Abstract
Objective
Physician distress is a well-documented phenomenon with costly consequences for individuals, patients, and society. Existing services are not informed by physician preferences and are consequently underutilized. We sought to design an evidence-based intervention based on the attitudes towards support among physicians at our hospital.
Design
A 56-item survey was administered to a convenience sample (n= 108) of resident and attending physicians at Surgery, Emergency Medicine, and Anesthesiology departmental conferences.
Setting
A large tertiary-care academic hospital.
Main Outcome Measures
Likelihood of seeking support, perceived barriers, awareness of available services, sources of support, and experience with stress.
Results
79% experienced either a serious adverse patient event and/or a traumatic personal event within the preceding year. Willingness to seek support was reported for legal situations (72%), involvement in medical errors (67%), adverse patient events (63%), substance abuse (67%), physical (62%) or mental health illness (50%), and interpersonal conflict at work (50%). Barriers included lack of time (89%), stigma (74%), lack of confidentiality (77%), and access (69%). Physician colleagues were the most popular potential sources of support (88%), outnumbering traditional mechanisms such as the Employee Assistance Program (29%) and mental health professionals (48%). Based upon these results, one-on-one peer physician support program was incorporated into support services at our hospital.
Conclusions
Despite the prevalence of stressful experiences and the desire for support among physicians, established services are underutilized. As colleagues are the most acceptable sources of support, we advocate peer support as the most effective way to address this sensitive, but important issue.
Introduction
Physicians comprise a population susceptible to the development of emotional distress, as evidenced by the high prevalence of career dissatisfaction and burnout, with rates ranging from 15–29%1–5 and 22–75%3, 6–11, respectively. Mental health disorders commonly arise; 18–30% of physicians have screened positive for depression in national surveys3, 10, 12. If unaddressed, physicians may turn to maladaptive coping mechanisms such as withdrawal13, denial13, substance abuse14, or suicide15–16.
Physician distress is devastating beyond an individual level; by impacting performance, its fallout touches patients. Distressed providers make more medical errors10, 12, 17–20, have riskier prescribing profiles21, and display less empathy22–23. Their patients are less satisfied24, less compliant25, and more litigious26. These physicians’ tendencies to change specialties5, 7 and/or practices5–6, decrease their work hours4–6, and leave patient care entirely4–5, 7 have significant implications for health care organizations and our health care system. The price of a single physician turnover is estimated at up to $123,000 in recruiting fees and $2,000,000 in lost revenue27. Decreased productivity among distressed physicians may exacerbate looming healthcare workforce problems such as shortages or specialty imbalances2, 28. Accordingly, physician wellness has been termed the “missing quality indicator”29.
Despite repeated calls across disciplines3, 7, 9–10, 12, 15, 18–20, 22, 29–37, efforts to address physician distress have been limited. Only a handful of interventions have been described in the literature, and still fewer demonstrate evidence of effectiveness37–41 –not in small part due to the general lack of knowledge regarding best practices. We know little about how physicians currently cope and nothing about which support mechanisms they find acceptable. Without this crucial information, even the best-intentioned interventions risk underutilization; such data is instrumental in the design of a program that will adequately service this gaping need within our community.
At our own institution, a program was launched in July 2006 to provide support to healthcare professionals following adverse medical events in the operating room42. Modeled after support networks used by first responders (police, fire, and emergency services), the Peer Support Team (PST) initially trained representatives from all disciplines (surgery, anesthesia, nursing) to participate in group debriefing sessions organized by the Employee Assistance Program (EAP). PST education included outreach, basic support skills (active listening, validation, acceptance), signs of need for escalation of care, and pathways by which such intensification may be accomplished (e.g. professional mental health services); such “emotional first aid” comprises a key stage in the natural history of provider recovery and has historically been difficult to identify and/or access43. By employing clinician colleagues already integrated and respected within the system, we expected PST to be more approachable, and hence more widely utilized, than existing services.
