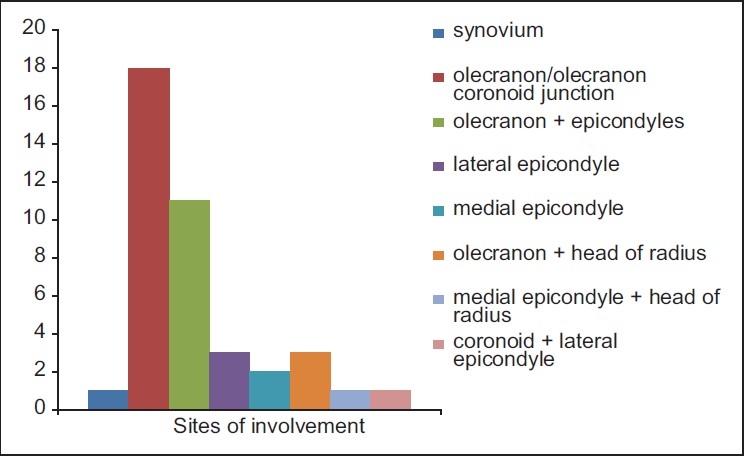
Bar diagram giving site wise details of involvement
Twenty-two elbows were grouped as stage 3, with 5 being in stage 3A and 17 in stage 3B. Stage 3A elbows had pre-treatment average ROM of 63° (60°–70°) and stage 3B had an average ROM of 36° (range 0°–60°).
Eight elbows were classified as stage 4 and had a limited ROM (0°–45°). Three of the stage 3B and stage 4 cases had bony ankylosis and three had fibrous ankylosis at presentation. Seven patients had lymph node enlargement (2 epithochlear and 5 axillary), while 7 patients had one or multiple sinuses.
The most common site of osseous lesion was the olecranon, followed by lateral epicondyle [Figure 4]. On review of our patients, we found that out of 30 stage 3 (A and B) and stage 4 elbows, 20 patients with poor response to initial chemotherapy of 4–6 weeks or with radiologically destructive lesions had undergone either a synovectomy or intraarticular debridement and curettage to remove caseous and necrotic material. Four patients with stage 4 disease and six with stage 3B disease, with poor range of preoperative mobility (<20°), were treated conservatively, expecting a bony/fibrous ankylosis. No formal elbow arthrodesis was done, and only in one elbow had excision arthroplasty been recommended to improve the range of motion, which was refused by the patient.
Followup periods at final review for purposes of this study averaged 5.3 years (range 1.5–14.2 years). The average ranges of movement at final followup were 107° for the stage 2 elbows (range 85°-130°), 90° for the stage 3A elbows (range 85°-100°), 47° for stage 3B elbows (range 0°-80°) and 32° for stage 4 elbows (range 0°-60°) [Table 2, Figure 6]. The range of pronation and supination was less satisfactory; only 17 patients had more than 90° of pronation and supination. 23 of 40 elbows were painless, while 13 elbows had pain with stressful activity, with 4 having residual disabling pain. No surgical procedure was carried out as pain was on stress only. Pain was managed symptomatically with oral analgesics whenever required.
Table 2.
Results according to different stages of involvement
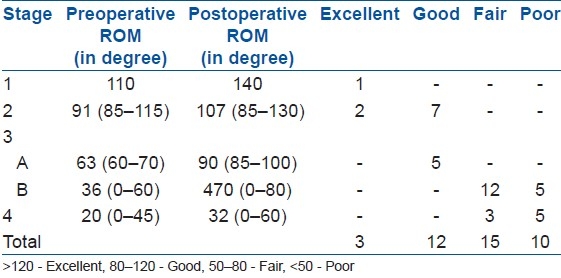
Figure 6.

Anteroposterior (a) and lateral (b) radiographs showing bony ankylosis after anti tubercular chemotherapy
DISCUSSION
Tuberculous infection in the elbow joint usually starts in the olecranon and lower end of humerus,9 and very rarely is the primary disease limited to the synovium.2 This was reflected in our study also where the olecranon was noted to be the most common site of involvement, followed by the lateral humeral condyle. Only one case presented with a purely synovial lesion.
