Abstract
Background:
Severe crouch gait in adolescent cerebral palsy is a difficult problem to manage. The patients develop loading of patellofemoral joint, leading to pain, gait deviation, excessive energy expenditure and progressive loss of function. Patella alta and avulsion of patella are the other complications. Different treatment options have been described in the literature to deal with this difficult problem. We evaluated outcome of supracondylar femoral extension osteotomy (SCFEO) and patellar tendon advancement (PTA) in the treatment of crouch gait in patients with cerebral palsy.
Materials and Methods:
Fourteen adolescents with crouch gait were operated by SCFEO and PTA. All subjects were evaluated pre and postoperatively. Clinical, radiographic, observational gait analysis and functional measures were included to assess the changes in knee function.
Results:
Cases were followed up to 3 years. The patients walked with increased knee extension and improvement in quadriceps muscle strength. Knee pain was decreased and improvements in functional mobility and radiologic improvement were found.
Conclusion:
SCFEO and PTA for adolescent crouch gait is effective in improving knee extensor strength, reducing knee pain and improving function.
Keywords: Crouch gait, patellar tendon advancement, supracondylar osteotomy
INTRODUCTION
Correction of crouch gait is difficult. Body mechanics contribute to the progression of knee flexion, hip flexion, and ankle dorsiflexion.1 The loss of adequate plantar flexion/knee extension couple keeps the ground reaction force behind the knee joint and in front of hip and ankle joints.2 Overactivity of the hamstring muscles is a basic finding in the electromyographic (EMG) patterns during crouch gait.3 Abnormal forces generated by a tight iliopsoas or a spastic gastrocnemius may also contribute to crouch gait, as these muscles have the potential to accelerate the hip and the knee toward flexion.4
Tight hamstrings and other muscles that are thought to restrict movement are often lengthened surgically or injected with botulinum toxin in an effort to improve stance phase knee extension and hip extension in persons with crouch gait. Many authors described hamstring lengthening or weakening as the only procedure to take care of knee flexion deformity.5–8 Multilevel orthopedic surgeries have been used to correct severe crouch gait, but no cohort studies or long term results have been reported to the best of our knowledge.9
Sutherland and Cooper propose that the two principles of treatment to overcome crouch gait are to reduce the knee flexion contracture and to restore quadriceps femoris muscle strength.10 It also seems reasonable that when both knee flexion contracture and quadriceps insufficiency can lead to crouch gait, surgical procedures targeting both need to be used.11,12
Stout et al.12 used combined distal femoral extension osteotomy along with patellar tendon advancement (PTA) with encouraging results with regard to relief of pain and improvement in community walking levels. Supracondylar osteotomy has been described in the management of poliomyelitis, myelomeningocele and other arthritic conditions, along with its complications.13,14 Distal transplantation of patellar tendon was originally described by Chandler in 1933 and a modified technique was described by Roberts et al.15
We report a prospective study of supracondylar femoral extension osteotomy (SCFEO) along with PTA in the management of adolescent crouch gait in cerebral palsy.
MATERIALS AND METHODS
Fourteen patients (M:F = 11:3) with a mean age of 13.6 (range 11–16 years) were studied prospectively [Table 1]. There were 10 diplegics and 4 quadriplegics. Four of the above said patients were operated previously by hamstring lengthening with recurrent crouch gait. All patients were admitted in a single unit and operated by the same group of surgeons. The mean followup was 2.48 years (range 1.6–3 years). Two of the patients in the study had iliopsoas spasticity.
Table 1.
