Abstract
Deng, Bingjun, Tingguang Luo, Yanfei Huang, Tianhang Shen, Jing Ma. Prevalence and determinants of hyperlipidemia in moderate altitude areas of the Yunnan-Kweichow Plateau in Southwestern China. High Alt. Med. Biol. 13:13–21.—The objective of the current study was to determine the prevalence and determinants of hyperlipidemia among the populations living at moderate altitude on the Yunnan-Kweichow Plateau in Southwestern China. We randomly recruited 1415 people for this study. These subjects underwent a physical examination and a comprehensive questionnaire regarding their daily habits and diets. Furthermore, blood samples from the participants were collected for assessing the lipid profile. We found that 49.3% of participants (95% CI: 46.7–51.9%) suffered from hyperlipidemia. The prevalence in men was significantly higher than that in women (53.6% vs. 44.7%, p<0.01). The prevalence of hypercholesterolemia was 23.3% and of hypertriglyceridemia was 34.1%. Low HDL-C showed a prevalence of 17.5% and high LDL-C of 9.0%. The prevalence of hyperlipidemia also increased with age, as did the prevalence of high TC, TG, and LDL-C. Hyperlipidemic subjects tended to be older and have a higher BMI and WHR than the normolipidemic subjects in the study cohort (p<0.05). The hyperlipidemic subjects, both men and women, tended to dine out often and consume more animal-based foods and alcohol. In addition, the hyperlipidemic men in our cohort consumed more salted food then their normolipidemic counterparts (p<0.01). Normolipidemic subjects of both sexes were also found to prefer a vegetarian diet (p<0.01). Age, alcohol consumption, a preference for meat and animal products, regular dining out, and BMI were found to be the main determinants of hyperlipidemia in women, whereas a prevalence of salted food was observed to be related to hyperlipidemia in men from the Yunnan-Kweichow Plateau subpopulation under study (p<0.05). The average daily energy, and protein and fat intakes of the sampled subjects were also higher than the levels set by the Chinese Recommendation Nutrient Intakes (RNI), while hyperlipidemic subjects had an even higher average daily intake of total fat, cholesterol, and lower dietary fiber compared with the normolipidemic subjects in the study group (p<0.05). In conclusion, this study reveals a higher prevalence of hyperlipidemia, hypercholesterolemia, hypertriglyceridemia, increased BMI and WHR values in men, as well as a slightly higher prevalence of low HDL-C and high LDL-C in women from Yunnan-Kweichow Plateau. The incidence of hyperlipidemia also increased with age, as did the prevalence of an abnormal TC, TG, LDL-C, and WHR in our study cohort. A high BMI, and less healthy living habits and dietary preferences thus play significant roles in the onset of hyperlipidemia.
Key Words: hyperlipidemia, moderate altitude, lifestyle, dietary pattern
Introduction
Cardiovascular disease (CVD) has become the most common cause of mortality in many countries in recent decades. Coronary heart disease (CHD) is therefore the most frequent cause of morbidity, mortality, and loss of potentially functional life years (Mohanna et al., 2006). In China, from 1980 to 2000, the mortality associated with CHD increased from 386 to 713 per million in urban areas, and from 186 to 316 per million in rural areas, and approximately 3.8 million Chinese people suffered from CHD in 1991 (Wu et al., 2003). Among the various risk factors, and as a component of metabolic syndrome, hyperlipidemia plays an important role in the onset and progression of CHD. Changes in the serum lipoprotein profile are associated with an altered risk of CHD (i.e.,+1% cholesterol,+2%–3% risk;+1% LDL-C,+1.2%–2.0% risk; −1% HDL-C,+3% risk) (Anderson et al., 2001). Results from recent trials have also shown that premature death and disability from CHD can be decreased by increasing the number and type of patients receiving lipid-lowering therapy (Cannon et al., 2004; Colhoun et al., 2004; Sever et al., 2003).
Although genetic predisposition has been suggested to be an important determinant of hyperlipidemia (Andreotti et al., 2009; Liao et al., 2008; Willer et al., 2008), genetic factors alone cannot explain the recent increase in prevalence of hyperlipidemia and CHD. Unhealthy living habits and an unbalanced diet have been identified as the most significant risk factors for development of hyperlipidemia and for which an intervention can be most effectively designed (Mohanna et al., 2006).
Since altitude has been reported to be associated with risk factors for CHD such as obesity (Sherpa et al., 2010), physical activity, and diet, we predict that the lipid distribution may differ among people with varied altitudes. Many studies on the prevalence and the related factors associated with hyperlipidemia have now been conducted in China and other countries, but a survey of populations living at moderate altitude on the Yunnan-Kweichow Plateau, Southwestern China are few, particularly in relation to lifestyles and dietary preferences.
The aims of our present study were to determine the prevalence of hyperlipidemia and related risk factors of abnormal lipid profiles in a subpopulation living at a moderate altitude (1500–2500 m) on the Yunnan-Kweichow Plateau in Southwestern China.
Materials and Methods
Study population
A cross-sectional study was conducted from July to October 2010 among a sample group of residents living at a moderate altitude in mountainous rural areas of Yunxian County (Yunnan province), known as the Yunnan-Kweichow Plateau, in Southwestern China. Three towns (Yongbao, Dachaoshanxi, and Chafang) located at 1500–2500 m above the sea level were selected randomly from a total of nine in this area, and two groups of resident committees were chosen randomly from each selected town. Individuals who had resided for more than 10 years continuously in the selected committees, and were 20 years of age or older were recruited into the study cohort. Pregnant women and those who were mentally or physically unfit to undergo the study were excluded, including individuals with psychiatric disorders, hypophrenia, paralysis, and cancer. Subjects out of the random selection list who had volunteered were also rejected. A total of 1430 subjects were eventually invited to participate. Only 15 persons (1.0%) in this group declined to participate due to time constraints. The final study cohort comprised 724 men and 691 women aged 22–84 years.
Tests include a physical examination, completion of a comprehensive questionnaire, and plasma lipid profiles. All data were collected by trained medical personnel. The study was approved by a Regional Ethics Committee and verbal informed consent was obtained from all participants.
