Abstract
Objective
To examine the usefulness of the Scale for the Assessment and Rating of Ataxia (SARA) in ataxic stroke patients.
Method
This was a retrospective study of 54 patients following their first ataxic stroke. The data used in the analysis comprised ambulation status on admission and scores on the SARA, the Korean version of the Modified Barthel Index (K-MBI) and the Berg Balance Scale (BBS). The subjects were divided into four groups by gait status and into five groups by level of dependency in activities of daily living (ADLs) based on their K-MBI scores. Data were subjected to a ROC curve analysis to obtain cutoff values on the SARA for individual gait status and levels of activity dependency. The correlations between the SARA, K-MBI and BBS scores were also computed.
Results
There was significant correlation between the SARA and the K-MBI scores (p<0.001), and this correlation (r=-0.792) was higher than that found between the BBS and the K-MBI scores (r=0.710). The SARA scores of upper extremity ataxia categories were significantly related to the K-MBI scores of upper extremity related function (p<0.001). The SARA scores were also significantly correlated negatively with ambulation status (p<0.001) and positively with ADL dependency (p<0.001). In the ROC analysis, patients with less than 5.5 points on the SARA had minimal dependency in ADL, while those with more than 23 points showed total dependency.
Conclusion
SARA corresponds well with gait status and ADL dependency in ataxic stroke patients and is considered to be a useful functional measure in that patient group.
Keywords: Ataxia, Stroke, Scale for the assessment and rating of ataxia
INTRODUCTION
Ataxia is recognized as one of various signs and symptoms, which may occur in a number of neurologic diseases, including stroke, and often has both clinical and anatomical diagnostic significance. Smooth and effective voluntary movement is achieved via the appropriate coordination and combination of agonist, antagonist, synergist, and fixator muscles. When such coordination is lost, ataxia, including defective fixation, decreased muscle strength, disorder of muscle tension, or involuntary movements, occur. In other words, although muscle strength is relatively well maintained, appropriate motor functions cannot be performed due to motor dysfunction and inappropriate motor responses.1 Ataxia is important not only for motor functions but also for the performance of daily living activities. Accordingly, accurate assessment of ataxia after a stroke is required to provide ataxia patients with an appropriate supplementary tool for walking, to determine the most effective treatment, and to identify safe and unsafe activities.2
The International Cooperative Ataxia Rating Scale (ICARS) has been widely used as a tool for assessing the severity and treatment effectiveness of cerebellar ataxia. However, the daily use of this scale in ataxic patients is difficult due to its many assessment items.3 Accordingly, Schmitz-Hübsch et al. recently proposed the Scale for the Assessment and Rating of Ataxia (SARA) as an alternative. This new assessment tool has fewer assessment items than the ICARS and therefore has the advantage of easier daily assessment of ataxia.4 Studies on the usefulness of SARA have been conducted to compare it with the existing ICARS and Barthel Index in cerebellar ataxia patients, but no study has been yet conducted on patients with ataxic stroke. Accordingly, this study was conducted on patients with ataxic stroke to investigate the usefulness of SARA by examining the correlation of SARA with the Korean Modified Barthel Index (K-MBI), the Berg Balance Scale (BBS), and gait status.
MATERIALS AND METHODS
Subjects
This study involved a retrospective review of the medical records of patients, who were admitted to the author's hospital and underwent comprehensive rehabilitation during the period March 2008 to February 2010. The patients selected for the study were those with ataxia, who were grade four or more in the defective area on the Medical Research Council Scale for assessing manual muscles strength.
Patients were excluded if they had previous brain diseases, difficulty in participating due to severe disorder of cognitive function, severe orthopedic problems such as loss of their lower extremities, fracture or arthritis, or a subarachnoid hemorrhage.
Methods
In the first neurological examination at the time of the patients' hospitalization, screening tests such as the finger to finger test, nose to finger test, and heel to shin sliding test were conducted. If abnormal findings were observed, the patients were suspected as having ataxia. Subsequently, the SARA, which Schmitz et al. proposed in 2006, the K-MBI, and the BBS were completed, and gait status was assessed. All the assessments were conducted by experienced doctors from the Department of Rehabilitation Medicine. The patients were divided into four groups: the independent gait group, the independent Q-cane gait group, the independent walker gait group, and the W/C ambulation group. 'Independent gait' was defined as the ability to walk 20 m or further without assistance.
