Abstract
Transient osteoporosis of the hip (TOH) is a rare disorder of unknown etiology that is characterized by acute onset of disabling bone pain. The locally increased bone turnover and low bone mineral density (BMD) associated with this disorder indicate a potential role for an antiresorptive agent such as bisphosphonate as a treatment. A previously healthy 46-year-old man developed the sudden onset of pain in his right buttock and inguinal area, especially during walking and caused him to limp. A thorough medical workup including X-ray, MRI, and bone SPECT revealed transient osteoporosis of the hip, and he was treated with an infusion of zoledronate (5 mg). Two weeks later, he was fully recovered from pain and the gait disturbance. A follow-up MRI of the hip joint taken after 6 months showed complete resolution. The use of intravenous zoledronate provided a successful outcome in the treatment of TOH. The possibility of TOH should be considered in patients complaining of sudden hip pain and a limping gait. MR imaging played an important role for differentiation of TOH from other aggressive conditions with long term sequelae.
Keywords: Transient osteoporosis of hip (TOH), Bisphosphonate
INTRODUCTION
Transient osteoporosis of the hip, a rare clinical syndrome whose causes are unknown, shows transient osteopenia and rapid or gradual progression of pain, leading to maximum functional disability within 4-8 weeks, followed by subsequent improvement. In particular, it occurs in middle-aged males, and females in their third trimester of pregnancy. In most cases, it is spontaneously resolved by conservative treatments such as limited weight bearing and conservative therapies within 6-12 months, or sometimes within 24 months.1 The authors used intravenous infusion of zoledronate for one patient diagnosed with transient osteoporosis of the hip, and obtained effective reduction of disease duration and pain. Accordingly, this case is reported with a review of relevant references.
CASE REPORT
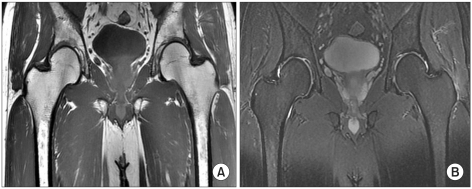
A male patient aged 46 years old visited the hospital due to pain in the right buttock and the inguinal area while standing up from a chair. Under the suspected condition of bursitis of the hip, nabumetone (1,000 mg/day) was orally administered to the patient for 2 weeks. However, the pain was not relieved and the symptoms deteriorated upon weight bearing. The patient experienced a limping gait 10 days after symptom expression and depended on a wheelchair. The patient had no previous history of trauma and had been taking medication due to hypertension for 5 years. The patient was relatively healthy except for smoking one pack of cigarettes a day and drinking 3 times a week. During a physical examination conducted upon hospitalization 2 weeks after expression of symptoms, no muscle weakness of the bilateral lower extremities was observed in manual muscle testing (MMT). Limited range of motion of the right hip joint due to pain, a positive right Patrick sign, and pain in the right inguinal area and the buttock were observed. Meanwhile, normal findings were observed in the deep tendon reflex of the lower extremities and the straight leg raising test. In hematologic tests, erythrocyte sedimentation rate was 11 mm/hr (normal range, 0-22), and C-reactive protein was 0.62 mg/dl (normal range, 0.00-0.50). When hip joint MRI was performed, the joint space of the bilateral hip was shown to be maintained, and a lesion, which showed patch low signal intensity with unclear border in a T1 weighted image and non-homogeneous high signal intensity in a T2 weighted image, was found across the right femoral head and neck (Fig. 1). In addition, the joint surface of the femoral head was shown to be maintained, and no circular band of the bone marrow of the femoral head, which is shown in avascular necrosis, was found. In a bone scan test, avascular necrosis was ruled out due to the increased uptake of radioisotopes in the bone marrow of the femoral head. After being diagnosed with transient osteoporosis of the hip, nabumetone administration (1,000 mg/day for 15 days) was discontinued. Subsequently, a single dose of zoledronate (5 mg) was intravenously infused for more than 15 minutes. Weight bearing was minimized by using crutches and a wheelchair. Hot pack, ultrasound, and interferential current therapies were performed on the hip. Normal gait was achieved one week after the treatments. No pain was observed upon weight bearing despite a slight pain in the inguinal area 2 weeks after treatments. However, the patient was asked to use crutches for an additional 2 weeks to minimize weight bearing on the hip joint. No pain in the inguinal area and no pain in the hip joint upon weight bearing were shown 4 weeks after treatments. When MRI was taken 6 months later, previous abnormal findings were completely resolved and no clinical recurrence was found (Fig. 2).
Fig. 1.
(A) The coronal T1 weighted image of hip joint shows patchy low signal intensity lesion in right femoral head (arrow), (B) which demonstrates high signal intensity lesion on fat suppressed coronal T2 weighted image (arrow).
Fig. 2.
Follow-up hip MRI showed no abnormal lesion in both femoral heads.
