Synonyms
Vasa praevia.
Definition
Fetal vessels crossing or running in close proximity to the inner cervical os. These vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture.
Etymology
“Vasa” is the plural of “Vas” which comes from Latin word denoting a vessel or a dish (thus the word “vase”). “Previa” is a combination of two words: “pre” (or “prae”) meaning before, and “via” meaning way. “Previa” in medicine, usually refers to anything obstructing the passage in childbirth. Literally therefore, vasa previa means “vessels in the way, before the baby”.
History
Lobstein reported the first case of rupture of vasa previa in 1801 (1). Before ultrasound became common practice, the diagnosis of vasa previa was often made (too late) on the triad of ruptured membranes, painless vaginal bleeding (fetal bleeding: Benckiser’s hemorrhage) and fetal distress (or demise). The first ultrasound description of vasa previa dates back to 1987 (2).
Prevalence
The largest studies report a prevalence of 1.5–4:10,000 (3, 23). Older numbers are based on less reliable data and should probably be abandoned. About 10% of vasa previa occur in twins (8). Yet even in careful studies, the diagnosis of vasa previa is easy to miss, even postnatally and thus be underreported. Thus it is likely that the condition is not as uncommon as generally thought.
Pathogenesis
The 2 main causes of vasa previa are velamentous insertions (where the cord inserts directly into the membranes, leaving unprotected vessels running to the placenta) (25–62%) and vessels crossing between lobes of the placenta such as in succenturiate or bilobate placentas (33–75%) (36, 56). Less commonly, a vessel that courses over the edge of a marginal placenta or a placenta previa may become a vasa previa after extension of the placenta over better vascularized area (trophotropism) (4) and involution of the cotyledons that were previa (5, 6).
Risk factors
Conditions associated with vessels that run close to the cervix, such as low-lying placenta (7, 8), placenta previa (9), multiple pregnancies (10), and of course multilobate placentas and velamentous insertion [1% of singleton pregnancy (38), 10% in multifetal pregnancies (11–13)]. About 2% of velamentous insertions are associated with a vasa previa (14–16).
Placenta membranacea (22) is also a risk factor. It is less clear why, but in-vitro fertilization increases the risk of vasa previa (17–20), (about 1:300 pregnancies) (21). Many of these conditions present with vaginal bleeding which should be considered a possible alert symptom for vasa previa.
Sonographic findings
Although vasa previa can be recognized in grey-scale as linear structures in front of the inner os (22, 23), the diagnosis is considerably simpler by putting a flash of color Doppler (color or power) (24, 25), over the cervix. Arterial flow but also venous flow can be recognized. Although some have obtained the diagnosis by perineal scan (26), a transvaginal image is clearly superior to an abdominal scan. Some have also advocated the use of 3D (27, 59). Our impression is that 3D does not contribute much either in the diagnosis nor the mapping of the vessels since this is quite straightforward from 2D alone. Since 3D is not universally available, its unavailability should not be construed as a reason to not seek vasa previa. Nevertheless, 3D allows review of the volume if an unexpected finding is found at delivery. Another recent idea is to attempt to diagnose the cord insertion in the first trimester during the nuchal lucency screening, at a time when the fetus is less likely to obscure the cord insertion (28).
Other diagnostic procedures
Alternative methods of diagnosis such as digital palpation of a vasa previa, amnioscopy, Apt, Ogita (29) or similar (30) tests (fetal blood detection), and palpation have mostly a historical significance. MRI has been suggested too (31, 32). All these methods require a greater expertise then color Doppler thus cannot compare in speed and availability.
Implications for targeted examinations
In all pregnancies, we recommend sonographic examination for the placental cord insertion. In cases where the cord insertion is central and there is no succenturiate lobe, the likelihood of a vasa previa is negligible. Only those cases where the placenta is low-lying should be examined more carefully. In practice, a short sweep with color Doppler over the internal os will usually detect abnormal vessels over the cervix. If anything is seen in color, greater attention needs to be paid to the region. Transvaginal (TV) sonography with color Doppler is ideal, not only because the proximity of the transducer to the os and the vessels but also vessels that are in a coronal plane of the patient are easier to recognize on transvaginal exam than on abdominal sonography. However, due to the extra time required and the invasiveness, this is only justified when there is a sufficient presumption on the abdominal scan or risk factors (low–lying placenta, multi-lobed placenta, multiple pregnancies, in-vitro fertilization, unidentified cord insertion, or abnormal flow over the cervix) or when there is an additional reason to do a TV scan.
The following is a proposed diagnostic algorithm for the second-trimester detection of vasa previa (Fig. 12). During the second trimester examination (or later examination if the previous information is missing), observation of the placental cord insertion and the lower margin of the placenta shows that they are both clearly far from the inner os. In those cases there is essentially no risk of vasa previa and no further assessment for vasa previa is required.
Figure 12.
The same second trimester vaginal sonography as in figure 2 using color Doppler showing a flushing artefact, caused by the movement of the amniotic fluid during fetal movement, imitating vasa previa.
Or, during the exam a succenturiate or multilobate placenta, velamentous insertion, a multifetal pregnancy, a low placenta, or an in-vitro fertilization is found or exists. Then an abdominal scan of cervix with color Doppler is suggested. If it is clearly normal then we go back to the “No risk” category.