The majority of the cases in our series had significant joint involvement at presentation. This is similar to previous studies [Table 3] and is probably related to the delay is diagnosis (mean diagnostic delay seen by us was 8 months). The common diagnostic confusion in elbow TB is due to the similarity of disease with the more common pathologies like rheumatoid arthritis, low virulence pyogenic arthritis, gout, pigmented villonodular synovitis and even sometimes neoplasms.10 Although lymph node involvement was observed in seven patients (2 epitrochlear and 7 axillary), none underwent lymph node biopsy as all of them underwent open biopsy based on our clinical judgment regarding patients requiring operative intervention. Presence of enlarged nodes may help in obtaining tissue for establishing tuberculous infection of bone. Although helpful in diagnosis, lymph node biopsy may not be better than obtaining histopathologic tissue from osseous lesion itself and may give false-positive results as lymph node enlargement can have variable causes other than TB, especially in tropical countries.11,12
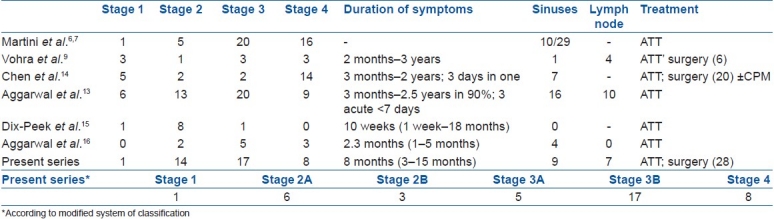
Table 3.
Summary of distribution of cases according to the classification of Martini et al. and clinical presentation of major reports published after use of chemotherapy
There are no clear recommendations regarding which cases can be managed medically and which would require surgical interventions. Keeping this in mind, our evaluation of cases, although retrospective, looked at those cases where surgery had been done and noted the functional outcomes. Our results have led us to believe that apart from cases not showing clinicoradiological improvement after 4–6 weeks of chemotherapy, several patients with extra-articular disease with an imminent danger of joint invasion (stage 3A) may benefit from early surgical intervention by rapid local control of the disease process and thereby halting it from involving the joint. Among the patients with joint involvement at presentation, those with some preservation of joint movements may also benefit from surgical debridement, but results may not be as gratifying as in extra-articular disease. All such patients undergoing surgical debridement in the present series had >20° range of movement remaining at the time of presentation and universally showed improvement in the range of movement postoperatively. Cases presenting with pure synovial involvement usually respond well to chemotherapy and short-term immobilization and adequate physiotherapy.9,13,14 This is probably because muscle spasm subsides with reduced disease activity.13 Nine cases in our series presented with ankylosis or residual movement less than 20°, and all went on to heal with a stiff but painless and stable elbow. This has also been the experience of previous authors.6,13
Many previous authors have reported favorable outcomes after surgical intervention in selected cases.9,14 Vohra et al.9 recommended curettage and synovectomy even in cases with minimal joint involvement and the patients were able to regain almost a full ROM; in advanced stages, however, they found poor results. A similar observation was made by Chen et al.,14 who noted that elbows with stage 3 and 4 disease which underwent synovectomy and intraarticular debridement went on to regain a good ROM; they, however, emphasized the importance of continuous passive motion (CPM) in the postoperative period. In our series, 20 out of 30 cases with stage 3 and 4 disease underwent synovectomy and debridement, while 10 elbows were treated conservatively with expectation of ankylosis. We also believe that the high rate of surgical intervention in our series is related to the high percentage (75%) of cases presenting with relatively advanced disease (stage 3 or 4) at our institute. Thus, there is a specific need to identify those joints which are relatively preserved, but have significant potential for invasion or destruction by the disease process, and this is the reason why we have added a new subgroup to the existing classification. However, this need of surgical intervention in a large percentage of patients (as seen in our series) might not be a true representation of the natural history of early diagnosed elbow TB; it represents only a scenario in cases which have reached an advanced stage due to inadequate treatment of diagnostic delays.
We modified the existing Martini classification and included elbows with osseous lesions close to joint or threatening to involve the joint in stage 3A, which would have been classified as stage 2 disease in the original classification. The rationale of this change in classification was that all five elbows classified as stage 3A had significantly less mean ROM at presentation as compared to those with lesions away from joint (stage 2) and all responded favorably to surgical curettage or debridement after inadequate response to ATT for 6 weeks. All other cases of stage 2 disease responded well to chemotherapy alone. To the best of our knowledge we could not find any previous study in English language literature which has made this distinction.