Measurements and data collection
A formal invitation letter was sent to appropriate local departments one month prior to commencing the study. This correspondence outlined the objectives of the survey and provided details regarding administration and procedures. The selected participants were asked to gather at a designated address of the resident committee. Anthropometric measurements including weight, height, and waist and hip circumference were taken. The body mass index (BMI) and waist-to-hip ratio (WHR) were also calculated for the participants. In addition, all participants completed a five-page questionnaire on their sociodemographic characteristics, personal and family medical history, medications, smoking habits, alcohol consumption, physical activities, and dietary habits. A validated quantitative food frequency questionnaire was also included. Some of the questions were modified to suit local customs and language. The ages of the participants were divided into five groups: 20–30, 31–40, 41–50, 51–60, and 61+years. Ethnicity was classified as Han or Minority. Cigarette smoking was categorized as “yes” (occasional or daily smokers) or “no” (nonsmokers or ex-smokers). Data on the frequency of alcohol consumption were obtained by asking the question “Do you drink alcoholic beverages at least once a week and has this been the case for more than 6 months?” Physical activity was defined as taking exercise or participating in physical labor activities more than twice each week for at least 30 minutes each time. In accordance with the Dietary Guidelines of China, we defined seven food groups for the purposes of this study: cereals, vegetables, fruits, nuts, beans, animal foods (for which the subgroups are milk products, meat, fish, and eggs) and others (coffee, tea, drink, and edible oil). A total of 71 kinds of food were included in our food frequency questionnaire. There were four levels of frequency to choose on the survey: never, daily, weekly, and monthly. Data were obtained by asking “Do you eat…?”, “How often do you eat…?” and “How many do you eat…per time?” Bowl, cup, spoon, and food photographs were used to assist the participant in estimating their food intake levels. Dietary data were converted into nutriment data using Food Calculator software 2.1 (Chinese Center for Disease Control and Prevention, Beijing, China).
Laboratory measurements
Venous blood samples were collected following fasting for 8–12 hours and with no alcohol consumption from the previous night. Samples were then clotted at room temperature and centrifuged at 2000 rpm for 15 min. Serum obtained was then subjected to the measurements of total serum cholesterol (TC), triglyceride (TG), high density lipoprotein-cholesterol (HDL-C), and low density lipoprotein-cholesterol (LDL-C). These biomarkers were assayed using an automated biochemical analyzer (Hitachi, 7080, Tokyo, Japan). The concentrations of TC and TG were determined using enzymatic colorimetric tests. HDL-C and LDL-C concentrations were measured by direct methods. Commercial kits were purchased from the Sichuan Maker Biotechnology Co. Ltd., (Chengdu, China). The analyzers were calibrated each morning using a standard liquid. All laboratory analyses were carried out at the Department of Clinical Chemistry, People's Hospital of Yunxian County, Yunnan Province, China. This laboratory routinely participates in formal quality assurance exercises.
Definitions
In accordance with the guidelines for dyslipidemic prevention and treatment in Chinese adults (Joint Commission, 2007), hyperlipidemia was defined as meeting at least one of the following three criteria: hypercholesterolemia, TC≥5.18 mM; hypertriglyceridemia, TG≥1.70 mM; low HDL-C, HDL-C<1.04 mM. Other definitions included high LDL-C (≥3.37 mM); abnormal BMI (≥24.0 kg/m2); and an abnormal WHR [>0.92 (men);>0.81(women)].
Statistical analysis
SPSS statistical software package version 11.5 (SPSS, Inc., Chicago, IL) was utilized to perform statistical analyses. The data are expressed as the mean±standard deviation (SD) or frequencies at 95% confidence intervals (95% CI) and were calculated for all prevalence estimates. Interval-scaled, normally distributed data were analyzed using the Student's t test to investigate differences between two groups (e.g., hyperlipidemia and normolipidemia). Qualitative data and data not normally distributed were analyzed using the Mann Whitney U-test, chi-square test. Multiple logistic regression analysis was applied to evaluate ordinary characteristics, lifestyle, and physiological markers (independent factors) in relation to the incidence of hyperlipidemia (independent factors). A two-sided p value of less than 0.05 was considered to be statistically significant. Sample size calculations were based on a previous prevalence study of hyperlipidemia in Yunxian County (Deng et al., 2011). Given an estimated prevalence of hyperlipidemia of 50%, a maximum relative error of 25% was set for estimators, with a confidence interval of 95%. A sample size of 1430 subjects was thus estimated to be required for statistical purposes. To facilitate comparisons with other studies, age-standardized prevalence estimates for the total subpopulation, separately for men and women are presented, and were calculated in accordance with the reported age and gender composition of the Chinese population in 2007.
Results
Characteristics of the study cohort
Of the 1430 participants selected, 1415 subjects (corresponding to 99.0% of all those invited) comprising 724 men and 691 women completed all interviews and tests. The ethnic composition of the cohort was 51% Han and 49% other minorities, including Yi, Bulang, Lahu, Dai, Miao, Hui, Lisu, Wa, and Naxi. The broad characteristics of this cohort are listed in Table 1. Women in this group tended to be older and have a lower level of education. A higher proportion of the single, divorced, and widowed participants were also women. Men were more likely to be smokers, alcohol consumers, and more frequently to take exercise or participate in physical labor.
Table 1.