However, PST discovered that physicians failed to access the support offered within these group sessions; affected physicians tended to avoid the sessions, and those that attended were reluctant to share their distress. In private discussions with such physicians and the trained peer supporters, it became clear that in public, most physicians felt the need to maintain their role as healthcare team leader; it was countercultural for them to admit emotional vulnerability in the presence of non-physicians. To understand the unique challenges faced by physicians in seeking support, we turned to a survey conducted around the time of PST’s inception. These data, which we report here, informed the program’s redesign to specifically address physician needs.
Methods
Survey Instrument
No existing surveys addressed our domains of interest (willingness to seek support, perceived barriers, preferred mechanisms) at the time of this study; we developed our own items with input from survey research experts. Items were tested informally with physician colleagues and refined prior to administration.
The Physician Support Survey includes 56 items divided into 6 sections. The first 15 items query the likelihood that respondents would seek support for various theoretical situations (e.g. personal life struggles, medical error, legal situation), using a 4-point Likert scale (definitely would not, probably would not, probably would, definitely would). The next 13 items ask respondents to rate their level of agreement that certain factors (e.g. lack of time, stigma, cost) would present a barrier to seeking support on a 4-point Likert scale (strongly disagree, somewhat disagree, somewhat agree, strongly agree). Four items address respondents’ level of awareness of existing services (e.g. Employee Assistant Program, Physician Health Services), as characterized by one of four responses (never heard of, aware of but do not know how to contact, aware of and know how to contact, and aware and have used). The next 13 items assess the likelihood that respondents would utilize particular services (e.g. psychiatrist, faculty, resident, clergy), using a 4-point Likert scale (would not seek support, not very likely to seek support, somewhat likely to seek support, very likely to seek support). Eight items query respondents (yes/no) about their experience with stressful situations (e.g. adverse event, personal physical illness, illness among family) over the past year. The last three items represent demographic questions: training level (resident, fellow, attending, other), department (surgery, anesthesia, emergency medicine), and post-graduate year level (PGY1, PGY2, PGY3, PGY4, PGY5).
Survey Administration
The senior author (JS) introduced the study and distributed the surveys at the end of a departmental conference for each of the three departments: surgery, anesthesia, and emergency medicine. Audience members were invited to participate anonymously. Surveys were collected by an administrative assistant at the end of each meeting.
Statistical Analysis
For ease of interpretation and to increase power, all Likert scales were dichotomized into yes and no at the halfway point (e.g. definitely would not and probably would not became no; probably would and definitely would became yes). Training level was dichotomized into trainees (residents and fellows) and attendings. Other respondents (n=15) were excluded from analysis. All stressful situations experienced over the past year were condensed into a single binary variable, such that an affirmative response to any one of the 8 items constituted a positive stressor or indicator of distress. Descriptive statistics were obtained for the entire sample. Chi-square tests were performed to assess differences in responses between training levels, departments, and those who had experienced a stressor or indicator of distress. A subgroup analysis was performed to compare those who had experienced a specifically personal stressor or indicator of distress (i.e. serious personal physical illness, personal mental illness, feelings of wanting to harm yourself, serious illness among family, death in the family, other personal crisis, other) to those who either had not or had experienced a patient-related event. All calculations were performed in SAS 9.1 with significance set at p<0.05.
Results
We collected 108 surveys. Table 1 contains descriptive statistics for the entire sample.
Table 1.