Or if the exam is not obviously normal, then a transvaginal color Doppler should be performed. If it is normal, we go back to the “no or low risk” category. If the transvaginal color Doppler is “Suspicious or abnormal”, then manage the patient as having a vasa previa. If during the initial abdominal exam there is any additional reason for performing a transvaginal examination, perform one and if it is strictly normal, the matter can be dropped, otherwise manage the patient as having a vasa previa.
This should cover most clinical situation but exceptions are bound to happen and should be judged as they arise.
Although some studies have claimed that adding a transvaginal ultrasound to an abdominal ultrasound only adds about a minute of examination time (33–35), this does not include the time to explain the procedure to the patient, obtain verbal consent, as well as patient preparation.
Several studies, have shown that when specifically sought, velamentous insertions and thus vasa previa can be reliably recognized (36–39), and that further, in prenatally detected vasa previa, the newborn survival rate ranged from 97–100% in the study group. Yet, other studies have demonstrated that velamentous insertions are regularly missed (40, 41).
Even in skilled centers specifically attempting to identify vasa previa, some cases are likely to be missed (42). In one study 1 or possibly 2 out of 11 (or 12) cases was missed, and false positive ranged from 10–16% (36, 37). Even when specifically sought, a predisposing factor such as velamentous insertion which some authors report to recognize with 100% (39) accuracy, is only recognized by others in 62% (43), with higher result in anterior placenta (92%) and worst result in fundal (40%) or posterior (50%) placenta. In less skilled environment, the diagnosis can be missed even in the presence of risk factors (44). Some of these studies are getting a little old and results are improving.
When a vasa previa is identified, serial scans, decreased maternal activity and close attention to early signs of labor or bleeding should be recommended (36).
The bottom line is that although it is unlikely that all vasa previa will be recognized, awareness of the risk factors and adoption of a protocol, such as the one suggested below, to specifically seek vasa previa plus careful examination should substantially decrease the number of unsuspected cases at delivery and baring technical problems of maternal obesity or scarring a majority (90–95%) should be recognized.
Differential diagnosis
“Linear structures” in front of the inner os in grey-scale may also represent marginal placental sinus, chorioamniotic separation and simple folds of the membranes. The differential diagnosis of those is easily established by color Doppler. Pulsed Doppler will demonstrate a fetal umbilical or venous waveform if it is a vasa previa. Sometimes marginal placental sinus may present with flow, but it will be a maternal heart frequency.
Pitfalls and artifacts
Although the diagnosis of vasa previa appears straight forward, the diagnosis of cord insertion by the abdominal approach is not always feasible in obese patients, those with scars or even simply difficult fetal presentations. In case where the inner os is not seen on abdominal scans, a transvaginal examination would be recommended.
Even on transvaginal examination there are possible pitfalls such as motion artifacts. Motion artifacts can occasionally give the impression on transvaginal color Doppler of previa flow simply due to sloshing of amniotic fluid resulting from fetal motion. This artifact can be recognized by its irregular nature and lack of reproducibility. Another pitfall is to confuse a funic presentation for a vasa previa. These are differentiated by the shifting in position of the cord, easily done by gently tapping with the transducer over the region.
Finally, a vessel seen during a first trimester transvaginal scan should not be assumed to represent a vasa previa. Too often the vessel will be of maternal origin and be confused because of lateral resolution issues. Pulse Doppler will demonstrate a maternal pulse. The diagnosis of vasa previa is thus best made in the 2nd to 3rd trimester. Should a suspicious vessel be found in the first trimester, a repeat scan in the second trimester is suggested.
Review of the literature is provided in Tables I and II. Since vasa previa have been considered difficult to diagnose, have not specifically been sought and are not common, there are unfortunately no large prospective studies of the condition, and the evidence about the benefit of antenatal diagnosis relies on many small series or case report.
Table I.
Review of studies attempting to identify vasa previa.