Only 3 of our patients presented in the skeletally immature age group (below 18 years) and all of them were managed with chemotherapy alone as they had a stage 2 disease. Dix-Peek et al.15 and Aggarwal et al.16 recently reported on the results of chemotherapy alone for treatment of elbow TB in skeletally immature patients and reported favorable outcomes. Both these authors recommended nonoperative treatment for this age group. Bilateral involvement of the elbow is also very rare. Tuli2 reported 1 case out of 44 seen in his series. We encountered two patients with bilateral disease; the contralateral elbow was involved at initial presentation in one case and the second case was diagnosed with contralateral disease 3 months after the first joint involvement. Both were immunocompetent and their healing pattern was no different than rest of the patients.
The surgical intervention could appreciably alter the outcome especially in patients with extra-articular involvement close to the joint. We have classified this subgroup separately.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Dhillon MS, Tuli SM. Osteoarticular Tuberculosis of the Foot and ankle. Foot Ankle Int. 2001;22:679–86. doi: 10.1177/107110070102200812. [DOI] [PubMed] [Google Scholar]
- 2.Tuli SM. In Tuberculosis of the skeletal system. 2nd ed. N Delhi: Jaypee Brothers; 1997. Tuberculosis of elbow joint; pp. 132–40. [Google Scholar]
- 3.Skoll PJ, Hudson DA. Tuberculosis of the upper extremity. Ann Plast Surg. 1999;43:374–8. doi: 10.1097/00000637-199910000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Wilson JN. Tuberculosis of the elbow. A study of thirty one cases. J Bone Joint Surg Br. 1953;35:551–60. doi: 10.1302/0301-620X.35B4.551. [DOI] [PubMed] [Google Scholar]
- 5.Martini M, Gottesman H. Tuberculosis of the elbow. In: Martini M, editor. Tuberculosis of the bones and joints. Berlin: Springer Verlag; 1988. pp. 87–96. [Google Scholar]
- 6.Martini M, Benkeddache Y, Medjani Y, Gottesman H. Tuberculosis of the upper limb joints. Int Orthop. 1986;10:17–23. doi: 10.1007/BF00266268. [DOI] [PubMed] [Google Scholar]
- 7.Martini M, Gottesman H. Results of conservative treatment in Tuberculosis of the elbow. Int Orhtop. 1980;4:83–6. doi: 10.1007/BF00271089. [DOI] [PubMed] [Google Scholar]
- 8.Silva KF. A review of patients with skeletal tuberculosis treated at the university Hospital, Kuala Lumpur. Int orthop. 1980;4:79–81. doi: 10.1007/BF00271088. [DOI] [PubMed] [Google Scholar]
- 9.Vohra R, Kang HS. Tuberculosis of the elbow. A report of 10 cases. Acta Orhtop Scand. 1995;66:57–8. doi: 10.3109/17453679508994641. [DOI] [PubMed] [Google Scholar]
- 10.Domingo A, Nomdedeu M, Tomas X, Garcia S. Elbow tuberculosis; And unusual location and a diagnostic problem. Arch Orthop Trauma Surg. 2005;125:56–8. doi: 10.1007/s00402-003-0612-y. [DOI] [PubMed] [Google Scholar]
- 11.Raviglione MC, O’Brien RJ. Harrison's Infectious Diseases. McGraw Hill; 2010. Tuberculosis in Kasper LD, Fauci's AS; pp. 596–617. [Google Scholar]
- 12.Pangalis GA, Vassilakopoulos TP, Boussiotis VA, Fessas P. Clinical approach to lymphadenopathy. Semin Oncol. 1993;20:570–82. [PubMed] [Google Scholar]
- 13.Aggarwal A, Dhammi I. Clinical and radiological presentation of tuberculosis of the elbow. Acta Orthop Belg. 2006;72:282–7. [PubMed] [Google Scholar]
- 14.Chen WS, Wang CJ, Eng HL. Tuberculous arthritis of the elbow. Int Orthop (SICOT) 1997;21:367–70. doi: 10.1007/s002640050187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dix-Peek SI, Vrettos BC, Hoffman EB. Tuberculosis of the elbow in children. J Shoulder Elbow Surg. 2003;12:282–6. doi: 10.1016/s1058-2746(02)00042-3. [DOI] [PubMed] [Google Scholar]
- 16.Agarwal A, Mumtaz I, Kumar P, Khan S, Qureshi NA. Tuberculosis of the elbow joint in children: A review of ten patients who were managed nonoperatively. J Bone Joint Surg Am. 2010;92:436–41. doi: 10.2106/JBJS.I.00805. [DOI] [PubMed] [Google Scholar]


