Abstract
A compelling association has been observed between cardiovascular disease (CVD) and depression, suggesting individuals with depression to be at significantly higher risk for CVD and CVD-related mortality. Systemic immune activation, hypothalamic–pituitary–adrenal (HPA) axis hyperactivity, arterial stiffness and endothelial dysfunction have been frequently implicated in this relationship. Although a differential epidemiological association between CVD and depression subtypes is evident, it has not been determined if this indicates subtype specific biological mechanisms. A comprehensive systematic literature search was conducted using PubMed and PsycINFO databases yielding 147 articles for this review. A complex pattern of systemic immune activation, endothelial dysfunction and HPA axis hyperactivity is suggestive of the biological relationship between CVD and depression subtypes. The findings of this review suggest that diagnostic subtypes rather than a unifying model of depression should be considered when investigating the bidirectional biological relationship between CVD and depression. The suggested model of a subtype-specific biological relationship between depression and CVDs has implications for future research and possibly for diagnostic and therapeutic processes.
Keywords: biological mechanisms, cardiovascular disease, endothelial dysfunction, inflammation, subtypes of depression
Introduction
The association between cardiovascular disease (CVD) and depression is well established and is suggested to be bidirectional. Numerous clinical and epidemiological studies investigating the association of depression and CVD have suggested that depression independently increases the risk of CVD 1.5-fold on average, and that patients with coronary artery disease and depression have a two- to threefold increased risk of future non-fatal and fatal cardiac events compared with those cardiac patients without depression.1, 2, 3, 4 Biological mechanisms that might link these two conditions together include the hypothalamic–pituitary–adrenal (HPA) axis, pro-inflammatory cytokines, changes of arterial elasticity and endothelial function (for reviews see refs 1,4,5,6,7,8,9,10,11,12,13,14).
Many epidemiological and clinical studies examining biological models of the relationship between CVD and depression have classified depression dichotomously either as yes/no or restricted analyses to major depression (MD) only. However, more recent research has begun to differentiate depressive subtypes such as dysthymia, melancholic MD (MMD), MD with typical or atypical features (see description of subtypes in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR); American Psychiatric Association15). Although differences in the strength of the association between various depression subtypes and CVD have been demonstrated,16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 it remains unclear if these subtype-specific associations are caused by a subtype-specific biological mechanism. Surprisingly, studies directly addressing this question are lacking. If this assumption would be true one would expect firstly that subtypes of depression are characterized by specific biological models and secondly that these specific models are also relevant for the pathogenesis of CVD.
The aim of this review is to identify biological models and correlates of subtypes of depression that might be involved in the relationship with CVD. This review proposes a differential subtype model of depression relevant for the association with CVD as opposed to a unifying model of depression that is commonly used in the literature on CVD and depression comorbidity.
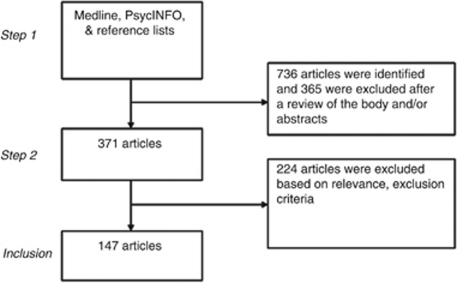
The literature search for this review was carried out according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines as they apply to systematic reviews.28 A systematic literature search was performed using the PubMed and PsycINFO databases covering articles from 1969–2011. The following search terms were used: (dysthymi* or (subsyndromal and depression) or (minor and depression) or (subthreshold and depression)) or bipolar disorder (BD) or MD or melanchol* or (depressi* and (melanchol* or atypical or psycho* or vascular)) and (immune or inflamm* or cytokine or glucocorticoid or cortisol or hypothalamus or endothelium or coag* or clotting or thrombosis). A second search was conducted as above, but with the addition of the following: and (CVD or stroke or ischemic heart disease or myocardial infarction or coronary heart disease or arterial stiffness or atherosclerosis). Articles were also obtained by reviewing reference lists of review and research articles. A total of 736 studies were found using these search terms. A total of 371 articles remained after assessment of abstracts for relevance to the aims of this review. Of these, 224 studies were excluded after review of the full text if they did not directly compare between subtypes of depression, did not provide data for individual subtypes, included child/adolescent populations or did not include measurement of relevant biomarkers. In most cases cross-sectional studies were also excluded; however, where studies of a longitudinal design were not available then cross-sectional studies were retained. In all, 147 studies were included in the final review (Figure 1).
Figure 1.
Study inclusion flowchart.
The bidirectional relationship between depression and CVD
The relationship between depression and CVD has been proposed to be bidirectional; existing depression increases the risk of incident CVD and a history of CVD increases the risk of depression. Many prospective and retrospective studies have investigated the association of existing depression and incident CVD.29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 Several meta-analyses of these studies have demonstrated a significant positive correlation with a moderate effect size of 1.5–2.7.3, 40, 41, 42
Similarly, several studies have investigated the role of depression status as a prognostic factor in patients with existing CVD.43, 44, 45, 46, 47, 48, 49, 50 Meta-analysis of these studies suggests that depressed patients have a 1.6–2.7-fold increased risk for further cardiovascular events within 24 months.42, 51, 52, 53 Conversely, relatively few studies have investigated the role of existing CVD in increasing the risk for the onset of depression (Supplementary Table).39, 43, 54 To our knowledge, this data has not been subjected to meta-analysis.
Analysis of the association between CVD and subtypes of depression reveals that the relationship with CVD appears to be particularly strong in patients with dysthymic disorder,16, 18, 19, 23 and BDs.16, 17, 22, 27 However, this literature is significantly limited by the paucity of prospective studies and studies that investigate a larger range of subtypes of depression (Table 1).
Table 1. Incidence, prevalence and associations between depression subtypes and cardiovascular diseases among clinical and community samples.
| Study | Objective | Design/sample | Subjects | Procedure | Differentiated between depressive subtypes | Cardiovascular outcomes | Results |
|---|---|---|---|---|---|---|---|
| Larson et al.19 | Examine relationship between lifetime occurrence of depressive disorder & stroke | Prospective/community | 1703 participants | Depression assessed with DIS. CVA self report or death certificate. Follow-up 13 years | Yes Depressive disorder, Dt | CVA | Depressive disorder RR of CVA: 2.67 (95% CI: 1.08–6.63) Dysthymia RR of CVA: 2.65 (95% CI: 0.69–10.11) |
| Osby et al.22 | Assess mortality in unipolar & bipolar disorders | Retrospective/population based | 15 386 bipolar and 39 182 unipolar disorder patients | Patients identified from inpatient register. ICD-8 definitions. | Yes Unipolar & bipolar depression | Cardiovascular cause of death Fatal CVA | Unipolar depression SMR for cardiovascular death in males: 1.5 (95% CI: 1.4–1.6), females 1.7 (95% CI: 1.7–1.8) SMR for fatal CVA in males: 1.5 (95% CI: 1.3–1.7), females 1.6 (95% CI: 1.5–1.8) Bipolar depression SMR for cardiovascular death in males: 1.9 (95% CI:1.8–2.1), females 2.6 (95% CI: 2.4–2.9) SMR for fatal CVA in males: 1.9 (95% CI:1.5–2.4), females 2.0 (95% CI: 1.7–2.4) |
| Penninx et al.23 | Examine & compare depression on cardiac mortality | Prospective/community | 2847 participants | CES-D, DIS assessed depression. CVD assessment unclear. Mean follow-up 4.2 years. | Yes Minor depression, MD | Cardiovascular cause of death | Major depressive disorder RR for cardiovascular death in patients without CVD at baseline: 3.9 (95% CI: 1.4–10.9) RR for cardiovascular death in patients with CVD at baseline: 3.0 (95% CI: 1.1–7.8) Minor depression RR for cardiovascular death in patients without CVD at baseline: 1.5 (95% CI: 0.9–2.6) RR for cardiovascular death in patients with CVD at baseline: 1.6 (95% CI: 1.0–2.7) |
| Baune et al.16 | Examine relation between affective subtypes & CHD, stroke, & HTN | Cross-sectional/community | 4181 participants | Depression assessed with CIDI. Self report CVDs. | Yes MD, BP I, BP II, Dt | Non-fatal CVA, CHD. HTN. | Unipolar major depressive disorder OR for CVA: 2.27 (95% CI: 1.29–3.99), CHD: 1.58 (95% CI: 1.09–2.30), HTN: 1.08 (95% CI: 0.86–1.37) Dysthymia OR for CVA: 2.10 (95% CI: 0.92–4.79), CHD: 2.03(95% CI: 1.21–3.39), HTN: 1.39 (95% CI: 0.97–1.99) Bipolar I OR for CVA: 5.71 (95% CI: 1.23–26.66), CHD: 3.04 (95% CI: 0.82–11.42), HTN: 1.44 (95% CI: 0.54–3.88) Bipolar II OR for CVA: no cases, CHD: no cases, HTN: 1.1 (95% CI: 0.23–5.21) |
| Herbst et al.18 | Examine the relationships between psychiatric disorders and CHD | Cross-sectional/community | 10 573 older adults | AUDADIS-IV assessed lifetime and past-year mood and anxiety disorders. Self report CVDs. | Yes MD, Dt, BP I, BP II | Non-fatal CHD. | Major depressive disorder OR for CHD with lifetime history: 2.05 (95% CI: 1.70–2.48), past-year history: 2.49 (95% CI: 1.81–3.43) Dysthymia OR for CHD with lifetime history: 2.37 (95% CI: 1.71–3.29), past-year history: 3.69 (95% CI: 2.37–5.75) Bipolar I OR for CHD with lifetime history: 2.64 (95% CI: 1.54–4.51), past-year history: 2.32 (95% CI: 1.08–4.97) Bipolar II OR for CHD with lifetime history: 1.29 (95% CI: 0.64–2.59), past-year history: 0.60 (95% CI: 0.19–1.94) |
| Goldstein et al.17 | Examine prevalence of CVDs (angina, arteriosclerosis, or MI) and HTN in bipolar I patients | Cross-sectional/clinical | 43 093 non-institutionalized subjects (BD-I=1411, MDD=6831, non-BDI=34 851) | AUDADIS-IV assessed for psychiatric diagnoses. Self report CVD. | Yes MDD, BD-I | Non-fatal CHD. HTN | Major depressive disorder OR for CHD: 2.70 (95% CI: 2.53–2.88), OR for HTN: 1.63 (95% CI: 1.55–1.72) Bipolar I OR for CHD: 4.95 (95% CI: 4.27–5.57), OR for HTN: 2.38 (95% CI: 2.16–2.62) |
Abbreviations: AUDADIS-IV, Alcohol Use Disorder and Associated Disabilities Schedule-DSM-IV Version; BP, bipolar disorder; CES-D, Centre for Epidemiologic Studies Depression Scale; CHD, coronary heart disease; CIDI, composite international diagnostic interview; CVA, cerebrovascular accident; CVD, cardiovascular disease; DIS, diagnostic interview schedule; Dt, dysthymia; HTN, hypertension; MD, major depression; MDD, major depressive disorder; OR, odds ratio; RR, risk ratio; SMR, standardized mortality ratio.