Ordinary Characteristics of the Study Participants
| |
Total |
Men |
Women |
|
|||
|---|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % | p |
| Age (years) | <0.001** | ||||||
| 20–30 | 135 | 9.5 | 50 | 6.9 | 85 | 12.3 | |
| 31–40 | 517 | 36.5 | 312 | 43.1 | 205 | 29.7 | |
| 41–50 | 410 | 29.0 | 214 | 29.6 | 196 | 28.4 | |
| 51–60 | 173 | 12.2 | 61 | 8.4 | 112 | 16.2 | |
| 61+ | 180 | 12.7 | 87 | 12.0 | 93 | 13.5 | |
| Ethnicity | 0.314 | ||||||
| Han | 732 | 51.7 | 384 | 53.0 | 348 | 50.4 | |
| Minority | 683 | 48.3 | 340 | 47.0 | 343 | 49.6 | |
| Marital status | 0.037* | ||||||
| Single | 94 | 6.6 | 35 | 4.8 | 59 | 8.5 | |
| Married | 1306 | 92.3 | 684 | 94.5 | 622 | 90 | |
| Divorced | 8 | 0.6 | 3 | 0.4 | 5 | 0.7 | |
| Widow(er) | 7 | 0.5 | 2 | 0.3 | 5 | 0.7 | |
| Education | 0.001** | ||||||
| Never | 21 | 1.5 | 6 | 0.8 | 15 | 2.2 | |
| Elementary school | 116 | 8.2 | 38 | 5.2 | 78 | 11.3 | |
| Junior-middle school | 348 | 24.6 | 171 | 23.6 | 177 | 25.6 | |
| Senior-high school | 386 | 27.3 | 220 | 30.4 | 166 | 24.0 | |
| Higher | 544 | 38.4 | 289 | 39.9 | 255 | 36.9 | |
| Current smoking | 476 | 33.6 | 414 | 57.2 | 62 | 9.0 | <0.001** |
| Current drinking | 557 | 39.4 | 461 | 63.7 | 96 | 13.9 | <0.001** |
| Exercise or physical labor | 806 | 57.0 | 439 | 60.6 | 367 | 53.1 | 0.004** |
| Total | 1415 | 100.0 | 724 | 100.0 | 691 | 100.0 | |
p<0.05, **p<0.01, men compared with women.
Prevalence of hyperlipidemia in the study cohort
Among the 1415 subjects who lived at moderate altitudes (1500–2500 m) in Yunxian County, 697 (49.3%, 95%CI: 46.7–51.9%) were found to suffer from hyperlipidemia. Among the participants with hyperlipidemia, 14.1% had hypercholesterolemia (98/697), 25.1% had hypertriglyceridemia (175/697), mixed hyperlipidemia was found in 45.6% (318/697), and 15.2% showed low HDL-C (106/697). The prevalence of hyperlipidemia in men was 53.6% (388/724) and in women was 44.7% (309/691). This gender difference was found to be statistically significant ((2=11.138, p=0.001). After standardization using the reported demographics for the whole population of China in 2007 for age and gender, the prevalence of hyperlipidemia was determined to be 49.0% for the whole study cohort (54.2% of the men and 44.8% of the women).
Profiles of the physiological and biochemical markers of hyperlipidemia among the study participants
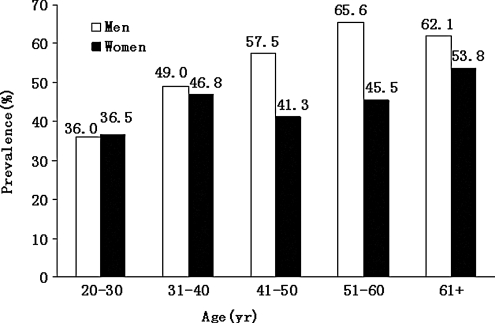
The prevalence of high TC, TG, or LDL-C was found to increase with age in both sexes in the study cohort (Table 2), as did the overall prevalence of hyperlipidemia. The prevalence of hyperlipidemia was similar in the men and women in the youngest age group of the cohort (36.0% vs. 36.5%), but was higher in the men in the older age groups (Fig. 1).The WHR also showed a similar change in the men and women in the study group, but this trend was not obvious for the HDL-C and BMI markers. The incidence of a higher BMI and WHR was clearly higher in the men.
Table 2.
Proportion of Abnormal Physiological or Biochemical Marker Profiles by Age Group and Sex
| |
Age-groups |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
20–30years (n=135) |
31–40years (n=517) |
41–50years (n=410) |
51–60years (n=173) |
61 and over (n=180) |
Total (n=1415) |
||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Men | ||||||||||||
| TC | 10.0 | 1.7–18.3 | 21.8 | 17.2–26.4 | 36.4 | 30.0–42.8 | 37.7 | 25.5–49.9 | 37.9 | 27.7–48.1 | 28.6 | 25.3–31.9 |
| TG | 32.0 | 19.1–44.9 | 41.3 | 35.8–46.8 | 45.3 | 38.6–52.0 | 42.6 | 30.2–55.0 | 50.6 | 40.1–61.1 | 43.1 | 39.5–46.7 |
| HDL-C | 16.0 | 5.8–26.2 | 15.1 | 11.1–19.1 | 17.3 | 12.2–22.4 | 14.8 | 5.9–23.7 | 14.9 | 7.4–22.4 | 15.7 | 13.0–18.4 |
| LDL-C | 6.0 | 0.0–12.6 | 6.4 | 3.7–9.1 | 8.4 | 4.7–12.1 | 8.2 | 1.3–15.1 | 10.3 | 3.9–16.7 | 7.6 | 5.7–9.5 |
| BMI | 32.0 | 19.1–44.9 | 43.9 | 38.4–49.4 | 53.7 | 47.0–60.4 | 41.0 | 28.7–53.3 | 57.5 | 47.1–67.9 | 47.4 | 43.8–51.0 |
| WHR | 36.0 | 22.7–49.3 | 35.6 | 30.3–40.9 | 58.4 | 51.8–65.0 | 37.3 | 25.5–49.9 | 59.8 | 49.5–70.1 | 45.4 | 41.8–49.0 |
| Women | ||||||||||||
| TC | 9.4 | 3.2–15.6 | 17.6 | 12.4–22.8 | 19.9 | 14.3–25.5 | 20.5 | 13.0–28.0 | 17.2 | 9.5–24.9 | 17.7 | 14.9–20.5 |
| TG | 25.9 | 16.6–35.2 | 22.4 | 16.7–28.1 | 20.9 | 15.2–26.6 | 25.0 | 17.0–33.0 | 35.5 | 25.8–45.2 | 24.6 | 21.4–27.8 |
| HDL-C | 15.3 | 7.6–23.0 | 20.5 | 15.0–26.0 | 19.4 | 13.9–24.9 | 13.4 | 7.1–19.7 | 28.0 | 18.9–37.1 | 19.4 | 16.5–22.3 |
| LDL-C | 5.9 | 0.9–10.9 | 8.3 | 4.5–12.5 | 8.7 | 4.8–12.6 | 16.1 | 9.3–12.9 | 16.1 | 8.6–23.6 | 10.4 | 8.1–12.7 |
| BMI | 21.2 | 12.5–29.9 | 25.4 | 19.4–31.4 | 24.0 | 18.0–30.0 | 29.5 | 21.1–37.9 | 21.5 | 13.2–29.8 | 24.6 | 21.4–27.8 |
| WHR | 29.4 | 19.7–39.1 | 35.6 | 29.0–42.2 | 33.7 | 27.1–40.3 | 39.3 | 30.3–48.3 | 38.7 | 28.8–48.6 | 35.3 | 31.7–38.9 |
CI, confidence interval.
