Abstract
Fungal infections are one of the important cause of morbidity and mortality in immunocompromised patients. Aspergillus vertebral osteomyelitis is extremely rare. We report two cases of aspergillus vertebral osteomyelitis in immunocompetent men in the absence of an underlying disorder. The clinical and radiological findings were suggestive of Pott's spine. The absolute CD4, CD8 counts and their ratio were normal. The HIV status was negative in both patients. Both patients underwent surgical decompression. The histopathology of tissue obtained were suggestive of aspergillus osteomyelitis. One patient had antifungal treatment for 3 months and was doing well at 1 year followup, whereas other patient did not turnup after 2 months.
Keywords: Aspergillus, immunocompetent, osteomyelitis, vertebrae
INTRODUCTION
Immunocompromised patients are at a high risk of invasive fungal infection associated with high morbidity.1 Among the fungi, Candida is the most common organism causing infection in neutropenics or after organ transplantation.2 Musculoskeletal involvement, especially vertebrae and intervertabral disc space, is uncommon. Still rarer is aspergillus vertebral osteomyelitis3 and only few case reports of this disease have been described in literature occurring in immunocompetent men.3,4
CASE REPORTS
Case 1
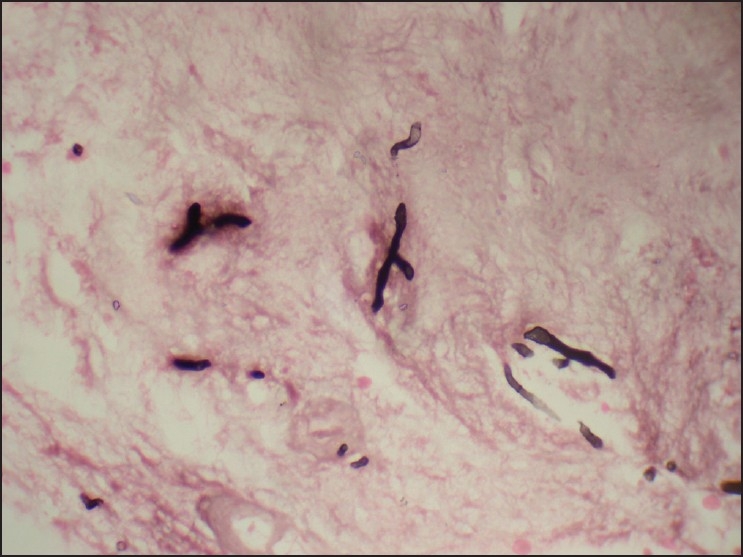
A 25-year-old man, hailing from Bihar and working in a multinational company, presented with pain in lower back since last 6 months, which was dull aching, nonradiating, and relieved by rest. Pain gradually increased in intensity associated with decrease in walking distance. He had fever in the initial days, which later resolved with medication. He had lost 6-7 kg weight in the last six months. No foray into forested area or residence in neighborhood jungle were observed. Physical examination was unremarkable except for tenderness present over the spine in lower lumbar region (L2-L5). No gross spinal deformity was seen. There was no neural deficit. He was diagnosed as having Pott's spine and was taking antitubercular treatment, prescribed by referral hospital; however, no improvement was noted in the patient. General and systemic evaluation revealed no manifestation of acquired immunodeficiency syndrome (AIDS) or any underlying immunosuppressive disorder. The CD4:CD8 ratio was normal and HIV status was negative. Chest radiographs revealed no pulmonary lesion and sputum culture was negative for acid-fast bacilli (AFB). X-ray of the spine revealed lytic lesion in the L4-L5 vertebral region [Figure 1]. Magnetic resonance imaging (MRI) of the spine revealed destruction of L4-L5 vertebrae, with abscess formation and cauda equina compression [Figure 2]. He underwent L4-L5 instrumentation, with posterior decompression and interbody fusion with tricortical bone graft from the iliac crest [Figure 3]. Direct fluorescence for AFB was negative and the culture and sensitivity for AFB and pyogenic organism were also negative. Fungal culture was not attempted. The biopsy tissue was received in multiple fragments together measuring 4 × 3 × 1 cm. Microscopy revealed fibrocollagenous tissue, normal, necrotic and new bone, degenerated cartilage, and dense inflammatory infiltrate composed of lymphocytes, plasma cells, histiocytes, few eosinophils, polymorphs, and several granulomas containing giant cells [Figure 4a and b]. Numerous fungal profiles were seen in the granulation tissue, which were septate and showed acute angle branching. These hyphae were highlighted by modified Gomori Methenamine stain [Figure 4c]. After the diagnosis of fungal osteomyelitis, the patient was started on itraconazole 200 mg twice a day for 3 months. At 1 year followup, he was doing well with no complaints of back pain.