In addition to its association with CVD, depression is also significantly associated with several other major cardiac risk factors including smoking, obesity and diabetes.55, 56 Many studies, however, have demonstrated that depression remains independently associated with CVD even after adjusting for these risk factors. This suggests that there are other mediators of this relationship including both biological and behavioral mediators.2, 55
Biological mechanisms involved in the CVD-depression association
The relationship between depression and CVD has been proposed to be bidirectional; that is, existing depression increases the risk of incident CVD and a history of CVD increases the risk of depression. Many prospective and retrospective studies have investigated the association of existing depression and incident CVD.29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 Several meta-analyses of these studies have demonstrated a significant positive correlation with a moderate effect size of 1.5–2.7.3, 40, 41, 42 Similarly, several studies have investigated the role of depression status as a prognostic factor in patients with existing CVD.43, 44, 45, 46, 47, 48, 49, 50 Meta-analysis of these studies suggests that depressed patients have a 1.6–2.7-fold increased risk for further cardiovascular events within 24 months.42, 51, 52, 53 Conversely, relatively few studies have investigated the role of existing CVD in increasing the risk for the onset of depression.39, 43, 54 To our knowledge, this data has not been subjected to meta-analysis.
The association with CVD appears to be particularly strong in patients with dysthymic disorder,16, 18, 19, 23 and BDs.16, 17, 22, 27 However, this literature is significantly limited by the paucity of prospective studies and by studies that investigate a larger range of subtypes of depression.
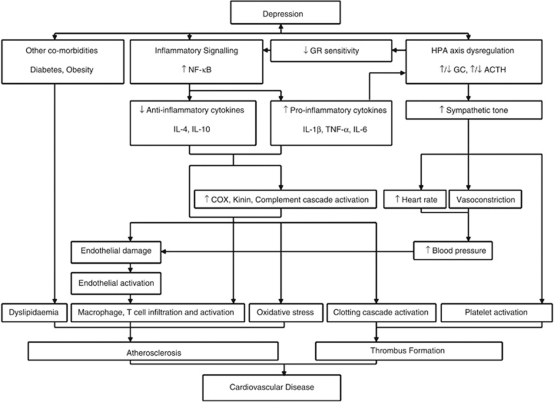
In addition to its association with CVD, depression is also significantly associated with several major cardiovascular risk factors, including smoking, obesity and diabetes.55 Many studies, however, have demonstrated that depression remains independently associated with CVD even after adjusting for these risk factors. This suggests that there are other factors impacting on this relationship, including both biological and behavioral mediators2, 55 (Figure 2).
Figure 2.
Biological mechanisms for the bidirectional relationship between depression and CVD.
Studies investigating immune system functioning in individuals with ‘depression', irrespective of depressive subtypes, have found that many of these individuals manifest elevated inflammatory markers, particularly c-reactive protein (CRP), interleukin-6 (IL-6), interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α).57, 58 Several authors have suggested that this association of depression and inflammatory markers may be a key biological link in the comorbidity of depression and CVD (see for reviews refs 1,4,7,10,12,13,59). This may be mediated by interactions of inflammatory signaling cascades with several key processes implicated in the pathogenesis and pathophysiology of CVD. Key among these processes is atherosclerosis. It has been proposed that inflammatory mediators may accelerate the progression of atherosclerosis through several mechanisms, including chemoattraction of leukocytes to atherosclerotic lesions, inducing endothelial activation and expression of adhesion molecules and stimulating the expression of vascular endothelial growth factors (see for review ref. 60). Furthermore, inflammatory signaling cascades may amplify and accelerate the process of coagulation and thrombus formation.61
It has been suggested that the dysfunction of the HPA axis may also contribute to the pathogenesis of depression and comorbid CVD.1, 7 This contribution may be mediated, at least in part, by the loss of glucocorticoid receptor-mediated negative feedback on inflammatory signaling. It is also worth noting that the disruptions of the HPA axis may be reciprocally regulated by altered expression of pro-inflammatory cytokines constituting a complex bidirectional biological crosstalk.62 Dysregulation of the HPA axis may also lead to sympathoadrenal hyperactivity via central pathways. This hyperactivity may lead to an increase in vasoconstrictive tone, heart rate and platelet activation each of which have been implicated in the progression to CVD.7, 63 Furthermore, excess sympathetic drive may result in reduced heart rate variability, which may increase vulnerability to arrhythmia.64
Endothelial dysfunction is a recognized risk factor for CVD that is also often observed in patients with depression.65, 66, 67, 68 In both ‘healthy' young volunteers and patients with CVD, depression status was associated with attenuated arterial dilatory responses to flow and nitroglycerin in addition to an increased expression of endothelial adhesion molecules and chemokines.69, 70 These factors may function to predispose these patients to atherosclerosis, thrombosis and vasospasm.
Biological mechanisms in depression subtypes relevant to CVD-depression comorbidity
More recent research has begun to investigate immune activation among depressed patients according to depression subtype, which might help to improve the understanding of the biological mechanisms underlying the relationship between CVD and depression.
MMD
Much research over the last decades has investigated whether the subtype of MMD may have a separate underlying pathophysiology to other non-melancholic forms of MD (NMMD) (Table 2a). Particularly relevant to CVDs are the investigation of immune alterations in MMD.
Table 2a. Differential biological mechanisms in subtypes of depression—melancholic vs atypical vs non-melancholic/atypical.
| Authors | Objective | Design/sample | Subjects | Procedure | Depressive subtypes | Results |
|---|---|---|---|---|---|---|
| Maes et al.21 | Examine if severe depression characterized by IL-6 production, if IL-6 activity in depression is related to alterations in APPs and HPA axis activity | Cross-sectional/clinical | 24 unipolar depressed inpatients and 8 control subjects | SCID, HSRD assessed depression | md, MMD, NMMD | PBMC IL-6 production: MMD >NMMD/md/controls (P<0.02) Haptoglobin: MDD/NMMD >controls/md (P<0.014) Transferrin: MDD/NMMD/md >controls (P<0.007) All other subgroup comparisons non-significant. DST non-significant. |
| Maes et al.79 | Determine if platelet aggregation, APTT or PT are disordered in subtypes of depression | Cross-sectional/clinical | 40 NMMD, 23 MMD, 16 MD and 16 controls | SCID assessed depression | NMMD, MMD, md | No significant difference between any subtypes and controls in PT, APTT or platelet aggregation to collagen or ADP. |
| Nelson and Davis78 | To perform a meta-analysis of DST studies published before 1997 | Meta-analysis of cross-sectional studies | 708 non-psychotic, 276 psychotic, 662 MMD and 617 NMMD | Meta-analysis | MMD, NMMD, psychotic/non-psychotic | Psychotic: OR of DST non-suppression in psychotic patients: 3.0 (95% CI, 2.2–4.1) Effect size did not differ significantly between studies (P=0.58) Melancholic: OR of DST non-suppression in MMD patients: 2.0 (95% CI, 1.5–2.6) Effect size varied significantly between studies (P<0.001) No effect for MMD when controlled for inpatient/outpatient status. |
| Ravindran et al.83 | Examine the levels of circulating lymphocyte subsets in depressive subtypes | Cross-sectional/clinical | 153 outpatients and 44 controls | MINI, HAM-D, BDI assessed depression | Depression, atypical depression, Dt, atypical Dt | NK cell counts: Typical MDD >atypical MDD/typical dysthymia >controls (P<0.01) No significant difference for atypical dysthymia No significant differences between T-cell populations in typical/atypical depression/dysthymia and controls. |
| Anisman et al.81 | Determine if cytokine alterations associated with depression related to neurovegative Sx or illness chronicity | Prospective/clinical | 74 depressed outpatients and 27 controls | HAM-D, MADRS and BDI measured depressive symptoms | Depression, atypical depression, Dt, atypical Dt | Relative to controls, ACTH levels elevated in atypical MD. Modest ACTH elevation in typical MD, but not in Dt. ↓ cortisol levels in atypical groups compared with typical groups. IL-1β levels elevated in Dt, irrespective of typical or atypical features. IL-1β correlated with illness duration. IL-2 production ↓ among each group. |
| Zaharia et al.84 | Examine mitogen-stimulated lymphocyte proliferation in subtypes of depression before and after treatment | Prospective/clinical | 88 depressed outpatients and 17 controls | SCID, CGI, MADRS, HAM-D, Atypical Depression Diagnostic Scale assessed depression | Depression, atypical depression, Dt, atypical Dt | Lymphocyte proliferative response to mitogen is reduced in both atypical and typical dysthymia relative to controls. Atypical dysthymia vs typical dysthymia=no significant difference. Typical MDD: attenuated proliferative response to Con A and low-dose PHA Atypical MDD: no difference in Con A response. Attenuated response to low-dose PHA. |
| Rothermundt et al.75 | Examine lymphocyte patterns in MMD and NMMD including whole blood mitogen-stimulated cytokine production | Prospective/clinical | 43 patients with depression and 43 controls | CIDI and HAM-D assessed depression. Immune functioning assessed at T1 (admission), T2 (after 2 weeks treatment), T3 (after 4 weeks treatment) | MMD, NMMD | IL-2: MMD < NMMD and controls at baseline (P<0.01) IFN-γ: MMD <NMMD and controls at baseline (P<0.05) Absolute lymphocyte count: NMMD >MMD and controls at all time points (P<0.05) No significant difference in serum cortisol, IL-10. |
| Rothermundt et al.75 | Examine innate immune patterns MMD and NMMD via whole blood LPS-stimulated cytokine production | Prospective/clinical | 43 patients with depression and 43 controls | CIDI and HAM-D assessed depression. Immune functioning assessed at T1 (admission), T2 (after 2 weeks treatment), T3 (after 4 weeks treatment) | MMD, NMMD | MMD had ↑ monocyte count and α-2-macroglobulin relative to NMMD and controls NMMD had ↑ CRP at T2 relative to MMD and controls. No significant differences for haptoglobins and ex-vivo whole blood-mitogen stimulated IL-1β production. |
| Schlatter et al.77 | Examine differences in lymphocyte and lymphocyte produced cytokines in MMD and NMMD | Prospective/clinical | 42 inpatients with depression and 20 controls | SCID, HAM-D, Newcastle Endogenicity Scale, assessed depression | MMD, NMMD | MMD had ↑CD4 and CD4:CD8 ratio >NMMD and controls (P=0.038). Difference remains in remission. No significant differences for CD8 or memory cells. MMD had ex-vivo PBMC mitogen-stimulated production ↑IL-2 >NMMD and controls (P=0.008). Normalized in remission. No significant differences for IL-4. ↓NK cell activity in NMMD patients in remission. Negative correlation between HAM-D and NK cell activity in NMMD patients at baseline. |
| Gecici et al.82 | Determine if serum leptin levels differ between depressive disorders with/without atypical features | Cross-sectional/clinical | 57 drug-free patients with depression and 26 controls | HDRS+unspecified assessment of atypical features | Depressive symptoms +/− atypical features | ↑Serum leptin in patients with atypical features relative to controls and those without atypical features. No significant difference between patients without atypical features and controls. |
| Kaestner et al.72 | Determine if HPA axis hyperactivity ↓ pro-inflammatory response in acute MD and if HPA axis hyperactivity and cytokine production normalizes during remission | Prospective/clinical | 37 acute MD inpatients and 37 controls | SCID and Newcastle Endogenicity Scale assessed depression | Acute and remitted MMD and NMMD | ACTH and serum cortisol concentrations ↑ MMD but not NMMD. NMMD >baseline IL-1β and IL-1RA than MMD and controls. Compared with MMD, NMMD had ↓ IL-1 RA/IL-1β ratio and ↑ upon remission. |
| Huang and Lee71 | Determine if there are differential serum cytokine expression profiles in patients with/without melancholic features and with/without suicide attempts | Cross-sectional/clinical | 42 inpatients with depression and 40 controls | SCID, HDRS assessed depression | MMD, NMMD | IL-1β: MMD >NMMD (P=0.023) IL-1β/IL-10 ratio: MMD >NMMD (P=0.015) No significant difference for TNF-α or IL-10 (P=0.22 and 0.17, respectively) |
| Marques-Deak et al.74 | Examine the levels of circulating cortisol and cytokines in patients with subtypes of MDD | Prospective/clinical | 46 female inpatients with depression and 41 controls | SCID, HDRS, CGI assessed depression | MMD, NMMD | No significant differences in serum IL-1β, IL-6, IFN-γ, cortisol between depressed patients and controls or MMD and NMMD. |
| Erdem et al.76 | Examine whether serum haptoglobin concentrations vary between patients with MMD, NMMD and controls | Cross-sectional/clinical | 37 MMD, 45 NMMD and 40 controls | SCID, HDRS assessed depression | MMD, NMMD | Serum haptoglobin was significantly higher in patients with MMD than NMMD (P<0.001). |
| Yoon et al.80 | Examine the profile of whole blood LPS stimulated cytokine expression in patients with major depression +/− atypical features | Cross-sectional/clinical | 70 patients with MDD and 35 patients with Atypical MDD | SCID, HDRS, BPRS assessed depression | MDD, Atypical MDD | TNF-α: no significant difference (P=0.64) IL-6: no significant difference (P=0.32) IL-2: atypical >non-atypical (P=0.002) IL-4: non-atypical >atypical (P=0.035) IL-2/IL-4: atypical >non-atypical (P=0.011) |
| Maes et al.73 | Examine indices of cell mediated immunity according to various symptom subgroups within depressive disorders | Cross-sectional/clinical | 83 patients with MDD and 26 controls | SCID, HDRS assessed depression | MMD, NMMD | Serum neopterin: MMD >NMMD (P=<10−6), depressed >controls. (P=4 × 10−5) Serum TNF-α: MMD >NMMD (P=6 × 10−6), depressed >controls. (P=5 × 10−5) Serum IL-1β: MMD=NMMD (P=0.08), depressed >controls (P=0.008). |
Abbreviations: ACTH, adrenocorticotropic hormone; APPs, acute phase proteins; APTT, activated partial thromboplastin time; BDI, beck depression inventory; CGI, Clinical Global Impressions Scale; CIDI, composite international diagnostic interview; CRP, C-reactive protein; Dt, dysthymia; DST, dexamethasone test; HAM-D, The Hamilton Depression Scale; HPA, hypothalamic–pituitary–adrenal Axis; IL, interleukin; INF-γ, interferon-γ MADRS, Montgomery-Asberg Depression Rating Scale; md, minor depression; MD, major depression; MDD, major depressive disorder; MINI-Plus, mini-international neuopsychiatry interview; MMD, melancholic major depression; NK-cells, natural killer cells; NMMD, non-melancholic major depression; OR, odds ratio; PT, prothrombin time; SCID, structured clinical interview for DSM; Sx, symptoms; TNF-α, tumor necrosis factor-alfa.