Survey Respondent Characteristics
| Variable | N (%) |
|---|---|
| Level of Training | |
| Resident | 69 (64) |
| PGY 1 | 13 (12) |
| PGY 2 | 22 (20) |
| PGY 3 | 16 (15) |
| PGY 4 | 14 (13) |
| PGY 5+ | 4 (4) |
| Fellow | 4 (4) |
| Attending | 35 (32) |
|
| |
| Department | |
| Anesthesia | 46 (43) |
| Emergency Medicine | 23 (21) |
| Surgery | 39 (36) |
Prior Experiences
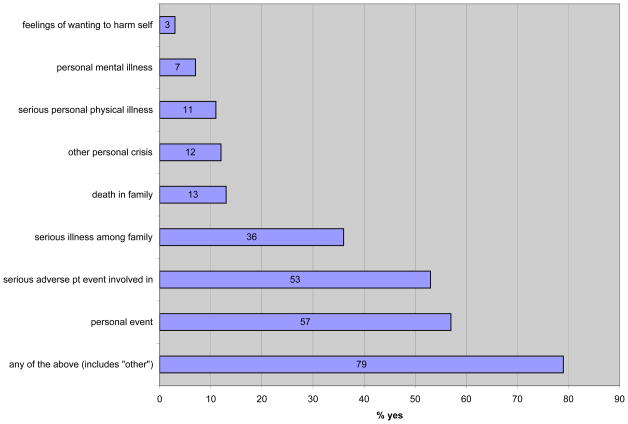
Over half of respondents had been involved in a serious adverse patient event (53%) or had experienced a personal stressor or indicator of distress (57%) in the past year; three-quarters (79%) had experienced at least one of these two. Among personal stressors or indicators of distress, serious illness among family members had affected more than a third (36%), while death in the family (13%), serious personal physical illness (11%), and other personal crises (12%) were somewhat less common, but not rare. These results are displayed in Figure 1.
Figure 1.
In the past year, have you experienced any of the following?
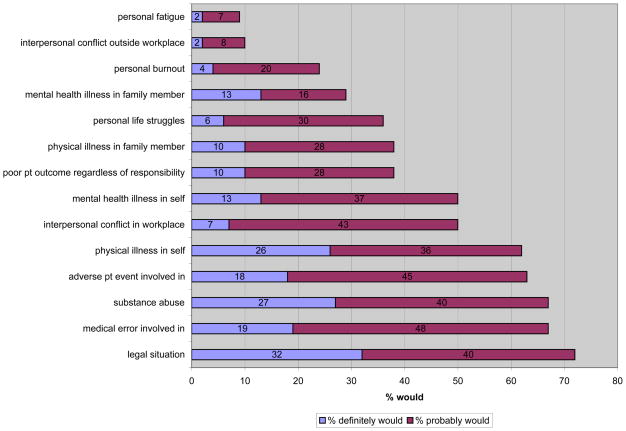
Willingness to Seek Support
The vast majority of responders (94%) indicated that they would anticipate wanting support for one or more of the listed stressful situations. Legal situations were the most commonly cited reason for which support would be desired (72%). Involvement in medical errors (67%) and adverse patient events (63%), substance abuse (67%), physical illness (62%), interpersonal conflict at work (50%), and mental health illness (50%) would also motivate a majority of people. Less common reasons for seeking support are described in Figure 2.
Figure 2.
Please indicate whether you would or would not seek support for the following difficulties.
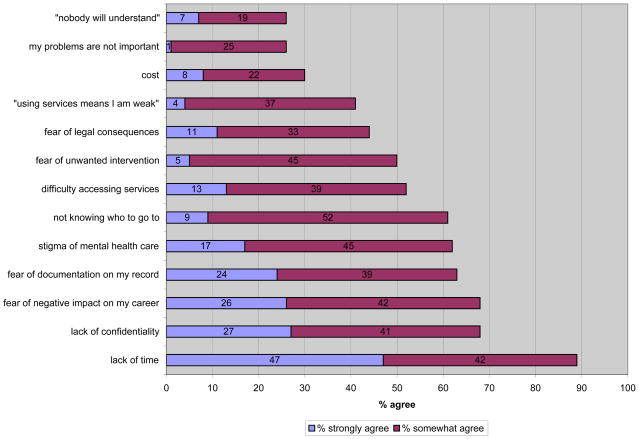
Barriers to Seeking Support
Nearly all respondents (89%) perceived that lack of time would present a barrier to seeking support. A majority also indicated that concerns about lack of confidentiality (68%), negative impact on career (68%), documentation on their records (63%), the stigma of mental health care (62%), uncertainty about whom to see (61%), difficulty accessing services (52%) and unwanted interventions (50%) would prevent them from seeking care. Figure 3 contains an exhaustive list of barriers.
Figure 3.
Please indicate whether you agree or disagree that the following factors would be a barrier.