Age, sex distribution, GMFCS level and soft tissue procedures performed concurrently with the index operation
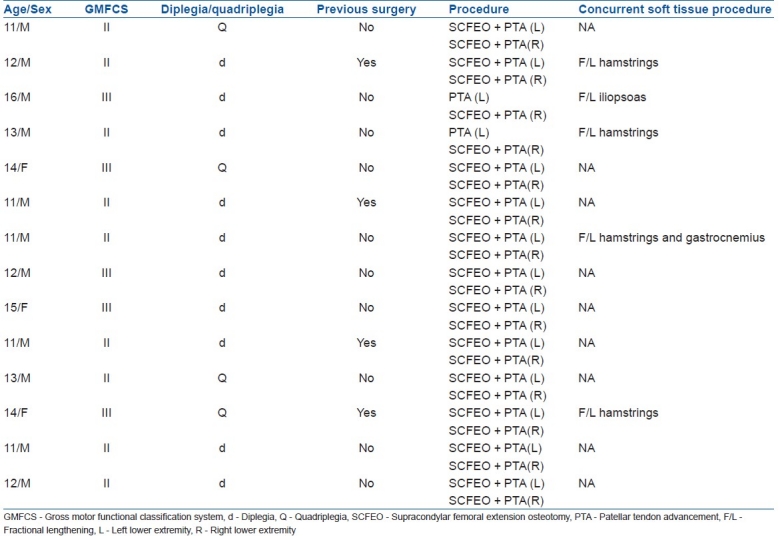
All cases were able to walk with crouch gait with or without assistance. All were able to use both upper limbs. The criteria for selection were: (1) a diagnosis of cerebral palsy; (2) ability to walk without assistance for a minimum distance of 50 m enabling observational gait analysis and Functional Mobility Scale; (3) knee flexion deformity of 15° or higher; (4) Gross Motor Function Classification System (GMFCS) level II or III. Subjects who were not able to comply with postoperative rehabilitation protocol were excluded from the study.
The institutional ethical committee of SVNIRTAR provided ethical clearance before the beginning of study. Written consent was obtained from the primary caregiver/parents/guardians before the patients were enrolled in the study.
Outcome measures
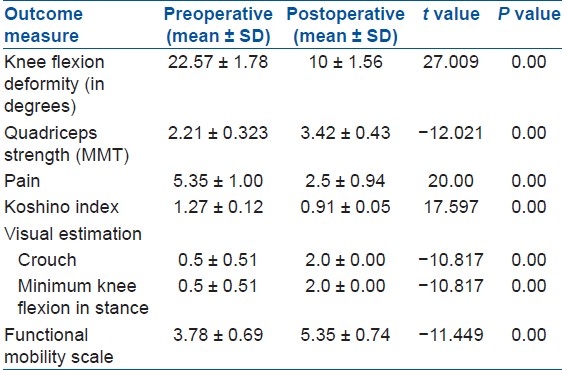
Outcome measures included knee flexion deformity, quadriceps strength, pain, patellar height on lateral knee radiographs using Koshino index, visual estimation of crouch and minimum knee flexion in stance using Physician's rating scale16 and Functional Mobility Scale [Table 2].17]
Table 2.
Outcome measures
Knee flexion deformity
The knee flexion deformity was measured with a 180° goniometer. With the patient lying in prone position and supported till the level of thighs, the static arm of the goniometer was placed parallel to the long axis of thigh, with the fulcrum at the knee joint axis, and the movable arm was then adjusted with reference to the long axis of leg, measuring the flexion deformity of knee. In the two patients with iliopsoas spasticity, the starting position was adjusted to prone knee alleviating any pelvic tilt.
Quadriceps strength
The manual muscle testing (MMT) method devised by McFarland allows strength grading in half grade.18 Although MMT is not a consistent measure of strength in patients with neurological disorders, there have been studies where strength has been measured in MMT.19,20 Subjects were allowed to lean back until tension in the hamstrings was relieved. Thigh was stabilized without pressure over the quadriceps. Subjects were then instructed to extend the knee through the range of motion.
Pain
Horizontal visual analog scale (VAS) was used to measure pain intensity subjectively. It is shown to be valid and sensitive and has a reasonable degree of reproducibility.21,22 Each patient estimated his/her pain level subjectively by moving the pointing device along the uncalibrated scale, between 0 and 10. Then, the exact value of pain intensity was recorded subjectively by referring the uncalibrated scale to the ruler on the back side.
Patellar height by Koshino index
Patellar height was measured on lateral knee radiographs with the method described by Koshino et al.23 It has been shown to be a stable assessment for skeletally immature children. The femur–tibia distance and the patella-tibia distance were measured with the use of the epiphyseal line midpoints of the tibia and femur and the midpoint of the long axis of the patella. The Koshino index is the ratio of patella-tibia to femur-tibia and is dependent upon the knee flexion range. All calculations were made by one of the authors both preoperatively and postoperatively using the latest lateral X-ray.