| Author | No. of cases | Objectives of the Study to identify | G.A (wks) at diagnosis | Methods of Investigation | Umbilical cord insertion identification | Pathogenesis of vasa previa | Associated complications | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Nomiyama et al. (1998) | 587 (555 singletons, 16 sets of twin) | Identify umbilical cord insertion Velamentous cord insertion Vasa previa |
Mid-trimester scan 18–20 wks |
Color Doppler during routine sonography as (TVS*) & (TAS) | Specificity 99.8% (580/581) 1 not seen turned out normal |
Velamentous cord insertion:
|
Premature rupture of membrane | 99.8% (586/587) of all cord insertions identified |
| Lee et al. (2000) | 93,874 | Prenatal ultra-sound diagnosis, and clinical out-comes of vasa previa | Average 26 weeks Earliest 16 weeks |
Abdominal and transvaginal with Doppler ultrasound | Record shows all cases were identified | Velamentous: 10 Bilobed placenta: 3 Succenturiate placenta: 2 Marginal: 2 |
Antepartum bleeding in 6/18 (some with fetal intraventricular hemorrhage) Fetal heart rate abnormalities Intra-uterine fetal death & preterm delivery Low Apgar scores |
Identify asymptomatic patients before delivery Delivery at 35–36 wks after maturity amniocentesis |
| Catanzarite et al. (2001) | 33,208 | Specificity of sonographic diagnosis of vasa previa and pregnancy | Most at 20–24 wks (67%) | Abdominal and transvaginal approach + color or power Doppler |
Velamentous: 2 Multilobar placenta: 8 |
Scimitar syndrome Ventriculomegaly |
10 of 11 cases identified (91%) 1 marginal placenta Delivery at 32–37 weeks |
|
| Sepulveda et al. (2003) | 832 | Identifying velamentous insertion of the cord in routine obstetric ultrasound | 2nd and 3rd trimester (at least 16 weeks) Mean = 23 wk |
Color Doppler ultrasound + (2D) + (3D) | 825/832 (99%) | Velamentous: 7/8 Eccentric: 1/8 |
Infant with transient tachypnea Cephalocele Trisomy 21 Respiratory distress syndrome |
825/832 (99%) cord insertion detected |
| Hasegawa et al. (2006) | 340 | Detection of cord insertion site (in the lower third of uterus) during the late first trimester | 9–11 weeks | Gray-scale transvaginal sonography | 318/340 (93.5%) 283 normal cord insertion 35 cord insertion in lower 1/3 of the uterus |
4/283 + 10/35 = velamentous cord insertion 4/283 + 5/35 = accessory placenta |
SGA = 4/35 PROM = 9/35 Emergency C.S. = 2/35 |
Cord insertion in ower 1/3 of the luterus in 1st trimester lead to frequent developmental abnormalities of placenta & cord. Useful for the identification of high-risk pregnancies |
| Hasegawa et al. (2006) | 3446 | Umbilical cord insertion | 18–20 weeks | Gray-scale ultrasonography and color-flow imaging | 3367/ 3421 40 suspected velamentous cord insertion 39 suspected Marginal cord insertion |
Velamentous 25/40 and 10/3367 Marginal 28/39 and 10/3367 |
Fetal heart rate abnormalities Low Apgar scores |
Pregnancy with velamentous cord insertion should be high risk pregnancy |
G.A. = gestational age; SGA = small for gestational age; PROM = premature rupture of membranes; CS = cesarean section; TAS = trans-abdominal sonography; TVS = trans-vaginal sonography.
Table II.
Review of reported cases 1990–2006.
| Reference | No. of cases | Vaginal bleeding as initial presentation | G.A. (wks) at diagnosis | TAS + CDU | TVS + CDU | Pathology | Number of vessels | Time and mode of delivery | Associated anomalies or neonatal complications |
|---|---|---|---|---|---|---|---|---|---|
| Harding et al. (1990) | 1 | Yes | 24 wk 4d | 1 | Succenturiate lobe | One large vessel | |||
| Nelson et al. (1990) | 1 | No | 26 wk | 1 | Velamentous Cord insertion | Four major vessels | |||
| Hsieh et al. (1991) | 1 | No | 30 wk | 1 | Succenturiate Lobe | Fetal vessels | |||
| Arts et al. (1993) | 1 | Yes | 39 wk | 1* | Succenturiate Lobe + Velamentous Cord insertion | Several vessels | 39 wk, Elective C.S | Normal | |
| Meyer et al. (1993) | 1 | No | 27 wk | 1 | 1 | Marginal Cord insertion | Large vein and small artery | ||
| Hata et al. (1994) | 1 | Yes | 30 wk | 1 | Velamentous Cord insertion | Network of vessels | |||
| Fleming et al. (1996) | 1 | No | 1 | 1 | Bilobed Placenta | Several vessels | |||
| Sauerbrei and Davies (1998) | 1 | No | 36 wk | 1 | 1 | Velamentous Cord insertion | Several vessels | 36 wk, Elective C.S. | Normal |
| 1 | Yes | 28 wk | 1 | 1 | Placenta Membranacea | 4 Vessels | 33 wk, Elective C.S. | Normal | |
| Devesa et al. (1996) | 1 | No | 20 wk | 1 | 1 | Velamentous cord insertion | Large vessel | 37 wk, Elective C.S. | Normal |
| Fung et al. (1998) | 1 | Yes | 35 wk | 1 | Bilobed placenta | Network of vessels | 36 wk, Elective C.S. | Normal | |
| 1 | Yes (heavy) | Not diagnosed | 1 | Velamentous cord insertion | Network of vessels | 39 wk, Elective C.S. | Resuscitation + blood Transfusion + convulsion | ||
| 1 | No | Not diagnosed | Velamentous cord insertion | Network of vessels | 39 wk, Emergency C.S. 37 wk, Elective C.S. |
Normal | |||
| Oyelese et al. (1998) | 1 | Yes | 38 wk | 1 | Velamentous cord insertion | Network of vessels | 38 wk, Normal Vaginal Delivery | Stillborn ex sanguinated fetus | |