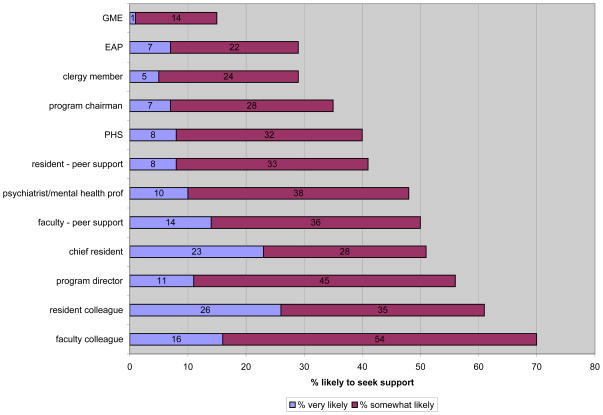
Sources of Support
Figure 4 contains the results for the questions regarding the likelihood of seeking support from various people and/or services. Physician colleagues – faculty (70%), residents (61%), program directors (56%), and chief residents (51%) – were the most commonly identified potential sources of support. A smaller, but substantial minority (35%) chose departmental chairmen as a potential source of support. Institutional organizations such as Physician Health Services (40%), Employee Assistance Program (29%), and Graduate Medical Education (15%) drew the fewest physicians. Indeed, 32%, 38%, and 30% of respondents had never heard of these services, respectively, while only a minority (21%, 19%, and 30%) knew how to contact them. We did not ask about the role of family members, friends, or spouses in physician support in our survey, but 20 respondents wrote them in under “other,” either as a potential or a previously utilized resource.
Figure 4.
Please state the likelihood that you would or would not seek support from each of the following when faced with stressful situations.
Trainee and Attending Differences
Trainees were significantly more likely than attendings to report that they would seek support for legal situations (82% v. 50%, p<0.01). The majority of both trainees and attendings cited lack of time as a barrier, although the trainees cited this more frequently (93% v. 79%, p=0.05). Three times as many trainees as attendings would be hindered by cost (38% v. 13%, p=0.01).
Predictably, residents were significantly more likely than attendings to seek support from other residents (53–82% v. 10–13%, p<0.01); however, there were no significant differences in the use of faculty, including chairmen and/or program directors, between trainees and attendings. Perhaps due to their increased willingness to pay, attendings were significantly more likely to seek support from mental health professionals (64% v. 41%, p=0.04). There were no significant differences between trainees and attendings in their experience with stress over the past year.
Interdisciplinary Differences
Emergency Medicine physicians were significantly less likely to seek support for involvement in a medical error (EM 48%, Surgery 62%, Anesthesia 77%, p=0.02). Likewise, anesthesiologists were significantly more likely to seek support for involvement in adverse events (Anesthesia 78%, Surgery 51%, EM 52%, p=0.02). Surgeons were less likely to seek support for an interpersonal conflict in the workplace (Surgery 28%, Anesthesia 62%, EM 61%, p<0.01).
There were higher levels of concern regarding a lack of confidentiality in seeking support (Surgery 70%, Anesthesiology 77%, EM 48%, p=0.0461) among surgeons and anesthesiologists. Similarly, anesthesiologists had more prevalent fears of legal consequences (Surgery 35%, Anesthesia 60%, EM 26%, p=0.01).
Differences Based Upon Prior Experiences
Those who had reported any type of stressor in the past year were more likely to seek support from colleagues (faculty 75% v. 48%, p=0.02; chief residents 57% v. 30%, p=0.03), perhaps because they already had. Similarly, experience may have informed responses for those who reported a specifically personal stressor or indicator of distress within the past 12 months. These respondents were less likely to fear legal consequences (33% v. 58%, p=0.02).
Comment
Physicians in this study indicate a desire to seek support for a number of fairly common issues. Two-thirds expressed an interest in support for involvement in a medical error and/or an adverse patient event, an experience that over half reported having in the preceding year. While these events are, to some degree, an inescapable part of the medical profession, conventional training does not address their potentially devastating emotional impact on health care providers. Thus, physicians have been called “the second victims” of medical mistakes44–45. Support of the medical team during the aftermath of an adverse event is a well-described, yet largely unmet need13, 20, 46–49; institutions should note that such support may mitigate the increased risk of future errors that is engendered by providers’ feelings of self-doubt or guilt18, as well aspsychologically sustain providers.
