Abstract
The aim of this study is to ascertain the relationship between ingestion of raw cow liver and Toxocara canis infection. A total of 150 apparently healthy adults were divided into 2 groups; 1 group consisted of 86 adults with positive results of Toxocara ELISA, and the other group of 64 adults with negative results. One researcher collected the history of ingestion of raw cow liver within 1 year and recent history of keeping dogs. Among 86 seropositive adults for T. canis, 68 (79.1%) had a recent history of ingestion of raw cow liver. Multivariate statistical analysis showed that a recent ingestion of raw cow liver and keeping dogs were related to an increased risk of toxocariasis (odds ratios, 4.4 and 3.7; and 95% confidence intervals, 1.9-10.2 and 1.2-11.6, respectively). A recent history of ingestion of raw cow liver and keeping dogs was significantly associated with toxocariasis.
Keywords: Toxocara canis, toxocariasis, visceral larva migrans, liver, food-borne helminthiasis
INTRODUCTION
The life cycle of Toxocara canis, a common round worm residing in the small intestine of dogs, is complex. Infection of dogs occurs by ingestion of eggs that are passed in the feces and contained in soil. The ingested embryonated eggs hatch in the stomach and small intestine, and the larvae liberate. The larvae invade the intestinal mucosa, enter into the mesenteric and portal veins, reach the liver, and then pass to the lungs. From the lungs, some larvae pass through the bronchioles, trachea, and pharynx, and are swallowed and develop into adults in the small intestine. Other larvae, from the lungs, are carried to the heart and are distributed throughout the body by systemic circulation, mainly to the lungs, liver, kidneys, and muscles. The larvae can be transferred to pups through transplacental circulation or transmammary passage through milk during lactation [1-4].
Toxocara spp. are capable of infecting other animals. As in infection of dogs, infection to other animals takes place by ingestion of egg-contaminated soil in dooryards and parks. The infected larvae, which are 0.5 mm long, reach the liver, may become encapsulated, and dormant in the liver parenchyma, and move slowly from place to place (i.e., visceral larva migrans), or may migrate to the lungs and may continue to be distributed in other tissues [2,3]. These arrested larvae in animal tissues do not grow into an adult ascarid, but are capable of transmitting to other animals that eat the infected tissue harboring the encapsulated larvae. This mode of transmission among carnivous vertebrates has been experimentally established [4-8]. If these animals form a part of the food chain of the definitive host, i.e., dogs and cats, the life cycle of the parasite is completed. This phenomenon is called paratenic infection [1]. A large variety of non-canid animals may be infected. For T. canis, the known paratenic hosts include mice, rats, chickens, pigeons, lambs, pigs, and cows. Thus, animals are infected by ingestion of embryonated eggs in contaminated soil or by ingestion of encapsulated larvae in the tissues of paratenic hosts through cannibalism.
As in animals, human infection occurs in 2 ways; by ingestion of embryonated eggs or, alternatively, by transfer of the encapsulated larvae of T. canis in the tissues of a paratenic host to humans [1]. In certain ethnic groups, some adults tend to eat uncooked animal tissues that contain encapsulated infective larvae. After swallowing, the encapsulated larvae hatch in the small intestine, liberate and penetrate the intestinal wall, get into the portal vein and reach the liver and lungs, and again encapsulate and remain alive for a certain period. Uncooked livers of cows [8-11], pigs [12], lambs [13], and chickens [14,15] have been reported as the sources of human infections. A recent retrospective study with Korean patients with peripheral blood eosinophilia showed that a recent history of eating raw cow liver was related to an increased risk of toxocariasis [16]. However, epidemiological data on the role of ingestion of raw cow liver in the transmission of T. canis from animals to humans is limited, and there has been no explicitly designed study. In order to assess the role of eating raw cow liver for human infection of T. canis, we performed a cross-sectional study.
MATERIALS AND METHODS
Subjects
Since the goal of this study was to assess the role of ingestion of raw cow liver in toxocariasis in the general population, we enrolled a population of healthy adults who visited a health-screening center from January to December 2009. One nurse interviewer chose the participants randomly by selecting those subjects who responded voluntarily. The interviewer asked for voluntary individual participation in this study and the subjects were provided with a questionnaire and a document for informed consent. The subjects were told of the possibility of T. canis infection through ingestion of uncooked animal tissues or breeding dogs in the house or garden. There were 122 men and 28 women (age range, 25-71 years; median age, 50 years; mean age, 50.3 years) who were enrolled in the study. The institutional review board approved this study and the informed consent was obtained from each patient.