Many studies have investigated the profile of pro-inflammatory cytokines expressed in MMD as compared with NMMD; however, no consistent pattern has emerged. Of the pro-inflammatory cytokines IL-1β has been the most frequently investigated. Studies of serum IL-1β have variously reported increased,71 decreased72 or non-significantly different73, 74 levels in MMD relative to NMMD. Similarly, study of ex-vivo lipopolysaccharide stimulated whole blood IL-1β production have produced equivocal results.75 Other aspects of the IL-1 system have seldom been investigated, however, one study did report a decrease in the ratio of serum IL-1 receptor antagonist to IL-1β in NMMD compared with MMD, which normalized in clinical remission.72
Study of the cytokines IL-6 and TNF-α have also produced mixed results in similar investigations. No significant difference between MMD and NMMD was reported in serum;74 however, a study of ex-vivo mitogen-stimulated peripheral blood mononuclear cells did demonstrate an increase in IL-6 production in MMD relative to both NMMD and controls.21 There is also poor evidence of increased serum TNF-α in MMD relative to NMMD as reported by one study,73 yet others have found no significant difference in serum.71
In addition further aspects of the inflammatory response have also been investigated in MMD, including the acute phase proteins: CRP, haptoglobin and transferrin, and α-2-macroglobulin. Of these factors, CRP has been found to be elevated in NMMD relative to MMD and controls, whereas α-2-macroglobulin was higher in MMD relative to NMMD and controls.75 Haptoglobin and transferrin were found to be higher in both MMD and NMMD relative to controls but did not significantly vary between depressive groups.21 In contrast with these results, others have reported that serum haptoglobin was significantly higher in patients with MMD than NMMD,76 or else not different between MMD, NMMD or controls.75 Taken together, these consistently contradictory results in both pro-inflammatory cytokines and acute phase proteins suggest that the inflammatory system is unlikely to be differentially disordered in MMD as compared with NMMD.
Several authors have compared indices of adaptive immunity in MMD and NMMD. One study suggests an impairment of Th1-mediated immunity in MMD as these patients demonstrated reduced mitogen-stimulated whole blood IL-2 and interferon gamma (IFN-γ) production relative to both NMMD and controls at the untreated baseline.24 Other studies, however, have demonstrated an increase in the Th1 marker neopterin in serum relative to NMMD,73 and no significant difference in constitutive serum levels of the Th1 cytokine IFN-γ.74 A contrasting result has also been reported for IL-2 where MMD had greater ex-vivo peripheral blood mononuclear cell mitogen-stimulated production of IL-2 relative to NMMD and controls.77 This discrepancy from the earlier result may be explained by the reduction in absolute lymphocyte numbers observed in MMD patients in that study—thereby confounding the result in whole blood.24 In contrast to the Th1 cytokines no significant differences have been reported in the Th2 cytokines IL-4 and IL-10.24, 71, 77
Alterations in cell population numbers have also been observed in MMD relative to NMMD. One group noted an increase in the absolute CD4+ cell count in addition to an increased CD4+:CD8+ ratio that was not altered in clinical remission. This was not accompanied by any changes in absolute CD8+ cell count or other T-cell populations when comparing MMD and NMMD patients although natural killer cell activity was reduced in NMMD patients and significantly negatively correlated with depression severity.77 Another group reported an increased absolute monocyte count in NMMD relative to both MMD and controls,75 and the same group found no significant difference in absolute natural killer cell count between MMD and NMMD although the depressed groups were significantly higher than controls.24
HPA axis dysfunction has also been assessed as a potential differential biological marker for MMD. Several decades of studies utilizing the dexamethasone (DEX) suppression test as a potential discriminator between MMD and NMMD were included in a meta-analysis by Nelson and Davis,78 which found that there was no significant difference in rates of DEX suppression test non-suppression between MMD and NMMD after adjustment for inpatient/outpatient status. Other measures of HPA axis function such as serum adrenocorticotrophic hormone (ACTH) or cortisol have occasionally been reported in elevated levels in MMD as compared with NMMD,72 however, the majority of studies report no significant difference.21, 24, 74
It is also of particular relevance to note that a small study found no significant difference between MMD, NMMD, ‘minor depression' or controls in regards to several indices of coagulation; prothrombin time, activated partial thromboplastin time and platelet aggregation to collagen or adenosine diphosphate.79
Atypical depression
Relatively few studies have assessed differentially disordered biomarkers in atypical depression. A study of whole blood lipopolysaccharide stimulated cytokine production found that patients with atypical depression expressed more IL-2 and less IL-4 resulting in an overall increased IL-2:IL-4 ratio as compared with typical depression. The same study found no significant difference for TNF-α or IL-6.80 Such a report would suggest a Th1 shift in the basal immune state associated with atypical depression relative to typical depression. Another study of mitogen-stimulated peripheral blood mononuclear cells found no significant difference in IL-1β or IL-2 production between the atypical and typical depressive subtypes.81 A single report has also identified increased serum leptin as a marker of atypical depression, which was significantly different from both typical depression and controls.82 The significance of this result is unclear as it awaits replication.
Some evidence also suggests differentially disordered cell populations in typical compared with atypical depression. Although there appears to be no significant difference in lymphocyte cell counts,83 one study found that lymphocyte proliferative response to mitogens differed slightly between the subtypes; typical MD showed an attenuated proliferative response to both concavalin A and low-dose phytohemagglutanin whereas atypical MD showed an attenuated response to phytohemagglutanin only.84 The (patho-) physiological significance of this result is questionable. A single report also found natural killer cell counts to be significantly higher in typical MD than atypical MD, which was in turn significantly higher than controls.83 Indices of HPA axis dysfunction also do not appear to be differentially disordered between atypical and typical depression81 (Table 2a).
Dysthymia
The evidence for a differential biological profile in dysthymia is again inconsistent. Much of this investigation has focused on the pro-inflammatory cytokine IL-1β. One group investigated IL-1β in individuals with dysthymia and MD, and distinguished between typical and atypical features for both of these subtypes. Their results suggested that individuals with dysthymia, irrespective of whether typical or atypical features were present, had significantly elevated levels of IL-1β relative to controls. Although typical and atypical dysthymics had higher levels of IL-1β relative to typical and atypical major depressives, the authors did not report if these differences reached statistical significance. Additionally, concentrations of IL-1β increased with phytohemagglutinin dosage among all depressive subtypes but not for controls. Taken together, this study would seem to suggest that dysthymia, but not MD, is characterized by overexpression of IL-1β. Moreover, this overexpression was significantly and positively associated with baseline severity scores and duration of illness.81
More recent studies have also suggested that dysthymia may be characterized by higher overexpression of IL-1β than MD. In a study by Schlatter et al. the dysthymic group had significantly higher levels of IL-1β relative to controls, and ∼30% higher levels of IL-1β production relative to those with MD, however, this latter difference again did not reach significance. They also reported the absence of any associations between IL-1β and clinical characteristics of dysthymia such as severity or duration of illness.25, 26 Furthermore, they did not find significant differences in TNF-α expression between any of the depressive subtypes or between dichotomized depression and controls.25
These findings are somewhat complicated by those reported by Maes et al.20 In their study, Maes et al. found that MD patients had significantly higher IL-1β levels relative to controls, whereas intermediate levels of IL-1β were evident among patients with minor depression (dysthymia, adjustment disorder with depressed mood). However, as with the aforementioned studies, the differences in IL-1β levels between MD and dysthymia for IL-1β levels was not actually significant. However, comparison of these findings is difficult as in Maes et al. dysthymia and adjustment disorder with depressed mood were combined into the category of ‘minor depression', and information regarding the duration of depressive symptoms among dysthymic and MD patients was not reported.20
These same studies suggest that MD and dysthymia do not differ significantly in the level of overexpression of IL-6.21, 25, 26 A more recent study also found no significant difference between MD and dysthymia in plasma IL-6 or serum brain-derived neurotrophic factor.85
A recent genotypic analysis of patients with post-stroke depression determined that several polymorphisms were differentially associated with major and minor post-stroke depression. The IL-4+33C/C genotype was associated with post-stroke MD only, whereas the IL-10-1082A/A genotype was found to be associated with both post-stroke MD and minor depression.86
In addition to these investigations of cytokines, a series of studies by Thomas et al. detail the lack any significant differences between MD, controls and ‘subsyndromal depression' in serum levels of IL-1β, CRP, intercellular adhesion molecule-1 or vascular cell adhesion molecule-1.87, 88
Evidence of HPA axis dysfunction in dysthymia is also somewhat inconsistent. One group investigated cortisol levels in samples of patients with MD and minor depression, they found that with DEX and basal cortisol levels as covariates, MD patients had significantly higher post-DEX cortisol levels relative to controls, whereas patients with minor depression had intermediate levels.20 However, an earlier study by the same group found no significant difference between any subgroups of depression, including dysthymia and their controls.21
Little evidence suggests differential derangement of cellular indices in dysthymia. One study found natural killer cell counts to be higher in the atypical/typical subtypes of MD than the atypical/typical subtypes of dysthymia. The same study did not find any difference between MD and dysthymia in lymphocyte populations.83 No significant differences between MD and dysthymia were detected on mitogen-induced lymphocyte proliferation assays.84
A study investigating the indices of clotting prothrombin time, activated partial thromboplastin time and platelet aggregation to collagen or adenosine diphosphate found no significant difference between patients with minor depression and MD, or between depression groups and controls79 (Table 2b).