| 1 | No (clear fluid only) | 23 wk | 1 | 1 | Succenturiate lobe | Network of vessels | 24 wk, Emergency C.S. (chorio-amionitis) | Died at 7 days of life sepsis and prematurity | |
| 1 | Yes | 34 wk | 1 | Velamentous cord insertion | 2 Vessels (A & V) | 36 wk, Elective C.S. | Normal | ||
| Lee et al. (2000) | 1 | No | 21 wk 1d | 1(3D) Multiplanar volume | Bilobed Placenta + Velamentous cord | Large vessel | 33 wk, Elective C.S. | Normal | |
| 1 | No | 34 wk 3d | (3D) Flight-path | Velamentous cord | Large vessel | 35 wk, Elective C.S. | Normal | ||
| Canterino et al. (2004) | 1 | No | 19 wk | 1(3D) | 1 | Velamentous cord insertion | Network of vessels | 35 wk, Elective C.S. | Respiratory distress Syndrome |
| Stafford et al (2004) | 1 | Yes | 28wk | 3 | Bilobed Placenta (low-lying ) | Network of vessels | 30 wk 2d, elective C.S. | Normal | |
| Oyelese et al. (2004) | 1 | No | 30 wk | 1 | 1 + 3D | Bilobed placenta | Large vessel | 35 wk, elective C.S. | Normal |
| 1 | Yes | 24 wk | 1 (3D) | 1 + 3D | Velamentous cord insertion | Network of vessels | 34 wk, elective C.S. | Normal | |
| Hsieh et al. (2006) | 1 | Yes | 27 wk | 1 (3D) | Velamentous cord insertion | Network of vessels | 34 wk, elective C.S. | Normal | |
| 1 | Yes | 35 wk | 1 (3D) | Succenturiate lobe | Network of vessels | 35 wk 2d, elective C.S. | Normal | ||
| Ushakov et al. (2006) | 1 | 15 wk | 1 | Velamentous cord insertion | Fetal vessels (in all 4 cases) as a network of vessels | Elective C.S. was done to all the cases | |||
| 1 | 22 wk | 1 | (All 4 cases) | ||||||
| 1 | 26 wk | 1 | |||||||
| 1 | 30 wk | 1 | |||||||
G.A. = gestational age; SGA = small for gestational age; PROM = premature rupture of membranes; CS = cesarean section; TAS = trans-abdominal sonography; TVS = trans-vaginal sonography; CDU = Color-Doppler ultrasonography.
Associated anomalies
The various reported associated anomalies are probably coincidental and include cephalocele (38), Scimitar syndrome (36) and Trisomy 21 (38). A few others can be related to compression or damage of the vessels by the presenting parts and includes heart rate anomalies (43), small for gestational age, and intra-ventricular hemorrhage in a twin or even intra-uterine fetal death (23).
Prognosis
The major complication from vasa previa is the rupture of the vessels carrying fetal blood. This occurs at or near delivery if the condition is undetected. These results in a perinatal mortality of 56% (56) in undiagnosed cases, and 3% in those diagnosed prenatally (56). The median Apgar score (1 and 5 min) is 8 and 9 when detected prenatally versus only 1 and 4 for survivors of undetected cases (56). Further, transfusion is required in 58% of newborn without prenatal diagnosis, versus only 3% of those diagnosed prenatally (56). A less well quantified complication is the compression of the vasa previa by the presenting part resulting in decreased flow to the fetus and possibly hypoxia (57). Postnatal complications are related to either prematurity (due to early C-section with no confirmation of lung maturity) and include hyaline membrane disease, bronchopulmonary dysplasia, transient tachypnea, respiratory distress syndrome, or to partial exsanguination and complications related to anemia, hypovolemic shock (23) or complications of transfusions (8).
Recurrence risk
No reported increased risk.
Management
The outcome is markedly improved (97% survival versus 44%) when a prenatal diagnosis is followed by elective C-section is performed at 35 weeks or earlier if signs of labor or membrane rupture occurs (56). Some have advocate hospitalization from 30–32 weeks with corticosteroids to assist in promoting lung maturity when the cervix is not demonstrated to be long and closed (58). When time permits, an amniocentesis to assess lung maturity is justified (59).
Advocacy
In the UK – UKVP raising awareness (http://www.vasapraevia.co.uk) has been very active in raising awareness on the issue (and their originators Daren & Natalie Samat deserve a lot of credit for their tireless work). The authors express their gratitude for their work and of the work of the International Vasa Previa Foundation (http://www.IVPF.org). Further, Dr. Oyelese has had the great kindness to review this manuscript and his many corrections are greatly appreciated.
Conclusions
Although no large-scale prospective studies are there to support these conclusions, personal experiences, case reports and smaller studies all concur to demonstrate a marked improvement in outcome when a vasa previa is detected prenatally. The obvious conclusion, until proven otherwise, is that a substantial improvement in outcome will depend only on prenatal detection. This implies a greater awareness of the condition and an effort at detecting it. The purpose of this manuscript is to help alert those who do prenatal examination that vasa previa are not difficult to recognize when sought and that they are common enough to be worth seeking.
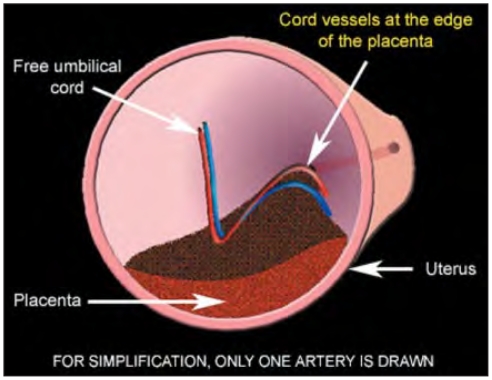
Figure 1.