Figure 1.

X-ray of lumbar spine (Lateral view) depicting lytic lesion in the L4-L5 region
Figure 2.
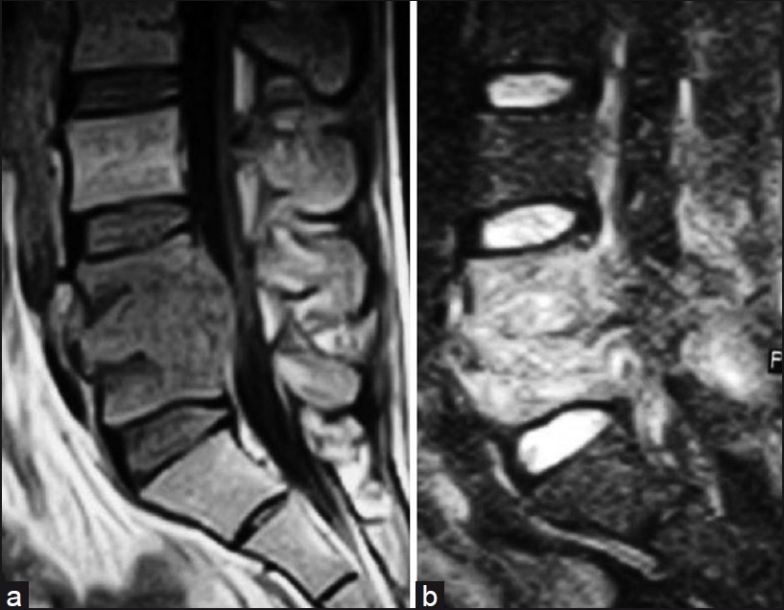
(a) T1WI sagittal MR image showing L4 and L5 vertebral body with intervertebral disc involvement. (b) T2WI showing L4 and L5 vertebral body hyperintensity with intervertebral disc involvement
Figure 3.
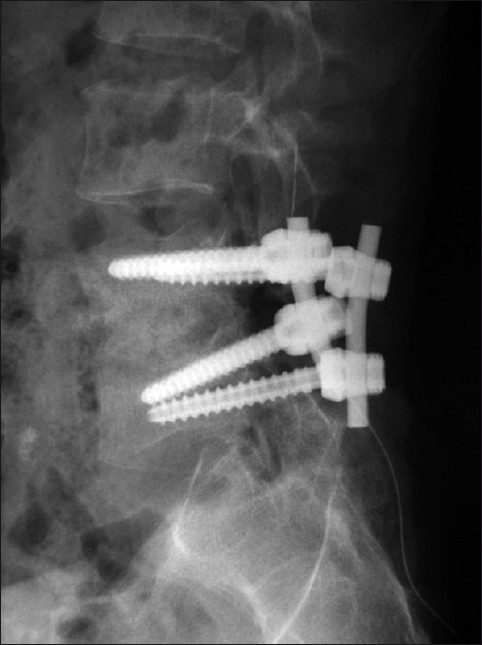
Posterior instrumented interbody fusion (L4-L5) with autogenous bone grafting
Figure 4.
