Abstract
Background
Patterns of heroin and cocaine use vary and may be associated with unique risk factors for bloodborne infections.
Methods
Latent class analysis identified sub-populations of 552 heroin and cocaine users in Baltimore, Maryland. Using latent class regression, these classes were analyzed for associations with demographic characteristics, risky behaviors, Hepatitis C, and HIV.
Results
Three classes were found: Crack / Nasal-Heroin users (43.5%), Polysubstance users (34.8%), and Heroin Injectors (21.8%). Compared to Polysubstance users, Crack / Nasal-Heroin users were almost 7 times more likely to identify as Black (OR = 6.97, 95% CI = 4.35-11.2). Sharing needles was over 2.5 times more likely among Polysubstance users than among Heroin Injectors (OR = 2.66, 95% CI = 1.49-4.75). Crack/Nasal-Heroin users were 2.5 times more likely than Polysubstance users to exchange drugs for sex (OR = 2.50, 95% CI = 1.22-5.13). Crack/Nasal-Heroin users were less likely than Heroin Injectors to have Hepatitis C (OR = 0.10, 95% CI = 0.06-0.18), but no significant differences were found for HIV.
Conclusions
Subpopulations of cocaine and heroin users differed in demographic classifications, HIV-risk behaviors, and Hepatitis C infection. All subpopulations included substantial numbers of HIV-positive individuals. Findings provide further evidence that non-injection drug users face significant infectious disease risk.
Keywords: Cocaine, heroin, polydrug, injection, sex trade, HIV/AIDS
1. Introduction
Heroin and cocaine use costs society billions due to healthcare, lost productivity, and crime (Cartwright, 2000; Mark et al., 2001). Heroin and cocaine users are overlapping populations; i.e., many individuals who use heroin also use cocaine. Rates of cocaine use range from 30-80% among opioid-dependent substance users not currently in treatment and from 50-73% among patients in methadone treatment (Leri et al., 2003). Either substance can be injected, leading to a greater potential for harm. Injection drug use (IDU) alone is attributable to over 2.5 billion dollars of healthcare costs due to Acquired Immunodeficiency Disease Syndrome (AIDS) and over half a billion dollars due to Hepatitis C (Mark et al., 2001). The link between non-injection drug use (NIDU) and infectious disease is also strong, but an understanding of the mechanism driving this association is more nebulous (Drumright and Colfax, 2009). IDU is believed to be associated with infectious diseases due to sharing of needles, but multiple pathways have been suggested for how NIDU may influence disease status. There is a paucity of research investigating patterns of drug use among heavy drug users, including NIDU, and how these patterns relate to infectious disease. The current study seeks to fill this gap by exploring patterns of drug use among a sample of heroin and/or cocaine users from Baltimore, Maryland using Latent Class Analysis. These latent classes are examined in depth for relationships with risky behaviors and infectious diseases.
1.1. Patterns of drug use
Patterns of heroin and cocaine use vary dramatically among different populations. For example, in the United States (US), the simultaneous injection of heroin and cocaine, referred to as a “speedball,” is relatively common. Over 18% of illicit drug users in Miami, Florida used speedball in the last 30 days (McCoy et al., 2004) in comparison to less than 4% in Canada (Leri et al., 2004). On the other hand, crack cocaine is typically smoked in the US and rarely injected (Substance Abuse and Mental Health Services Administration, 2009), but in the United Kingdom, crack cocaine injection is a primary form of drug administration (Hickman et al., 2007). Patterns of heroin and cocaine use also vary in different historical contexts. Present-day diverse patterns of opioid and cocaine polydrug use are in stark contrast with mid-20th Century conceptions of heroin addicts focused nearly exclusively on illegal heroin use (Courtwright, 1982; Lindesmith, 1947; Monga et al., 2007).
The various patterns of drug use and routes of administration (ROAs) are associated with unique health consequences (Gossop et al., 1992; Strang et al., 1998). Smoking of cigarettes and other substances by drug users is associated with substantial adverse outcomes including medical complaints and higher mortality rates (Hser et al., 1994; Hurt et al., 1996; Patkar et al., 2005; Patkar et al., 2002; Strang et al., 1999). Smoking crack cocaine, as opposed to nasal use, is associated with increased risk of dependence (Chen and Anthony, 2004). IDU is associated with increased risk for drug dependence (Gossop et al., 1994; Strang et al., 1999) and overdose (Gossop et al., 1996).
1.2. Relationships with infectious diseases
Infectious diseases such as Human Immunodeficiency Virus (HIV) are potential consequences of drug use. In particular, IDU is known to be associated with HIV and hepatitis C infection (Chitwood et al., 2003; Nelson et al., 2002). NIDU can also be a risk factor for HIV. For example, alcohol (Hutton et al., 2008) and marijuana (Boyer et al., 2000; Boyer et al., 1999) use are both associated with increased risk for sexually transmitted diseases (STD’s). A recent comprehensive chapter on HIV risk and prevention for NIDU noted that most published studies on HIV and opioids fail to distinguish non-injection from injection opioid use (Drumright and Colfax, 2009). The relatively few studies demonstrate high rates of infectious disease among non-injection heroin users (Ferreira et al., 2009; Rich et al., 2006; Vallejo et al., 2008). Further investigation is warranted to understand the nature of the association between NIDU and infectious disease.
One difficulty in understanding this association is the wide range of substance use patterns. Since substance users often use a variety of drugs by different ROAs, focusing on individual drugs may be difficult or lack real-world generalizability. Examinations of patterns of drug use may be a more productive approach. In contrast to an approach focusing on variables of interest, such as particular drugs or ROAs, Latent Class Analysis (LCA) is an effective person-centered approach for identifying subpopulations empirically. Effective use of LCA has allowed for furthering our understanding of the development of cocaine dependence (Reboussin and Anthony, 2006), drug abuse and dependence in the US general population (Agrawal et al., 2007), ecstasy use problems (Martins et al., 2011; Scheier et al, 2008), and patterns of drug use among cocaine and heroin users in Canada (Monga et al., 2007; Patra et al., 2009). However, until quite recently (Kuramoto et al., 2011), there appeared to be no published LCA identifying classes of heroin and cocaine use patterns in the US. Patterns of drug use in the US differ in important ways from those in Canada. For example, prior LCA research did not investigate speedball use due to the low prevalence rates in Canada (Monga et al., 2007; Patra et al., 2009). Further, prior research in the United States did not specifically investigate risky sexual behaviors (Kuramoto et al., 2011). This study addresses these critical gaps in the literature by using LCA to identify specific polydrug use patterns in heroin and cocaine users and examine how these classes relate to risky behaviors and infectious diseases, specifically Hepatitis C and HIV. We expected that, although infectious disease would be relatively high in all classes, classes using more substances, particularly via injection routes, would also engage in more risky behaviors, resulting in higher rates of Hepatitis C and HIV.