For the level of independence in performing daily living activities, the patients were divided into five groups according to the classification criteria of the K-MBI: total dependence, severe dependence, maximal dependence, moderate dependence, and minimal dependence.
In the statistical analysis, receiver operating characteristic (ROC) curves were constructed. The ROC curves were used to determine the optimal (highest combination of sensitivity and specificity) cut-off scores on the SARA for discriminating between the various different levels of gait status and independence in ADLs. Pearson correlation coefficients were calculated to investigate the relationships between the SARA and K-MBI scores, the SARA and BBS scores, and the BBS and K-MBI scores. An observed p-value<0.05 was considered statistically significant.
RESULTS
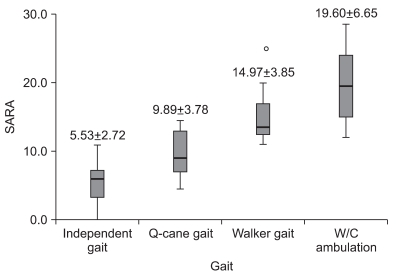
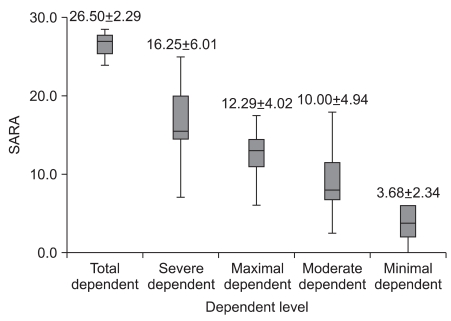
A total of 54 patients, who had suffered from ataxic stroke and were hospitalized and underwent rehabilitation treatment from March 2008 to February 2010, were eligible for inclusion in this study. The patients' mean age was 61.63±15.30 years, and the patients consisted of 32 males and 22 females (Table 1). No differences in the SARA scores were found in terms of stroke type or lesion location (p>0.05) (Table 2). In terms of gait status, the mean SARA scores for independent gait, Q-cane gait, walker gait, and W/C ambulation were 5.53, 9.89, 14.97, and 19.60, respectively, and gait status was significantly correlated with the SARA scores (p<0.01) (Fig. 1). With regard to level of ADL independence, the mean SARA scores for total dependence, severe dependence, maximal dependence, moderate dependence, and minimal dependence were 26.50, 16.25, 12.29, 10.00, and 3.68 points, respectively, and levels of independence were also significantly correlated with scores on the SARA (p<0.01) (Fig. 2).
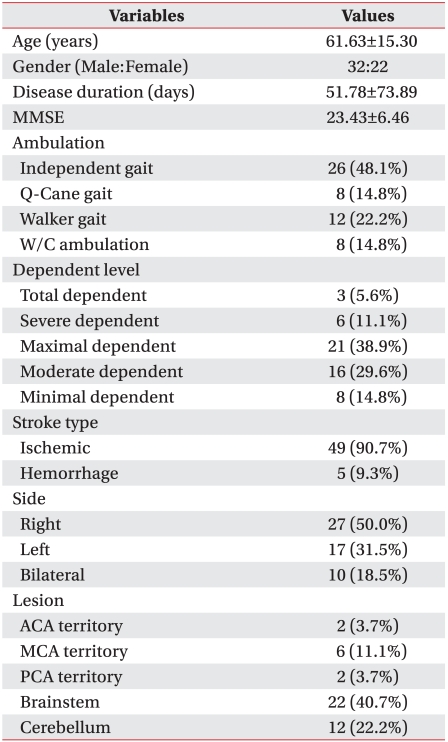
Table 1.
Characteristics of Study Participants
Values are mean±SD or N (%)
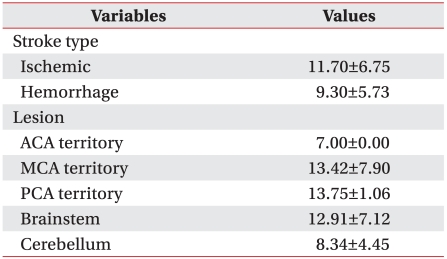
Table 2.