Drawing showing the inner view to the uterus, towards the cervix, demonstrating the anatomical relations in case of succenturiate placenta. The vessels between the main and succenturiate lobe are crossing the inner cervical os.
Figure 2.
Drawing showing the inner view to the uterus, towards the cervix, demonstrating the anatomical relations in case of velamentous insertion of the umbilical cord.
Figure 3.
Drawing showing the inner view to the uterus, towards the cervix, demonstrating the anatomical relations in case of marginal placenta with vessels running at the edge of placenta and crossing the inner cervical os. By trophotropism, the marginal edge of the placenta regresses, leaving the vessel in front of the inner cervical os.
Figure 4.
Pathological specimen shows the fetal side of bilobate placenta with velamentous insertion of the umbilical cord between the placental lobes. (Courtesy Francois Manson and TheFetus.net).
Figure 5.
Pathological specimen shows the maternal side of the bilobate placenta. (Courtesy Francois Manson and TheFetus. net).
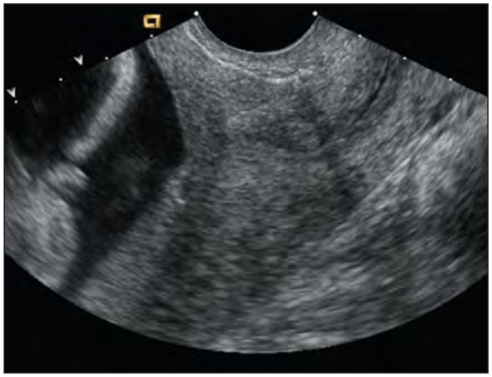
Figure 6.
Second trimester vaginal 2D sonography shows a sagittal section through the cervix. In this gray scale mode no vessels are visible crossing the inner cervical os.
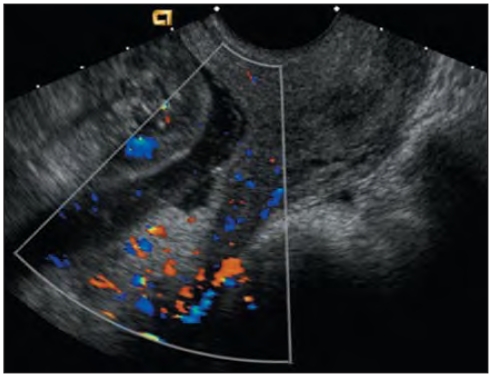
Figure 7.
The same scan as in image 5 using color Doppler shows a vasa previa crossing the inner cervical os.
Figure 8.
Second trimester vaginal 2D sonography shows a sagittal section through the cervix with the marginal placenta previa localized at the dorsal wall of the uterus.
Figure 9.
The same scan as in image 3 using color Doppler showing a vessel crossing the inner cervical os (vasa previa).
Figure 10.
Proposed diagnostic algorithm for the second-trimester detection of the vasa previa.
Figure 11.
A second trimester vaginal 2D ultrasonographic scan shows sagittal section through the cervix with amniotic fluid above.
Figure 13.
A second trimester vaginal 2D ultrasonographic scan shows sagittal section through the cervix with suspicious vessels crossing inner cervical os (arrow).
Figure 14.
The same scan as in figure 15 using the color Doppler clearly show that the suspicious structure is without Doppler signal and thus is not a vessel.
Figure 15.
Second trimester vaginal Doppler image shows a high frequency fetal hart rate at the level of vasa previa. This helps to distinguish vasa previa from maternal cervical vessels.
References
- 1.Lobstein J. Archives de L’art des Accouchements 1801. Strasbourg: p. 320. [Google Scholar]
- 2.Gianopoulos J, Carver T, Tomich PG, Karlman R, Gadwood K. Diagnosis of vasa previa with ultrasonography. Obstet Gynecol. 1987 Mar;69(3 Pt 2):488–91. [PubMed] [Google Scholar]
- 3.Oyelese KO, Turner M, Lees C, Campbell S. Vasa previa: an avoidable obstetric tragedy. Obstet Gynecol Surv. 1999 Feb;54(2):138–45. doi: 10.1097/00006254-199902000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Strassmann P. Placenta previa. Arch Gynecol. 1902;67:112. [Google Scholar]
- 5.Oyelese Y, Chavez MR, Yeo L, Giannina G, Kontopoulos EV, Smulian JC, Scorza WE. Three-dimensional sonographic diagnosis of vasa previa. Ultrasound Obstet Gynecol. 2004 Aug;24(2):211–5. doi: 10.1002/uog.1097. [DOI] [PubMed] [Google Scholar]
- 6.Francois K, Mayer S, Harris C, Perlow JH. Association of vasa previa at delivery with a history of second-trimester placenta previa. J Reprod Med. 2003 Oct;48(10):771–4. [PubMed] [Google Scholar]
- 7.Lee W, Kirk JS, Comstock CH, Romero R. Vasa previa: prenatal detection by three-dimensional ultrasonography. Ultrasound Obstet Gynecol. 2000 Sep;16(4):384–7. doi: 10.1046/j.1469-0705.2000.00188.x. [DOI] [PubMed] [Google Scholar]
- 8.Fung TY, Lau TK. Poor perinatal outcome associated with vasa previa: is it preventable? A report of three cases and review of the literature. Ultrasound Obstet Gynecol. 1998 Dec;12(6):430–3. doi: 10.1046/j.1469-0705.1998.12060430.x. [DOI] [PubMed] [Google Scholar]