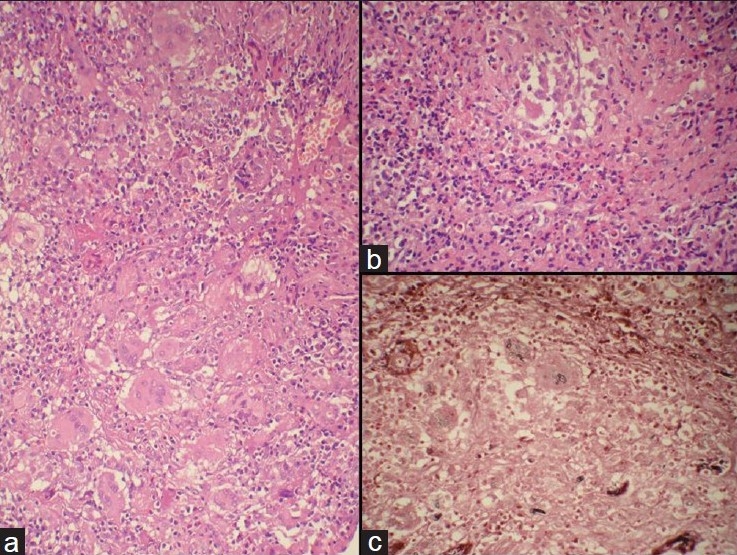
Photomicrograph showing (a) ill-formed granulomas with many giant cells (H and E, ×200). (b) Inflammatory infiltrate comprising numerous eosinophils and ill-formed granuloma (H and E, ×400). (c) Gomori Methenamine Stain showing septate and acute angle branching fungal hyphae and few spores in the giant cells (GMS, ×400)
Case 2
A 19-year-old college student was apparently healthy 9 months ago, when he developed pain in the midback, which radiated to both the flanks and had difficulty in walking. Pain gradually increased with bending, walking, or any movement and was relieved by rest and medication. Three days after the pain he noticed a swelling in the midback region, which was increasing continuously. No impairment in motor, sensory, bladder, and bowel function was seen. He was diagnosed clinically as having Pott's spine by the referral hospital. No foray into forested area or residence in neighborhood jungle were observed. Physical examination was unremarkable, except for mild tenderness and gibbus formation at the D10-D11 vertebral level. General and systemic examination in this patient also did not reveal any manifestation of AIDS or any underlying immunosuppressive disorder. The CD4:CD8 ratio was normal and HIV status was negative. Chest X-ray was within normal limits. X-ray/MRI of the spine showed D10-D11 vertebral collapse with kyphosis and cord compression. The patient underwent transthoracic D10-D11 corpectomy and fusion with D9-D12 expandable cage with staple and rod fixation. Biopsy tissue revealed fragments of normal and necrotic bone with extensive and diffuse necrosis and numerous surrounding eosinophils [Figure 5]. Grocott's Methenamine Silver (GMS) stain revealed numerous septate and branching fungal profiles having morphological features of Aspergillus species [Figure 6]. Direct fluorescence and Ziehl Nelson stain for AFB was negative in the patient. Culture and sensitivity for AFB and pyogenic organism were also negative. The patient was postoperatively started on anti-fungal treatment (Itraconazole 200 mg BD) for 2 months; however, no followup was available in this case.
Figure 5.
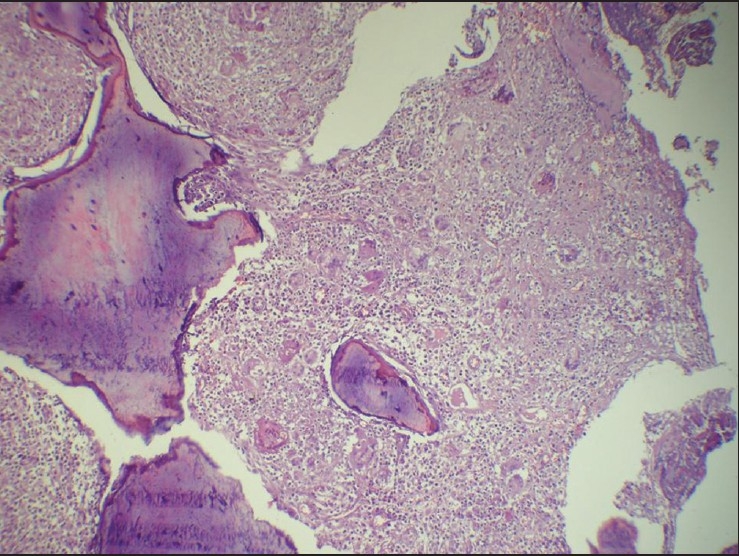
Photomicrograph showing necrotic bony trabaeculae with giant cell reaction in marrow spaces (H and E, ×4)
Figure 6.