Table 2b. Differential biological mechanisms in subtypes of depression—dysthymia vs major depressive disorders.
| Authors | Objective | Design/Sample | Subjects | Procedure | Depressive subtypes | Results |
|---|---|---|---|---|---|---|
| Maes et al.21 | Examine if IL-1β production related to HPA axis activity in depressives | Cross-sectional/clinical | 28 inpatients with MDD or md (Dt or adjustment disorder with depressed mood) depression, 10 controls | SCID diagnosed depression. DST administered | MDD, md | MD patients ↑ post-DST cortisol relative to controls, md had intermediate levels. MDD patients ↑ IL-1β than controls. md had intermediate levels. IL-1β and post-DST cortisol values were correlated in depressives and controls. Cortisol non-suppressors had ↑ IL-1β than cortisol suppressors. |
| Maes et al.21 | Examine if severe depression characterized by IL-6 production, if IL-6 activity in depression is related to alterations in APPs and HPA axis activity | Cross-sectional/clinical | 24 unipolar depressed inpatients, 8 control subjects | SCID, HSRD assessed depression | md, MMD, NMMD | PBMC IL-6 production: MMD >NMMD/md/controls (P<0.02) Haptoglobin: MDD/NMMD >controls/md (P<0.014) Transferrin: MDD/NMMD/md >controls (P<0.007). All other subgroup comparisons non-significant. DST non-significant |
| Maes et al.79 | Determine if platelet aggregation, APTT or PT are disordered in subtypes of depression | Cross-sectional/clinical | 40 NMMD, 23 MMD, 16 md, 16 controls | SCID assessed depression | NMMD, MMD, md | No significant difference between any subtypes and controls in PT, APTT or platelet aggregation to collagen or ADP |
| Ravindran et al.83 | Examine the levels of circulating lymphocyte subsets in depressive subtypes | Cross-sectional/clinical | 153 outpatients, 44 controls | MINI, HAM-D, BDI assessed depression | Depression, atypical depression, Dt, atypical Dt | NK cell counts: typical MDD >atypical MDD and typical dysthymia >controls (P<0.01) No significant difference for atypical dysthymia. No significant differences between T cell populations in typical/atypical depression/dysthymia and controls. |
| Anisman et al.81 | Determine if cytokine alterations associated with depression related to neurovegative Sx or illness chronicity | Prospective/clinical | 74 outpatient depressives, 27 controls | HAM-D, MADRS, BDI measured depressive Sx | Depression, atypical depression, Dt, atypical Dt | Relative to controls, ACTH levels elevated in atypical MD. Modest ACTH elevation in typical MD, but not in Dt. ↓ cortisol levels in atypical groups compared with typical groups. IL-1β levels elevated in Dt, irrespective of typical or atypical features. IL-1 β correlated with illness duration. IL-2 production ↓ among each group |
| Zaharia et al.84 | Examine mitogen-stimulated lymphocyte proliferation in subtypes of depression before and after treatment | Prospective/clinical | 88 depressed outpatients, 17 controls | SCID, CGI, MADRS, HAM-D, atypical depression diagnostic scale assessed depression | Depression, atypical depression, Dt, atypical Dt | Lymphocyte proliferative response to mitogen is reduced in both atypical and typical dysthymia relative to controls. Atypical dysthymia vs typical dysthymia=no significant difference. Typical MDD: attenuated proliferative response to Con A and low dose PHA Atypical MDD: no difference in Con A response. Attenuated response to low-dose PHA. |
| Schlatter et al.25 | Examine cytokine production in depressed patients | Cross-sectional/clinical | 22 depressed patients, 15 controls | HAM-D and CGI were used to assess depression. HAM-A assessed anxiety | Depressed patients, Dt, MDD | Depressed patients (MD and Dt combined) had ↑ IL-1β and IL-6 relative to controls. No differences in TNF-α. Subtypes did not differ. Relative to controls, Dt patients had ↑ IL-1β, all subtypes had ↑IL-6. No correlation between IL production and HAM-D scores. Duration of illness correlated with TNF-α production in the depressed groups |
| Schlatter et al.26 | Examine differences in monocytic function in MD and Dt | Prospective/clinical | 22 depressed patients, 15 controls | Depressive Sx assessed with HAM-D-21 item, CGI and the Newcastle Scale | MDD, Dt | NS ↑ in monocyte count in depressives. ↑ IL-1β and IL-6 in depressives relative to controls. No differences between MD and Dt. No correlation between cytokine production and depression severity. TNF-α production after mitogen stimulation not different between patients and controls. Monocytic parameters not different between Dt and MD |
| Thomas et al.88 | Examine if IL-1β levels are ↑in late life depression | Prospective/clinical | 19 MD, 20 subsyndromal depressives, 21 controls | MMSE assessed cognition. Depressive Sx assessed with MADRS and GDS | MDD, subsyndromal depression | MDD ↑ IL-1β relative to controls. No significant difference between MDD, subsyndromal depression and controls in IL-1β or CRP. |
| Thomas et al.87 | Examine serum levels of cell adhesion molecules in elderly patients with depression | Cross-sectional/clinical | 23 MDD, 20 subsyndromal depression, 25 controls | MADRS, GDS assessed depression | MDD, subsyndromal depression | No significant correlations for ICAM-1, VCAM-1 or CRP |
| Yoshimura et al.85 | Examine serum BDNF and plasma IL-6 levels in patients with depression/dysthymia. | Cross-sectional/clinical | 20 MDD, 18 Dysthymic patients, 20 matched controls | SCID, HAM-D assessed depression | MDD, Dt | Serum BDNF: dysthymia/MDD < controls (P<0.0001). No significant difference dysthymia vs MDD. IL-6: dysthymia/MDD >controls. (P<0.0001). No significant difference dysthymia vs MDD. No correlation between BDNF and IL-6 |
| Kim et al.86 | Examine the association between cytokine gene polymorphisms and subtypes of post-stroke depression | Cross-sectional/clinical | 276 patients with stroke. (29 MDD, 48 minor depression, 199 controls) | MINI assessed depression | MDD, md | IL-4+33C/C genotype was associated with MDD only post-stroke (P=0.004) IL-10 -1082A/A genotype was associated with all post-stroke depression (P=0.012) |
Abbreviations: ACTH, adrenocorticotropic hormone; APPs, acute phase proteins; BD, bipolar disorder; BDI, beck depression inventory; BDNF, brain-derived neurotrophic factor; CGI, Clinical Global Impressions Scale; CRP, C-reactive protein; DST, dexamethasone test; Dt, dysthymia; GDS, Geriatric Depression Scale; HAM-A, Hamilton Anxiety Scale; HAM-D, The Hamilton Depression Scale; HPA, hypothalamic–pituitary–adrenal axis; IL, interleukin; INF-γ, interferon-γ MADRS, Montgomery-Asberg Depression Rating Scale; md, minor depression; MD, major depression; MDD, major depressive disorder; MINI-Plus, mini-international neuopsychiatry interview; MMD, melancholic major depression; MMSE, mini mental status examination; NK-cells, natural killer cells; NMMD, non-melancholic major depression; SCID, structured clinical interview for DSM; Sx, symptoms; TNF-α, tumor necrosis factor-alfa.
Psychotic depression
In biomarker studies of the psychotic subtype of depression most attention has concentrated on differential dysregulation of the HPA axis. Meta-analysis of DEX suppression test studies suggests that patients with psychotic depression were significantly more likely to be non-suppressors in response to DEX (odds ratio: 3.0, 95% confidence interval, 2.2–4.1),78 however, DEX suppression test studies published since have continued to report inconsistent results.89, 90 Other indices of HPA axis functioning have also been shown to discriminate between psychotic and non-psychotic MD. Intensive monitoring of serum cortisol levels suggests that patients with psychotic MD may have a higher mean serum cortisol,91 a higher cortisol nadir and higher evening cortisol relative to both patients with non-psychotic MD and controls.92, 93 However, others have found that the mean serum cortisol and 24 h cortisol amplitude did not differ between psychotic and non-psychotic MD.89, 94 Similarly, opposing results for 24 h ACTH levels have also been reported.91, 94 Examination of other hormones in the hypothalamus–pituitary axis have also shown no significant differences between psychotic and non-psychotic MD in assays of thyroid-stimulating hormone response to thyrotrophin-releasing hormone or growth hormone response to growth hormone releasing factor.90 These results may be tentatively interpreted to suggest there may be some degree of differential dysregulation in the HPA axis related to the psychotic/non-psychotic distinction within MD.
Other differential mechanisms potentially relevant to CVD have been reported. One study suggests that platelet serotonin was increased in samples from patients with psychotic MD as compared with non-psychotic MD.89 Also, plasma dopamine β-hydroxylase (the enzyme converting dopamine to norepinephrine) activity has been reported to be lower in patients with psychotic relative to non-psychotic MD95 (Table 2c).