2. Methods
2.1. Participants and design
The present study sample consisted of 552 self-identified Black and White adult drug users in Baltimore, Maryland, United States, from the NEURO-HIV Epidemiologic study, a longitudinal investigation funded by the National Institute on Drug Abuse to evaluate neuropsychological and social-behavioral risk factors of contracting infectious diseases among injection and non-injection drug users (Severtson et al., 2010a). Recruitment involved advertisements in local newspapers, referrals, and street outreach. To be eligible for the study, participants needed to report using cocaine or heroin in the past 6 months and be between 18 and 50 years old. Upon arrival, participants provided informed consent, received blood tests, gave urine samples, and completed the HIV-Risk Behavior Interview, a semi-structured interview about drug use and sexual practices. This interview was adapted from a similar interview used for the REACH study and included questions on demographic variables in addition to medical, education, and neurodevelopment histories (Strathdee and Sherman, 2003). The study was approved and monitored by the Institutional Review Board at the Johns Hopkins Bloomberg School of Public Health. Demographic characteristics are presented in Table 1. The sample included 321 men (58%) and 231 women (42%). Half self-identified as Black (n=276) and the other half self-identified as White (n=276).
Table 1.
Characteristics of 552 users of cocaine and/or heroin in the past 6 months.
| n | % | |
|---|---|---|
| Latent Class Indicators1 | ||
| Cigarettes | 504 | 91.3 |
| Alcohol | 329 | 59.6 |
| Heroin – injection | 292 | 52.9 |
| Crack cocaine – smoking | 237 | 43.0 |
| Marijuana – smoking | 202 | 36.7 |
| Heroin – nasal | 203 | 36.9 |
| Cocaine – injection | 168 | 30.5 |
| Heroin and cocaine together (“Speedball”) – injection | 157 | 28.4 |
| Demographics | ||
| Over 33 years old | 288 | 52.2 |
| Female gender | 231 | 41.8 |
| Black race | 276 | 50.0 |
| HIV/HCV Risk Behaviors | ||
| Lifetime polydrug use | 306 | 55.8 |
| Smokes 20+ cigs per day | 269 | 48.8 |
| Positive for opioids | 323 | 66.9 |
| Positive for cocaine | 268 | 55.5 |
| Shared needle in lifetime | 188 | 35.4 |
| Sold drugs for sex | 57 | 10.6 |
| Disease Status | ||
| Hepatitis C | 248 | 50.9 |
| HIV | 43 | 8.5 |
These variables refer to substances used in the past month.
2.2. Measures
2.2.1. Latent class indicators
Table 1 notes all routes of administration (ROAs) and substances used in the past month by 20% or more of the sample. Past month substance use is often used as a variable of interest in substance abuse research (Monga et al., 2007) including national surveys, such as Monitoring the Future (Johnston et al., 2002). Although not without limitations, this measure avoids being over too long a length of time to result in unreliable memory as well as including a long enough time span to avoid incorrect categorizations due to random, recent events (e.g., short periods of abstinence coinciding with research interview despite typical patterns of use). Prior research used 20% as a cut-off (Monga et al., 2007). Over a quarter (28.4%) of the sample used speedball in the past month. However, the next most prevalent category, “Downers,” a composite group including barbiturates and sedatives, was only used by 14.5% of the sample. Notably, less than 1% of this Baltimore sample used stimulant drugs more common in other geographical areas, such as amphetamines. Thus, we chose to use the methodology from the prior published study. The eight indicators chosen based on 20% or higher prevalence were as follows: alcohol, cigarettes, injecting speedball, injecting heroin, snorting heroin, injecting cocaine, smoking crack, and smoking marijuana.
2.2.2. Demographics, HIV-risk behaviors, and disease status
Demographic and drug use variables were used to examine characteristics of individuals within classes and to elucidate the general meaning of the classes. Dichotomous variables were used for ease of interpretation. Based on a median age of 33, substance users were divided into those over 33 years old and those 33 years old or younger. Behaviors and environments associated with infectious disease risk, and thus examined in analysis, include drug use (Drumright and Colfax, 2009), jail (Jurgens et al., 2009), needle sharing (Chitwood et al., 2003; Nelson et al., 2002) and sexual risk behaviors (Jenness et al., 2011). Cigarette smoking was included as well, primarily due to its association with increased mortality (Pines et al., 2011), but also due to the remote possibility that it may be a risk factor for HIV (Marshall et al., 2009). Casual sex was defined as having sex with someone for less than 3 months, including one-night stands, but not transactional sex. For drug use, separate questions were asked for each substance based on ROA. Questions regarding injection of heroin, for example, were asked separately from questions regarding snorting of heroin. There were a total of 63 substance-ROA pairs. The median number of substances used in an individual’s lifetime was 8. Thus, individuals who used over 8 substances in their lifetime were labeled “Lifetime Polydrug Use.” Urinalysis results included cocaine and opioid use. In addition, we included items from the interview regarding lifetime history of incarceration, any diagnosis of a psychiatric disorder, injection drug use, needle sharing, and exchanging drugs for sex. Disease status for Hepatitis C or HIV was determined via blood samples.
2.3. Statistical analysis
Latent class analysis (LCA) was used to examine profiles of substance use. LCA is a statistical method in which several items (or indicators) are used to determine subgroups or classes of individuals who exhibit a similar pattern of responses (McCutcheon, 1987; Whitesell et al., 2006). LCA assumes that the class structure accounts for the similar reporting by individuals on the indicator variables within each class (Reboussin et al., 2006). Responses to the indicator variables are statistically independent conditional on class membership (Lazarsfeld and Henry, 1968; McCutcheon, 1987; Reboussin et al., 2006), i.e., the class membership explains any association between the reported indicators (Lazarsfeld and Henry, 1968; McCutcheon, 1987; Reboussin et al., 2006). The resulting assumption permits that classes are interpreted as homogenous and distinct from each other and that within any class the item reporting patterns differ only by random error (McCutcheon, 1987; Reboussin et al., 2006).
The eight drug use indicator variables were entered into the LCA model. Starting with a one class model and incrementally increasing the number of classes, a series of LCA models were fit to the data. In order to ensure that global, rather than local, maxima were reached, we used a minimum of 500 random starts. If necessary, the number of starts was increased until the log likelihood was replicated a minimum of five times. Multiple fit statistics were used to determine the best-fitting, most parsimonious model, including the Bayesian Information Criteria (BIC; Schwartz, 1978), the parametric bootstrap likelihood ratio test (BLRT; McLachlan and Peel, 2000), and the Lo-Mendell-Rubin adjusted likelihood ratio test (LMR; Lo et al., 2001).
The value and utility of the resultant classes was assessed using entropy (Ramaswamy et al., 1993). Entropy uses individual estimated posterior probabilities to summarize the degree to which the latent classes are distinguishable and the precision of assignment of individuals into classes. It ranges from 0 to 1 with higher values indicating better class separation. Entropy is not a measure of fit, nor was it originally intended for model selection; however, low values of entropy may indicate that the model is failing to find homogeneous groupings of individuals with distinct profiles. Finally, the choice of latent class solution presented was also informed by substantive criteria, such as meaningfulness in terms of the current epidemiology of drug use. The n reported in each class is a total based on individual probabilities of class membership, i.e., a number ranging from 0.0, or no chance of membership in that specific class for that specific individual, and 1.0, or 100% certainty of class membership. Thus, these numbers are decimals, rather than whole numbers. Mplus version six was used for the LCA modeling (Muthén and Muthén, 2010).