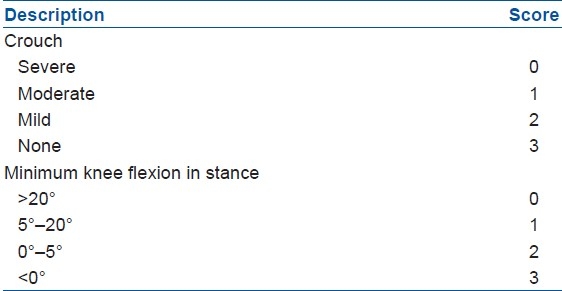
Visual estimation of crouch and minimum knee flexion in stance using Physician Rating Scale of observational gait analysis
Computerized gait analysis is not available in all set ups and it requires specialized equipment and specially trained personnel. The Physician Rating Scale is an observational tool that has been used to evaluate gait. The visual assessment using modified Physician Rating Scale is found to be valid and reliable for assessing crouch and maximum knee extension during stance. Each subject walked a distance of 20 m both pre and post surgery and was videotaped. One of the authors scored each subject for crouch and minimum knee flexion in stance using the Physician Rating Scale [Table 3].
Table 3.
Physican rating scale
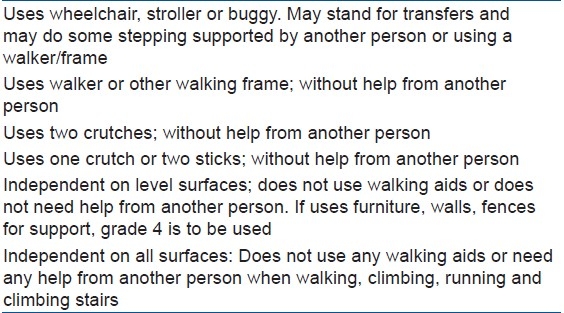
Functional mobility scale
Devised by Graham et al.,17 this scale is found to be useful for discriminating varying levels of functional mobility and is sensitive to detect changes after operative intervention. From the original scale, we evaluated walking for 50 m only and the grading was made in a rating scale of 1–6 [Table 4].
Table 4.
Functional mobility score17
Detailed examination was done and then the subjects were assessed for dependant variables.
Operative procedure and rehabilitation
After giving appropriate anesthesia,24 a tourniquet was applied. The patient was positioned supine and the leg was draped free. Firstly, a No. 5 ethibond suture as a tension band from patella to the tibia to protect the repair was passed. A 3.2 mm drill hole was made transversely in the center of patella and No. 5 ethibond suture was passed on a straight needle in the hole. The suture was taken subcutaneously on both sides of patella [Figure 1]. The patellar tendon detachment was performed by a direct anterior incision in line with the tibial tubercle [Figure 2]. Patellar tendon was exposed and separated from medial and lateral extensor aponeurosis up to its insertion. The tendon was meticulously separated from the cartilaginous tibial tubercle apophysis without damaging it. Four Krackow stitches25 were placed in the patellar tendon. A T-shaped periosteal incision was made just distal to the tibial tubercle apophysis and medial and lateral flaps were elevated.
Figure 1.

Peroperative photograph showing drilling at center of patella for passage of Ethibond No 5
Figure 2.

Peroperative photograph showing detachment of patellar tendon
Then, distal femoral anterior base wedge osteotomy was performed. A 5-cm skin incision was made on antero-lateral surface of supracondylar area. Supracondylar area was exposed after lifting vastus lateralis. Periosteum was incised. The distal osteotomy was done proximal to the physis parallel to the articular surface of tibia, and proximal osteotomy was done perpendicular to the shaft of femur. Apex of osteotomy was posterior and base was anterior in relation to the shaft of femur. Bone wedge was excised and osteotomy was closed and fixed by two 3 mm K-wires on medial and lateral sides of condyles [Figure 3] along with the above knee cast. Anterior aspect of tibia below the tubercle was made rough by an osteotome so that patellar ligament would take a good attachment. The Krackow sutures were tied deeply under the periosteum flaps and periosteal flaps were sewn over the patellar tendon [Figure 4]. No. 5 ethibond suture was passed through a transverse drill hole in the tibia distal to tubercle. The tension suture was then tied between patella and tibia by advancing the patella until the inferior pole of the patella reached the femoro-tibial joint line. The patellar tendon was tightened after releasing the tourniquet to avoid quadriceps laxity. Tourniquet was released and bleeding checked. Drain was applied. The wound was closed in a routine fashion and the above knee cast was applied for 6 weeks.
Figure 3.