Given the high profile of malpractice in the public eye, it is unsurprising that legal situations were the most universally motivating stressor. The mere perception of risk of litigation has a harmful emotional effect on physicians49. We suspect that trainees’ increased desire for support in this situation is driven by their inexperience and thus their higher levels of anxiety about lawsuits.
Barriers to obtaining support were numerous and widely perceived. Time constraints, concerns about discovery (e.g. lack of confidentiality, documentation, fear of legal consequences or negative impact on career), and the stigma of mental health disease have been cited by physicians as impediments to seeking care in previous studies49–50. Furthermore, physicians are notoriously poor at self-care, failing to follow basic health recommendations like routine preventive screening51. A socially stigmatized condition like psychiatric disease is even more likely to be neglected.
A substantial proportion of physicians were unaware of the existence of traditionally available support mechanisms such as the Employee Assistance Program. Nationally, multi-component models centered around EAP-provided services have been developed to support providers following adverse events52. However, given the nature of barriers cited by respondents, increased knowledge is unlikely to result in increased use. Nearly 20% of our sample spontaneously wrote in a family member, friend, or spouse as a source of support. While friends and family are easily accessible, approachable, and undoubtedly comprise a large component of physicians’ support systems, their ability to provide appropriate support is perhaps limited by an incomplete understanding of medicine and hospital culture. Nevertheless, the importance of this resource to physicians is worth noting.
Limitations
This survey used a convenience sampling method; as the survey was entirely anonymous, and responses depended upon attendance at departmental conferences, which we are unable to ascertain, a non-response analysis is infeasible. These results may reflect a non-response bias, with more of those who had experienced a previous event or an interest in support electing to respond. However, given the number of people who responded at the lowest Likert point on every question, we suspect that we did capture a full range of responses. Additionally, using the average recorded attendance at these conferences, we estimate our n=108 to represent a response rate in the range of 88% – respectable for a physician survey. Our survey results derive from a single institution and may not be generalizable to other populations. Lack of access to EAP, for example, may be unique to our hospital. Nevertheless, as concerns about confidentiality are certainly not exclusive to our physicians, it is likely that others elsewhere share their wariness of formalized programs.
No attempt was made to validate respondents’ experiences, but given that it is the perception of an event that drives an individual’s need for support rather than an objective measure, we do not feel such confirmation offers any incremental value.
Our survey was unable to attribute specific barriers to particular services. Nevertheless, assuming – conservatively – that physicians’ concerns regarding confidentiality and stigma are pervasive across support mechanisms, we believe it is possible to design a support mechanism that addresses many, if not all, of these concerns. As the most desired potential sources of support are other physicians, a result corroborated by other studies13, 18, 33, 53, we advocate for a peer-based system of support. Indeed, among our respondents, those with prior stressful experiences – presumably our target population – were even more likely to choose physician colleagues.
Redesign of the Peer Support Team Program
Given the prevalence of concerns regarding stigma and confidentiality in our population, it is unsurprising that physicians are reluctant to utilize EAP-organized group support. Despite the fact that these sessions are conducted confidentially and without documentation, the program does maintain ties to an institutional structure with which many physicians are unfamiliar. The mere presence of other members of the healthcare team is likely uncomfortable for physicians; they are accustomed to assuming a leadership role within these teams, rather than one of a true peer. As our survey illustrates, physicians seek support from other physicians. We posit that the most effective physician support system involves peers who have the unique qualification of having “been there” with experiences such as errors and/or litigation.
In 2009, we instituted a one-on-one, physician-to-physician peer support program. Since that time, over 30 physicians have been trained. To ensure that these individuals are approachable to those that need them, we have transitioned from a selection process of appointment to one of nomination. Invitations to undergo peer support training are now offered to (and accepted by) a range of people who have been suggested by their fellow residents and faculty members.