2.4. Missing data
Mplus uses a full information maximum likelihood estimation with the assumption the data is missing at random (MAR; Hogan et al., 2004). This approach is widely accepted (Schafer and Graham, 2002). No participants needed to be removed due to missing data on latent class indicators. Covariance coverage ranged from 0.993-1.0, well over minimum thresholds for adequate coverage (e.g., .10, Muthén and Muthén, 2010).
2.5. Class associations
After deciding on the appropriate number of classes that best fit the data, we examined the association between class membership and several demographic and predictor variables as well as outcomes utilizing the auxiliary option (Bandeen-Roche et al., 1997; Muthén and Asparouhov, 2007; Wang et al., 2005). This option was used to study the association of classes with demographics, hiv-risk behaviors, and disease status without changing the unconditional latent class model (Muthén and Muthén, 2010). The AUXILIARY (r) option was used to examine which covariates are important predictors of latent classes. This is done using posterior-probability based multinomial logistic regression of a categorical latent variable on a set of covariates. For disease status, we adjusted results for age, sex, and race. The AUXILIARY (e) option was used to examine the extent to which HIV status varied as a function of latent class membership by testing the equality of means across latent classes using posterior probability-based multiple imputations. Percentages obtained are reported with standard errors based on probabilities of class membership.
In summary, the use of auxiliary information, potentially derived from substantive theory, is highly relevant to determine the concurrent and prognostic validity of specific latent class profiles. The inclusion of auxiliary information in mixture analysis is a necessary step in understanding as well as evaluating the fidelity and utility of the resultant profiles (Petras and Masyn, 2010 ).
3. Results
3.1. Class Membership
A latent class model consisting of three classes was selected as it had the lowest Bayesian Information Criteria (BIC) score, 5029.94 (see Table 2). The Lo-Mendell-Rubin (LMR) adjusted likelihood ratio test and Bootstrap Likelihood Ratio Test (BLRT) also supported a 3-class solution, although the ideal solutions for the LMR and BLRT were 4-class and 5-class, respectively. Thus, out of the three main fit indices, a 3-class model was supported by all 3 indices. Although Monte Carlo simulations suggest that a BLRT fares best overall in LCA, simulations also favor the BIC over the AIC and, in certain situations, over the Adjusted BIC (Nylund et al., 2007). Further, the relative frequency was lower for the 4-class and 5-class solutions, which indicates concern about wide confidence intervals for the regression coefficients (Petras and Masyn, 2010). Thus, based on concerns of parsimony, practical utility, and theoretical concerns, we chose the 3-class model presented. For reference, the four class model included a separate class with high probabilities for injection drug use, but a 0% probability for snorting of heroin. In addition, there was a 0% probability for smoking crack among a class with high probabilities for injecting heroin. In the five class model, a class with a 100% probability of injecting heroin, but 0 % probability for injecting cocaine was found. In addition, there was a class with about a 50% probability of injecting heroin, but a 0 % probability for snorting heroin or smoking crack.
Table 2.
Fit statistics and entropy for a latent class analysis of 8 substances used in the past month among 552 users of cocaine and heroin in the past 6 months.
| Classes | LLa | parameters | BICb | LMRc | BLRTd | Entropy | s.c. r.f. (f)e |
|---|---|---|---|---|---|---|---|
| 1 | −2685.88 | 8 | 5422.27 | NAf | NAf | NAf | NAf |
| 2 | −2486.57 | 17 | 5080.47 | p < .001 | p < 0.001 | 0.769 | .49 (268.2) |
| 3 | −2432.89 | 26 | 5029.94 | p = .002 | p < 0.001 | 0.742 | .22 (120.1) |
| 4 | −2417.04 | 35 | 5055.06 | p = .028 | p < 0.001 | 0.744 | .13 (70.3) |
| 5 | −2402.25 | 44 | 5082.29 | p = .147 | p < 0.001 | 0.784 | .08 (44.1) |
| 6 | −2395.05 | 53 | 5124.71 | p = .591 | p = 0.600 | 0.796 | .05 (26.4) |
Log Likelihood;
Bayesian Information Criteria;
Lo-Mendell-Rubin adjusted likelihood ratio test;
parametric Bootstrap Likelihood Ratio Test;
smallest class relative frequency (frequency);
Not Applicable
Ideal number of classes based on fit statistic shown in bold.
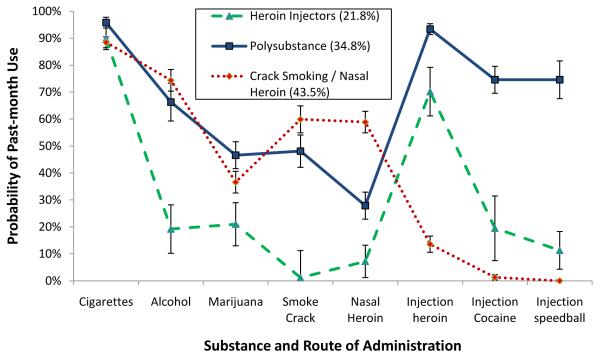
Class 1, consisting of 43.5% (n = 240.1) of the sample, was composed of individuals with high (over 50 %) probabilities of cigarette smoking, drinking alcohol, snorting heroin, and smoking crack. Probabilities for any type of injection use in this sample did not exceed 14%. Snorting heroin and crack smoking is higher in this group than any other group, so we refer to this group as Crack/Nasal-Heroin users. In contrast, class 2, over a third of the sample (34.8%), n = 191.8, had relatively high probabilities (> 45%) for every indicator except nasal heroin. This class is thus referred to as Polysubstance. The final class, representing a little over a fifth (21.8%) of the sample, n = 120.1, had high probabilities of cigarette smoking and heroin injection, but relatively low (less than 25%) probabilities of all other indicators. This third class is referred to as Heroin Injectors. See Figure 1.
Figure 1.
Three class solution of a latent class analysis of 552 users of cocaine and/or heroin in Baltimore, MD. Estimated probabilities for past-month drug use are graphed based on latent class membership. Error bars indicate standard errors of estimated probabilities.
3.2. Characteristics of classes
3.2.1. Demographics
Table 3 provides odds ratios and 95% confidence intervals comparing latent classes on demographics, HIV-risk behaviors, and disease status. Analyses of demographic variables found significant class-level differences for all demographic variables examined (see Table 3). Individuals in the Crack/Nasal-Heroin group were almost two times more likely to be in the over 33 years old age group as compared to Heroin Injectors and 2.5 times more likely as compared to Polysubstance users. These individuals with high probabilities of crack smoking and heroin snorting were over 5.5 times as likely to identify themselves as Black compared to both Heroin Injectors and Polysubstance users .
Table 3.