Peroperative photograph showing supracondylar osteotomy with K-wire fixtion
Figure 4.

Peroperative photograph showing reattachment of patellar tendon distally
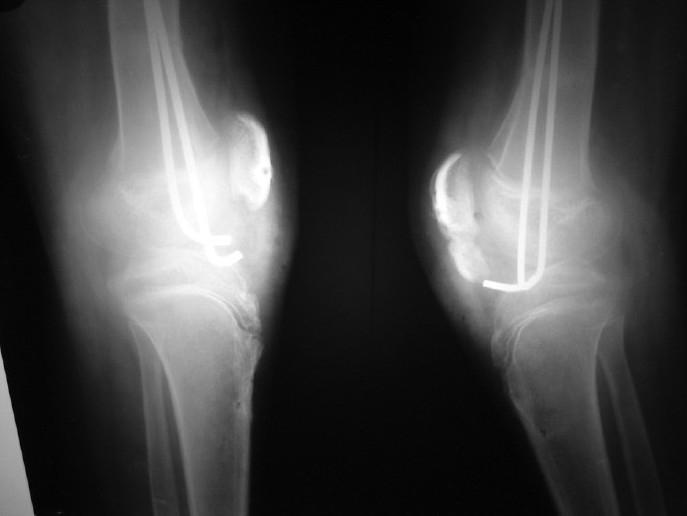
Postoperatively, AP and lateral radiographs were taken to confirm proper alignment and patellar index and compared with preoperative X-rays [Figures 5 and 6]. The knee cast was removed after 6 weeks, and quadriceps strengthening, active range of motion and weight bearing were initiated. Postoperative physiotherapy was performed in our institution. The postoperative physiotherapy protocol followed was as follows:
Figure 5.
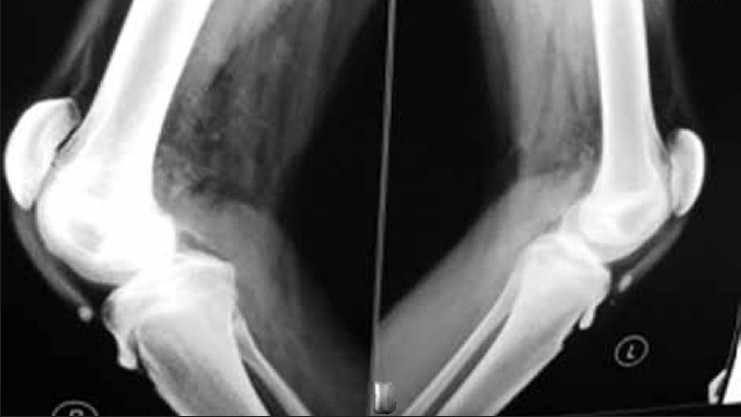
Preoperative X-ray of both knee joints (lateral view) showing deformity
Figure 6.
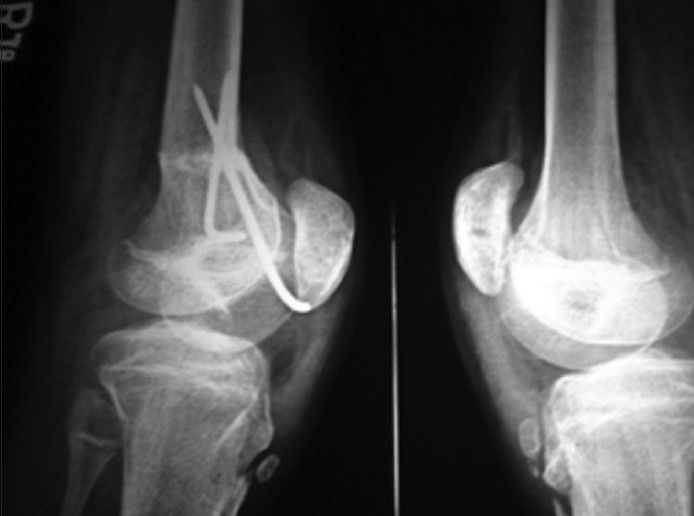
Postoperative X-ray (lateral view) showing k-wires in situ with deformity correction
No passive range of motion was allowed till 8 weeks. Active range of motion to full extension and 60°–90° of knee flexion was continued till 2 weeks. No weight bearing was permitted till 12 weeks. Isometrics to quadriceps in supine and knee in full extension was started at 2 weeks. By 4–8 weeks active range of motion greater than 90° and active and active-assisted range of motion in flexion and extension were allowed. Isometric exercises to quadriceps and hamstrings were initiated. Between 8–12 weeks active, active-assistive, passive range of motion, Isometric and isotonic exercises to quadriceps and hamstrings were performed. Active and passive range of motion emphasizing terminal extension/isometric, isotonic exercises to hamstrings and quadriceps were started between 12–16 weeks progressing to resistance exercises. Weight bearing was allowed: Toe touch to partial weight bearing progressing to full weight bearing.