- 9.Francois K, Mayer S, Harris C, Perlow JH. Association of vasa previa at delivery with a history of second-trimester placenta previa. J Reprod Med. 2003 Oct;48(10):771–4. [PubMed] [Google Scholar]
- 10.Raga F, Ballester MJ, Osborne NG, Bonilla-Musoles F. Role of color flow Doppler ultrasonography in diagnosing velamentous insertion of the umbilical cord and vasa previa. A report of two cases. J Reprod Med. 1995 Nov;40( 11):804–8. [PubMed] [Google Scholar]
- 11.Bernirschke K, Kaufmann P. Pathology of the human placenta. New York, NY: Springer-Verlag; 2000. pp. 353–359. [Google Scholar]
- 12.Israel R. Vasa previa in binovular twins. Report of a case. Obstet Gynecol. 1961 Jun;17:691–4. [PubMed] [Google Scholar]
- 13.Whitehouse DB, Kohler HG. Vasa praevia in twin pregnancy: report of two cases. J Obstet Gynaecol Br Emp. 1960 Apr;67:281–3. doi: 10.1111/j.1471-0528.1960.tb06993.x. [DOI] [PubMed] [Google Scholar]
- 14.Vago T, Caspi E. Antepartum bleeding due to injury of velamentous placental vessels. Obstet Gynecol. 1962 Nov;20:671–4. [PubMed] [Google Scholar]
- 15.Quek SP, Tan KL. Vasa previa. Aust N Z J Obstet Gynecol. 1972;12:206–9. doi: 10.1111/j.1479-828x.1972.tb00503.x. [DOI] [PubMed] [Google Scholar]
- 16.Toivonen S, Heinonen S, Anttila M, Kosma VM, Saarikoski S. Reproductive risk factors, Doppler findings, and outcome of affected births in placental abruption: a population-based analysis. Am J Perinatol. 2002 Nov;19(8):451–60. doi: 10.1055/s-2002-36868. [DOI] [PubMed] [Google Scholar]
- 17.Spellacy WN. Vasa previa, multiple pregnancies, and in vitro fertilization clarification. Fertil Steril. 2003 May;79( 5):1254–5. doi: 10.1016/s0015-0282(02)04943-9. [DOI] [PubMed] [Google Scholar]
- 18.Schachter M, Tovbin Y, Arieli S, Friedler S, Ron-El R, Sherman D. In vitro fertilization is a risk factor for vasa previa. Fertil Steril. 2002 Sep;78(3):642–3. doi: 10.1016/s0015-0282(02)03253-3. [DOI] [PubMed] [Google Scholar]
- 19.Oyelese Y, Spong C, Fernandez MA, McLaren RA. Second trimester low-lying placenta and in-vitro fertilization? Exclude vasa previa. J Matern Fetal Med. 2000 Nov-Dec;9(6):370–2. doi: 10.1002/1520-6661(200011/12)9:6<370::AID-MFM1011>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 20.Oyelese KO, Schwarzler P, Coates S, Sanusi FA, Hamid R, Campbell S. A strategy for reducing the mortality rate from vasa previa using transvaginal sonography with color Doppler. Ultrasound Obstet Gynecol. 1998 Dec;12(6):434–8. doi: 10.1046/j.1469-0705.1998.12060434.x. [DOI] [PubMed] [Google Scholar]
- 21.Schachter M, Tovbin Y, Arieli S, Friedler S, Ron-El R, Sherman D. In vitro fertilization is a risk factor for vasa previa. Fertil Steril. 2002 Sep;78(3):642–3. doi: 10.1016/s0015-0282(02)03253-3. [DOI] [PubMed] [Google Scholar]
- 22.Sauerbrei EE, Davies GL. Diagnosis of vasa previa with endovaginal color Doppler and power Doppler sonography: report of two cases. J Ultrasound Med. 1998 Jun;17( 6):393–8. doi: 10.7863/jum.1998.17.6.393. [DOI] [PubMed] [Google Scholar]
- 23.Lee W, Lee VL, Kirk JS, Sloan CT, Smith RS, Comstock CH. Vasa previa: prenatal diagnosis, natural evolution, and clinical outcome. Obstet Gynecol. 2000 Apr;95(4):572–6. doi: 10.1016/s0029-7844(99)00600-6. [DOI] [PubMed] [Google Scholar]
- 24.Clerici G, Burnelli L, Lauro V, Pilu GL, Di Renzo GC. Prenatal diagnosis of vasa previa presenting as amniotic band. ’A not so innocent amniotic band’. Ultrasound Obstet Gynecol. 1996 Jan;7(1):61–3. doi: 10.1046/j.1469-0705.1996.07010061.x. [DOI] [PubMed] [Google Scholar]
- 25.Devesa R, Munoz A, Torrents M, Carrera JM. Prenatal diagnosis of vasa previa with transvaginal color Doppler ultrasound. Ultrasound Obstet Gynecol. 1996 Aug;8(2):139–41. doi: 10.1046/j.1469-0705.1996.08020137-3.x. [DOI] [PubMed] [Google Scholar]