Association between latent class membership and characteristics of heroin and cocaine users in Baltimore, MD.1
| Polysubstance vs. Heroin Injectors |
Crack/Nasal-H. vs. Heroin Injectors |
Crack/Nasal-H. vs. Polysubstance |
|
|---|---|---|---|
| Demographics | |||
| Over 33 years old | 0.78 (0.46-1.33) | 1.93 (1.17-3.19)* | 2.48 (1.62-3.81)*** |
| Female gender | 0.68 (0.40-1.16) | 1.14 (0.69-1.90) | 1.68 (1.11-2.54)* |
| Black race | 0.80 (0.45-1.43) | 5.60 (3.18-9.84)*** | 6.97 (4.35-11.2)*** |
| HIV/HCV Risk Behaviors | |||
| Lifetime polydrug use | 4.01 (2.23-7.23)*** | 0.74 (0.45-1.24) | 0.19 (0.11-0.30)*** |
| Smokes 20+ cigs per day | 1.36 (0.80-2.31) | 0.48 (0.29-0.79)** | 0.35 (0.23-0.53)*** |
| Positive for opioids | 1.70 (0.85-3.40) | 0.43 (0.24-0.80)** | 0.25 (0.15-0.42)*** |
| Positive for cocaine | 3.25 (1.74-6.08)*** | 1.78 (1.00-3.18)* | 0.55 (0.35-0.86)* |
| Psychiatric disorder | 1.02 (0.59-1.77) | 0.95 (0.63-1.43) | 0.93 (0.56-1.55) |
| Jail | 0.70 (0.40-1.24) | 0.76 (0.48-1.19) | 1.07 (0.61-1.89) |
| Shared needle in lifetime | 2.66 (1.49-4.75)** | 0.15 (0.07-0.30)*** | 0.06 (0.03-0.10)*** |
| Casual sex | 1.97 (1.01-3.83)* | 1.09 (0.56-2.10) | 0.55 (0.33-0.91)* |
| Sold sex | 1.00 (0.54-1.86) | 0.96 (0.53-1.75) | 0.96 (0.59-1.56) |
| Paid for sex | 1.50 (0.63-3.55) | 2.22 (0.98-5.06)† | 1.48 (0.85-2.58) |
| Drugs for sex | 1.19 (0.38-3.65) | 2.97 (1.07-8.21)* | 2.50 (1.22-5.13)* |
| Disease Status2 | |||
| Hepatitis C | 0.72 (0.38-1.34) | 0.10 (0.06-0.18)*** | 0.14 (0.07-0.29)*** |
| HIV | 0.94 (0.32-2.73) | 0.57 (0.25-1.31) | 0.61 (0.22-1.69) |
p=0.057
p ≤ .05
p < .01
p < .001
Associations are given as odds ratios with 95% confidence intervals in parentheses.
Adjusted for Demographics
3.2.2. HIV-risk behaviors
As expected, Polysubstance users were more likely to report “Lifetime Polydrug Use” than Heroin Injectors. Urinalysis results supported the class structures. As compared to Heroin Injectors, Crack/Nasal-Heroin users were more likely to test positive for cocaine, but less likely to be positive for opioids. Polysubstance users were over 2.5 times more likely to share needles as compared to Heroin Injectors. Crack/Nasal-Heroin users were much less likely to share needles compared to both Heroin Injectors and Polysubstance users, but 2.5 times more likely to have sold drugs for sex as compared to Polysubstance users and nearly 3 times more likely than Heroin Injectors. To more fully understand the lifetime, as opposed to past 30 day, histories of the Crack/Nasal-Heroin users, we used most likely class membership to examine lifetime history of injection drug use. Only 36.6% of members of this class injected any drugs in their lifetime.
3.2.3. Disease Status
There were no differences in the significant relationships reported here whether or not we adjusted for demographic differences. Crack/Nasal-Heroin users were less likely to have Hepatitis C as compared to both Heroin Injectors and Polysubstance users. There were no significant associations between latent class membership and HIV status. Since this was unexpected, we investigated the equality of means across classes. Although the differences were not significant, χ2 (degrees of freedom=2) = 0.20, p = 0.86, the percentage of HIV-positive individuals was higher in the Crack/Nasal-Heroin class (9.3%, Standard Error = 2.0) than in either the Polysubstance class (7.8%, SE = 2.2) or the Heroin Injectors class (7.7%, SE = 2.9).
4. Discussion
4.1 Review of Major Findings
Overall, our findings are consistent with research demonstrating high rates of infectious diseases among cocaine and heroin users (Buchacz et al., 2000; Chitwood et al., 2003; Drumright and Colfax, 2009; Ferreira et al., 2009; Kuo et al., 2004; Rich et al., 2006; Vallejo et al., 2008). Due to differing recruitment strategies, indicator variables, and other issues, it is difficult - if not impossible - to compare results of prior latent class analyses. Nonetheless, some patterns can be noted. The three classes identified in the analysis are in some ways consistent with prior research (Kuramoto et al, 2011; Monga et al., 2007; Patra et al., 2009), although some notable differences emerged. The largest class included participants with relatively high probabilities of smoking crack and snorting heroin, but low probabilities of injection drug use (IDU). This differs from Canadian samples of opioid users wherein, although classes with low probabilities of IDU were identified, the majority of participants used via IDU (Monga et al., 2007; Patra et al., 2009). It resembles more closely a sample from Baltimore in finding classes with low probabilities of injection drug use (Kuramoto et al., 2011). The existence of these classes provide further evidence of an aversion to injection drug use among certain segments of the cocaine and heroin-using population who prefer other routes of administration (ROAs). The next largest class included participants with high probabilities of every substance and ROA except for nasal heroin. Injection heroin leads to a larger subjective “high” than nasal heroin (Comer et al., 1999), so individuals who are not resistant to injection are likely to prefer the injection route.
The smallest class, though still substantial at over one fifth of the sample, included individuals that almost exclusively used injection heroin. Although historically this pattern was considered a norm (Courtwright, 1982; Lindesmith, 1947), prior research suggested that this type of drug use may be rarer in this century (Monga et al., 2007). Indeed, recent Canadian samples demonstrated widespread cannabis, alcohol, and other drug use among heroin injectors (Monga et al., 2007; Patra et al., 2009). However, certain individuals may use heroin to self-medicate an underlying issue with aggression or rage (Khantzian, 1985, 1997) and thus prefer sedative effects over stimulative effects of drugs. This “self-medicating” type of individual may be in contrast to those who are more euphoria-seeking, as is likely the case with the Polysubstance or Crack/Nasal-Heroin users. Nevertheless, all classes likely have some euphoria-seeking qualities and all classes have some probability of using cocaine. Further research is needed to understand the underlying mechanisms for these patterns of use.
The classes in the current study showed distinct demographic differences. Crack/Nasal-Heroin users were more likely to self-report Black race, compared to the other 2 classes. This is consistent with findings that in the past decade, young White drug users in Baltimore were more likely than African-American substance users to inject drugs (Broz and Ouellet, 2008). Crack/Nasal-Heroin users were also more likely to be older than the other 2 classes. Research shows that African-American substance users often start illicit drug use later in their life than their White counterparts, which may partially explain this age effect (Green et al., 2010). Polysubstance users were less likely to be female than the other two classes. This supports research showing that, among individuals with opioid disorders in the US, men are more likely than women to have additional substance use disorders, although women appear more likely to have additional mental disorders (Grella et al., 2009). Given the demographic characteristics of the classes, it is perhaps not surprising that the Crack/Nasal-Heroin class smoked fewer cigarettes, as heavy smokers were previously found to be more likely to be White in this sample (Harrell et al., 2011) and among other illicit drug-using samples (Haas et al., 2008).