DISCUSSION
Transient osteoporosis of the hip rarely occurs, but causes pain independent from trauma, and increases bone turnover.2 Due to difficulty of early diagnosis caused by rareness and normal early radiological findings, TOH is often overlooked.3 So far, approximately 300 cases have been reported. Despite controversy about the causes and pathophysiology of the disease, it has been generally accepted that transient osteoporosis of the hip is a self-limiting disease. It is spontaneously resolved by conservative treatments such as limited weight bearing and analgesic treatment within 6-24 months. Restoration of bone density and normal MRI are achieved within 6-12 months.4,5 Due to its non-specific symptoms and signs, distinguishing TOH from avascular necrosis or other inflammatory or neoplastic diseases is difficult, but bone marrow edema observed in MRI is useful for early diagnosis and discrimination.6 Characteristic MRI findings include a diffuse low signal intensity in a T1 weighted image, and high signal intensity in a T2 weighted image. These types of MRI findings decrease as the symptoms improve. Discrimination is possible due to the lack of a low signal intensity band in a T1 weighted image, or a double line sign in a T2 weighted image, which are shown in avascular necrosis.7,8
For treatment of transient osteoporosis of the hip, conventional managements such as limited weight bearing and analgesic treatment have been mainly applied, but various other treatments have recently been performed to shorten the clinical course of the disease. Among such treatments, bisphosphonate has been reported to be successfully used to treat the disease by strongly inhibiting bone turnover, because its efficacy for other metabolic bone diseases has been proven.3,9 Although the mechanism via which bone pain is effectively reduced remains unknown, pain reduction is likely to be attributable to the resolution of fundamental causes and the anti-inflammatory property of bisphosphonate, considering the drug has no analgesic effect involved in its mechanism.2 Transient osteoporosis of the hip shows increased bone turnover and bone loss due to increased bony destructive activities, resulting in the deterioration of the stability of bone structure. This result causes gradual weakness, torsion, and pain at the bone. It is expected that bisphosphonate, which is intravenously administered to treat such conditions, reduces increased bony destructive activities and rapidly restores bone, resulting in concurrent pain reduction. Varrena et al.3 reported that symptoms were resolved in 15 patients two months after intravenous injection of pamidronate, and normal findings were shown in MRI three months after injection. Ringe et al.2 reported that symptoms improved in 12 patients one month after intravenous injection of ibandronate. Accordingly, the authors administered zoledronate, one of the bisphosphonate class of drugs that is administered once a year. As a result, the patient's symptoms were almost resolved two weeks after treatment, suggesting that this treatment might be more effective in reducing disease duration compared with those mentioned in previous studies. Therefore, transient osteoporosis of the hip is necessary to be considered in middle-aged male patients suffering from hip joint pain and gait disturbance as a differential diagnosis from other diseases leaving long-lasting sequelae, such as avascular necrosis of the femoral head and joint destructive diseases due to joint inflammation and tumor.10 In the cases of transient osteoporosis diagnosed using MRI or bone scanning, invasive diagnosis or treatment is unnecessary, and intravenous injection of bisphosphonate such as zoledronate, rather than anti-inflammatory drugs, could be safer and more effective.
This case report has the limitation that follow-up using MRI was not conducted earlier than 6 months, which is a reported time point for the initiation of spontaneous resolution. However, it is meaningful because the complete resolution of the lesion was observed; a result not previously reported in Korea. Additionally, faster recovery was observed in patients who had more severe symptoms than those reported in foreign patients. The authors obtained an effective reduction of pain and disease duration by intravenously injecting zoledronate into the patients who suffered from inguinal and femoral pain, and who were diagnosed with transient osteoporosis of the hip by MRI. Accordingly, this case is reported herein.
References
- 1.Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Bone marrow edema syndrome. Skeletal Radiol. 2009;38:425–436. doi: 10.1007/s00256-008-0529-1. [DOI] [PubMed] [Google Scholar]
- 2.Ringe JD, Dorst A, Faber H. Effective and rapid treatment of painful localized transient osteoporosis (bone marrow edema) with intravenous ibandronate. Osteoporos Int. 2005;16:2063–2068. doi: 10.1007/s00198-005-2001-6. [DOI] [PubMed] [Google Scholar]
- 3.Varenna M, Zucchi F, Binelli L, Failoni S, Gallazzi M, Sinigaglia L. Intravenous pamidronate in the treatment of transient osteoporosis of the hip. Bone. 2002;31:96–101. doi: 10.1016/s8756-3282(02)00812-8. [DOI] [PubMed] [Google Scholar]
- 4.Daniel WW, Sanders PC, Alarcon GS. The early diagnosis of transient osteoporosis by magnetic resonance imaging. A case report. J Bone Joint Surg Am. 1992;74:1262–1264. [PubMed] [Google Scholar]
- 5.Guerra JJ, Steinberg ME. Distinguishing transient osteoporosis from avascular necrosis of the hip. J Bone Joint Surg Am. 1995;77:616–624. doi: 10.2106/00004623-199504000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Fabbriciani G, Pirro M, Manfredelli MR, Bianchi M, Sivolella S, Scarponi AM, Mannarino E. Transient osteoporosis of the hip: successful treatment with teriparatide. Rheumatol Int. 2010 Mar 18; doi: 10.1007/s00296-010-1404-7. [DOI] [PubMed] [Google Scholar]
- 7.Hayes CW, Conway WF, Daniel WW. MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome, or osteonecrosis. Radiographics. 1993;13:1001–1012. doi: 10.1148/radiographics.13.5.8210586. [DOI] [PubMed] [Google Scholar]
- 8.Parker RK, Ross GJ, Urso JA. Transient osteoporosis of the knee. Skeletal Radiol. 1997;26:306–309. doi: 10.1007/s002560050241. [DOI] [PubMed] [Google Scholar]
- 9.Schapira D, Braun Moscovici Y, Gutierrez G, Nahir AM. Severe transient osteoporosis of the hip during pregnancy. Successful treatment with intravenous biphosphonates. Clin Exp Rheumatol. 2003;21:107–110. [PubMed] [Google Scholar]
- 10.Miyanishi K, Kaminomachi S, Hara T, Maeda H, Watanabe H, Shimizu A, Torisu T. A subchondral fracture in transient osteoporosis of the hip. Skeletal Radiol. 2007;36:677–680. doi: 10.1007/s00256-006-0248-4. [DOI] [PubMed] [Google Scholar]