FIG. 1.
Sex-specific prevalence of hyperlipidemia by age groups.
Age, BMI, and WHR characteristics of the study cohort
The male participants showed higher BMI and WHR values and these differences were statistically significant (BMI: t=8.785, p<0.001; WHR: t=20.664, p<0.001). Statistical significance was also observed for the participants with higher age, BMI, and WHR values of the hyperlipidemic subjects when compared with the normolipidemic subjects regardless of sex (Table 3).
Table 3.
Characteristics of Participants with and without Hyperlipidemia
| |
BMI |
WHR |
Age |
|||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| Total (n=1415) | 23.8±3.4 | 22.3±2.7 | 0.89±0.08 | 0.82±0.06 | 43.2±11.3 | 45.3±13.5 |
| Hyperlipidemia (n=697) | 24.7±3.3 | 23.1±3.0 | 0.91±0.07 | 0.83±0.07 | 44.7±11.3 | 46.5±14.3 |
| Normalipidemia (n=718) | 22.7±3.2 | 21.7±2.4 | 0.87±0.08 | 0.81±0.05 | 41.5±11.1 | 44.4±12.7 |
| t | −8.462 | −6.468 | −7.439 | −4.252 | −3.832 | −2.027 |
| P | <0.001** | <0.001** | <0.001** | <0.001** | <0.001** | 0.043* |
Data are the means±standard deviation (SD).
p<0.05, **p<0.01, hyperlipidemic compared with normalipidemic subjects.
Lifestyle and dietary characteristics of the study cohort
A high frequency of dining out, and an increased consumption of animal-based food products and alcohol were associated with hyperlipidemia in both sexes in our study cohort, but this was more pronounced in men. The intake of salted foods was significantly higher in hyperlipidemic compared with normolipidemic male subjects, whereas the rate of smoking was significantly higher in hyperlipidemic compared with normolipidemic female subjects. In addition, we found that a vegetarian diet was more prominent among normolipidemic subjects, regardless of genders (Table 4).
Table 4.
Living and Dietary Habits of the Study Participants
| |
Men |
Women |
||
|---|---|---|---|---|
| Hyperlipidemia (n=388) | Normalipidemia (n=336) | Hyperlipidemia (n=309) | Normalipidemia (n=382) | |
| Have breakfast every day | 315 (81.2%) | 279 (83.0%) | 265 (85.8%) | 340 (89.0%) |
| Dine out often | 167 (43.0%)* | 110 (32.7%) | 91 (29.4%)* | 87 (22.8%) |
| Eat snacks often | 62 (16.0%) | 58 (17.3%) | 121 (39.2%) | 143 (37.4%) |
| Take late night snack often | 80 (20.6%) | 53 (15.8%) | 23 (7.4%) | 26 (6.8%) |
| High intake of fried foods | 34 (8.8%) | 28 (8.3%) | 38 (12.3%) | 40 (10.5%) |
| Moderate intake of fried foods | 112 (28.9%) | 97 (28.9%) | 49 (15.9%) | 47 (12.3%) |
| Low intake of fried foods | 242 (62.4%) | 211 (62.8%) | 222 (71.8%) | 295 (77.2%) |
| Like to eat sweetmeat | 121 (31.2%) | 98 (29.2%) | 161 (52.1%) | 177 (46.3%) |
| Like to eat animal-based foods | 332 (85.6%)* | 268 (79.8%) | 230 (74.4%)* | 248 (64.9%) |
| Like to eat vegetarian foods | 152 (39.2%)* | 160 (47.6%) | 234 (75.7%)* | 313 (81.9%) |
| Like to eat salted foods | 211 (54.4%)* | 156 (46.4%) | 169 (54.7%) | 195 (51.0%) |
| Smoker | 225 (58.0%) | 189 (56.2%) | 36 (11.7%)* | 26 (6.8%) |
| Consume alcohol | 261 (67.3%)* | 200 (59.5%) | 60 (19.4%)** | 36 (9.4%) |
| Physical activity | 232 (59.8%) | 207 (61.6%) | 167 (54.0%) | 200 (52.4%) |
Data are expressed as n (%).
p<0.05, **p<0.01, hyperlipidemic compared with normolipidemic subjects.
Determinants of hyperlipidemia
Based on the aforementioned results, the following variables were tested as determinants of hyperlipidemia using multiple logistic regression analysis: age, gender, smoking status, current alcohol consumption, consumption of animal-based foods, vegetarian dietary preference, consumption of salted food, frequency of dining out, BMI, and WHR. These analyses revealed that a higher age and alcohol intake, consumption of animal-based foods, regular dining out and a higher BMI were the main determinants of hyperlipidemia in the female participants in our study cohort. In the men from this group, we found that a preference for salted food instead of animal-based food was most strongly related to hyperlipidemia (Table 5).
Table 5.
Evaluation of Variables Related to the Incidence of Hyperlipidemia by Multiple Logistic Regression Analysis
| |
Total (n=1415) |
Men (n=724) |
Women (n=691) |
|||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Age (per 10 years) | 1.246 (1.219, 1.273) | <0.001** | 1.271 (1.232, 1.311) | 0.001** | 1.209 (1.174, 1.245) | 0.003** |
| Consumes alcohol (yes/no) | 2.462 (1.613, 3.760) | <0.001** | 1.430 (1.038, 1.971) | 0.029* | 2.165 (1.368, 3.426) | 0.001** |
| Like to eat animal-based foods (yes/no) | 1.646 (1.261, 2.148) | <0.001** | / | / | 1.777 (1.233, 2.561) | 0.002** |
| Like to eat salted foods (yes/no) | / | / | 1.400 (1.026, 1.909) | 0.034* | / | / |
| Dine out often (yes/no) | 1.556 (1.223, 1.980) | <0.001** | 1.575 (1.140, 2.175) | 0.006** | 1.555 (1.082, 2.236) | 0.017* |
| BMI (≥24.0 kg/m2) | 2.649 (2.101, 3.341) | <0.001** | 2.906 (2.127, 3.970) | <0.001** | 2.482 (1.725, 3.572) | <0.001** |
p<0.05, **p<0.01. Method, Forward: Conditional.