There were notable differences in behaviors relevant to increased risk of infectious diseases. Polysubstance users were more likely to share needles and engage in casual sex than Heroin Injectors, i.e., those with a high probability of heroin injection, but low probabilities of drinking alcohol or using cocaine. This suggests that polysubstance use is associated with an increased likelihood of risky behaviors. In contrast, Crack/Nasal-Heroin users were more likely to give someone drugs in exchange for sex. Given the severe substance use profiles of Polysubstance users and Heroin Injectors, this may be surprising, but consistent with research showing that transactional sex is associated with cocaine use to a greater extent than alcohol or injection heroin use (Jenness et al., 2011; Raj et al., 2007; Ross et al., 2003; Windle, 1997). Further research is needed to explain the mechanism driving this difference.
As expected, those who primarily used injection routes for drug administration were more likely to have Hepatitis C. Injection drug use is associated with increased risk of Hepatitis C and evidence suggests it is more transmissible via blood than HIV (Mehta et al., 2011; Sulkowski et al., 2002). The rates of HIV were not significantly different across the classes. The point estimates were actually lower among those who used via injection routes than those with low probabilities of injection use. A variety of possibilities exist for this negative finding. Slightly over a third (37%) of the class with low probabilities of IDU reported injecting drugs at some prior point in their lifetime, so it is possible this prior IDU resulted in HIV transmission. On the other hand, the increased rates of HIV among this class may be due to the increased rates of Black individuals. In 2007, the Center for Disease Control (CDC) estimated that over 65% of new HIV/AIDS cases between 2001 and 2005 were attributed to high-risk heterosexual contact for African-Americans, compared to less than 15% for Whites in the same time frame (CDC, 2008). Social network structure (Latkin et al., 2010) is a potential source of these disparities, particularly among African-American non-injection drug users (Kuo et al., 2011; Miller et al., 2007; Miller and Neaigus, 2002; Neblett et al., 2011; Pilowsky et al., 2007). In addition, novel harm minimization strategies aimed at reducing needle sharing and other risky injection practices (e.g., Tobin et al., 2011) may have reduced the risk of infection for IDU. Further research is needed.
The mechanism of infectious disease transmission among non-injection drug users is currently unclear. One possible explanation is that intoxication through the use of various substances may lead to a lack of attention to engaging in the practice of safe sex or a propensity toward engaging in high-risk sex (Castor et al., 2010; Strathdee and Sherman, 2003). Crack use, in particular, is associated with more risky sexual activities (Kuo et al., 2011; Miller et al., 2007). Although there is supportive evidence that illicit drug use leads directly to increased risky sexual behavior (Neaigus et al., 2001; Strathdee and Sherman, 2003), there is also contradictory evidence (for a review, see Drumright and Colfax, 2009). Thus, another possibility is that both the higher presence of sexually transmitted diseases and illicit drug use are explained by a third causal variable, such as desire for disengagement from risk awareness (McKirnan et al., 1996), impulsivity (Lejuez et al., 2005), personality disorder (Kokkevi et al., 1998), and/or cognitive factors (Mitchell et al., 2006). Heroin and cocaine users with cognitive deficits are more likely to have a history of Hepatitis B and/or C infection, supporting the idea that cognitive factors may lead to increased risky behaviors and thus transmission of infections (Severtson et al., 2010a; Severtson et al., 2010b). Further research, whether at a biochemical, behavioral, or sociological level, is needed to determine if cognitive factors or another mechanism are behind the association between illicit drug use, particularly crack, and risky sexual behaviors.
4.2 Limitations and strengths
There are some limitations to this study. The classic form of the latent class model assumes observed variables within each class to be independent. This assumption is questionable in many cases and the current study is no exception. For example, there may be some level of continuity of severity among the indicator variables, such that someone who injects heroin is more likely to also inject cocaine. Factor Mixture Models can be useful in addressing these concerns in future research (Lubke and Muthen, 2005). Nonetheless, LCA is a useful approach and helpful complement to other methods of classification across the Dimensional-Categorical spectrum (Masyn et al., 2010). In addition, if the classes truly represented only a ranking in severity, we would not expect profile classes to intersect, but yet we found the classes do intersect. As with all cross-sectional studies, no causal relationships can be established from the cross-sectional data presented. Associations noted may be due to confounding factors within the classes rather than directly due to the patterns of drug use observed. Longitudinal and experimental research may provide better answers to causal questions such as how drugs impact sexual activity. As the longitudinal data for this dataset recently became available, future research may explore this issue in more detail, including models to examine transition between classes.
Additionally, further research in other areas of the country is needed to see if our study results are generalizable outside of Baltimore, MD. It is possible, for example, that substance users with an exclusive focus on heroin injection may be a cultural factor specific to Baltimore. Also, data were obtained by self-report, which may be limited by memory biases or trust issues. The urinalysis data, however, is consistent with the findings presented, and self-report is generally recognized as relatively valid (Darke, 1998). The use of past 30 day substance use helps to reduce memory bias, but may miss important individual characteristics if patterns in the past month were atypical for the individual. Nonetheless, this is a commonly used method (Monga et al., 2007, Johnston et al., 2002).
Despite these limitations, there are several notable strengths to the current study. Prior latent class analyses based on drug administration patterns of heroin and cocaine were in Canada rather than the US, and did not include speedball injection in the model (Monga et al., 2007; Patra et al., 2009). Further, unlike the recent study from Baltimore (Kuramoto et al., 2011), the LCA in the present study was used to investigate needle sharing and risky sexual behaviors, which are important HIV-risk variables. This allows for a deeper understanding of how these variables may play a role in the HIV epidemic.
4.3 Implications
LCA and other epidemiological research techniques can help understand at-risk populations for purposes of intervention. All of the classes identified demonstrate substantial risk for contracting infectious diseases, but risk profiles varied by group. The existence of these subgroups suggests a need for targeted prevention and intervention efforts. For example, among polysubstance users, the clearest need is for reductions in needle-sharing behaviors, as may be accomplished via needle exchange programs (Clark and Fadus, 2010).
Despite notable reduction in infectious disease risk among non-injection drug users, substantial risks still exist, most notably from unsafe sexual behaviors. Further effort is needed to address these concerns. Fortunately, substance abuse treatment, and similar types of treatment, are associated with reductions in sexual risk behavior (Drumright and Colfax, 2009; Magura et al., 1994; St Lawrence et al., 2002; Wechsberg et al., 2008). Interventions focusing on sexual behaviors associated with drug use – regardless of ROA, but perhaps especially for non-injection cocaine and heroin users – are needed to reduce the risk of STD transmission among vulnerable populations. Prevention and treatment outcomes can be improved by a more thorough understanding of the interrelations between different substances of abuse.
Acknowledgements
The authors wish to acknowledge the help and support of the Drug Dependence Epidemiology Training Program staff, fellows and faculty. We would especially like to thank members of the publication workgroup.
Role of Funding Source: This research was funded by a grant awarded to William Latimer from the National Institute on Drug Abuse (NIDA-R01 DA14498) and by the Drug Dependence Epidemiology Training Grant (NIDA T32 DA007292) at the Johns Hopkins Bloomberg School of Public Health, William Latimer, Director. NIDA had no further role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors: Author Harrell conducted the statistical analysis and wrote the first draft of this manuscript. Authors Petras and Mancha wrote significant portions of the Methods section and provided extensive statistical consulting. Author Trenz wrote portions of the Introduction and Discussion section and critically reviewed and revised the manuscript. Author Latimer was the principal investigator of the study where these data were collected. All authors have approved of the final manuscript.
Conflict of Interest: The authors have no conflicting interests to report.