Following notification by clinician colleagues, Risk Management, or EAP, a physician peer supporter makes an outreach call to each of the individual physicians involved in an adverse event, and one-on-one support is offered. In partnership with the hospital’s Risk Management office and Controlled Risk Insurance Company (CRICO), our medical malpractice insurer, we also provide training and support services for the disclosure of medical errors. If and when legal complaints are filed, Peer Support is notified by Risk Management, and defendant clinicians are put in contact with senior physicians who have experienced the litigation process and are able to provide support.
Conclusions
The culture of an institution may be both the cause and the victim of moral distress54. Thus, an operational support system requires a visible commitment from leadership as well as a predictable, organized infrastructure55. We explicitly support a culture of trust at our hospital, predicated on mutual respect for individuals, teams, and the institution; we hold a basic assumption that everyone is trying to do his or her best. In establishing the Peer Support Team, we set out to strengthen that culture of trust by supporting providers at their most vulnerable moments, protecting them against burnout and emotional impairment. When the first iteration of the PST program demonstrated an inadequacy in reaching physicians, we used the survey data presented here to expand the program and address their unique concerns. We anticipate that this programmatic reform – novel in its use of physician-provided services, both on a one-on-one and a group basis – will increase our presence within the hospital. Only by becoming part of the normal social fabric may we hope to penetrate this “conspiracy of silence”29 surrounding physician distress and to, ultimately, help each other heal.
Acknowledgments
Study concept and design: Fix, Weissman, and Shapiro.
Acquisition of data: Fix, Hevelone, and Shapiro.
Analysis & interpretation of data: Hu, Hevelone, Lipsitz, Greenberg, Weissman, and Shapiro.
Drafting of manuscript: Hu, Greenberg, and Shapiro.
Critical revision of manuscript for important intellectual content: Hu, Fix, Hevelone, Lipsitz, Greenberg, Weissman, and Shapiro.
Statistical expertise: Hevelone and Lipsitz.
Administrative, technical, or material support: Greenberg and Shapiro.
Supervision: Greenberg, Weissman, and Shapiro.
Footnotes
Prior Presentations:
New England Surgical Society 91st Annual Meeting, Saratoga Springs, NY, October 30, 2010
Financial Disclosure: None reported.
References
- 1.Troppmann KM, Palis BE, Goodnight JE, Ho HS, Troppmann C. Career and lifestyle satisfaction among surgeons: what really matters? The National Lifestyles in Surgery Today Survey. J Am Coll Surg. 2009 Aug;209(2):160–169. doi: 10.1016/j.jamcollsurg.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Leigh JP, Kravitz RL, Schembri M, Samuels SJ, Mobley S. Physician career satisfaction across specialties. Arch Intern Med. 2002 Jul 22;162(14):1577–1584. doi: 10.1001/archinte.162.14.1577. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009 Sep;250(3):463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 4.Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006 Mar;44(3):234–242. doi: 10.1097/01.mlr.0000199848.17133.9b. [DOI] [PubMed] [Google Scholar]
- 5.Williams ES, Konrad TR, Scheckler WE, et al. Understanding physicians’ intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical health. Health Care Manage Rev. 2001 Winter;26(1):7–19. doi: 10.1097/00004010-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, West CP, Sloan JA, et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009 May 25;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 7.Campbell DA, Jr, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001 Oct;130(4):696–702. doi: 10.1067/msy.2001.116676. discussion 702–695. [DOI] [PubMed] [Google Scholar]