All the statistical analyses were performed using paired “t” test to assess the significance of changes from before to after surgery. Statistical significance experiment wise was set up at 95% confidence interval. SPSS version 16 was used for statistical analysis.
RESULTS
The overall results of the study showed significant improvement in all the dependant variables after the surgery and rehabilitation. The primary outcome measures are knee flexion deformity, Koshino index and Functional Mobility Scale.
Knee flexion deformity
There was a significant improvement in the knee flexion deformity post surgery [Figures 7 and 8, [Graph 1]. Paired t test showed significance at P<0.005.
Figure 7.

Preoperative clinical photograph shows crouch gait
Figure 8.

Postoperative clinical photograph shows correction of flexion deformity
Graph 1.
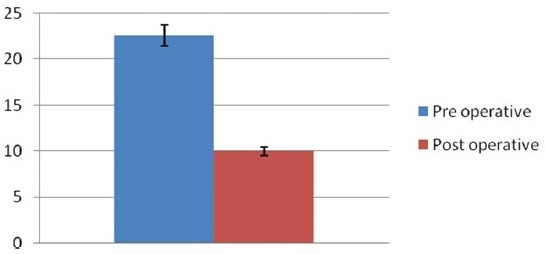
Bar diagram showing preoperative and Postoperative changes in knee flexion deformity
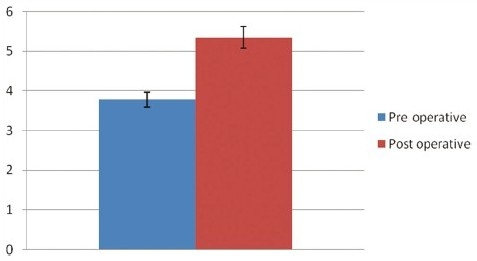
Quadriceps strength
The quadriceps showed improved strength post surgery [Table 2, Graph 2]. Paired t test showed significance at P<0.005.
Graph 2.
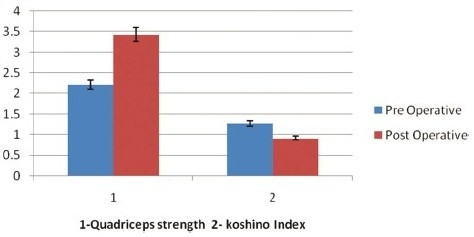
Bar diagram showing preoperative and postoperative changes in quadriceps strength and Koshino index
Koshino index
There was a significant difference in the patellar height post surgery [Table 2, Graph 2]. Paired t test showed significance at P<0.005. All osteotomies united within 6–8 weeks.
Pain
There was a statistically significant reduction in pain post surgery [Table 2, Graph 3]. Paired t test showed significance at P<0.005.
Graph 3.
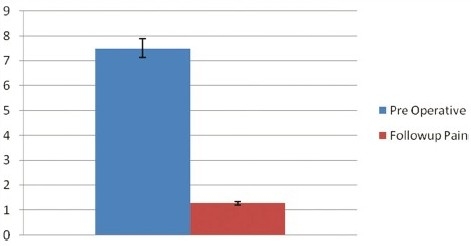
Bar diagram showing preoperative and postoperative improvement in pain
Visual estimation of crouch and minimum knee flexion in stance
The visual estimation of crouch and minimum knee flexion in stance improved with surgery [Table 2, Graph 4]. Paired t test showed significance at P<0.005.
Graph 4.