Questionnaire on the history of eating raw animal tissues and keeping dogs
At a face-to-face interview, a trained nurse interviewer used a structured questionnaire to collect data concerning social characteristics of the subjects. The data included the history of ingestion of raw cow liver or raw liver of other animals, the history of ingestion of raw cow meat or of raw meat of other animals, the history of ingestion of raw blood of animals, and the history of ingestion of raw freshwater fish. The data also included the time and frequency of ingestion, the number of occasions and the amount consumed, the species of animals, and any history of keeping a dog in the house or garden. The study coordinator and medical doctors made every efforts to keep the interviewer blind to the clinical diagnosis of the participants.
After a thorough review of the questionnaire filled-in by the interviewer, an experienced physician without knowledge of any other information concerning the participants determined whether the subject had a significant history of eating raw tissues of animals or freshwater fish. The subject was considered to have a significant history of recent ingestion of raw tissues if the subject met all of the following criteria: 1) definite experience of ingestion of raw tissues of animals or fish, 2) the amount consumed was more than a single mouthful, and 3) the time of ingestion within 1 year.
Diagnosis of T. canis infection
An ELISA kit (Bordier Affinity Products SA, Crissier, Switzerland) was used for the diagnosis of human toxocariasis through detection of human IgG antibodies to Toxocara excretory/secretory (E/S) antigens. This system was reported with 91% sensitivity and 86% specificity [17]. The titers for positive results were variable according to the daily reference controls. Although some cross reactions may occur by other human helminthiases, such as trichinosis, fascioliasis, and strongyloidiasis, the titers in these helminthiases are lower than the titers of positive control serum samples of individuals infected with T. canis [17]. All individuals underwent serological (ELISA) tests for common parasites (Clonorchis sinensis, Paragonimus westermani, sparganosis, and cysticercosis) in our country.
Statistical analysis
We evaluated the relationship of adults with positive results of Toxocara ELISA and the history of recent ingestion of raw cow liver or raw liver of other animals, raw meat of animals, or raw blood of animals, a recent history of eating raw freshwater fish, a history of keeping dogs, and the serologic test results of other parasites with the use of multivariate statistical analysis. Odds ratios (OR) of results of Toxocara ELISA, together with the corresponding 95% confidence intervals (CI), in relation to 7 variables, were derived using multiple logistic regression analysis. A P-value of <0.05 was considered significant. Data analyses were performed with a commercially available software program (PASW Statistics, release 17.0.2; SPSS, Chicago, Illinois, USA).
RESULTS
Sixty-eight (79.1%) of 86 seropositive adults for T. canis had a recent history of ingestion of raw cow liver within 1 year, while 29 (45.3%) of 64 seronegative adults had a history of raw cow liver ingestion. Ten adults ate raw livers of animals other than cows, such as pigs (n=7), dogs (n=3), goats (n=2), chickens (n=2), ducks (n=1), or geese (n=1).
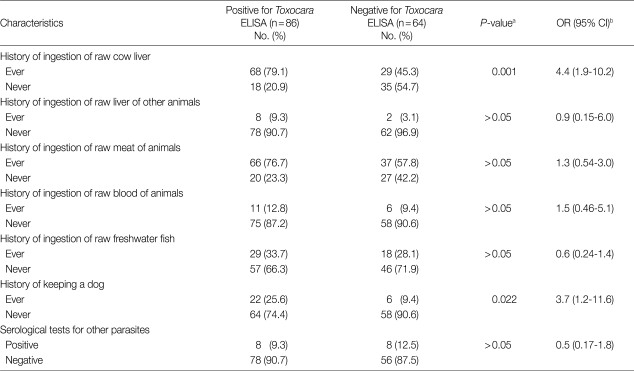
Table 1 presents the distribution of the 86 seropositive adults and 64 negative adults for the Toxocara ELISA. According to multivariate analyses, a recent history of ingestion of raw cow liver was related to an increased risk of toxocariasis (OR, 4.4; 95% CI, 1.9-10.2; P=0.001). A history of keeping dogs also showed an increased risk of toxocariasis (OR, 3.7; 95% CI, 1.2-11.6; P=0.022). A recent history of ingestion of raw liver of other animals, raw meat of animals, raw blood of animals, raw freshwater fish, and the serologic results for other parasites were not related with the increased risk of toxocariasis.
Table 1.