- 8.Kuhn G, Goldberg R, Compton S. Tolerance for uncertainty, burnout, and satisfaction with the career of emergency medicine. Ann Emerg Med. 2009 Jul;54(1):106–113. e106. doi: 10.1016/j.annemergmed.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 9.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001 Aug;111(2):170–175. doi: 10.1016/s0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 10.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. Bmj. 2008 Mar 1;336(7642):488–491. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work-home conflicts and burnout among american surgeons: a comparison by sex. Arch Surg. 2011 Feb;146(2):211–217. doi: 10.1001/archsurg.2010.310. [DOI] [PubMed] [Google Scholar]
- 12.Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997 Apr;44(7):1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- 13.Engel KG, Rosenthal M, Sutcliffe KM. Residents’ responses to medical error: coping, learning, and change. Acad Med. 2006 Jan;81(1):86–93. doi: 10.1097/00001888-200601000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Hughes PH, Conard SE, Baldwin DC, Jr, Storr CL, Sheehan DV. Resident physician substance use in the United States. JAMA. 1991 Apr 24;265(16):2069–2073. [PubMed] [Google Scholar]
- 15.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003 Jun 18;289(23):3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 16.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011 Jan;146(1):54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 17.Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: a prospective study. Lancet. 2002 Apr 20;359(9315):1373–1378. doi: 10.1016/S0140-6736(02)08350-2. [DOI] [PubMed] [Google Scholar]
- 18.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. Jama. 2006 Sep 6;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 19.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. Jama. 2009 Sep 23;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and Medical Errors Among American Surgeons. Ann Surg. 2009 Nov 19; doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 21.Melville A. Job satisfaction in general practice: implications for prescribing. Soc Sci Med Med Psychol Med Sociol. 1980 Dec;14A(6):495–499. doi: 10.1016/0160-7979(80)90050-8. [DOI] [PubMed] [Google Scholar]
- 22.Shanafelt TD, West C, Zhao X, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005 Jul;20(7):559–564. doi: 10.1111/j.1525-1497.2005.0108.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bellini LM, Baime M, Shea JA. Variation of mood and empathy during internship. JAMA. 2002 Jun 19;287(23):3143–3146. doi: 10.1001/jama.287.23.3143. [DOI] [PubMed] [Google Scholar]
- 24.Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000 Feb;15(2):122–128. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DiMatteo MR, Sherbourne CD, Hays RD, et al. Physicians’ characteristics influence patients’ adherence to medical treatment: results from the Medical Outcomes Study. Health Psychol. 1993 Mar;12(2):93–102. doi: 10.1037/0278-6133.12.2.93. [DOI] [PubMed] [Google Scholar]
- 26.Crane M. Why burned-out doctors get sued more often. Med Econ. 1998 May 26;75(10):210–212. 215–218. [PubMed] [Google Scholar]
- 27.Misra-Hebert AD, Kay R, Stoller JK. A review of physician turnover: rates, causes, and consequences. Am J Med Qual. 2004 Mar–Apr;19(2):56–66. doi: 10.1177/106286060401900203. [DOI] [PubMed] [Google Scholar]
- 28.Leigh JP, Tancredi DJ, Kravitz RL. Physician career satisfaction within specialties. BMC Health Serv Res. 2009;9:166. doi: 10.1186/1472-6963-9-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009 Nov 14;374(9702):1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 30.Scheurer D, McKean S, Miller J, Wetterneck T. U.S. physician satisfaction: a systematic review. J Hosp Med. 2009 Nov;4(9):560–568. doi: 10.1002/jhm.496. [DOI] [PubMed] [Google Scholar]
- 31.Sangi-Haghpeykar H, Ambani DS, Carson SA. Stress, workload, sexual well-being and quality of life among physician residents in training. Int J Clin Pract. 2009 Mar;63(3):462–467. doi: 10.1111/j.1742-1241.2008.01845.x. [DOI] [PubMed] [Google Scholar]
- 32.Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009 Apr;144(4):371–376. doi: 10.1001/archsurg.2008.575. [DOI] [PubMed] [Google Scholar]
- 33.Yeo H, Viola K, Berg D, et al. Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. JAMA. 2009 Sep 23;302(12):1301–1308. doi: 10.1001/jama.2009.1386. [DOI] [PubMed] [Google Scholar]