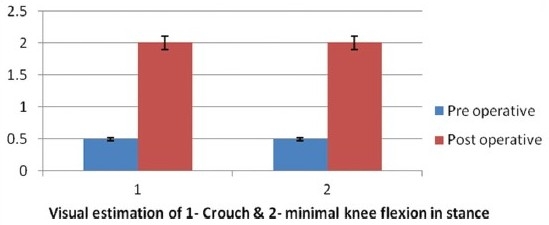
Bar diagram showing preoperative and postoperative improvement in visual estimation of crouch and minimum knee flexion in stance
Functional mobility scale
There was a significant improvement in the Functional Mobility Scale after the surgery [Table 2, Graph 5]. Paired t test showed significance at P<0.005.
Graph 5.
Bar diagram showing preoperative and postoperative improvement in functional mobility scale
Neurapraxia (n=1) irritation of K-wire to skin (n=2) avulsion fracture of patella (n=1) [Figure 9] preventing mobilization were found as complications. Neurapraxia was temporary and improved with gabapentin. Irritating K-wires were removed after union.
Figure 9.
Post operative X-ray showing union of avulsion fracture of patella
DISCUSSION
The crouch gait has been defined as hip flexion, knee flexion and ankle calcaneus.7 Crouch gait is marked by excessive knee flexion in both swing and stance.10,11 Limb advancement is attenuated as part of this crouch pattern. Both hamstring and quadriceps muscles may be involved. Kinesiologic EMG may demonstrate prolonged activity of the medial hamstrings. Knee flexion contracture is common.
Rate of recurrence of knee flexion contracture is 32% without concomitant correction of patella alta.12 Progressive crouch gait often develops rapidly around pubertal growth due to weakness of muscles of lower limb, unfavorable body mass to strength ratio and the development of musculoskeletal deformities referred to as lever arm deformities.26
Detrimental effects of crouch gait in the long term are patella alta,27 anterior knee pain,28,29 avulsion of distal pole of patella,30–32 cosmetically unacceptable gait, high energy consumption and ultimately limiting ambulatory endurance.3,27,28,30,33
Crouch gait may lead to the contracture of two joint muscles around hip and knee (psoas, hamstrings, rectus femoris and gastrocnemius) and elongation of one joint muscle (gluteus maximus, quadriceps, soleus) occurs. Further growth leads to posterior capsular contracture and extension lag. The persistent crouch patterning seen in patients after soft tissue release may be due to severity of posterior capsular contracture around knee and by the insufficient capacity of the hip extensors, knee extensors or ankle plantar flexors to accelerate the limb into extension. Abnormal forces generated by tight iliopsoas or spastic gastrocnemius may also contribute to crouch gait as these muscles have the capacity to accelerate the hip and knee into flexion. SCFEO with PTA in a single stage was selected as the operative procedure to overcome both these problems of knee flexion contracture and reduced quadriceps force production, and thereby restore the upright posture.
The improvement in the muscle strength post surgery may be hypothesized to the PTA surgery increasing the mechanical efficiency of quadriceps mechanism. The reduction in pain after surgery may be contributed to the increment in quadriceps strength, more extended knee joint and the reduction in the patello femoral compressive forces across the knee joint. The improvement in the Functional Mobility Scale may be due to the reduction of pain, as knee pain has been mentioned as one of the primary factors that limits the walking ability of these patients.34,35
Though the results of the study showed an improvement in the outcome measures post surgery, none of the subjects had full correction of knee flexion deformity and no single subject was graded with a score of 3 in visual observation of crouch and minimum knee flexion in stance in Physician Rating Scale, showing that crouch gait was not fully correctable in this study. This may be explained with EMG studies on crouch gait. EMG analysis has shown that the gluteus maximus, and the soleus, in addition to the vasti make substantial contributions to knee extension during the stance phase of normal gait.4 In fact, per unit force, the gluteus maximus has greater potential than the vasti to accelerate the knee toward extension. The gluteus maximus, vasti, and the soleus also help to generate normal hip extension. These data suggest that excessive hip and knee flexion of persons with crouch gait may be caused by insufficient capacity of the hip extensors, knee extensors, or ankle plantar flexors to accelerate the limb into extension.
Limitations
We do accept the fact that the study done was not a randomized controlled trial (RCT) and the sample size was less. All calculations were made at 95% confidence level. With a confidence interval of 10%, the sample size comes to 96. We recommend that the same study be repeated with a larger sample size. However it is very difficult to get that a huge population fitting the inclusion criteria. We have not used EMG gait analyzer to evaluate gait and identify the abnormality at the hip and ankle kinetics. The gluteus maximus strength was not measured and long term followup was not done to prove crouch gait did not reoccur post adolescent, and these were the major limiting factors.