- 26.Hertzberg BS, Kliewer MA. Vasa previa: prenatal diagnosis by transperineal sonography with Doppler evaluation. J Clin Ultrasound. 1998 Oct;26(8):405–8. doi: 10.1002/(sici)1097-0096(199810)26:8<405::aid-jcu6>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 27.Araujo Junior E, Filho HA, Pires CR, Zanforlin Filho SM, Moron AF. Prenatal diagnosis of vasa previa through color Doppler and three-dimensional power Doppler ultrasonography. A case report. Clin Exp Obstet Gynecol. 2006;33( 2):122–4. [PubMed] [Google Scholar]
- 28.Sepulveda W. Velamentous insertion of the umbilical cord: a first-trimester sonographic screening study. J Ultrasound Med. 2006 Aug;25(8):963–8. doi: 10.7863/jum.2006.25.8.963. [DOI] [PubMed] [Google Scholar]
- 29.Odunsi K, Bullough CH, Henzel J, Polanska A. Evaluation of chemical tests for fetal bleeding from vasa previa. Int J Gynaecol Obstet. 1996 Dec;55(3):207–12. doi: 10.1016/s0020-7292(96)02746-4. [DOI] [PubMed] [Google Scholar]
- 30.Lindqvist PG, Gren P. An easy-to-use method for detecting fetal hemoglobin-A test to identify bleeding from vasa previa. Eur J Obstet Gynecol Reprod Biol. 2006;22 doi: 10.1016/j.ejogrb.2006.05.011. [DOI] [PubMed] [Google Scholar]
- 31.Oyelese Y, Jha RC, Moxley MD, Collea JV, Queenan JT. Magnetic resonance imaging of vasa praevia. BJOG. 2003 Dec;110(12):1127–8. [PubMed] [Google Scholar]
- 32.Nimmo MJ, Kinsella D, Andrews HS. MRI in pregnancy: the diagnosis of vasa previa by magnetic resonance imaging. Bristol Med Chir J. 1988 May;103(2):12. [PMC free article] [PubMed] [Google Scholar]
- 33.Lauria MR, Smith RS, Treadwell MC, Comstock CH, Kirk JS, Lee W, Bottoms SF. The use of second-trimester transvaginal sonography to predict placenta previa. Ultrasound Obstet Gynecol. 1996 Nov;8(5):337–40. doi: 10.1046/j.1469-0705.1996.08050337.x. [DOI] [PubMed] [Google Scholar]
- 34.Farine D, Peisner DB, Timor-Tritsch IE. Placenta previa--is the traditional diagnostic approach satisfactory? J Clin Ultrasound. 1990 May;18(4):328–30. doi: 10.1002/jcu.1870180418. [DOI] [PubMed] [Google Scholar]
- 35.Leerentveld RA, Gilberts EC, Arnold MJ, Wladimiroff JW. Accuracy and safety of transvaginal sonographic placental localization. Obstet Gynecol. 1990 Nov;76(5 Pt 1):759–62. doi: 10.1097/00006250-199011000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Catanzarite V, Maida C, Thomas W, Mendoza A, Stanco L, Piacquadio KM. Prenatal sonographic diagnosis of vasa previa: ultrasound findings and obstetric outcome in ten cases. Ultrasound Obstet Gynecol. 2001 Aug;18(2):109–15. doi: 10.1046/j.1469-0705.2001.00448.x. [DOI] [PubMed] [Google Scholar]
- 37.Lee W, Lee VL, Kirk JS, Sloan CT, Smith RS, Comstock CH. Vasa previa: prenatal diagnosis, natural evolution, and clinical outcome. Obstet Gynecol. 2000 Apr;95(4):572–6. doi: 10.1016/s0029-7844(99)00600-6. [DOI] [PubMed] [Google Scholar]
- 38.Sepulveda W, Rojas I, Robert JA, Schnapp C, Alcalde JL. Prenatal detection of velamentous insertion of the umbilical cord: a prospective color Doppler ultrasound study. Ultrasound Obstet Gynecol. 2003 Jun;21(6):564–9. doi: 10.1002/uog.132. [DOI] [PubMed] [Google Scholar]
- 39.Nomiyama M, Toyota Y, Kawano H. Antenatal diagnosis of velamentous umbilical cord insertion and vasa previa with color Doppler imaging. Ultrasound Obstet Gynecol. 1998 Dec;12(6):426–9. doi: 10.1046/j.1469-0705.1998.12060426.x. [DOI] [PubMed] [Google Scholar]
- 40.Heinonen S, Ryynanen M, Kirkinen P, Saarikoski S. Perinatal diagnostic evaluation of velamentous umbilical cord insertion: clinical, Doppler, and ultrasonic findings. Obstet Gynecol. 1996 Jan;87(1):112–7. doi: 10.1016/0029-7844(95)00339-8. [DOI] [PubMed] [Google Scholar]
- 41.Eddleman KA, Lockwood CJ, Berkowitz GS, Lapinski RH, Berkowitz RL. Clinical significance and sonographic diagnosis of velamentous umbilical cord insertion. Am J Perinatol. 1992 Mar;9(2):123–6. doi: 10.1055/s-2007-994684. [DOI] [PubMed] [Google Scholar]
- 42.Robert JA, Sepulveda W. Fetal exsanguination from ruptured vasa previa: still a catastrophic event in modern obstetrics. J Obstet Gynaecol. 2003 Sep;23(5):574. doi: 10.1080/0144361031000156636. [DOI] [PubMed] [Google Scholar]