- 34.Spickard A, Jr, Gabbe SG, Christensen JF. Mid-career burnout in generalist and specialist physicians. Jama. 2002 Sep 25;288(12):1447–1450. doi: 10.1001/jama.288.12.1447. [DOI] [PubMed] [Google Scholar]
- 35.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003 Apr 15;114(6):513–519. doi: 10.1016/s0002-9343(03)00117-7. [DOI] [PubMed] [Google Scholar]
- 36.Cole TR, Carlin N. The suffering of physicians. Lancet. 2009 Oct 24;374(9699):1414–1415. doi: 10.1016/s0140-6736(09)61851-1. [DOI] [PubMed] [Google Scholar]
- 37.Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C. Calibrating the physician. Personal awareness and effective patient care. Working Group on Promoting Physician Personal Awareness, American Academy on Physician and Patient. JAMA. 1997 Aug 13;278(6):502–509. doi: 10.1001/jama.278.6.502. [DOI] [PubMed] [Google Scholar]
- 38.McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: is there hope? Fam Med. 2008 Oct;40(9):626–632. [PMC free article] [PubMed] [Google Scholar]
- 39.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. Jama. 2009 Sep 23;302(12):1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 40.Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med. 2007 Nov;22(11):1544–1552. doi: 10.1007/s11606-007-0363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shapiro SL, Shapiro DE, Schwartz GE. Stress management in medical education: a review of the literature. Acad Med. 2000 Jul;75(7):748–759. doi: 10.1097/00001888-200007000-00023. [DOI] [PubMed] [Google Scholar]
- 42.van Pelt F. Peer support: healthcare professionals supporting each other after adverse medical events. Qual Saf Health Care. 2008 Aug;17(4):249–252. doi: 10.1136/qshc.2007.025536. [DOI] [PubMed] [Google Scholar]
- 43.Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care. 2009 Oct;18(5):325–330. doi: 10.1136/qshc.2009.032870. [DOI] [PubMed] [Google Scholar]
- 44.Wears RL, Wu AW. Dealing with failure: the aftermath of errors and adverse events. Ann Emerg Med. 2002 Mar;39(3):344–346. doi: 10.1067/mem.2002.121996. [DOI] [PubMed] [Google Scholar]
- 45.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. Bmj. 2000 Mar 18;320(7237):726–727. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aasland OG, Forde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Qual Saf Health Care. 2005 Feb;14(1):13–17. doi: 10.1136/qshc.2002.003657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Newman MC. The emotional impact of mistakes on family physicians. Arch Fam Med. 1996 Feb;5(2):71–75. doi: 10.1001/archfami.5.2.71. [DOI] [PubMed] [Google Scholar]
- 48.Wu AW, Folkman S, McPhee SJ, Lo B. How house officers cope with their mistakes. West J Med. 1993 Nov;159(5):565–569. [PMC free article] [PubMed] [Google Scholar]
- 49.Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf. 2007 Aug;33(8):467–476. doi: 10.1016/s1553-7250(07)33050-x. [DOI] [PubMed] [Google Scholar]
- 50.Thompson WT, Cupples ME, Sibbett CH, Skan DI, Bradley T. Challenge of culture, conscience, and contract to general practitioners’ care of their own health: qualitative study. Bmj. 2001 Sep 29;323(7315):728–731. doi: 10.1136/bmj.323.7315.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gross CP, Mead LA, Ford DE, Klag MJ. Physician, heal Thyself? Regular source of care and use of preventive health services among physicians. Arch Intern Med. 2000 Nov 27;160(21):3209–3214. doi: 10.1001/archinte.160.21.3209. [DOI] [PubMed] [Google Scholar]
- 52.Devencenzi T, O’Keefe J. To err is human: supporting the patient care provider in the aftermath of an unanticipated adverse clinical outcome. Int J Emerg Ment Health. 2006 Spring;8(2):131–135. [PubMed] [Google Scholar]
- 53.Wallace JE, Lemaire J. On physician well being-you’ll get by with a little help from your friends. Soc Sci Med. 2007 Jun;64(12):2565–2577. doi: 10.1016/j.socscimed.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 54.Nelson WA, Beyea SC. The role of an ethical culture for the prevention and recovery of “second victims”. Qual Saf Health Care. 2009 Oct;18(5):323–324. doi: 10.1136/qshc.2009.034843. [DOI] [PubMed] [Google Scholar]
- 55.Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf. 2010 May;36(5):233–240. doi: 10.1016/s1553-7250(10)36038-7. [DOI] [PubMed] [Google Scholar]