Variables entered in steps 1–5:
Total: BMI, Consume alcohol, Age, Like to eat animal-based foods, Dine out often.
Women: BMI, Consume alcohol, Like to eat animal-based foods, Age, Dine out often.
Men: BMI, Age, Dine out often, Consume alcohol, Like to eat salted foods.
Nutriment intake among the study cohort
The average daily energy, and protein and fat intakes of the study participants were found to be higher than the current Chinese Recommendation Nutrient Intakes (RNI), and hyperlipidemic subjects in our cohort had a higher average daily intake of total fat, cholesterol, and a lower consumption of dietary fiber than the normolipidemic study participants (p<0.01). In addition, the normolipidemic subjects showed a higher intake of carbohydrate than the hyperlipidemic participants, but this was not statistically significant (Table 6).
Table 6.
Average daily intake of Dietary Nutrients Among the Study Participants
| Energy (kJ/d) | Protein (g/d) | Fat (g/d) | CHO (g/d) | Diet fiber (g/d) | Cholesterol (mg/d) | |
|---|---|---|---|---|---|---|
| Hyperlipidemia (n=697) | 10255.0±3788.5 | 102.47±34.58 | 89.11±38.39 | 298.68±129.80 | 11.84±5.37 | 315.50±117.44 |
| Normalipidemia (n=718) | 9798.8±3739.3 | 96.44±34.53 | 73.14±33.67 | 306.94±136.74 | 14.07±6.78 | 280.98±101.35 |
| t | 2.101 | 3.035 | 7.504 | −1.066 | −6.624 | 5.323 |
| p | 0.036* | 0.002** | <0.001** | 0.287 | <0.001** | <0.001** |
Data are expressed as the mean±standard deviation (SD).
p<0.05, **p<0.01, hyperlipidemic compared with normalipidemic subjects.
Discussion
Yunnan-Kweichow Plateau is located in Southwestern China at an altitude of 1000–3000 meters above sea level. In addition to the ethnic Han majority, 26 ethnic minorities live in this region, and some of the rural communities still practice traditional agriculture and animal breeding. Because of the geographical characteristics of Yunnan-Kweichow Plateau, including chronic hypoxia and distinctive cultural habits, many of the populations in this region show various levels of economic development, urbanization, and disease status. Moreover, with the changes in lifestyle and dietary choices that have come about in recent decades, the potential risk of developing various chronic noncommunicable diseases has gradually increased. Based on the basic information available from local hospital records, there are approximately three deaths from CVD each day, and a mortality rate of 50% in 2009. These numbers are higher than that of other districts and above the national average of China (Lin LP, 2005).
Hyperlipidemia is one of the main risk factors for CVD, and it is positively associated with the risks of ischemic heart disease, ischemic stroke, and other vascular disorders (Primatesta et al., 2006; Ravnskov U, 1992). The increased cardiovascular risks associated with elevated blood lipids appear to be common worldwide. In a World Health Report in 2002, raised cholesterol was listed as one of the top five leading causes of global mortality (World Health Organization, 2002). We therefore wanted to evaluate whether hyperlipidemia is related to the high prevalence of CVD in Yunnan-Kweichow Plateau, as there was a paucity of information regarding the prevalence and distribution of abnormal lipids in the inhabitants of this region.
The data collected in this cross-sectional study revealed a 49.3% prevalence of hyperlipidemia among the participants, 53.6% in men and 44.7% in women. Following standardization of these figures using the age and gender composition of the Chinese population reported in 2007, the prevalence of hyperlipidemia was revised to 49.0% among all of the study participants, 54.2% in men and 44.8% in women. These small differences indicated that our sample population was a representative and unbiased cohort. However, it is noteworthy that the prevalence of hyperlipidemia in Chinese adults was reported in 2002 to be 18.6%, indicating a very large increase in this condition throughout China, even in moderate altitude areas which are less developed and have higher relative poverty levels.
Among the types of hyperlipidemia, hypertriglyceridemia (25.1%) is the most prevalent one, consistent with the main prevalent type in Chinese. In this cohort, however, the prevalence of hypercholesterolemia was 23.3%, hypertriglyceridemia was 34.1%, low HDL-C was 17.5%, and high LDL-C was 9.0%. In contrast to these findings, a survey conducted in 2006 reported a slightly higher prevalence of hypercholesterolemia at 31.0%, and low HDL-C at 22.4% among highland communities in Lhasa, Tibet (3660 m), but the prevalence of hypertriglyceridemia in these communities was considerably lower at 12.2% (Sherpa et al., 2011). Likewise, a high hypercholesterol and low HDL-C prevalence of 34.3% and 30.4% have been reported among high altitude natives of Peru (4100 m) in which the prevalence of hypertriglyceridemia was considerably higher at 53.9% of the tested subjects (Mohanna et al., 2006). In a previous survey of the resident committees of Hunan province (100–1000 m) in 2002, a prevalence of 15.6% was reported for hyperlipidemia, 7.9% for hypercholesterolemia, 10.9% for hypertriglyceridemia, and 2.9% for low HDL-C (Lin et al., 2006). These observations collectively suggest that a low altitude has a “protective” effect against hyperlipidemia, and hyperlipidemia alone cannot explain the high prevalence and mortality of CVD on Yunnan-Kweichow Plateau. However, these remarkable disparities might be due to differences in the designs as the respective studies, including the investigation time, the diagnostic criteria used, the sample sizes, the demographic characteristics of the subjects, and ethnic differences (de Koning et al., 2008; Zhang et al., 2010). More surveys in each of these regions and in adjacent areas or districts at a similar altitude are thus needed.