GMS stain showing narrow and acute angle branching fungal hyphae consistent with Aspergillus (GMS, ×1000)
DISCUSSION
Staphylococcus aureus, accounts for 60% of pyogenic vertebral osteomyelitis.5 Other causes of spinal infection include Mycobacterium tuberculosis, and rarely fungi. The rate of occurrence of fungal infections has risen over the last decade, as the population of immunocompromised patients has increased. The diagnosis and treatment of fungal infection of the spine is often delayed, as clinical suspicion is often low, particularly in immunocompetent individuals.6
The most common organism causing mycotic infections are Candida and, rarely, Aspergillus. These infections mainly present as discitis or osteomyelitis in the spine.7 Most reviews of fungal spinal infections have included a limited number of patients and short followup. In a study by Eismont et al.,2 of 65 cases of spondylitis were caused by fungal organisms.8 Fungal organisms are slow growing and difficult to identify by culture. Therefore, histopathological examination is important to obtain correct diagnosis.6
The deficiency in the immune system secondary to infection with the human immunodeficiency virus, the widespread and injudicious use of broad-spectrum antibiotics, the use of corticosteroids and other immunosuppresive drugs, and the use of parenteral hyperalimentation are listed as risk factors for fungal infection.2,5,7,8
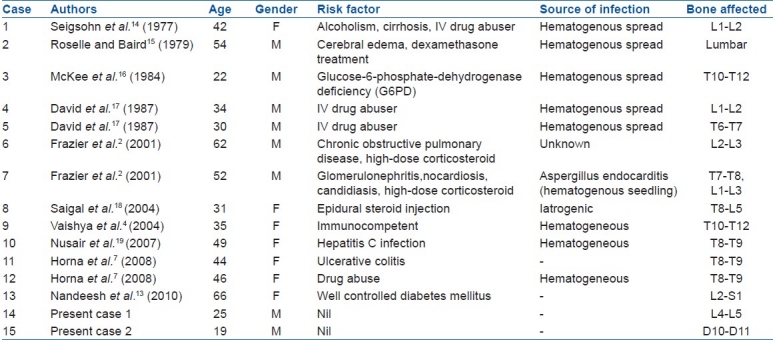
In the series by Frazier, 9 of 11 patients with spinal osteomyelitis were immunocompromised and 7 had infection due to Candida.2 Spinal infection by Aspergillus is uncommon.9,10 Aspergillus species are ubiquitous saprophytic organisms. More than 300 species are known, but only a few of them are of importance regarding opportunistic infection. Invasive aspergillosis (IA) usually involves the sinopulmonary tract, with the lung being the most common site of infection, while osteomyelitis due to Aspergillus species is rare.11 It affects bone tissues by contiguity, hematogenous spread, and direct implantation, eg, traumatic or iatrogenic. The incidence of Aspergillus affecting the bone among all cases of invasive aspergillosis (IA) is estimated to be 3%.11 In a series by Horn, the incidence of IA was 2.6%, similar to those reported by Denning and Steven in 1990.7,12 Nandeesh et al. described less than 50 cases with spinal aspergillus osteomyelitis, and most of these patients were immunocompromised.13 A comprehensive literature search yielded approximately 15 cases of aspergillus osteomyelitis affecting the spine in immunocompetent young adults without any underlying disorders, including the present 2 cases [Table 1]. Aspergillus spinal osteomyelitis cases have a bimodal age distribution pattern; children with chronic granulomatous disease and the older adults with other underlying disorder. Back pain is an almost universal initial symptom of vertebral osteomyelitis caused by Aspergillus species. Unfortunately, some patients have also presented with paraparesis.20
Table 1.
Reported cases of Aspergillus vertebral osteomyelitis in immunocompetent patients
Spinal osteomyelitis forming abscess and causing compressive myelopathy is not common, and current literature is largely limited to case reports only. Typical complications of spinal osteomyelitis include osteolytic destruction of body endplates, paravertebral soft tissue swelling, disc space narrowing, and spinal cord compression.11 The overall 12-week mortality among the patient with aspergillus osteomyelitis was 25%.7
Choice of treatment in fungal infection, especially aspergillus osteomyelitis, is debridement of necrotic bone in addition to the use of antifungal like Voriconazole, Itraconazole, Amphotericin B, and, possibly, 5-Fluorocytosine or Rifampin.7,10 In advanced cases, antimycotic drug therapy may not be effective and emergency surgical debridement may be indicated when the destruction is progressive and spinal cord compression is imminent or manifest. In such cases, spinal instrumentation can help maintain and restore spinal stability and spinal alignment.10