Distribution of 86 positive and 64 negative adults for Toxocara as determined by ELISA and corresponding P-values and OR with 95% CI, according to histories of ingestion of raw animals and fish, the history of keeping a dog, and serological results for other parasites
aMultivariate statistical results using a multiple logistic regression analysis.
bOR, odds ratio; 95% CI, 95% confidence intervals.
DISCUSSION
Chops of raw cow liver is one of the popular dishes in Korea, served in meat restaurants or buffet restaurants, sometimes along with chops of raw cow meat. Chops of raw liver and meat are served together with the usual cooked or barbecued meats. Some people believe that raw liver or raw meat is good for health, particularly the raw liver for eyesight. In our study population, about 2/3 (64.7%, 97 of 150) of adults had an experience of ingestion of raw cow liver. In the Korean society, some people eat chops of raw cow liver frequently when they dine at meat restaurants. Not infrequently, raw livers of chickens, goats, pigs, ducks, geese, or rabbits are also consumed. Because of this eating habit, there are many patients with subclinical toxocariasis. Usually, these people are checked by clinicians because of eosinophilia [10] or sometimes because of incidentally found small nodular lesions in the liver and/or lungs as seen on radiological imaging, such as sonography or CT [9].
The results of our study suggest that ingestion of raw cow liver substantially increases the risk for infection with T. canis. The seropositive rate for T. canis in adults that ate raw cow liver (70.1%, 68 of 97) was more than 2 times higher than in adults that did not consume raw cow liver (34.0%, 18 of 53). In a retrospective study with Korean patients with peripheral blood eosinophilia, 87.5% of seropositive patients had a recent history of eating raw cow liver, and 25.0% of seronegative patients had this history [16]. In 20 individuals that ate raw cow liver frequently (4 times or more per year), the seropositive rate was 95.0% (19 of 20). In 35 individuals that ate raw cow liver within 6 months prior to the interview, the seropositive rate was 94.3% (33 of 35). It appeared that the seropositive rate was higher in people with a history of ingestion of raw cow liver frequently and recently.
In spite of being seropositive for T. canis, 18 (20.9%) of 86 individuals denied a history of ingestion of cow livers. Ingestion of raw livers of pigs, lambs, and chickens have been reported as routes of human infections. We attempted to establish a role of eating habits of raw animal livers other than cows, such as goats, chickens, pigs, ducks, or geese for T. canis infection. There were 10 seropositive individuals with a history of consuming raw livers of other animals, but they had a history of ingestion of cow livers as well. Therefore, we could not verify the relation between ingestion of raw livers of other animals and toxocariasis.
Five of 18 subjects that denied a history of ingestion of cow livers were keeping dogs; 2 dogs lived in the house and the other 3 dogs lived in gardens. Infection might take place by ingestion of T. canis eggs that were spread by the dogs. In our study, the history of keeping dogs was statistically significant with T. canis infection. However, a retrospective study with Korean patients with peripheral blood eosinophilia could not show that the history of keeping dogs was related to an increased risk of toxocariasis [16].
In another 7 subjects who were seropositive without a history of raw cow liver ingestion, infection might have occurred by ingestion of raw cow meat. There have been several case reports describing Toxocara infection that probably took place by ingestion of raw meat of animals [18,19]. In animal experiments, Toxocara larvae were recovered in the lungs, liver, kidneys, brain, and muscles [8,20]. Tahira et al. [7] suggested the possibility of zoonotic risk of T. canis infection through ingestion of animal meat. In our study, many adults (84.5%, 82 of 97) that ate raw cow liver also ate raw cow meat. Therefore, we could not make a differentiation of subjects infected with Toxocara through ingestion of raw cow liver from subjects infected through ingestion of raw cow meat.
We do not know the route of T. canis infection in 6 individuals. We could not exclude the possibility of toxocariasis by other Toxocara spp., such as T. cati. Also, there may be cross reactions with other helminthiasis, such as trichinosis, fascioliasis, and strongyloidiasis.
T. canis seropositive rates in general population are variable depending on the country. The rate has been reported as 18% in a rural area in China [21], 20% in Malaysia [22], 26% in Iran [23], 6-36% in the Czech Republic [24], 2-5% and 14-37% in urban and rural areas of the Midi-Pyrenees area in France [25], 5% in Switzerland [26], and 5% in a rural area in Korea [27]. As dogs and cats are popular pets, there is widespread contamination of the environment with infective stage eggs and, therefore, toxocariasis is a worldwide disease, irrespective of developed or developing countries. In a total of 150 subjects enrolled in this study, 86 (57.3%, 86 of 150) were T. canis seropositive. Considering the seroprevalence rate in a rural population in Korea (5%), the seropositive rate in this study was very high. Higher seroprevalences have been reported in Indonesia (68%) [28] and Nepal (81%) [29]. Fan et al. [12] assumed that the high seroprevalence among healthy adults of Taiwanese aboriginal populations (46%) was due to the habit of eating raw liver of wild boar. The population enrolled in this study were healthy subjects who voluntarily visited the clinic for health screening. Therefore, these people were relatively wealthy and they dine at meat restaurants more frequently than other people, and they might have had more chances to consume raw cow livers.