SARA Scores According to Stroke Type and Lesion
Values are mean±SD
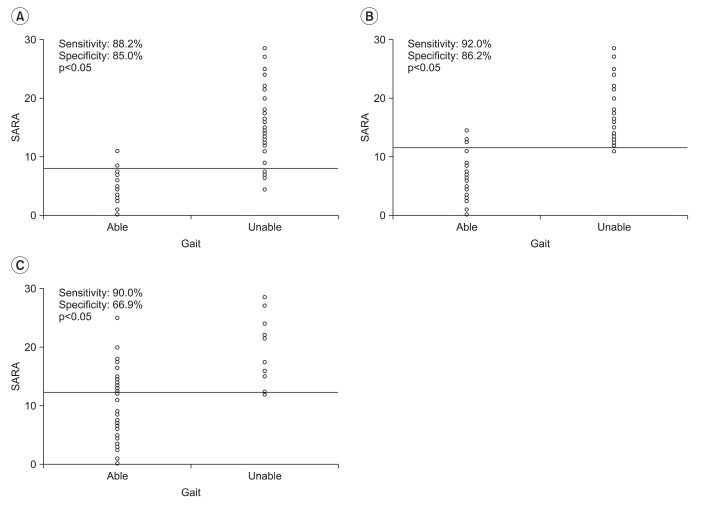
Fig. 1.
SARA score according to gait status. Values are mean±SD. Correlation is significant at the 0.01 level (2-tailed).
Fig. 2.
SARA score according to dependency level of ADL. Values are mean±SD. Correlation is significant at the 0.01 level (2-tailed).
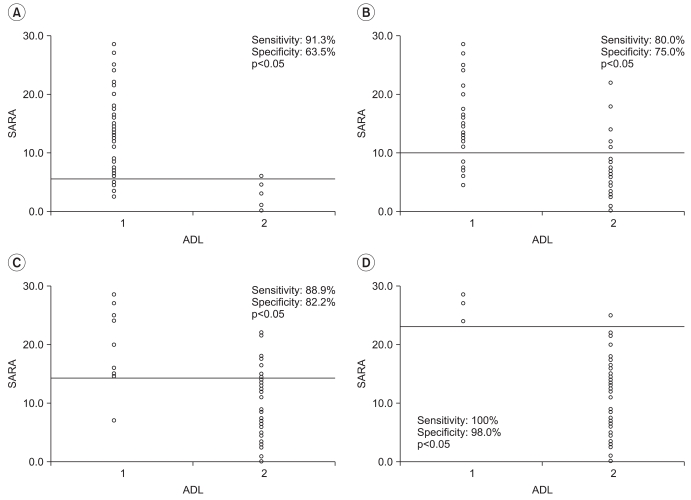
The analysis of the gait status showed that independent gait was achieved at a SARA score of 8 or lower, the Q-cane gait at 11.5 or lower, and the walker gait at 12.25 or lower (Fig. 3). For the performance of daily living activities, total dependence were achieved at SARA scores of 5.5 or lower, minimal dependence at 10.0 or lower, moderate dependence at 14.25 or lower, and maximal dependence at 23 or higher (Fig. 4).
Fig. 3.
The cutoff values measured by ROC curve analysis for independent gait (A), independent Q-cane gait (B) and independent walker gait (C) in the SARA. Cutoff values: (A) independent gait, 8; (B) independent Q-cane gait, 11.5: (C) independent walker gait, 11.25
Fig. 4.
The cutoff values measured by ROC curve analysis for mild dependent ADL (A), moderate dependent ADL (B), severe dependent ADL (C) and total dependent ADL (D) in the SARA. Cutoff values: (A) mild dependent ADL, 5.5; (B) moderate dependent ADL, 10; (C) severe dependent ADL, 14.25; (D) total dependent ADL, 23.