The prevalence of an abnormal WHR increased with age for both genders in our current study cohort, as did the TC, TG, and LDL-C levels. The odds ratios for the risk of hyperlipidemia associated with a 10-year increase in age were 1.246 for the total cohort, 1.271 for men and 1.209 for women. In the process of aging, there is a progressive increase in visceral adiposity and lean tissue decrease, causing a reduction in the insulin sensitivity of the organism (Denino et al., 2001). This phenomenon also has been demonstrated in a Peruvian study of highland communities (Medina-Lezama et al., 2007).
The mean BMI measurement in our present study (23.1±3.2) is comparable with that reported previously for Chinese adults in rural plain area of Tianjin (23.7±3.8) (Huiguang Tian et al., 2009) and for rural Bolivians (22.7±0.4) (Frisancho et al., 1995), although the value is lower than that described for high-altitude Quechua populations from the Peruvian Central Andes (24.2±2.1) (Toselli, 2001) and the SPC district of Peru (25.4±3.7) (Mohanna et al., 2006). The WHRs measured in our current study were 0.85±0.08 for the total group, 0.89±0.08 in men and 0.82±0.06 in women, which are different from those of other reports: 0.90±0.09 in men and 0.91±0.10 in women in a population-based sample of 12,514 Iranian adults (Ali et al.,2010); 0.95±0.03 in both men and women aged over 40 years in the health survey in Yangpyeong County, Korea in 2004–2005 (Min et al.,2010); and 0.96±0.006 in healthy men, 0.92±0.005 in healthy women, 1.01±0.003 in men with metabolic syndrome, and 0.97±0.004 in women with metabolic syndrome in people aged 30 years and above of Asian Indian origin (Das et al., 2010). Our measurements are also lower than those reported for a Chinese cohort from the Plain of Shenyang (Yong Liu et al., 2011). However, these data may not be strictly amenable to a direct comparison due to the differences between the survey times and other factors, but the crude data indicate that the BMI and WHR levels in the Yunnan-Kweichow Plateau population are relatively lower than other areas of China and other countries.
The BMI and WHR can typically be used as predictors of chronic noncommunicable diseases such as high blood pressure, diabetes, hyperlipidemia, and CVD. However, the proposed cut-off values for these indicators remain controversial. The World Health Organization Western Pacific Region report (2000) suggests a cut-off value for defining obesity as a BMI of≥25 kg/m2. In contrast, a recent Chinese study (Yong Liu et al., 2011) suggests that the appropriate BMI cut-off values for predicting the presence of multiple metabolic risk factors are 22.85 kg/m2 and 23.30 kg/m2 in men and women, respectively. The results of our present study indicate that populations living at a moderate altitude on the Yunnan-Kweichow Plateau have a generally lower than average BMI and WHR, but show an increased prevalence of hyperlipidemia and an abnormal lipid profile, most notably in men. Moreover, by multiple logistic regression analysis, we found that a high BMI (≥24.0 kg/m2) increased the risk of hyperlipidemia by 2.649-fold in the total study cohort (2.906-fold for men and 2.482-fold for women). Hence, choosing an appropriate cut-off BMI and WHR value to predict the risk of CVD or other diseases may be particularly important in these regional areas.
Our study has further shown that hyperlipidemic participants in the sample cohort of both genders tended to dine out more often and consume more alcohol. The consumption of salted food was found to be the most significant risk factor for dyslipidemia in men in our study cohort, whereas in the female participants this was animal-based foods. In addition, the normolipidemic subjects among the participants were more likely to be vegetarian in both men and women. At the same time, we found that established unhealthy behaviors were more pronounced in men, which likely explains the differences in the blood lipid profile between the men and women in our cohort. There was also a high proportion (63.7%) of men in the study group who consumed alcohol, whereas in women this number was much lower (13.9%). We found from our analysis that drinking habits increased the risk of hyperlipidemia by 2.462-fold for total population, 1.430-fold for men and 2.165-fold for women. These findings are consistent with those of other surveys (de Campos et al., 2010; Neuhouser et al., 2002). Smoking was not selected as a determinant of hyperlipidemia in our logistic regression model because a very high smoking rate in men compared with women was found for both hyperlipidemic or normolipidemic participants, and we thus focused on more pronounced differences between these groups. It is noteworthy in this regard that in a previous investigation from our laboratory, an extremely high prevalence of hyperlipidemia (58.1%) was found in smoking men from Yunxian County, Yunnan Province (Deng et al., 2011). The reported results of other surveys have also reinforced the conclusion that smoking is closely associated with hyperlipidemia (Craig et al., 1989; Freedman et al., 1986).
The traditional dietary pattern among the residents of Yunnan-Kweichow Plateau is Oriental and is therefore dominated by plant-based foods that are known to be beneficial in the prevention of disorders such as hyperlipidemia and CVD. Economic prosperity in these districts has however produced a shift away from the more traditional lifestyles that has included changes in dietary habits. When compared against the current Dietary Guidelines of China, our current study population had a lower than optimal average intake of coarse grains, beans, vegetables, fruit, and milk, whereas the intake of meat was found to be higher than the recommended levels. This was particularly true for red meats such as pork and beef. Furthermore, the average daily energy, and protein and fat intakes in our cohort were higher than those advised by the RNI of China, and the differences in these intakes were found to be significant between the hyperlipidemic and normolipidemic subjects. It is worth noting that some of the current study participants reside in districts where the transport of nonlocal foods, including fish or sea food, is quite difficult. These individuals are therefore usually dependent on local livestock for their source of meat and this is commonly salted. It is well known that high salt foods are associated with hypertension and other chronic metabolic diseases, and animal-based food consumption has been shown to increase the total and/or LDL cholesterol levels in most previous reports. It is widely accepted that proper nutrition is the cornerstone of hyperlipidemia and CHD prevention (Castro et al., 2005; Eilat-Adar, 2010; Marinangeli et al., 2010; Sirtori et al., 2008). An earlier review has also summarized the cumulative evidence to date from randomized controlled trials showing that supplementation with plant soluble fiber, plant sterols and stanols, soy protein, and nuts lowers the LDL-C levels (Nijjar et al., 2010). Moreover, primary plant-based and ovolactovegetarian dietary interventions have been associated with decreases in the TC and LDL cholesterol levels of about 10%–15%, whereas vegan dietary interventions have been found to result in decreases of approximately 15%–25%, and combination dietary interventions (vegetarian diets with additional fiber, soy, and nuts) with decreases of approximately 20%–35%, in these levels (Ferdowsian et al., 2009).