Our study had some limitations. The study was of a cross-sectional nature and thus temporal associations could not be inferred. Therefore, we could not ascertain the inconsistency between seronegative subjects and remote infection by ingestion of raw cow livers. A bias arising from recall data based on the ability of an individual to recall the history of ingestion of raw tissue of animals could not be avoided. We did not count the number of chops of animal tissues ingested in determining the seropositivity of the enrolled participants. The study population might not be a representative of the general population as a nurse interviewer chose the participants randomly by selecting those subjects who responded voluntarily. Finally, positive results of ELISA do not definitely mean T. canis infection. Its sensitivity and specificity are around 90% [17].
With the limitations of the study in mind, we again suggest that ingestion of raw cow liver and keeping dogs increases the risk of T. canis infection in Korea. In view of many adults with subclinical toxocariasis, ingestion of uncooked livers of paratenic hosts is an important source for human infections that cannot be ignored.
ACKNOWLEDGMENT
This study was supported by the Samsung Biomedical Research Institute grant, #SBRI C-A9-241-1.
References
- 1.Orihel TC, Ash LR. Parasites in Human Tissues. Chicago, USA: American Society of Clinical Pathologists Press; 1995. [Google Scholar]
- 2.Beaver PC. The nature of visceral larva migrans. J Parasitol. 1969;55:3–12. [PubMed] [Google Scholar]
- 3.Beaver PC. Larva migrans. Exp Parasitol. 1956;5:587–621. doi: 10.1016/0014-4894(56)90032-7. [DOI] [PubMed] [Google Scholar]
- 4.Glickman LT, Schantz PM. Epidemiology and pathogenesis of zoonotic toxocariasis. Epidemiol Rev. 1981;3:230–250. doi: 10.1093/oxfordjournals.epirev.a036235. [DOI] [PubMed] [Google Scholar]
- 5.Pahari TK, Sasmal NK. Experimental infection of Japanese quail with Toxocara canis larvae through earthworms. Vet Parasitol. 1991;39:337–340. doi: 10.1016/0304-4017(91)90051-v. [DOI] [PubMed] [Google Scholar]
- 6.Pahari TK, Sasmal NK. Experimental infection of mice with Toxocara canis larvae obtained from Japanese quails. Int J Parasitol. 1990;20:263–264. doi: 10.1016/0020-7519(90)90110-9. [DOI] [PubMed] [Google Scholar]
- 7.Taira K, Saeed I, Permin A, Kapel CM. Zoonotic risk of Toxocara canis infection through consumption of pig or poultry viscera. Vet Parasitol. 2004;121:115–124. doi: 10.1016/j.vetpar.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 8.Lee KT, Min HK, Chung PR, Chang JK. Studies on the inducing possibility of human visceral larva migrans associated with eating habit of raw liver of domestic animals. Korean J Parasitol. 1976;14:51–60. doi: 10.3347/kjp.1976.14.1.51. [DOI] [PubMed] [Google Scholar]
- 9.Chang S, Lim JH, Choi D, Park CK, Kwon NH, Cho SY, Choi DC. Hepatic visceral larva migrans of Toxocara canis: CT and sonographic findings. AJR Am J Roentgenol. 2006;187:W622–W629. doi: 10.2214/AJR.05.1416. [DOI] [PubMed] [Google Scholar]
- 10.Kwon NH, Oh MJ, Lee SP, Lee BJ, Choi DC. The prevalence and diagnostic value of toxocariasis in unknown eosinophilia. Ann Hematol. 2006;85:233–238. doi: 10.1007/s00277-005-0069-x. [DOI] [PubMed] [Google Scholar]
- 11.Fitzgerald PR, Mansfield ME. Visceral larva migrans (Toxocara canis) in calves. Am J Vet Res. 1970;31:561–565. [PubMed] [Google Scholar]
- 12.Fan CK, Lan HS, Hung CC, Chung WC, Liao CW, Du WY, Su KE. Seroepidemiology of Toxocara canis infection among mountain aboriginal adults in Taiwan. Am J Trop Med Hyg. 2004;71:216–221. [PubMed] [Google Scholar]