Aspergillus vertebral osteomyelitis and abscess is a rare cause of compressive myelopathy. It closely mimics tubercular spine disease and presents with similar clinical features. Early definitive diagnosis remains a challenge and requires a high index of suspicion. Antifungal drugs in combination with surgery, is indicated in treatment of aspergillus osteomyelitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Vinas FC, King PK, Diaz FG. Spinal aspergillus osteomyelitis. Clin Infect Dis. 1999;28:1223–9. doi: 10.1086/514774. [DOI] [PubMed] [Google Scholar]
- 2.Frazier DD, Campbell DR, Garvey TA, Wiesel S, Bohlman HH, Eismont FJ. Fungal infections of spine.Report of eleven patients with long term follow up. J Bone Joint Surg Am. 2001;83:560–5. [PubMed] [Google Scholar]
- 3.Govender S, Rajoo R, Goga IE, Charles RW. Aspergillus osteomyelitis of the spine. Spine (Phila Pa 1976) 1991;16:746–9. doi: 10.1097/00007632-199107000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Vaishya S, Sharma MS. Spinal aspergillus vertebral osteomyelitis with extradural abscess: Case report and review of literature. Surg Neurol. 2004;61:551–5. doi: 10.1016/j.surneu.2003.06.005. [DOI] [PubMed] [Google Scholar]
- 5.Williams RL, Fukui MB, Meltzer CC, Swarnkar A, Johnson DW, Welch W. Fungal spinal osteomyelitis in the immunocompromised patient: MR findings in three cases. AJNR Am J Neuroradiol. 1999;20:381–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Yau E LK, Li KK. Concomitant fungal and bacterial atlanto-axial osteomyelitis: A case report. J Orthop Surg (Hong Kong) 2010;18:241–3. doi: 10.1177/230949901001800221. [DOI] [PubMed] [Google Scholar]
- 7.Horna D, Tiaa SS, Neofytosa D. Aspergillus osteomyelitis: review of 12 cases identified by the prospective antifungal therapy alliance registry. Diagn Microbiol Infect Dis. 2009;63:384–7. doi: 10.1016/j.diagmicrobio.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA. Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am. 1983;65:19–29. [PubMed] [Google Scholar]
- 9.Tew CW, Han FC, Jureen R, Tey BH. Aspergillus vertebral osteomyelitis and epidural abscess. Singapore Med J. 2009;50:e151–4. [PubMed] [Google Scholar]
- 10.Ranjan R, Mishra S, Ranjan S. Aspergillus vertebral osteomyelitis in an immunocompetent person. Neurol India. 2010;58:806–8. doi: 10.4103/0028-3886.72196. [DOI] [PubMed] [Google Scholar]
- 11.Winterstein AR, Bohndrof K, Vollert K, Wagner T, Gnekow A, Roemer FW. Invasive aspergillosis osteomyelitis in children-a case report and review of literature. Skeletal Radiol. 2010;39:827–31. doi: 10.1007/s00256-010-0967-4. [DOI] [PubMed] [Google Scholar]
- 12.Denning DW, Stevens DA. Antifungal and surgical treatmnent of invasive aspergillosis: Review of 2121 published cases. Rev Infect Dis. 1990;12:1147–201. doi: 10.1093/clinids/12.6.1147. [DOI] [PubMed] [Google Scholar]
- 13.Nandeesh BN, Kini U, Alexander B. Vertebral osteomyelitis with a rare etiology diagnosed by fine-needle aspiration cytology. Diagn Cytopathol. 2010;38:360–3. doi: 10.1002/dc.21212. [DOI] [PubMed] [Google Scholar]
- 14.Seligsohn R, Rippon JW, Lerner SA. Aspergillus terreus osteomyelitis. Arch Intern Med. 1977;137:918–20. [PubMed] [Google Scholar]
- 15.Roselle GA, Baird IM. Aspergillus flavipes group osteomyelitis. Arch Intern Med. 1979;139:590–2. [PubMed] [Google Scholar]
- 16.McKee DF, Barr WM, Bryan CS, Lunceford EM., Jr Primary aspergillosis of the spine mimicking Pott's paraplegia. J Bone Joint Surg Am. 1984;66:1481–3. [PubMed] [Google Scholar]
- 17.Brown DL, Musher DM, Taffet GE. Hematogenously acquired aspergillus vertebral osteomyelitis in seemingly immunocompetent drug addicts. West J Med. 1987;147:84–5. [PMC free article] [PubMed] [Google Scholar]
- 18.Saigal G, Donovan Post MJ, Kozic D. Thoracic intrdural aspergtillus abscess formation following epidural steroid injection. AJNR Am J Neuroradiol. 2004;25:642–4. [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmad N, Philip SM. Aspergillus vertebral osteomyelitis in an immunocompetent host treated with voriconazole. Infect Dis Clin Pract. 2007;15:122–4. [Google Scholar]
- 20.Paterson DL. New clinical presentations of invasive aspergillosis in non-conventional hosts. Clin Microbiol Infect. 2004;10:24–30. doi: 10.1111/j.1470-9465.2004.00840.x. [DOI] [PubMed] [Google Scholar]