The results of the study suggest that SCFEO and PTA is a useful intervention in the management of adolescent crouch gait. Knee function and level of walking improved after surgery and the technique has been found to be safe and effective.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Hicks JL, Schwartz MH, Arnold AS, Delp SL. Crouched postures reduce the capacity of muscles to extend the hip and knee during single-limb stance of gait. J Biomech. 2008;41:960–7. doi: 10.1016/j.jbiomech.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gage JR, editor. The treatment of gait problems in cerebral palsy. 2nd ed. London: Mac Keith press; 2004. pp. 382–9. [Google Scholar]
- 3.Perry J, Uewsam C. Function of the hamstrings in cerebral palsy. In: Sussman MD, editor. Diplegic Child: Evaluation and Management. Rosemont, 111: Am Acad Orthop Surg; 1992. pp. 299–308. [Google Scholar]
- 4.Arnold S, Anderson C, Pandy G, Delp L. Muscle actions during the stance phase of the normal gait (internet) [Last accessed on 2010 Sep 08]. Available from: http://www.gait.aidi.udel.edu/gaitlab/gcma/info/abstracts/o21.abs20092.pdf .
- 5.Keats S, Kambin P. An evaluation of surgery for the correction of knee flexion contracture in children with cerebral spastic paralysis. J Bone Joint Surg Am. 1962;44:1146–51. [Google Scholar]
- 6.Hoffinger SA. Hamstrings in cerebral palsy crouch gait. J Pediatr Orthop. 1993;13:722–6. doi: 10.1097/01241398-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Rodda JM, Graham HK, Nattrass GR, Galea MP, Baker R, Wolfe R. Correction of severe crouch gait in patients with spastic diplegia with use of multilevel orthopaedic surgery. J Bone Joint Surg Am. 2006;88(12):2653–64. doi: 10.2106/JBJS.E.00993. [DOI] [PubMed] [Google Scholar]
- 8.Straps CH. A long term retrospective study of proximal hamstrings release for hamstring contracure in cerebral palsy. J Pediatr Orthop. 1984;4:443–7. doi: 10.1097/01241398-198408000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Sutherland DH, Cooper L. The pathomechanics of progressive crouch gait in spastic diplegia. Orthop Clin North Am. 1978;9:143–54. [PubMed] [Google Scholar]
- 10.Kim YJ, Noonan KJ. What's new in paediatrics orthopaedics. J Bone Joint Surg Am. 2010;92:1575–82. doi: 10.2106/JBJS.J.00267. [DOI] [PubMed] [Google Scholar]
- 11.Graham HK. Classifying cerebral palsy. J Pediatr Orthop. 2005;25:127–8. doi: 10.1097/00004694-200501000-00026. [DOI] [PubMed] [Google Scholar]
- 12.Stout JL, Gage JR, Schwartz MH, Novacheck TF. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J Bone Joint Surg Am. 2008;90:2470–84. doi: 10.2106/JBJS.G.00327. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd-Roberts GC, Jackson AM, Albert JS. Avulsion of the distal pole of the patella in cerebral palsy, A cause of deteriorating gait. J Bone Joint Surg Br. 1985;67:252–4. doi: 10.1302/0301-620X.67B2.3980536. [DOI] [PubMed] [Google Scholar]
- 14.Asirvatham R, Mukherjee A, Agarwal S, Rooney RJ, Ellis RD, Watts HG. Supracondylar femoral extension osteotomy and its complications. J Pediatr Orthop. 1993;13:642–5. [PubMed] [Google Scholar]
- 15.Roberts WM, Adams JP. The patellar advancement operation in cerebral palsy. J Bone Joint Surg Am. 1953;4:958–66. [PubMed] [Google Scholar]
- 16.Wren TA, Rethlefsen SA, Healy BS, Do KP, Dennis SW, Kay RM. Reliability and validity of visual assessments of gait using a modified physician rating scale for crouch and foot contact. J Pediatr Orthop. 2005;25:646–50. doi: 10.1097/01.mph.0000165139.68615.e4. [DOI] [PubMed] [Google Scholar]