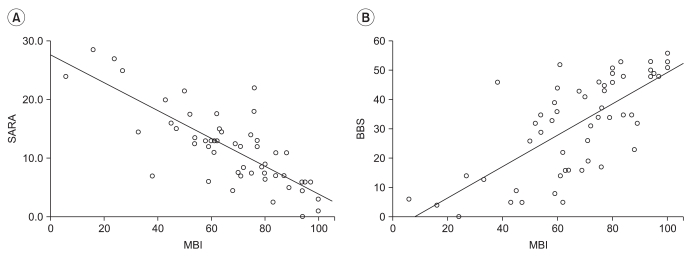
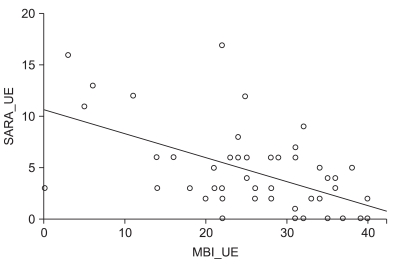
A strong inverse relationship was found between the SARA and K-MBI scores (r=-0.792, p<0.01), and the magnitude of this negative correlation was greater than that between the BBS and K-MBI scores (r=0.710, p<0.01) (Fig. 5). The SARA assessment items, which reflected ataxia of the upper extremities, showed a moderate negative correlation (r =-0.569, p<0.01) with the K-MBI assessment items related to the performance of daily living activities using the upper extremities (Fig. 6).
Fig. 5.
(A) Correlation between SARA and K-MBI scores (r=-0.792, p<0.01). (B) Correlation between BBS and K-MBI scores (r=0.710, p<0.01).
Fig. 6.
Correlation between SARA-UE and K-MBI-UE scores (r=-0.569, p<0.01).
DISCUSSION
This study was conducted to investigate the usefulness of the SARA with patients, who had suffered from ataxic stroke. The K-MBI scores were more highly correlated with SARA scores than with BBS scores.
The SARA, which Schmitz-Hubsch presented in 2004, is a tool for assessing ataxia. It has eight items with total scores ranging from 0 (no ataxia) to 40 (most severe ataxia). Scores for the eight items range as follows: no ataxia, 1: gait (0-8 points), 2: stance (0-6 points), 3: sitting (0-4 points), 4: speech disturbance (0-6 points), 5: finger chase (0-4 points), 6: nose-finger test (0-4 points), 7: fast alternating hand movement (0-4 points), 8: heel-shin slide (0-4 points), and 40: severe ataxia. For motor activities of the four extremities (items 5-8), assessments are performed bilaterally, and the mean values are used to obtain the total score.4
In a study of stroke patients with cerebral, cerebellar and brainstem lesions, Kim et al.5 reported that, using a sensory organization test, there were statistically significant differences in the balance coefficients and sensory analysis ratios between patients with cerebellar and brainstem lesions and patients with lobe lesions. They also found that patients with brainstem lesions were significantly different on a motor control test. No differences in the SARA scores were found according to the lesion location. This result was inconsistent with the result of a previous study, in which balance and posture control disorder was observed more in brainstem and cerebellar stroke patients than in middle cerebral artery stroke patients.5 This could be because the subjects of this study were stroke patients, whose ataxia was independent of the location of their lesions.
The most widely used assessment tools for the performance of daily living activities in current rehabilitation medicine are the Modified Barthel Index (MBI) and the Functional Independence Measure (FIM); in the present study the Korean version of the Modified Barthel Index (K-MBI), which was developed by Jung et al.6 in 2007, was used to assess the impacts of ataxia on the performance of daily living activities. A previous study of stroke patients reported a moderate correlation of the BBS with the FIM 7 and also a significant correlation of the SARA with the K-MBI. Thus, the correlation of ataxia with impaired performance of daily living activities was confirmed.
The correlation of SARA with K-MBI was shown to be stronger than the correlation of the BBS with the K-MBI. The K-MBI assessment items related to daily living activities involving use of the upper extremities were observed to be moderately correlated with those of SARA. Berg et al.8 developed the BBS in 1989 to assess the severity of falls among the elderly. The scale is composed of 14 items related to special movements, such as maintaining a standing posture with various degrees of difficulty and standing up from chair, and it can be used to measure the balance status and prognosis of stroke patients.9,10 It cannot, however, reflect problems in the performance of daily living activities, which are caused by the effects of ataxia on the upper extremities, because none of the items are designed to do this. In contrast, the SARA can reflect disorders of coordinated movement caused by ataxia in both the upper and lower extremities. To establish treatment goals and predict the prognosis for stroke patients during rehabilitation treatment, their status before the initiation of the rehabilitation treatment must be accurately assessed. If the degree of ataxia is pronounced without a correspondingly marked decrease in muscle strength, there is a risk of falls, and this risk is greater than for patients with decreased muscle strength.