It is undeniable that in a similar manner to the Tibetans (Xu et al., 2008), the population of Yunnan-Kweichow Plateau is undergoing an epidemiological transition, which may influence future health outcomes at the population level. For example, reduced physical activity and poor dietary choices can cause an increase in sedentary lifestyles and a higher incidence of obesity. Our current study confirms that these remain the most significant risk factors for hyperlipidemia, and that this is true for men and women of all ethnic groups.
Conclusions
Observations and analyses in this study reveal a higher prevalence of hyperlipidemia, hypercholesterolemia, hypertriglyceridemia, and elevated BMI and WHR values in men, and a marginally higher prevalence of low HDL-C and high LDL-C profiles in women from the Yunnan-Kweichow Plateau in Southwestern China. The prevalence of hyperlipidemia was found to increase with age, as did the prevalence of an elevated TC, TG, LDL-C, and WHR. Our analyses confirm that a high BMI and unhealthy living and dietary habits also play significant roles in the onset of hyperlipidemia. Additional studies of the health characteristics and related factors that can contribute to the prevention of diverse chronic noncommunicable diseases in populations living at moderate altitudes are needed.
Acknowledgments
This work was supported by Chinese National Natural Science Foundation (Grant No. 30872101). We appreciate the support and cooperation of the community office in Yunxian County, Yunnan province, and the medical personnel in People's Hospital of Yunxian County.
Author Disclosure Statement
The authors have no conflict of interest or financial ties to disclose.
References
- Ali Akbar T. Mojgan G. Alireza K, et al. Gender differences in obesogenic behaviour, socioeconomic and metabolic factors in a population-based sample of Iranians: The IHHP Study. J Health Popup Nutr. 2010;28:602–609. doi: 10.3329/jhpn.v28i6.6609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JW. Konz EC. Obesity and disease management: Effects of weight loss on comorbid conditions. Obes Res. 2001;9:326S–334S. doi: 10.1038/oby.2001.138. [DOI] [PubMed] [Google Scholar]
- Andreotti G. Menashe I. Chen J, et al. Genetic determinants of serum lipid levels in Chinese subjects: A population-based study in Shanghai, China. Eur J Epidemiol. 2009;24:763–774. doi: 10.1007/s10654-009-9402-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon CP. Braunwald E. McCabe CH, et al. for the Pravastatin or Atorvastatin Evaluation and Infection Therapy–Thrombolysis in Myocardial Infarction; 22 Investigators. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Eng J Med. 2004;350:1495–1504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- Castro IA. Barroso LP. Sinnecker P. Functional foods for coronary heart disease risk reduction: A meta-analysis using a multivariate approach. Am J Clin Nutr. 2005;82:32–40. doi: 10.1093/ajcn.82.1.32. [DOI] [PubMed] [Google Scholar]
- Colhoun HM. Betteridge J. Durrington PN, et al. on behalf of the CARDS investigators. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the collaborative atorvastatin diabetes study (CARDS): Multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- Craig WY. Palomaki GE. Haddow JE. Cigarette smoking and serum lipid and lipoprotein concentrations: An analysis of published data. BMJ. 1989;298:784–788. doi: 10.1136/bmj.298.6676.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das M. Pal S. Ghosh A. Association of metabolic syndrome with obesity measures, metabolic profiles, and intake of dietary fatty acids in people of Asian Indian origin. J Cardiovasc Dis Res. 2010;1:130–135. doi: 10.4103/0975-3583.70911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Campos W. Stabelini Neto A. Bozza R, et al. Physical activity, lipid consumption and risk factors for atherosclerosis in adolescents. Arq Bras Cardiol. 2010;94:601–607. doi: 10.1590/s0066-782x2010005000033. [DOI] [PubMed] [Google Scholar]
- de Koning L. Merchant AT. Hegele RA, et al. Study of Health Assessment and Risk in Ethnic Groups Investigators. Association of the FABP2 T54 variant with plasma triglycerides and insulin resistance in a multiethnic population. Clin Chem. 2008;54:1742–1744. doi: 10.1373/clinchem.2008.106682. [DOI] [PubMed] [Google Scholar]
- Deng BJ. Luo TG. Shen TH, et al. Hyperlipidemia and its related factors status in smoking men of Yun county, Yunnan province. Chin J Public Health. 2011;5:5–8. [Google Scholar]
- Denino WF. Tchernof A. Dionne IJ, et al. Contribution of abdominal adiposity to age-related differences in insulin sensitivity and plasma lipids in healthy non obese women. Diabetes Care. 2001;24:925–932. doi: 10.2337/diacare.24.5.925. [DOI] [PubMed] [Google Scholar]
- Eilat-Adar S. Goldbourt U. Nutritional recommendations for preventing coronary heart disease in women: Evidence concerning whole foods and supplements. Nutr Metab Cardiovasc Dis. 2010;20:459–466. doi: 10.1016/j.numecd.2010.01.011. [DOI] [PubMed] [Google Scholar]
- Ferdowsian HR. Barnard ND. Effects of plant-based diets on plasma lipids. Am J Cardiol. 2009;104:947–956. doi: 10.1016/j.amjcard.2009.05.032. [DOI] [PubMed] [Google Scholar]
- Freedman DS. Srinivasan SR. Shear CL, et al. Cigarette smoking initiation and longitudinal changes in serum lipids and lipoproteins in early adulthood: The Bogalusa Heart Study. Am J Epidemiol. 1986;124:207–219. doi: 10.1093/oxfordjournals.aje.a114379. [DOI] [PubMed] [Google Scholar]
- Frisancho AR. Frisancho HG. Milotich M, et al. Developmental, genetic, and environmental components of aerobic capacity at high altitude. Am J Phys Anthropol. 1995;96:431–442. doi: 10.1002/ajpa.1330960408. [DOI] [PubMed] [Google Scholar]