- 17.Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The Functional mobility scale (FMS) J Pediatr Orthop. 2004;24:514–24. doi: 10.1097/00004694-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Mcfarland G, Kim TK. Examination of the Shoulder: The Complete guide. Thieme Medical. 2006 [Google Scholar]
- 19.Gul SM, Steinbok P, McLeod K. Long-term outcome after selective posterior rhizotomy in children with spastic cerebral palsy. Pediatr Neurosurg. 1999;31:84–95. doi: 10.1159/000028839. [DOI] [PubMed] [Google Scholar]
- 20.Novacheck TF, Stout JL, Gage JR, Schwartz MH. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy. J Bone Joint Surg Am. 2008;90:2470–84. doi: 10.2106/JBJS.G.00327. [DOI] [PubMed] [Google Scholar]
- 21.Revill SI, Robinson JO, Rosen M, Hogg MI. The reliability of a linear analogue for evaluating pain. Anaesthesia. 1976;31:1191–8. doi: 10.1111/j.1365-2044.1976.tb11971.x. [DOI] [PubMed] [Google Scholar]
- 22.Murrin KR, Rosen M. Pain measurement. In: Smith G, Govindo BG, editors. Acute pain. London: Butterworth; 1985. [Google Scholar]
- 23.Koshino T, Sugimoto K. New measurement of patellar height in the knees of children using the epiphysial line midpoint. J Pediatr Orthop. 1989;9:216–8. [PubMed] [Google Scholar]
- 24.Novacheck TF, Stout JL, Gage JR, Schwartz MH. Distal femoral extension osteotomy and patellar tendon advancement to treat persistent crouch gait in cerebral palsy-Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):271–86. doi: 10.2106/JBJS.I.00316. [DOI] [PubMed] [Google Scholar]
- 25.Krackow KA, Thomas SC, Jones LC. A new stitch for ligament tendon fixation. J Bone Joint Surg Am. 1986;68:764–6. [PubMed] [Google Scholar]
- 26.Leong JC, Alade CO, Fang D. Supracondylar femoral osteotomy for knee flexion contracture resulting from poliomyelitis. J Bone Joint Surg Br. 1982;64:198–201. doi: 10.1302/0301-620X.64B2.7068740. [DOI] [PubMed] [Google Scholar]
- 27.Koman LA, Smith BP, Shilt JS. Lancet. 2004;363(9421):1619–31. doi: 10.1016/S0140-6736(04)16207-7. [DOI] [PubMed] [Google Scholar]
- 28.Eggers GW. Transplantation of hamstrings tendon in femoral condyles in order to improve hip extension and to decrease knee flexion in cerebral spastic paralysis. J Bone Joint Surg Am. 1952;34:827–30. [PubMed] [Google Scholar]
- 29.Senaran H, Holden C, Dabney KW, Miller F. Anterior knee pain in children with cerebral palsy. J Pediatr Orthop. 2007;1:12–6. doi: 10.1097/BPO.0b013e31802b715c. [DOI] [PubMed] [Google Scholar]
- 30.Thomson James EM. A comparative study of the relative value of various surgical procedures in the treatment of infantile paralysis of the lower extremity. J Bone Joint Surg Am. 1924;6:627–63. [Google Scholar]
- 31.Lotman DB. Knee flexion deformity and patella alta in spastic cerebral palsy ;18:315-9. Dev Med Child Neurol. 1976;18:315–9. doi: 10.1111/j.1469-8749.1976.tb03653.x. [DOI] [PubMed] [Google Scholar]
- 32.Rosenthal RK, Levine DB. Fragmentation of the distal pole of the patella in spastic cerebral palsy. J Bone Joint Surg Am. 1977;59:934–9. [PubMed] [Google Scholar]
- 33.Topoleski TA, Kurtz CA, Grogan DP. Radiographic abnormalities and clinical symptoms associated with patella alta in ambulatory children with cerebral palsy. J Pediatr Orthop. 2000;20:636–9. doi: 10.1097/00004694-200009000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Andersson C, Mattsson E. Adults with cerebral palsy; A survey describing problems, needs, and resources, with special emphasis on locomotion. Dev Med Child Neurol. 2001;43:76–82. doi: 10.1017/s0012162201. [DOI] [PubMed] [Google Scholar]
- 35.Murphy KP, Molnar GE, Lankasky K. Medical and functional status of adults with cerebral palsy. Dev Med Child Neurol. 1995;37:1075–84. doi: 10.1111/j.1469-8749.1995.tb11968.x. [DOI] [PubMed] [Google Scholar]