Table 2c. Differential biological mechanisms in subtypes of depression—psychotic vs non-psychotic.
| Authors | Objective | Design/sample | Subjects | Procedure | Depressive subtypes | Results |
|---|---|---|---|---|---|---|
| Nelson and Davis78 | To perform a meta-analysis of DST studies published before 1997 | Meta-analysis of cross-sectional studies | 708 non-psychotic, 276 psychotic, 662 MMD, 617 NMMD | Meta-analysis | MMD, NMMD, psychotic/non-psychotic | Psychotic: OR of DST non-suppression in psychotic patients: 3.0 (95% CI, 2.2–4.1). Effect size did not differ significantly between studies (P=0.58) Melancholic: OR of DST non-suppression in MMD patients: 2.0 (95% CI, 1.5–2.6) Effect size varied significantly between studies (P<0.001). No effect size for MMD when adjusted for inpatient/outpatient status. |
| Pivac et al.89 | Examine relationships between plasma cortisol and platelet 5-HT concentrations in depressives | Prospective/clinical | 78 inpatients with recurrent unipolar depression | Depression assessment unclear. DST administered. Platelet 5-HT and cortisol levels assessed next day | Psychotic/ non-psychotic | Psychotic and non-psychotic MDD had ↑ cortisol than controls. Platelet 5-HT significantly different between groups and ↑ in psychotics than non-psychotics and controls. Non-psychotics had ↓ 5-HT than controls. Significantly more DST suppressors in non-psychotic than psychotic subgroup |
| Posener et al.94 | Examine HPA axis abnormalities in psychotic and non-psychotic depressed patients by intensive (hourly) cortisol and ACTH monitoring | Cross-sectional/clinical | 11 psychotic, 38 non-psychotic, 33 controls | SCID, HDRS, BPRS, CGI assessed depression. Hourly serum cortisol and ACTH | Psychotic/ non-psychotic | Cortisol amplitude was lower in the non-psychotic group relative to controls (P=0.02). No significant difference for psychotic group relative to controls or non-psychotics. 24 h mean ACTH was significantly higher in psychotic than non-psychotic depressed patients (P=0.03). |
| Belanoff et al.93 | To examine the association between cortisol levels and cognitive changes in psychotic major depression | Cross-sectional/clinical | 10 psychotic, 17 non-psychotic, 10 controls | HDRS assessed depression. Half-hourly serum cortisol | Psychotic/ non-psychotic | Non-psychotic and control subject demonstrated decreasing cortisol over the course of the afternoon. Psychotic major depression subjects demonstrated stable (and significantly higher P=0.004) cortisol over the course of the afternoon. |
| Cubells et al.95 | To examine for association between plasma dopamine β-hydroxylase activity in psychotic major depression and genotypes | Cross-sectional/clinical | 33 psychotic, 45 non-psychotic | SCID or SADS assessed depression | Psychotic/ non-psychotic | Plasma dopamine β-hydroxylase activity was significantly lower in the group with psychotic features compared with non-psychotic depression (P=0.007). Dopamine β-hydroxylase activity was associated with the C-1021T genotype, however, this did not account for the differences between groups. |
| Gomez et al.91 | Examine the association between serum cortisol/ACTH levels and neuropsychological indices in psychotic major depression | Cross-sectional/clinical | 29 psychotic, 24 non-psychotic, 26 controls | SCID, HDRS, BPRS assessed depression | Psychotic/ non-psychotic | Psychotic depression was associated with elevated mean cortisol in the measured time period relative to non-psychotic depression and controls (P<0.05). Cortisol appeared to partially mediate the relationship between psychotic depression and impairment of neuropsychological indices—particularly verbal memory and working memory. No significant differences between groups in ACTH. Sparse, inconsistent associations with neuropsychological indices. |
| Keller et al.92 | Examine circadian cortisol/ACTH levels in psychotic major depression | Cross-sectional/clinical | 29 psychotic, 24 non-psychotic, 26 controls | SCID, HDRS, BPRS assessed depression | Psychotic/ non-psychotic | Psychotic depression associated with higher evening cortisol, and higher cortisol nadir than non-psychotic and controls (P<0.02 and <0.05, respectively). Non-psychotic depression and controls did not differ (P=0.57). |
| Contreras et al.90 | Examine hypothalamus-pituitary hormone responses in psychotic/non-psychotic patients with melancholic major depression | Cross-sectional/clinical | 19 psychotic MMD, 21 non-psychotic MMD | SCID, HDRS assessed depression | Psychotic/ non-psychotic (within MDD subtype) | No significant differences between psychotic and non-psychotic MMD in DST, thyroid stimulating hormone response to thyrotrophin-releasing hormone, or growth hormone response to growth hormone releasing factor. |
Abbreviations: ACTH, adrenocorticotropic hormone; CGI, Clinical Global Impressions Scale; DST, dexamethasone test; HPA, hypothalamic–pituitary–adrenal Axis; 5-HT, 5-hydroxytryptamine receptors; MDD, major depressive disorder; MMD, melancholic major depression; NMMD, non-melancholic major depression; OR, odds ratio; SCID, structured clinical interview for DSM.
BDs
Several studies in patients with BD observed an activation of the immune system during the manic, the depressed or the euthymic states of bipolar illness. Some authors suggested that certain markers may be specific to each state, however, no consistent pattern has emerged as of yet. Several pro-inflammatory cytokines have been investigated in BD. Investigating the ex-vivo mitogen-stimulated cytokine production of peripheral blood mononuclear cells from manic patients with BD, a reduced production of IFN-γ was observed that persisted in both acute mania and remission.96 These findings were replicated by others, who also observed an increase in plasma levels of IL-1 receptor antagonist, sCD4 and sCD8 in mania.97 In contrast, Kim et al.98 were unable to replicate the finding of increased IFN-γ in a cohort of medication free manic patients, however, they did note an increase in the IFN-γ/IL-4 ratio which is purported to be a more valid measure of the pro-inflammatory activities of IFN-γ than IFN-γ levels alone.
Other pro-inflammatory cytokines have also been found to be elevated in bipolar mania. Several authors have demonstrated an elevation of TNF-α levels,99, 100 and two studies demonstrated an increase in soluble TNF receptor 1 although they failed to replicate the finding of increased TNF-α.101, 102 Similarly, several authors have documented increased IL-6 during a manic phase of bipolar illness.98, 99, 103 Elevations in pro-inflammatory cytokines are not restricted to the manic state as TNF-α was increased in both manic and depressed patients,99 a finding also reported for IL-6.103 Other authors have demonstrated elevations in the production of pro-inflammatory cytokines and CRP as a trait marker of BD, independent of the current psychopathological state.104, 105, 106 Earlier studies had also demonstrated raised levels of serum sIL-2R among rapid cycling107 and manic108 bipolar patients with normalization in remission.107, 108, 109 In contrast, some studies found no significant association between pro-inflammatory cytokines and BD regardless of current state.102, 110, 111, 112
A dysregulation of the production of anti-inflammatory cytokines IL-4 and IL-10 has also been implicated in BD. For example, it was reported that IL-10 is increased in patients with BD irrespective of the current psychopathological state.100, 106, 112 However, studies in cohorts of exclusively manic96, 97 or euthymic113 patients found no significant association with IL-10 levels.99, 111 In support of an increase in anti-inflammatory cytokines in BD, elevated levels of the anti-inflammatory cytokine IL-4 were repeatedly reported in both the manic and euthymic states of bipolar illness.98, 103, 113 In contrast, an ex-vivo examination of IL-4 could not find an association with mania.97
Beyond the investigation of inflammatory proteins as markers of diagnostic subtypes of BD, these immunological factors appear to be positively correlated with the severity of bipolar symptoms. Although some reported that serum CRP was associated with scores of the Young Mania Rating Scale score, but not Hamilton Depression scale score,114 others found that a Young Mania Rating Scale score was positively correlated with IL-2 and IL-6, and the Hamilton Depression scale with IL-6 only.103 These findings are not uncontested, however, as several other studies found no association between several of these markers (CRP, IL-6, IL-8, TNF-α, IL-12 and IL-10) and symptom severity in BD.99, 110, 115
Beyond the innate immune markers discussed above, a recent study has demonstrated derangement of indices of adaptive immunity including T-cell subtypes and cytokines.111 An emerging body of literature proposes that disruptions of T-cell mediated immunity may interact with the aforementioned mechanisms of inflammatory markers and HPA axis to contribute to the progression of neuropsychiatric disorders.116, 117
A key complication of studies in bipolar patients is the purported immune effects of lithium and other mood stabilizers. Several studies have demonstrated differences in immune parameters between lithium-treated patients and un-medicated patients,104, 113, 118 however, this effect is not always replicated.101, 102, 109, 114 Any immune-modulatory effect appears to be related to chronic treatment with this agent and could not be replicated by in-vitro addition of lithium to samples from un-medicated patients.104 Additionally, it was suggested that the progressive nature of BD may act as a confounder as the early and late stages of the illness showed a differential profile of TNF-α, IL-6 and IL-10 expression.106
Several studies have reported dysfunction of the HPA axis in patients with BD. Similarly to unipolar depression, BD patients frequently demonstrate non-suppression of the cortisol response to DEX and/or corticotrophin releasing hormone in manic,119, 120 mixed120 and depressed states.121 It is notable, however, that the largest study of HPA axis functionality in BD did not find any significant difference in post-DEX cortisol between BD patients and controls.122 Overall, the study results remain inconclusive as both, a normalization119, 121 and a continued elevation123, 124 of post-DEX cortisol suppression was found in remitted BD patients.
BD has also been associated with increased basal cortisol levels119, 122, 124 and a greater cortisol awakening response and increased diurnal cortisol slope.122 In remission, though, basal cortisol secretion was not significantly different from controls, suggesting that this finding may be a marker of illness activity.125
It is also relevant to note that one study has demonstrated increased levels of serum von-Willebrand factor in patients with BD when compared with controls102 (Tables 2d and 3).
Table 2d. Differential biological mechanisms in subtypes of depression—bipolar disorders vs major depressive disorders.
| Authors | Objective | Design/sample | Subjects | Procedure | Depressive subtypes | Results |
|---|---|---|---|---|---|---|
| Lesch et al.146 | Explore HPA axis in MD patients | Prospective/clinical | 12 patients with MDD (7 unipolar, 5 bipolar), 12 controls | Hamilton DRS completed 1 day before CRH test. DST performed 1 day after CRH test | MDD, BD | Relative to controls, depressives (MDD patients combined) ↑ baseline cortisol and significant attenuation of net ACTH responses. Normal cortisol secretion in response to CRH |
| Schmider et al.119 | Investigate the functionality of the HPA axis in Manic, depressed and remitted patients | Prospective/clinical | 11 manic BD-I patients, 11 MDD, 11 controls | SCID diagnosed BD/MDD. Mania assessed with Bech scale. Depression with HDRS | BD-I, MDD | Relative to controls, basal cortisol and ACTH were significantly increased in both depressed and manic patients. Post DEX/CRH cortisol and ACTH were significantly increased in both manic and depressed patients relative to controls. Remitted manic patients demonstrated significant decreases in both basal and post DEX/CRH cortisol and ACTH. |
| Rybakowski and Twardowska121 | Compare the combined DEX/CRH test in unipolar and bipolar depression in acute illness and remission | Prospective/clinical | 16 depressed patients with BD (4 BD-I, 12 BD-II), 24 MDD, 20 controls | SCID diagnosed BD and MDD. DEX/CRH test performed on admission and in remission. Depression assessed with HDRS | BD-I, BD-II, MDD | Patients with BD demonstrated significantly higher post DEX/CRH cortisol at all timepoints than patients with unipolar depression or controls. Cortisol response to DEX/CRH improved in remission in both BD and unipolar depression. Symptom severity on HDRS was significantly correlated to post DEX/CRH cortisol in both BD and unipolar depression. |
| Kim et al.115 | Examine plasma levels of IL-12 and compare between patients with schizophrenia, MDD, and BD and determine effects of pharmacotherapy | Prospective/clinical | 102 medication free psychiatric inpatients (43 schizophrenia, 34 major depression, 25 bipolar mania), 85 controls | SCID diagnosed BD, MDD or schizophrenia. YMRS for BD, HAM-D for MDD | BD-I, MDD | Relative to controls, IL-12 levels are increased in MDD patients irrespective of subtype, but not BD-I or schizophrenia patients. IL-12 levels decreased across all groups in response to pharmacotherapy. Plasma IL-12 levels were not associated with symptom severity. |
| Watson et al.123 | Investigate the role of arginine vasopressin in the HPA axis dysfunction of patients with BD and MDD | Cross-sectional/clinical | 23 patients with chronic MDD, 41 BD (21 remitted, 10 depressed, 10 rapid cycling) | SCID diagnosed BD, MDD. Mania assessed with YMRS. Depression with HAM-D. DST | MDD, BD | Relative to controls, both MDD and BD patients demonstrated higher post-DST levels of arginine vasopressin. This was maintained in remitted BD patients. |
| Huang and Lin105 | Examine the relationship between hsCRP levels and patients with MDD or BD | Cross-sectional/clinical | 23 outpatients with MDD, 13 BD-I, 31 controls | SCID diagnosed BD and MDD. Mania assessed with YMRS. Depression with HAM-D | MDD, BD-I | Serum CRP levels were significantly higher in patients with BD-I than controls. Serum CRP levels were not significantly higher in MDD patients than controls after covariate adjustment. |
| Hung et al.110 | Examine the relationship between insulin sensitivity and inflammatory markers in patients with MDD or BD-I | Cross-sectional/clinical | 21 young males with MDD, 15 BD-I, 14 controls | SCID diagnosed BD and MDD. Depression assessed with HAM-D | MDD, BD-I | Relative to controls, insulin sensitivity and serum adiponectin were negatively correlated to both BD and MDD. Insulin sensitivity was inversely related to HAM-D score. No significant difference was detected in serum CRP, TNF-α or IL-6. |
| Jabben et al.122 | Determine the contribution of manic symptoms to HPA axis alteration in bipolar/unipolar depression | Cross-sectional/clinical | 1134 patients with unipolar depression (MDD or Dt), 113 with BD, 304 controls | CIDI diagnosed MDD, Dt, BD. Depression assessed with IDS-SR. Salivary cortisol awakening response and DST 9 days after interview | (MDD, Dt combined for all analysis), BD-I, BD-II | Relative to controls, both unipolar and bipolar depression demonstrated a greater cortisol awakening response. The difference was more marked for unipolar patients. Bipolarity is associated with increased diurnal cortisol slope. There was no significant difference between unipolar or bipolar patients and controls on DST. |
Abbreviations: ACTH, adrenocorticotropic hormone; BD, bipolar disorder; CIDI, composite international diagnostic interview; CRP, C-reactive protein; Dt, dysthymia; DST, dexamethasone test; HAM-D, The Hamilton Depression Scale; HPA, hypothalamic–pituitary–adrenal Axis; IDS, inventory of depressive symptoms; IL, interleukin; MD, major depression; MDD, major depressive disorder; SCID, structured clinical interview for DSM; TNF-α, tumor necrosis factor-alfa; YMRS, Young Mania Rating Scale.