Patients and their guardians are particularly interested in the recovery of gait and independence in the performance of daily living activities. In this study, the SARA was used in the assessment of ataxic stroke patients to provide the minimum SARA score for four gait-related activities and various degrees of independence in the performance of daily living activities. Independent gait, Q-cane gait, and walker gait were achieved at SARA scores of 8 or lower, 11.5 or lower, and 12.25 or lower, respectively. The analysis of the performance of daily living activities showed that minimal dependence, moderate dependence, maximal dependence, and total dependence were achieved at the SARA scores of 5.5 or lower, 10.0 or lower, 14.25 or lower, and 23 points or higher, respectively.
The results of this study can be used as a reference standard for assessing the gait ability of ataxic stroke patients and for setting rehabilitation treatment goals by indicating the appropriate gait status so that the risk of falls can be reduced.
This study had several limitations, such as the small sample size of patients and the lack of a standardized Korean version of the SARA. A further study is required to develop and standardize a Korean version of SARA. In addition, even though a significant statistical difference in the SARA scores was observed among the five daily living activity groups, there were no significant differences in the SARA scores between the severe and the maximal dependent group (p=0.06) nor between the maximal and the moderate dependent group (p=0.09). Further studies investigating the reference value of SARA in these K-MBI activity dependent groups will be necessary.
CONCLUSION
The SARA, which has been introduced as a new instrument for the assessment of ataxia, was found to be significantly correlated to the BBS and the K-MBI, and cutoff values were obtained for the four basic gait abilities and the five levels of independence in the performance of daily living activities. The use of the SARA with ataxic stroke patients as a rehabilitation index for gait ability and independence in the performance of daily living activities can be clinically valuable for both the assessment of ataxia and for rehabilitation planning.
Supplementary Material
Scale for the Assessment and Rating of Ataxia (SARA)
References
- 1.Hwang SH. Stroke and ataxia. Korean J Stroke. 1999;1:139–145. [Google Scholar]
- 2.Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008;88:559–566. doi: 10.2522/ptj.20070205. [DOI] [PubMed] [Google Scholar]
- 3.Trouillas P, Takayanagi T, Hallett M, Currier RD, Subramony SH, Wessel K, Bryer A, Diener HC, Massaquoi S, Gomez CM, et al. The Ataxia Neuropharmacology Committee of the World Federation of Neurology. International Cooperative Ataxia Rating Scale for pharmacological assessment of the cerebellar syndrome. J Neurol Sci. 1997;145:205–211. doi: 10.1016/s0022-510x(96)00231-6. [DOI] [PubMed] [Google Scholar]
- 4.Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, Giunti P, Globas C, Infante J, Kang JS, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66:1717–1720. doi: 10.1212/01.wnl.0000219042.60538.92. [DOI] [PubMed] [Google Scholar]
- 5.Kim HS, Lee KW, Sung DH, Hwang JH, Kim TU. Posturographic characteristics of lesion site in stroke patients. J Korean Acad Rehabil Med. 2000;24:363–369. [Google Scholar]
- 6.Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, Kim SH, Kim TH, Han TR. Development of the Korean Version of Modified Barthel Index (K-MBI): multicenter study for subjects with stroke. J Korean Acad Rehabil Med. 2007;31:283–297. [Google Scholar]
- 7.Jung HY, Kim TH, Park JH. Relationship between Berg Balance Scale and functional independence measure in stroke patients. J Korean Acad Rehabil Med. 2005;29:167–170. [Google Scholar]
- 8.Berg K, Wood-Dauphinee S, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311. [Google Scholar]
- 9.Dettmann MA, Linder MT, Sepic SB. Relationships among walking performance, postural stability, and functional assessments of the hemiplegic patient. Am J Phys Med. 1987;66:77–90. [PubMed] [Google Scholar]
- 10.Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Prediction of rehabilitation outcomes with disability measures. Arch Phys Med Rehabil. 1994;75:133–143. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Scale for the Assessment and Rating of Ataxia (SARA)