References
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2007;102:94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Bandeen-Roche K, Miglioretti DL, Zeger SL, Rathouz PJ. Latent variable regression for multiple discrete outcomes. J. Am. Stat. Assoc. 1997;92:1375–1386. [Google Scholar]
- Boyer CB, Shafer M, Wibbelsman CJ, Seeberg D, Teitle E, Lovell N. Associations of sociodemographic, psychosocial, and behavioral factors with sexual risk and sexually transmitted diseases in teen clinic patients. J. Adolesc. Health. 2000;27:102–111. doi: 10.1016/s1054-139x(99)00113-5. [DOI] [PubMed] [Google Scholar]
- Boyer CB, Shafer MA, Teitle E, Wibbelsman CJ, Seeberg D, Schachter J. Sexually transmitted diseases in a health maintenance organization teen clinic: associations of race, partner’s age, and marijuana use. Arch. Pediatr. Adolesc. Med. 1999;153:838–844. doi: 10.1001/archpedi.153.8.838. [DOI] [PubMed] [Google Scholar]
- Broz D, Ouellet LJ. Racial and ethnic changes in heroin injection in the United States: implications for the HIV/AIDS epidemic. Drug Alcohol Depend. 2008;94:221–233. doi: 10.1016/j.drugalcdep.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchacz K, McFarland W, Hernandez M, Klausner JD, Page-Shafer K, Padian N, Molitor F, Ruiz JD, Bolan G, Morrow S, Katz MH. Prevalence and correlates of herpes simplex virus type 2 infection in a population-based survey of young women in low-income neighborhoods of Northern California. The Young Women’s Survey Team. Sex. Transm. Dis. 2000;27:393–400. doi: 10.1097/00007435-200008000-00004. [DOI] [PubMed] [Google Scholar]
- Cartwright WS. Cocaine medications, cocaine consumption and societal costs. Pharmacoeconomics. 2000;18:405–413. doi: 10.2165/00019053-200018040-00008. [DOI] [PubMed] [Google Scholar]
- Castor D, Pilowsky DJ, Hadden B, Fuller C, Ompad DC, de Leon CL, Neils G, Hoepner L, Andrews HF, Latkin C, Hoover DR. Sexual risk reduction among non-injection drug users: report of a randomized controlled trial. Aids Care-Psycholog. Socio-Med. Aspects AIDS/HIV. 2010;22:62–70. doi: 10.1080/09540120903012510. [DOI] [PubMed] [Google Scholar]
- CDC . CDC Fact Sheet. Center for Disease Control; Atlanta: 2008. Estimates of new HIV infections in the United States; pp. 1–6. [Google Scholar]
- Chen CY, Anthony JC. Epidemiological estimates of risk in the process of becoming dependent upon cocaine: cocaine hydrochloride powder versus crack cocaine. Psychopharmacology (Berl.) 2004;172:78–86. doi: 10.1007/s00213-003-1624-6. [DOI] [PubMed] [Google Scholar]
- Chitwood DD, Comerford M, Sanchez J. Prevalence and risk factors for HIV among sniffers, short-term injectors, and long-term injectors of heroin. J. Psychoactive Drugs. 2003;35:445–453. doi: 10.1080/02791072.2003.10400491. [DOI] [PubMed] [Google Scholar]
- Clark PA, Fadus M. Federal funding for needle exchange programs. Med. Sci. Monit. 2010;16:PH1–13. [PubMed] [Google Scholar]
- Courtwright D. Dark Paradise: Opiate Addiction in America Before 1940. Harvard University Press; Cambridge: 1982. [Google Scholar]
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Drumright LN, Colfax GN. HIV risk and prevention for non-injection substance users. In: Mayer KH, Pizer H, editors. HIV Prevention: A Comprehensive Approach. Academic Press; Burlington, MA: 2009. pp. 340–375. [Google Scholar]
- Ferreira RC, Rodrigues FP, Teles SA, Lopes CL, Motta-Castro AR, Novais AC, Souto FJ, Martins RM. Prevalence of hepatitis B virus and risk factors in Brazilian non-injecting drug users. J. Med. Virol. 2009;81:602–609. doi: 10.1002/jmv.21464. [DOI] [PubMed] [Google Scholar]
- Gossop M, Griffiths P, Powis B, Strang J. Severity of dependence and route of administration of heroin, cocaine and amphetamines. Br. J. Addict. 1992;87:1527–1536. doi: 10.1111/j.1360-0443.1992.tb02660.x. [DOI] [PubMed] [Google Scholar]
- Gossop M, Griffiths P, Powis B, Strang J. Cocaine: patterns of use, route of administration, and severity of dependence. Br. J. Psychiatry. 1994;164:660–664. doi: 10.1192/bjp.164.5.660. [DOI] [PubMed] [Google Scholar]
- Gossop M, Griffiths P, Powis B, Williamson S, Strang J. Frequency of non-fatal heroin overdose: survey of heroin users recruited in non-clinical settings. BMJ. 1996;313:402. doi: 10.1136/bmj.313.7054.402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KM, Doherty EE, Reisinger HS, Chilcoat HD, Ensminger M. Social integration in young adulthood and the subsequent onset of substance use and disorders among a community population of urban African Americans. Addiction. 2010;105:484–493. doi: 10.1111/j.1360-0443.2009.02787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Niv N, Moore AA. Gender and comorbidity among individuals with opioid use disorders in the NESARC study. Addict. Behav. 2009;34:498–504. doi: 10.1016/j.addbeh.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyarmathy VA, Neaigus A, Miller M, Friedman SR, Jarlais D.C. Des. Risk correlates of prevalent HIV, hepatitis B virus, and hepatitis C virus infections among noninjecting heroin users. J. Acquir. Immune Defic. Syndr. 2002;30:448–456. doi: 10.1097/00042560-200208010-00011. [DOI] [PubMed] [Google Scholar]
- Haas AL, Sorensen JL, Hall SM, Lin C, Delucchi K, Sporer K, Chen T. Cigarette smoking in opioid-using patients presenting for hospital-based medical services. Am. J. Addict. 2008;17:65–69. doi: 10.1080/10550490701756112. [DOI] [PubMed] [Google Scholar]
- Harrell P, Trenz R, Zur J, Mancha B, Latimer W. Cigarette Smoking, Illicit Drug Use, and Routes of Administration Among Heroin and Cocaine Users. 2011 Society for Prevention Research conference; Washington, D.C.. 2011. [Google Scholar]
- Hickman M, Hope V, Brady T, Madden P, Jones S, Honor S, Holloway G, Ncube F, Parry J. Hepatitis C virus (HCV) prevalence, and injecting risk behaviour in multiple sites in England in 2004. J. Viral Hepat. 2007;14:645–652. doi: 10.1111/j.1365-2893.2007.00855.x. [DOI] [PubMed] [Google Scholar]
- Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat. Med. 2004;23:1455–1497. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Prev. Med. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, Melton LJ., 3rd Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA. 1996;275:1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- Hutton HE, McCaul ME, Santora PB, Erbelding EJ. The relationship between recent alcohol use and sexual behaviors: gender differences among sexually transmitted disease clinic patients. Alcohol. Clin. Exp. Res. 2008;32:2008–2015. doi: 10.1111/j.1530-0277.2008.00788.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenness SM, Kobrak P, Wendel T, Neaigus A, Murrill CS, Hagan H. Patterns of exchange sex and HIV infection in high-risk heterosexual men and women. J. Urban Health. 2011;88:329–341. doi: 10.1007/s11524-010-9534-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. Secondary School Students. vol. 1. National Institute on Drug Abuse; Bethesda, MD: 2002. Monitoring the Future: National Survey Results on Drug Use, 1975-2001. (NIH Publication No. 02-5106) [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. Am. J. Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv. Rev. Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kokkevi A, Stefanis N, Anastasopoulou E, Kostogianni C. Personality disorders in drug abusers: prevalence and their association with AXIS I disorders as predictors of treatment retention. Addict. Behav. 1998;23:841–853. [PubMed] [Google Scholar]
- Kuo I, Greenberg AE, Magnus M, Phillips G, 2nd, Rawls A, Peterson J, Hamilton F, West-Ojo T, Hader S. High prevalence of substance use among heterosexuals living in communities with high rates of AIDS and poverty in Washington, DC. Drug Alcohol Depend. 2011;117:139–144. doi: 10.1016/j.drugalcdep.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Kuo I, Sherman SG, Thomas DL, Strathdee SA. Hepatitis B virus infection and vaccination among young injection and non-injection drug users: missed opportunities to prevent infection. Drug Alcohol Depend. 2004;73:69–78. doi: 10.1016/j.drugalcdep.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Kuramoto SJ, Bohnert AS, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2011.03.030. epub ahead of print, PMID: 21530105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, Kuramoto SJ, Davey-Rothwell MA, Tobin KE. Social norms, Social networks, and HIV risk behavior among injection drug users. AIDS Behav. 2010;14:1159–1168. doi: 10.1007/s10461-009-9576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarsfeld P, Henry N. Latent Structure Analysis. Houghton Mifflin; New York: 1968. [Google Scholar]
- Lejuez CW, Bornovalova MA, Daughters SB, Curtin JJ. Differences in impulsivity and sexual risk behavior among inner-city crack/cocaine users and heroin users. Drug Alcohol Depend. 2005;77:169–175. doi: 10.1016/j.drugalcdep.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Leri F, Bruneau J, Stewart J. Understanding polydrug use: review of heroin and cocaine co-use. Addiction. 2003;98:7–22. doi: 10.1046/j.1360-0443.2003.00236.x. [DOI] [PubMed] [Google Scholar]
- Leri F, Stewart J, Tremblay A, Bruneau J. Heroin and cocaine co-use in a group of injection drug users in Montreal. J. Psychiatry Neurosci. 2004;29:40–47. [PMC free article] [PubMed] [Google Scholar]
- Lindesmith A. Addiction and Opiates. Aldine Publishing Company; Chicago: 1947. [Google Scholar]
- Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Lubke GH, Muthen B. Investigating population heterogeneity with factor mixture models. Psychol. Methods. 2005;10:21–39. doi: 10.1037/1082-989X.10.1.21. [DOI] [PubMed] [Google Scholar]
- Magura S, Kang SY, Shapiro JL. Outcomes of intensive AIDS education for male adolescent drug users in jail. J. Adolesc. Health. 1994;15:457–463. doi: 10.1016/1054-139x(94)90492-l. [DOI] [PubMed] [Google Scholar]
- Mark TL, Woody GE, Juday T, Kleber HD. The economic costs of heroin addiction in the United States. Drug Alcohol Depend. 2001;61:195–206. doi: 10.1016/s0376-8716(00)00162-9. [DOI] [PubMed] [Google Scholar]
- Marshall MM, McCormack MC, Kirk GD. Effect of cigarette smoking on HIV acquisition, progression, and mortality. AIDS Educ. Preven. 2009;21:28–39. doi: 10.1521/aeap.2009.21.3_supp.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Carlson RG, Alexandre PK, Falck RS. Perceived risk associated with ecstasy use: a latent class approach. Addict. Behav. 2011;36:551–554. doi: 10.1016/j.addbeh.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masyn KE, Henderson CE, Greenbaum PE. Exploring the latent structures of psychological constructs in social development using the dimensional-categorical spectrum. Soc. Dev. 2010;19:470–493. doi: 10.1111/j.1467-9507.2009.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann. Epidemiol. 2004;14:535–542. doi: 10.1016/j.annepidem.2003.10.001. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Latent Class Analysis. Sage Publications; Thousand Oaks, CA: 1987. [Google Scholar]
- McKirnan DJ, Ostrow DG, Hope B. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS Care. 1996;8:655–669. doi: 10.1080/09540129650125371. [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel D. Finite Mixture Models. John Wiley; New York: 2000. [Google Scholar]
- Mehta SH, Astemborski J, Kirk GD, Strathdee SA, Nelson KE, Vlahov D, Thomas DL. Changes in blood-borne infection risk among injection drug users. J. Infect. Dis. 2011;203:587–594. doi: 10.1093/infdis/jiq112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M, Korves CT, Fernandez T. The social epidemiology of HIV transmission among African American women who use drugs and their social network members. Aids Care-Psycholog. Socio-Med. 2007;19:858–865. doi: 10.1080/09540120701191540. Aspects of AIDS/HIV. [DOI] [PubMed] [Google Scholar]
- Miller M, Neaigus A. Sex partner support, drug use and sex risk among HIV-negative non-injecting heroin users. AIDS Care. 2002;14:801–813. doi: 10.1080/0954012021000031877. [DOI] [PubMed] [Google Scholar]
- Mitchell M, Severtson S, Graham C, Floyd L, Latimer W. The moderating influence of cognitive performance on risk awareness to predict HIV/AIDS risk-taking behaviors. Retrovirology. 2006;3:P41. [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, Noel L, Tyndall M, Wild C, Leri F, Fallu JS, Bahl S. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Asparouhov T. [accessed on April 19 2011];Wald test of mean equality for potential latent class predictors in mixture modeling. 2007 www.statmodel.com/download/MeanTest1.pdf.