Table 3. Differential biological mechanisms within bipolar disorders.
| Authors | Objective | Design/sample | Subjects | Procedure | Depressive subtypes | Reported Severity of symptoms | Results |
|---|---|---|---|---|---|---|---|
| Rapaport et al.109 | Examine immune function in euthymic BD patients | Cross-sectional/clinical | 16 euthymic patients with BD-I, 10 BD-II, 34 controls | SCID diagnosed BD | BD-I, BD-II | No | Relative to controls BD patients had similar lymphocyte populations, sIL-2R and IL-2 levels. |
| Cassidy et al.120 | Investigate the utility of the DST in patients with manic or mixed episodes of BD | Cross-sectional/clinical | 46 inpatients with BD (37 manic, 7 mixed) | Diagnosis of BD with mixed/manic episode on admission. DST administered around day 5 of admission. Mania severity assessed with in-house scale | BD (manic/mixed) | Yes | A mixed episode was significantly associated with dexamethasone non-suppression as compared with a manic episode. Cortisol levels were significantly higher at all time points for patients with a mixed episode compared to manic patients. The relationship between mania severity score and cortisol level was non-significant. |
| Rapaport et al.107 | Examine immune function in rapid cycling BD patients before and after lithium treatment | Prospective/clinical | 17 rapid cycling bipolar patients (3 BD-I, 14 BD-II), 18 controls | SCID diagnosed BD. Cytokine assays at initiation of lithium, and at 4 weeks | BD-I, BD-II | No | Relative to controls, unmedicated symptomatic BD patients had higher levels of sIL-2R and sIL-6R. These levels normalized with lithium treatment. |
| Tsai et al.108 | Examine induces of cell mediated immunity in Bipolar mania | Prospective/clinical | 23 inpatients with BD in acute mania, 23 controls | SCID diagnosed BD. Cytokine assays when ⩾26 on YMRS (Manic) and ⩽12 on YMRS (remission) | BD-I (manic/remitted) | Yes | Relative to controls, manic BD patients had higher levels of sIL-2R. These levels decreased in remission. Mitogen induced lymphocyte proliferation was also increased in manic BD patients relative to BD patients in remission. |
| Su et al.96 | Examine ex-vivo mitogen stimulated IFN-γ and IL-10 production in patients with bipolar mania | Prospective/clinical | 20 inpatients with bipolar mania, 15 controls | SCID diagnosed BD. Cytokine assays when ⩾26 on YMRS (Manic) and ⩽12 on YMRS (remission) | BD-I (manic/remitted) | Yes | Relative to controls, BD-I patients demonstrated significantly lower IFN-γ production than controls in both manic and remitted states. No significant difference for IL-10 |
| Liu et al.97 | Examine lymphocyte and cytokine activity in bipolar patients in medicated and pre-medicated states | Prospective/clinical | 29 inpatients with bipolar mania, 20 controls | SCID diagnosed BD. Cytokine assays when ⩾26 on YMRS (Manic) and ⩽12 on YMRS (remission) | BD-I (manic/remitted) | Yes | Relative to controls, manic BD patients demonstrated increased plasma levels of IL-1ra, sCD4, sCD8 and decreased IFN-γ production. IL-1ra and sCD8 remained increased, and IFN-γ production remained decreased relative to controls when BD patients were in remission. No significant differences in IL-4 or IL-10. |
| Watson et al.124 | Assess basal salivary cortisol, and post DEX/CRH serum cortisol in bipolar patients | Cross-sectional/clinical | 53 outpatients with BD (27 remitted, 14 depressed, 12 subclinically depressed) 28 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression with HAM-D. DEX/CRH test performed | BD (manic/depressed/remitted) | Yes | Relative to controls, patients with BD demonstrated higher post DEX/CRH cortisol irrespective of remission or current symptoms. Basal salivary cortisol was not significantly different between BD patients and controls. Symptom severity was not associated with either measure of cortisol. |
| O'Brien et al.99 | Examine cytokine and cortisol levels in the plasma of manic of depressed patients with BD | Cross-sectional/clinical | 21 patients with BD, 42 controls | SCID diagnosed BD. Mania⩾26 on YMRS, Depression ⩾17 on HAM-D | BD-I (manic/depressed) | Yes | Relative to controls, both manic and depressed BD patients demonstrated increased plasma levels of IL-8, TNF-α. IL-6 was elevated in manic BD patients but not depressed BD patients. No difference in cortisol or IL-10 levels was observed between patients and controls. No correlation between symptom severity and cytokine levels was observed. |
| Deshauer et al.125 | Examine the normalization of salivary cortisol in remitted BD patients and offspring of BD patients | Cross-sectional/clinical | 15 remitted patients with BD (5 BD-I, 10 BD-II), 28 offspring of BD patients, 33 controls | SCID diagnosed BD. Remission ⩽1 score of > 13 on BDI-II in past 2 years. Salivary cortisol collected 6 times a day for 3 days, 3 consecutive weeks | BD-I, BD-II | No | Relative to controls, there was no significant difference in salivary cortisol levels in remitted BD patients or offspring of BD patients at any time point in the day. |
| Dickerson et al.114 | Examine the relationship between serum CRP levels and severity of BD symptoms | Cross-sectional/clinical | 122 outpatients with BD (91 BD-I, 30 BD-II), 165 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression with HAM-D | BD-I, BD-II | Yes | Serum CRP levels were significantly associated with YMRS score, but not HAM-D score. Serum CRP was also not significantly different between BD-I and BD-II. |
| Kim et al.98 | Examine the relationship between mitogen induced cytokine production and BD | Prospective/clinical | 37 manic inpatients with BD-I, 74 controls | SCID diagnosed BD | BD-I (response to treatment/no response) | No | Relative to controls, IL-6 and TNF-α production were higher in BD-I patients, and IL-4 production was lower. IFN-γ and IL-2 were not different from controls. IFN-γ/IL-4 ratio was higher in BD-I patients than controls. After 6 weeks of pharmacotherapy IL-6 levels decreased, however there were no significant changes in IL-2, IFN-γ, TNF-α, or IL-4. |
| Knijff et al.104 | Examine the ex-vivo IL-1β and IL-6 production of BD patients with/without lithium treatment | Cross-sectional/clinical | 80 patients with BD (61 BD-I, 19 BD-II), 59 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with CGI. Samples for lithium-free patients were treated with in-vitro lithium | BD-I, BD-II | Yes | Relative to controls, monocytes from non-lithium treated BD patients demonstrated increased IL-6 and decreased IL-1β production. Lithium treated BD patients did not demonstrate altered cytokine production. In-vitro exposure of monocytes did not replicate the effects of lithium treatment on cytokine production. No significant associations were found between manic, depressed, or euthymic states and cytokine production. |
| Brietzke et al.103 | Investigate serum chemokine levels in euthymic patients with bipolar disorder | Cross-sectional/clinical | 30 patients with BD-I, 30 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with HAM-D | BD-I (manic/depressed) | No | Relative to controls, euthymic patients with BD-I demonstrated an increase in CXCL10 and a reduction in CCL24 levels. No significant difference was demonstrated for CCL2, CCL3, CCL11, CXCL8, and CXCL9. |
| Brietzke et al.103 | Compare cytokine levels in depressed, manic and euthymic patients with bipolar disorder | Cross-sectional/clinical | 61 patients with BD-I, 25 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with HAM-D | BD-I (manic/depressed) | Yes | Relative to controls, IL-2, IL-4, and IL-6 were increased in the manic state, and IL-6 was increased in the depressed state. IL-4 was also increased in the euthymic state relative to controls. Manic symptoms (YMRS) demonstrated a positive correlation with both IL-6 and IL-2. Depressive symptoms (HAM-D) demonstrated a positive correlation with IL-6 only. |
| Hope et al.102 | Examine cytokine levels in patients with bipolar disorder and schizophrenia | Cross-sectional/clinical | 125 patients with BD (73 BD-I, 44 BD-II), 186 schizophrenia, 244 controls | SCID diagnosed BD and schizophrenia | BD-I, BD-II | No | Relative to controls, sTNF-RI and von-Willebrand factor were elevated in the serum of BD and schizophrenic patients. No significant difference was detected in sCD40L, IL-1ra, hsCRP, or IL-6. |
| Kauer-Sant'Anna et al.106 | Examine neurotrophin and cytokine levels in patients with BD-I in early and late stages of the disease | Cross-sectional/clinical | 60 patients with BD-I (30 early, 30 late), 60 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with HAM-D | BD-I (early/late stage) | Yes | Relative to controls, early stage BD-I demonstrated increased levels of TNF-α, IL-6 and IL-10. Late stage BD-I demonstrated increased levels of TNF-α and IL-6. Comparing early and late stage BD-I, TNF-α was significantly increased in the late stage, whereas IL-6 and IL-10 were significantly decreased. |
| Guloksuz et al.113 | Examine cytokine levels in euthymic bipolar patients | Cross-sectional/clinical | 31 euthymic BD patients (16 medication free) (26 BD-I, 5 BD-II), 16 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with HAM-D | BD-I, BD-II | No | Relative to controls, lithium treated euthymic patients demonstrated higher levels of TNF-α and IL-4. There were no significant differences between medication free euthymic BD patients and controls. There were no significant differences detected for IFN-γ, IL-10, IL-5, or IL-2. |
| Barbosa et al.101 | Examine levels of TNF-α and its soluble receptors in manic and euthymic BD patients | Cross-sectional/clinical | 53 patients with BD-I, 38 controls | MINI-Plus diagnosed BD. Mania assessed with YMRS. Depression assessed with HAM-D | BD-I (manic/remitted) | Yes | Relative to controls, BD patients demonstrated significantly higher sTNFR1 than controls. sTNFR1 was significantly higher in mania than euthymia. No significant differences were detected for TNF-α or sTNFR2. |
| Drexhage et al.111 | Examine indices of monocyte and T cell activation in patients with BD | Cross-sectional/clinical | 38 patients with BD, 22 controls | SCID diagnosed BD. Mania assessed with YMRS. Depression assessed with IDS | BD-I, BD-II | Yes | Relative to controls, younger (<40 YO) patients with BD demonstrated significantly higher levels of sCD25 and Treg cells. CCL2 and PTX3 were elevated in BD patients relative to controls. No significant differences were detected in TNF-α, IFN-γ, IL-1β, IL-3, IL-5, IL-6, IL-10, IL-17A, or IL-22. |
| Kapczinski et al.100 | Examine peripheral biomarkers in patients with BD and compare to patients with sepsis | Cross-sectional/clinical | 60 inpatients with BD, 80 controls, 15 sepsis | SCID diagnosed BD | BD (manic/remitted) | No | Relative to healthy controls, IL-10, TNF-α, neurotrophin 3, and several markers of oxidative stress were increased in patients with BD. There were no significant differences in IL-6 or brain derived neurotrophic factor. IL-10 was a marker of the depressed state, while IL-10 and TNF-α were markers of mania. Evidence of immune activation and oxidative stress were similar between patients with sepsis and BD. |
| Kunz et al.112 | Examine serum levels of IL-6, IL-10 andTNF-α inpatients with BD and schizophrenia | Cross-sectional/clinical | 20 euthymic patients with BD, 53 schizophrenia, 80 controls | SCID diagnosed BD and schizophrenia. Mania assessed with YMRS. Depression assessed with HAM-D | BD, schizophrenia | No | Relative to healthy controls, IL-10 levels were higher in patients with BD or schizophrenia. IL-6 was also increased in schizophrenia. No significant differences were determined for TNF-α. |
Abbreviations: BD, bipolar disorder; BDI, beck depression inventory; CGI, Clinical Global Impressions Scale; CRP, C-reactive protein; DST, dexamethasone test; HAM-D, The Hamilton Depression Scale; IDS, inventory of depressive symptoms; IL, interleukin; IFN-γ, interferon-γ MINI-Plus, mini-international neuopsychiatry interview; PT, prothrombin time; SCID, structured clinical interview for DSM; Sx, symptoms; TNF-α, tumor necrosis factor-alfa; YMRS, Young Mania Rating Scale.