- 13.Salem G, Schantz P. Toxocaral visceral larva migrans after ingestion of raw lamb liver. Clin Infect Dis. 1992;15:743–744. doi: 10.1093/clind/15.4.743. [DOI] [PubMed] [Google Scholar]
- 14.Nagakura K, Tachibana H, Kaneda Y, Kato Y. Toxocariasis possibly caused by ingesting raw chicken. J Infect Dis. 1989;160:735–736. doi: 10.1093/infdis/160.4.735. [DOI] [PubMed] [Google Scholar]
- 15.Morimatsu Y, Akao N, Akiyoshi H, Kawazu T, Okabe Y, Aizawa H. A familial case of visceral larva migrans after ingestion of raw chicken livers: appearance of specific antibody in bronchoalveolar lavage fluid of the patients. Am J Trop Med Hyg. 2006;75:303–306. [PubMed] [Google Scholar]
- 16.Choi D, Lim JH, Choi DC, Paik SW, Kim SH, Huh S. Toxocariasis and ingestion of raw cow liver in patients with eosinophilia. Korean J Parasitol. 2008;46:139–143. doi: 10.3347/kjp.2008.46.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jacquier P, Gottstein B, Stingelin Y, Eckert J. Immunodiagnosis of toxocarosis in humans: evaluation of a new enzyme-linked immunosorbent assay kit. J Clin Microbiol. 1991;29:1831–1835. doi: 10.1128/jcm.29.9.1831-1835.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schantz PM. Toxocara larva migrans now. Am J Trop Med Hyg. 1989;41:21–34. doi: 10.4269/ajtmh.1989.41.21. [DOI] [PubMed] [Google Scholar]
- 19.Stürchler D, Weiss N, Gassner M. Transmission of toxocariasis. J Infect Dis. 1990;162:571. doi: 10.1093/infdis/162.2.571. [DOI] [PubMed] [Google Scholar]
- 20.Dubey JP. Migration of Toxocara cati larvae in mice. Trop Geogr Med. 1968;20:172–176. [PubMed] [Google Scholar]
- 21.Luo ZJ, Wang GX, Yang CI, Luo CH, Cheng SW, Liao L. Detection of circulating antigens and antibodies in Toxocara canis infection among children in Chengdu, China. J Parasitol. 1999;85:252–256. [PubMed] [Google Scholar]
- 22.Hakim SL, Mak JW, Lam PL. ELISA seropositivity for Toxocara canis antibodies in Malaysia, 1989-1991. Med J Malaysia. 1993;48:303–307. [PubMed] [Google Scholar]
- 23.Sadjjadi SM, Khosravi M, Mehrabani D, Orya A. Seroprevalence of toxocara infection in school children in Shiraz, southern Iran. J Trop Pediatr. 2000;46:327–330. doi: 10.1093/tropej/46.6.327. [DOI] [PubMed] [Google Scholar]
- 24.Uhlíková M, Hübner J. Seroprevalence of Toxocara canis infection in Czech Republic. Cent Eur J Public Health. 1998;6:195–198. [PubMed] [Google Scholar]
- 25.Pelloux H, Faure O. Toxocariasis in adults. Rev Med Interne. 2004;25:201–206. doi: 10.1016/s0248-8663(03)00258-3. [DOI] [PubMed] [Google Scholar]
- 26.Speiser F, Gottstein B. A collaborative study on larval excretory/secretory antigens of Toxocara canis for the immunodiagnosis of human toxocariasis with ELISA. Acta Trop. 1984;41:361–372. [PubMed] [Google Scholar]
- 27.Park HY, Lee SU, Huh S, Kong Y, Magnaval JF. A seroepidemiological survey for toxocariasis in apparently healthy residents in Gangwon-do, Korea. Korean J Parasitol. 2002;40:113–117. doi: 10.3347/kjp.2002.40.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uga S, Ono K, Kataoka N, Hasan H. Seroepidemiology of five major zoonotic parasite infections in inhabitants of Sidoarjo, East Java, Indonesia. Southeast Asian J Trop Med Public Health. 1996;27:556–561. [PubMed] [Google Scholar]
- 29.Rai SK, Uga S, Ono K, Nakanishi M, Shrestha HG, Matsumura T. Seroepidemiological study of Toxocara infection in Nepal. Southeast Asian J Trop Med Public Health. 1996;27:286–290. [PubMed] [Google Scholar]