- 43.Hasegawa J, Matsuoka R, Ichizuka K, Sekizawa A, Farina A, Okai T. Velamentous cord insertion into the lower third of the uterus is associated with intrapartum fetal heart rate abnormalities. Ultrasound Obstet Gynecol. 2006 Apr;27( 4):425–9. doi: 10.1002/uog.2645. [DOI] [PubMed] [Google Scholar]
- 44.Lijoi AF, Brady J. Vasa previa diagnosis and management. J Am Board Fam Pract. 2003 Nov-Dec;16(6):543–8. doi: 10.3122/jabfm.16.6.543. [DOI] [PubMed] [Google Scholar]
- 45.Hasegawa J, Matsouka R, Ichizuka K, Otsuki K, Sekizawa A, Farina A, Okai T. Cord insertion into the lower third of the uterus in the first trimester is associated with placental and umbilical cord abnormalities. Ultrasound Obstet Gynecol. 2006;28:183–186. doi: 10.1002/uog.2839. [DOI] [PubMed] [Google Scholar]
- 46.Hasegawa J, Matsuoka R, Ichizuka K, Sekizawa A, Farina A, Okai T. Velamentous cord insertion into the lower third of the uterus is associated with intrapartum fetal heart rate abnormalities. Ultrasound Obstet Gynecol. 2006;27:425–429. doi: 10.1002/uog.2645. [DOI] [PubMed] [Google Scholar]
- 47.Nelson LH, Malone PJ, King M. Diagnosis of vasa previa with transvaginal and color flow Doppler ultrasound. Obstet Gynecol. 1990;76:506. [PubMed] [Google Scholar]
- 48.Hseih F-J, Chen H-F, Ko T-M, et al. Antenatal diagnosis of vasa previa by color flow mapping. J Ultrasound Med. 1991;10:397. doi: 10.7863/jum.1991.10.7.397. [DOI] [PubMed] [Google Scholar]
- 49.Arts H, van Eyck Antenatal diagnosis of vasa previa by transvaginal color Doppler sonography. Ultrasound Obstet Gynecol. 1993;3:276. doi: 10.1046/j.1469-0705.1993.03040276.x. [DOI] [PubMed] [Google Scholar]
- 50.Meyer WJ, Blumenthal L, Cadkin A, et al. Vasa previa: Prenatal diagnosis with transvaginal color Doppler flow imaging. Am J Obstet Gynecol. 1993;169:1627. doi: 10.1016/0002-9378(93)90453-p. [DOI] [PubMed] [Google Scholar]
- 51.Hata K, Hata T, Fujiwaki R, et al. An accurate antenatal diagnosis of vasa previa with transvaginal color Dopplerultrasonography. Am J Obstet Gynecol. 1994;171:265. doi: 10.1016/0002-9378(94)90481-2. [DOI] [PubMed] [Google Scholar]
- 52.Fleming AD, Johnson C, Targy M, et al. Diagnosis of vasa previa with ultrasound and color flow Doppler: A case report. Nebraska Med J. 1996;81:191. [PubMed] [Google Scholar]
- 53.Stafford IP, Neumann E, Jarrell H. Abnormal Placental Structure and Vasa Previa. J Ultrasound Med. 2004;23:1521–2. doi: 10.7863/jum.2004.23.11.1521. [DOI] [PubMed] [Google Scholar]
- 54.Hsieh CTC, Wu JL, Wu HH, Yeh GP. Prenatal diagnosis of vasa previa with three-dimensional ultrasonography: report of two cases. Ultrasound in Obstetrics & Gynecology. 2006;28:512–14. [Google Scholar]
- 55.Ushakov F, Herman A, Tovbin Y, Sherman D, Maymon R. Vasa previa: early antenatal diagnosis. Ultrasound in Obstetrics & Gynecology. 2006;28:412. [Google Scholar]
- 56.Oyelese Y, Catanzarite V, Prefumo F, Lashley S, Schachter M, Tovbin Y, Goldstein V, Smulian JC. Vasa previa: the impact of prenatal diagnosis on outcomes. Obstet Gynecol. 2004 May;103(5 Pt 1):937–42. doi: 10.1097/01.AOG.0000123245.48645.98. [DOI] [PubMed] [Google Scholar]
- 57.Harding JA, Lewis DF, Major CA, Crade M, Patel J, Nageotte MP. Color flow Doppler--a useful instrument in the diagnosis of vasa previa. Am J Obstet Gynecol. 1990 Nov;163(5 Pt 1):1566–8. doi: 10.1016/0002-9378(90)90628-k. [DOI] [PubMed] [Google Scholar]
- 58.Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006 Apr;107(4):927–41. doi: 10.1097/01.AOG.0000207559.15715.98. [DOI] [PubMed] [Google Scholar]
- 59.Canterino JC, Mondestin-Sorrentino M, Muench MV, Feld S, Baum JD, Fernandez CO. Vasa previa: prenatal diagnosis and evaluation with 3-dimensional sonography and power angiography. J Ultrasound Med. 2005 May;24(5):721–4. doi: 10.7863/jum.2005.24.5.721. [DOI] [PubMed] [Google Scholar]