Vascular depression
Vascular depression is associated with vascular disease, risk factors (e.g., diabetes mellitus, obesity) and late onset or change in the course of early-onset depression following the onset of vascular disease.126 The ‘vascular depression' hypothesis proposed by Alexopoulos et al.126 suggests that characteristics of cerebrovascular disease and their risk factors are involved in the development of late-life depression. This hypothesis is based on the observed high comorbidity between depression and CVDs as well as risk factors such as hypertension, diabetes, coronary artery disease, stroke and the high rate of silent stroke and white matter hyperintensities among elderly individuals with depression.126, 127, 128 A study by Krishnan et al.129 reported that the crude and adjusted risks for vascular depression were associated with age and late-onset depression. Clinical features in patients with vascular depression are characterized by significant loss of interests (apathy), cognitive dysfunction and psychomotor retardation.130 The degree of cognitive dysfunction observed in patients with vascular depression is usually greater than in patients with non-vascular depression.131 Causative factors of depression in the elderly are not well understood, though a role of biological risk factors, such as decreased arterial elasticity contributing to this late-life depression has been discussed.132
Decreased arterial elasticity, which is an important biological marker of atherosclerosis, has been observed in depressed patients. Arterial elasticity is an indication of an artery's structural and functional properties, that is, the artery's ability to stretch when under stress.133, 134 Increased arterial stiffness (decreased arterial elasticity) is associated with cerebrovascular disease and death independent of atherosclerosis and other factors133, 135, 136, 137 as well as with depression in the elderly.135 The strongest associations were seen among those who met the criteria for a DSM-IV depressive disorder (major or minor depression, or dysthymia) compared with those who reached a clinical level of depressive symptoms (CES-D score ⩾16) but did not meet the criteria for a depressive disorder. Those with a depressive disorder tended to have an increased risk for an abnormal distensibility coefficient of the common carotid artery and for an abnormal pulse wave velocity measurements, two markers of structural and functional vessel wall properties.138, 139, 140 Further studies support the hypothesis of arterial stiffness in depression.141 Arterial elasticity was examined in a sample of females with a lifetime DSM-IV-TR diagnosis of MD, currently depressed (onset ⩽30 days) with very severe depressive symptoms (HDRS-17 score ⩾24). Depressed patients had significantly higher baseline pulse wave velocity values relative to controls. Patients' pulse wave velocity and HDRS scores significantly decreased following a 6-week antidepressant treatment period. Significantly greater vascular improvements were seen among full responders to treatment (HDRS scores reduced by ⩾50%) as compared with partial responders indicating that patients' degree of improvement in arterial stiffness was related to the degree of reduction of depressive symptoms. Interestingly, clinical features such as illness duration, number of previous episodes, melancholic or psychotic features or electroconvulsive therapy did not alter the results. Taken together, these results suggest that clinically acute MDE may have a short-term effect on the vascular wall, which results in increased arterial stiffness possibly explaining some of the associations observed between CVD and depression.141
Summary
The association between CVDs and depression using the latter as a single diagnostic entity is well established and suggested to be bidirectional.5 With regard to subtypes of depression the association is less clear, but seems to vary in its strength by subtype. Also, reviews investigating if biological mechanisms implicated in the association between CVD and depression defined as a single entity would also apply to the various subtypes of depression are lacking. Thus, the aim of this review was to determine if a differential involvement of biological mechanisms for subtypes of depression is evident in the published literature and if so, if this contributes to explain differences in the strength of the association between CVD and depression subtypes.
This review suggests a dose-response relationship between the increasing severity of depressive symptoms and immune activation as well as HPA axis hyperactivity. It also found evidence that these two mechanisms are differently involved in the relationship with CVD depending upon depression subtype.20, 21, 24, 25, 72, 81, 88, 89, 142, 143 However, the identification of a subtype-specific functional pattern for both mechanisms is not possible at this stage as study results are inconsistent. Other mechanisms such as arterial stiffness or endothelial dysfunction, which also are involved in the relationship between the disease entity depression and CVDs have not been investigated in subtypes of depression, with the notable exemption of BD.66 The inconsistent study results are likely to be explained by the respective studies' limitations in terms of design factors and inconsistent methodologies. Many of the studies investigating biological mechanisms used samples that were small in number and heterogeneous in clinical and demographic participant characteristics such as severity of symptoms, duration of illness, number of comorbidities and histories of pharmacological and psychological therapies. They also varied significantly in the instruments and criteria used to classify depression, and techniques utilized in the measurement of biological markers. Another problem in the comparison of results is the variation in the delay between occurrence of CVD and assessment of depression and the heterogeneity in severity of CVDs. The paucity of longitudinal studies with a repeated assessment of both disease status is another limitation of reported studies.
On the other hand, and despite some overlap, the group of ‘CVDs' is also heterogeneous with different clinical characteristics, risk factors and prognoses. The vast majority of studies examined myocardial infarction as an endpoint within the group of CVDs when studying the association with depression, and the number of studies reporting on other cardiovascular endpoints is considerably smaller. At least two of the biological mechanisms described above, arterial stiffness and endothelial dysfunction, are established steps in the pathophysiological cascade of disease development and could be considered endpoints in themselves. Thus, for a better understanding of a causal relationship it is not only necessary to differentiate between subtypes of depression but also between cardiovascular endpoints. An alternative approach for the latter is the analysis of the relationships of subtypes of depression with subclinical disease, for example, intima-media-thickness or vascular brain lesions such as white matter lesions and lacunar infarcts, or, to study the association between subtypes of depression and specific biological mechanisms directly. The latter is possible for some of the discussed mechanisms, for example, arterial stiffness, endothelial dysfunction and to some extent the activation of the immune system and dysfunction of the HPA axis. These analyses, however, have to be prospective in design with repeated assessments of the clinical disease status as well as the subclinical or biological surrogates. The differences in the strength of associations between specific subtypes of depression and CVDs, as reported in the literature, suggests that different biological mechanisms might be involved in mediating these associations. This assumption would enable researchers to describe distinct (patho-) physiological profiles for subtypes of depression.
The implications for psychological treatment in reducing CVD mortality have also been raised. It has been suggested that if depression does indeed cause an increase in CVD mortality, then one would expect to see a reduction in mortality following psychological intervention. However, recent studies have not confirmed this expectation.144, 145 Additionally, although depression may be a factor that predisposes a patient to the development of CVD, it may not necessarily be the factor that maintains the development of CVD. Systemic immune activation may be stimulated by one depressive episode and ongoing regardless of the episode going into remission through treatment. Very little research has investigated inflammation and depression longitudinally. Moreover, a different concept may be required for elderly patients among whom vascular depression is commonly seen.
A concept that applies a differential model of CVD and depressive subtypes may be more appropriate compared with a unifying model of depression used in the past. Research moving beyond the unifying model and assessing both single CVDs and depressive subtypes longitudinally may enhance efforts to unravel causes and mechanisms of the bidirectional relationship between CVD and depression. Such research would potentially lead to the development of timely and appropriate measures for detection, prevention and treatment for CVD and depression.