- Huiguang T. Hongxiang X. Guide S. Hong Z. Gang H. Prevalence of overweight and obesity among 2.6 million rural Chinese adults. Prevent Med. 2009;48:59–63. doi: 10.1016/j.ypmed.2008.10.020. [DOI] [PubMed] [Google Scholar]
- Joint Commission. Guidelines for dyslipidemic prevention and treatment of Chinese adults. People's Medical Publishing House; Beijing, People's Republic of China: 2007. [Google Scholar]
- Liao YC. Lin HF. Rundek T, et al. Multiple genetic determinants of plasma lipid levels in Caribbean Hispanics. Clin Biochem. 2008;41:306–312. doi: 10.1016/j.clinbiochem.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Lipin. The analysis for cause of death in Chinese residents. Shanghai J Prev Med. 2005;17:344–346. [Google Scholar]
- Lin Min. Jin Donghui. Li Guangchun, et al. Plasma lipids level profiles and epidemiological characteristics of dyslipidemia in people aged 18 years or over in Hunan Province. Pract Prev Med Chinese. 2006;13:1150–1154. [Google Scholar]
- Marinangeli CP. Jones PJ. Plant sterols, marine-derived omega-3 fatty acids and other functional ingredients: A new frontier for treating hyperlipidemia. Nutr Metab. 2010;7:76. doi: 10.1186/1743-7075-7-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Lezama J. Zea-Diaz H. Morey-Vargas OL, et al. Prevalence of the metabolic syndrome in Peruvian Andean Hispanics: The PREVENCION study. Diabetes Res Clin Pract. 2007;78:270–281. doi: 10.1016/j.diabres.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Min Jung Ko. Mi Kyung Kim. Jinho Shin. Bo Youl Choi. Relations of pulse wave velocity to waist circumference independent of hip circumference. Epidemiol Health. 2010;32:e2010004. doi: 10.4178/epih/e2010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanna S. Baracco R. Seclen S. Lipid profile, waist circumference, and body mass index in a high altitude population. High Alt Med Biol. 2006;7:245–255. doi: 10.1089/ham.2006.7.245. [DOI] [PubMed] [Google Scholar]
- Neuhouser ML. Miller DL. Kristal AR. Barnett MJ. Cheskin LJ. Diet and exercise habits of patients with diabetes, dyslipidemia, cardiovascular disease or hypertension. J Am Coll Nutr. 2002;21:394–401. doi: 10.1080/07315724.2002.10719241. [DOI] [PubMed] [Google Scholar]
- Nijjar PS. Burke FM. Bloesch A. Rader DJ. Role of dietary supplements in lowering low-density lipoprotein cholesterol: A review. J Clin Lipidol. 2010;4:248–258. doi: 10.1016/j.jacl.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Primatesta P. Poulter NR. Levels of dyslipidaemia and improvement in its management in England: Results from the Health Survey for England 2003. Clin Endocrinol. 2006;64:292–298. doi: 10.1111/j.1365-2265.2006.02459.x. [DOI] [PubMed] [Google Scholar]
- Ravnskov U. Cholesterol lowering trials in coronary heart disease: Frequency of citation and outcome. BMJ. 1992;305:15–19. doi: 10.1136/bmj.305.6844.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sever PS. Dahlof B. Poulter NR, et al. for the ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): A multicentre randomised controlled trial. Lancet. 2003;361:1149–1158. doi: 10.1016/S0140-6736(03)12948-0. [DOI] [PubMed] [Google Scholar]
- Sherpa LY. Deji SH, et al. Lipid profile and its association with risk factors for coronary heart disease in highlanders of Lhasa, Tibet. High Alt Med Biol. 2011;12:57–63. doi: 10.1089/ham.2010.1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherpa LY. Deji SH. Chongsuvivatwong V. Thelle DS. Bjertness E. Obesity in Tibetans aged 30–70 living at different altitudes under the north and south faces of Mt. Everest. Int J Environ Res Public Health. 2010;7:1670–1680. doi: 10.3390/ijerph7041670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirtori CR. Galli C. Anderson JW. Arnoldi A. Nutritional and nutraceutical approaches to dyslipidemia and atherosclerosis prevention: Focus on dietary proteins. Atherosclerosis. 2008;203:8–17. doi: 10.1016/j.atherosclerosis.2008.06.019. [DOI] [PubMed] [Google Scholar]
- Toselli S. Tarazona-Santos E. Pettener D. Body size, composition, and blood pressure of high-altitude quechua from the Peruvian Central Andes (Huancavelica, 3680 m) Am J Hum Bio. 2001;13:539–547. doi: 10.1002/ajhb.1086. [DOI] [PubMed] [Google Scholar]
- Willer CJ. Sanna S. Jackson AU, et al. Newly identified loci that influence lipid concentrations and risk of coronary artery disease. Nat Genet. 2008;40:161–169. doi: 10.1038/ng.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Reducing Risks. Promoting Healthy Life; WHO, Geneva: 2002. The World Health Report 2002. [Google Scholar]
- World Health Organization Western Pacific Region International Association for the Study of Obesity International Obesity Task Force. The Asian-Pacific Perspective: Redefining Obesity and its Treatment. World Health Organization Pacific Region; Geneva: 2000. [Google Scholar]
- Wu Xigui. The epidemiologic situation and tendency of coronary heart disease in Chinese population. Chinese J Prev Control Chronic Non-Commun Dis. 2003;8.11:190–191. [Google Scholar]
- Xu J. Yang Y. Tashi N. Sharma R. Fang J. Understanding land use, livelihoods, and health transitions among Tibetan nomads: A case from Gangga Township, Dingri County, Tibetan Autonomous Region of China. Ecohealth. 2008;5:104–114. doi: 10.1007/s10393-008-0173-1. [DOI] [PubMed] [Google Scholar]
- Yong Liu. Guanghui Tong. Weiwei Tong. Liping Lu. Xiaosong Qin. Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Public Health. 2011;11:35. doi: 10.1186/1471-2458-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L. Qiao Q. Tuomilehto J, et al. DECODE/DECODA Study Group. Distinct ethnic differences in lipid profiles across glucose categories. J Clin Endocrinol Metab. 2010;95:1793–1801. doi: 10.1210/jc.2009-2348. [DOI] [PubMed] [Google Scholar]