- Muthén LK, Muthén BO. Mplus User’s Guide. Sixth Edition Muthén and Muthén; Los Angeles, CA: 2010. [Google Scholar]
- Neaigus A, Friedman SR, Kottiri BJ, Jarlais DCD. HIV risk networks and HIV transmission among injecting drug users. Eval. Program Plann. 2001;24:221–226. [Google Scholar]
- Neblett RC, Davey-Rothwell M, Chander G, Latkin CA. Social network characteristics and HIV sexual risk behavior among urban african american women. J. Urban Health. 2011;88:54–65. doi: 10.1007/s11524-010-9513-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KE, Galai N, Safaeian M, Strathdee SA, Celentano DD, Vlahov D. Temporal trends in the incidence of human immunodeficiency virus infection and risk behavior among injection drug users in Baltimore, Maryland, 1988-1998. Am. J. Epidemiol. 2002;156:641–653. doi: 10.1093/aje/kwf086. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparoutiov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Modeling. 2007;14:535–569. [Google Scholar]
- Patkar AA, Batra V, Mannelli P, Evers-Casey S, Vergare MJ, Leone FT. Medical symptoms associated with tobacco smoking with and without marijuana abuse among crack cocaine-dependent patients. Am. J. Addict. 2005;14:43–53. doi: 10.1080/10550490590899844. [DOI] [PubMed] [Google Scholar]
- Patkar AA, Lundy A, Leone FT, Weinstein SP, Gottheil E, Steinberg M. Tobacco and alcohol use and medical symptoms among cocaine dependent patients. Subst. Abuse. 2002;23:105–114. doi: 10.1080/08897070209511480. [DOI] [PubMed] [Google Scholar]
- Patra J, Fischer B, Maksimowska S, Rehm J. Profiling poly-substance use typologies in a multi-site cohort of illicit opioid and other drug users in Canada-a latent class analysis. Addict. Res. Theory. 2009;17:168–185. [Google Scholar]
- Petras H, Masyn K. General growth mixture analysis with antecedents and consequences of change. In: Piquero A, Weisburd D, editors. Handbook of Quantitative Criminology. Springer; New York: 2010. pp. 69–100. [Google Scholar]
- Pilowsky DJ, Hoover D, Hadden B, Fuller C, Ompad DC, Andrews HF, De Leon CL, Hoepner L, Xia Q, Latkin C. Impact of social network characteristics on high-risk sexual Behaviors among non-injection drug users. Subst. Use Misuse. 2007;42:1629–1649. doi: 10.1080/10826080701205372. [DOI] [PubMed] [Google Scholar]
- Pines H, Koutsky L, Buskin S. Cigarette smoking and mortality among HIV-infected individuals in Seattle, Washington (1996-2008) AIDS Behav. 2011;15:243–251. doi: 10.1007/s10461-010-9682-3. [DOI] [PubMed] [Google Scholar]
- Raj A, Saitz R, Cheng DM, Winter M, Samet JH. Associations between alcohol, heroin, and cocaine use and high risk sexual behaviors among detoxification patients. Am. J. Drug Alcohol Abuse. 2007;33:169–178. doi: 10.1080/00952990601091176. [DOI] [PubMed] [Google Scholar]
- Ramaswamy V, Desarbo WS, Reibstein DJ, Robinson WT. An empirical pooling approach for estimating marketing mix elasticities with PIMS Data. Market Sci. 1993;12:103–124. [Google Scholar]
- Reboussin BA, Anthony JC. Is there epidemiological evidence to support the idea that a cocaine dependence syndrome emerges soon after onset of cocaine use? Neuropsychopharmacology. 2006;31:2055–2064. doi: 10.1038/sj.npp.1301037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reboussin BA, Song EY, Shrestha A, Lohman KK, Wolfson M. A latent class analysis of underage problem drinking: evidence from a community sample of 16-20 year olds. Drug Alcohol Depend. 2006;83:199–209. doi: 10.1016/j.drugalcdep.2005.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich JD, Anderson BJ, Schwartzapfel B, Stein MD. Sexual risk for hepatitis B virus infection among hepatitis C virus-negative heroin and cocaine users. Epidemiol. Infect. 2006;134:478–484. doi: 10.1017/S0950268805005248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L, Kohler CL, Grimley DM, Bellis J. Intention to use condoms among three low-income, urban African American subgroups: cocaine users, noncocaine drug users, and non-drug users. J. Urban Health. 2003;80:147–160. doi: 10.1093/jurban/jtg147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Office of Applied Studies. Rockville, MD: [accessed February 10, 2010]. 2009. Results from the 2008 National Survey on Drug Use and Health: National Findings. (NSDUH Series H-36). HHS Publication No. SMA 09-4434. Available at http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.pdf. [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol. Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Scheier LM, Abdallah A. Ben, Inciardi JA, Copeland J, Cottler LB. Tri-city study of ecstasy use problems: a latent class analysis. Drug Alcohol Depend. 2008;98:249–263. doi: 10.1016/j.drugalcdep.2008.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimension of a model. Ann. Stat. 1978;6:461–464. [Google Scholar]
- Severtson SG, Hedden SL, Martins SS, Latimer WW. Patterns of cognitive impairments among heroin and cocaine users: the association with self-reported learning disabilities and infectious disease. J. Learn. Disabil. 2010a doi: 10.1177/0022219409355481. epub ahead of print, PMID: 20574063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Severtson SG, Mitchell MM, Hubert A, Latimer W. The relationship between performance on the Shipley Institute of Living Scale (SILS) and hepatitis C infection among active injection drug users in Baltimore, Maryland. Am. J. Drug Alcohol Abuse. 2010b;36:61–65. doi: 10.3109/00952990903573264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. Lawrence JS, Crosby RA, Brasfield TL, O’Bannon RE., 3rd Reducing STD and HIV risk behavior of substance-dependent adolescents: a randomized controlled trial. J. Consult. Clin. Psychol. 2002;70:1010–1021. [PubMed] [Google Scholar]
- Strang J, Bearn J, Farrell M, Finch E, Gossop M, Griffiths P, Marsden J, Wolff K. Route of drug use and its implications for drug effect, risk of dependence and health consequences. Drug Alcohol Rev. 1998;17:197–211. doi: 10.1080/09595239800187001. [DOI] [PubMed] [Google Scholar]
- Strang J, Griffiths P, Powis B, Gossop M. Heroin chasers and heroin injectors: differences observed in a community sample in London, UK. Am. J. Addict. 1999;8:148–160. doi: 10.1080/105504999305956. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J. Urban Health. 2003;80:iii7–14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulkowski MS, Ray SC, Thomas DL. Needlestick transmission of hepatitis C. JAMA. 2002;287:2406–2413. doi: 10.1001/jama.287.18.2406. [DOI] [PubMed] [Google Scholar]
- Tobin KE, Kuramoto SJ, Davey-Rothwell MA, Latkin CA. The STEP into Action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106:366–375. doi: 10.1111/j.1360-0443.2010.03146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallejo F, Toro C, de la Fuente L, Brugal MT, Soriano V, Silva TC, Bravo MJ, Ballesta R, Barrio G. Prevalence of and risk factors for hepatitis B virus infection among street-recruited young injection and non-injection heroin users in Barcelona, Madrid and Seville. Eur. Addict. Res. 2008;14:116–124. doi: 10.1159/000130415. [DOI] [PubMed] [Google Scholar]
- Wang CP, Brown CH, Bandeen-Roche K. Residual diagnostics for growth mixture models: examining the impact of a preventive intervention on multiple trajectories of aggressive behavior. J. Am. Stat. Assoc. 2005;100:1054–1076. [Google Scholar]
- Wechsberg WM, Luseno WK, Karg RS, Young S, Rodman N, Myers B, Parry CD. Alcohol, cannabis, and methamphetamine use and other risk behaviours among Black and Coloured South African women: a small randomized trial in the Western Cape. Int. J. Drug Policy. 2008;19:130–139. doi: 10.1016/j.drugpo.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, Manson SM, Team A-S. Latent class analysis of substance use: comparison of two American Indian reservation populations and a national sample. J. Stud. Alcohol. 2006;67:32. doi: 10.15288/jsa.2006.67.32. [DOI] [PubMed] [Google Scholar]
- Windle M. The trading of sex for money or drugs, sexually transmitted diseases (STDs), and HIV-related risk behaviors among multisubstance using alcoholic inpatients. Drug Alcohol Depend. 1997;49:33–38. doi: 10.1016/s0376-8716(97)00136-1. [DOI] [PubMed] [Google Scholar]