Acknowledgments
The study is supported by a research grant from the German Ministry of Education and Research (BMBF).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
Supplementary Material
References
- Goldston K, Baillie AJ. Depression and coronary heart disease: a review of the epidemiological evidence, explanatory mechanisms and management approaches. Clin Psychol Rev. 2008;28:288–306. doi: 10.1016/j.cpr.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F. Depression and cardiac risk: present status and future directions. Heart. 2010;96:173–176. doi: 10.1136/hrt.2009.186957. [DOI] [PubMed] [Google Scholar]
- Van der Kooy K, Van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22:613–626. doi: 10.1002/gps.1723. [DOI] [PubMed] [Google Scholar]
- Rudisch B, Nemeroff CB. Epidemiology of comorbid coronary artery disease and depression. Biol Psychiatry. 2003;54:227–240. doi: 10.1016/s0006-3223(03)00587-0. [DOI] [PubMed] [Google Scholar]
- Grippo AJ, Johnson AK. Biological mechanisms in the relationship between depression and heart disease. Neurosci Biobehav Rev. 2002;26:941–962. doi: 10.1016/s0149-7634(03)00003-4. [DOI] [PubMed] [Google Scholar]
- Maes M. Evidence for an immune response in major depression: a review and hypothesis. Prog Neuropsychopharmacol Biol Psychiatry. 1995;19:11–38. doi: 10.1016/0278-5846(94)00101-m. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Whellan DJ, O'Connor CM. Depression and cardiovascular disease: mechanisms of interaction. Biol Psychiatry. 2003;54:248–261. doi: 10.1016/s0006-3223(03)00568-7. [DOI] [PubMed] [Google Scholar]
- Dantzer R, O'Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9:46–56. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronfol Z. Immune dysregulation in major depression: a critical review of existing evidence. Int J Neuropsychopharmacol. 2002;5:333–343. doi: 10.1017/S1461145702003024. [DOI] [PubMed] [Google Scholar]
- Lippi G, Montagnana M, Facaloro E, Franchini M. Mental depression and cardiovascular disease: a multifaceted, bidirectional association. Semin Thromb Hemost. 2009;35:325–336. doi: 10.1055/s-0029-1222611. [DOI] [PubMed] [Google Scholar]
- Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kop WJ, Gottdiener JS. The role of immune system parameters in the relationship between depression and coronary artery disease. Psychosom Med. 2005;67 (Supplement_1:S37–S41. doi: 10.1097/01.psy.0000162256.18710.4a. [DOI] [PubMed] [Google Scholar]
- Brown ES, Varghese FP, McEwen BS. Association of depression with medical illness: does cortisol play a role. Biol Psychiatry. 2004;55:1–9. doi: 10.1016/s0006-3223(03)00473-6. [DOI] [PubMed] [Google Scholar]
- Grippo AJ, Johnson AK. Stress, depression and cardiovascular dysregulation: a review of neurobiological mechanisms and the integration of research from preclinical disease models. Stress. 2009;12:1–21. doi: 10.1080/10253890802046281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association AP Diagnostic and Statistical Manual of Mental Disorders4th edn, Text Revision 2000,American Psychiatric Association: Arlington, VA [Google Scholar]
- Baune BT, Adrian I, Arolt V, Berger K. Associations between major depression, bipolar disorders, dysthymia and cardiovascular diseases in the general adult population. Psychother Psychosom. 2006;75:319–326. doi: 10.1159/000093955. [DOI] [PubMed] [Google Scholar]
- Goldstein BI, Fagiolini A, Houck P, Kupfer DJ. Cardiovascular disease and hypertension among adults with bipolar I disorder in the United States. Bipolar Dis. 2009;11:657–662. doi: 10.1111/j.1399-5618.2009.00735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbst S, Pietrazak R, Wagner J, White W, Petry N. Lifetime major depression is associated with coronary heart disease in older adults: results from the national epidemiologic survey on alcohol and related conditions. Psychosom Med. 2007;69:729–734. doi: 10.1097/PSY.0b013e3181574977. [DOI] [PubMed] [Google Scholar]
- Larson S, Owens P, Ford D, Eaton W. Depressive disorder, dysthymia, and risk of stroke: thirteen-year follow-up from the baltimore epidemiologic catchment area study. Stroke. 2001;32:1979–1983. doi: 10.1161/hs0901.094623. [DOI] [PubMed] [Google Scholar]
- Maes M, Bosmans E, Meltzer HY, Scharpe S, Suy E. Interleukin-1β: a putative mediator of HPA axis hyperactivity in major depression. Am J Psychiatry. 1993;150:1189–1193. doi: 10.1176/ajp.150.8.1189. [DOI] [PubMed] [Google Scholar]
- Maes M, Scharpe S, Meltzer H, Bosmans E, Suy E, Calabrese J, et al. Relationships between interleukin-6 activity, acute phase proteins, and function of the hypothalamic-pituitary-adrenal axis in severe depression. Psychiatry Res. 1993;49:11–27. doi: 10.1016/0165-1781(93)90027-e. [DOI] [PubMed] [Google Scholar]
- Osby U, Brandt L, Correia N, Ekbom A, Sparen P. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- Penninx B, Beekman A, Honig A, Deeg D, Schoevers R, Eijk JV, et al. Depression and cardiac mortality: results from a community-based longitudinal Study. Arch Gen Psychiatry. 2001;58:221–227. doi: 10.1001/archpsyc.58.3.221. [DOI] [PubMed] [Google Scholar]
- Rothermundt M, Arolt V, Fenker J, Gutbrodt H, Peters M, Kirchner H. Different immune patterns in melancholic and non-melancholic major depression. Eur Arch Psychiatry Clin Neurosci. 2001;251:90–97. doi: 10.1007/s004060170058. [DOI] [PubMed] [Google Scholar]
- Schlatter J, Ortuño F, Cervera-Enguix S. Differences in interleukins' patterns between dysthymia and major depression. Eur Psychiatry. 2001;16:317–319. doi: 10.1016/s0924-9338(01)00585-5. [DOI] [PubMed] [Google Scholar]
- Schlatter J, Ortuño F, Cervera-Enguix S. Monocytic parameters in patients with dysthymia versus major depression. J Affect Dis. 2004;78:243–247. doi: 10.1016/S0165-0327(02)00316-6. [DOI] [PubMed] [Google Scholar]
- Callaghan RC, Khizar A. The incidence of cardiovascular morbidity among patients with bipolar disorder: a population-based longitudinal study in Ontario, Canada. J Affect Dis. 2010;122:118–123. doi: 10.1016/j.jad.2009.06.029. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassertheil-Smoller S, Applegate W, Berge K, Chang C, Davis B, Grimm R, et al. Change in depression as a precursor of cardiovascular events. Arch Inter Med. 1996;156:553–561. [PubMed] [Google Scholar]
- Everson SA, Roberts RE, Goldberg D, Kaplan G. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Inter Med. 1998;158:1133–1138. doi: 10.1001/archinte.158.10.1133. [DOI] [PubMed] [Google Scholar]
- Ariyo AA, Haan M, Tangen CM, Rutledge JC, Cushman M, Dobs A, et al. Depressive symptoms and risks of coronary heart disease and mortality in elderly Americans. Circulation. 2000;102:1773–1779. doi: 10.1161/01.cir.102.15.1773. [DOI] [PubMed] [Google Scholar]
- Abramson J, Berger A, Krumholz HM, Vaccarino V. Depression and risk of heart failure among older persons with isolated systolic hypertension. Arch Intern Med. 2001;161:1725–1730. doi: 10.1001/archinte.161.14.1725. [DOI] [PubMed] [Google Scholar]
- Williams SA, Kasl SV, Heiat A, Abramson JL, Krumholz HM, Vaccarino V. Depression and risk of heart failure among the elderly: a prospective community-based study. Psychosom Med. 2002;64:6–12. doi: 10.1097/00006842-200201000-00002. [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, House JS, Mero RP. Depressive symptoms and mortality risk in a national sample: confounding effects of health status. Psychosom Med. 2004;66:823–830. doi: 10.1097/01.psy.0000145903.75432.1f. [DOI] [PubMed] [Google Scholar]
- Gump BB, Matthews KA, Eberly LE, Chang Y-f, for the MRG. Depressive symptoms and mortality in men: results from the multiple risk factor intervention trial. Stroke. 2005;36:98–102. doi: 10.1161/01.STR.0000149626.50127.d0. [DOI] [PubMed] [Google Scholar]
- Wulsin LR, Evans JC, Vasan RS, Murabito JM, Kelly-Hayes M, Benjamin EJ. Depressive symptoms, coronary heart disease, and overall mortality in the Framingham heart study. Psychosom Med. 2005;67:697–702. doi: 10.1097/01.psy.0000181274.56785.28. [DOI] [PubMed] [Google Scholar]
- Ahto M, Isoaho R, Puolijoki H, Vahlberg T, Kivela S-L. Stronger symptoms of depression predict high coronary heart disease mortality in older men and women. Int J Geriatr Psychiatry. 2006;22:757–763. doi: 10.1002/gps.1735. [DOI] [PubMed] [Google Scholar]
- Surtees PG, Wainwright NWJ, Luben RN, Wareham NJ, Bingham SA, Khaw K-T. Depression and ischemic heart disease mortality: evidence from the Epic-Norfolk United Kingdom prospective cohort study. Am J Psychiatry. 2008;165:515–523. doi: 10.1176/appi.ajp.2007.07061018. [DOI] [PubMed] [Google Scholar]
- Kendler K, Gardner C, Riske A, Gatz M. Major depression and coronary artery disease in the swedish twin registry. Arch Gen Psychiatry. 2009;66:857–863. doi: 10.1001/archgenpsychiatry.2009.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rugulies R. Depression as a predictor for coronary heart disease. a review and meta-analysis. Am J Prev Med. 2002;23:51–61. doi: 10.1016/s0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- Wulsin LR, Singal BM. Do depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative review. Psychosom Med. 2003;65:201–210. doi: 10.1097/01.psy.0000058371.50240.e3. [DOI] [PubMed] [Google Scholar]
- Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27:2763–2774. doi: 10.1093/eurheartj/ehl338. [DOI] [PubMed] [Google Scholar]
- Lauzon C, Beck CA, Huynh T, Dion D, Racine N, Carignan S, et al. Depression and prognosis following hospital admission because of acute myocardial infarction. CMAJ. 2003;168:547–552. [PMC free article] [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- Carney R, Rich M, Freedland K, Saini J, teVelde A, Simeone C, et al. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med. 1988;50:627–633. doi: 10.1097/00006842-198811000-00009. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Helms MJ, Mark DB, Blumenthal JA, Califf RM, Haney TL, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol. 1996;78:613–617. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- Lespérance F, Frasure-Smith N, Juneau M, Theroux P. Depression and 1-year prognosis in unstable angina. Arch Inter Med. 2000;160:1354–1360. doi: 10.1001/archinte.160.9.1354. [DOI] [PubMed] [Google Scholar]
- Rutledge T, Reis S, Olson M, Owens J, Kelsey S, Pepine C, et al. Depression symptom severity and reported treatment history in the prediction of cardiac risk in women with suspected myocardial ischemia. Arch Gen Psychiatry. 2006;63:874–880. doi: 10.1001/archpsyc.63.8.874. [DOI] [PubMed] [Google Scholar]
- Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–2388. doi: 10.1001/jama.2008.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66:802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med. 2004;66:814–822. doi: 10.1097/01.psy.0000146294.82810.9c. [DOI] [PubMed] [Google Scholar]
- Meijer A, Conradi HJ, Bos EH, Thombs BD, van Melle JP, de Jonge P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis of 25 years of research. Gen Hosp Psychiatry. 2011;33:203–216. doi: 10.1016/j.genhosppsych.2011.02.007. [DOI] [PubMed] [Google Scholar]
- Williams LS, Ghose SS, Swindle RW. Depression and other mental health diagnoses increase mortality risk after ischemic stroke. Am J Psychiatry. 2004;161:1090–1095. doi: 10.1176/appi.ajp.161.6.1090. [DOI] [PubMed] [Google Scholar]
- Skala JA, Freedland KE, Carney RM. Coronary heart disease and depression: a review of recent mechanistic research. Can J Psychiatry. 2006;51:738–745. doi: 10.1177/070674370605101203. [DOI] [PubMed] [Google Scholar]
- Stuart MJ, Baune BT. Depression and type 2 diabetes: inflammatory mechanisms of a psychoneuroendocrine co-morbidity. Neurosci Biobehav Rev. 2012;36:658–676. doi: 10.1016/j.neubiorev.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, et al. A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67:446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- Maes M. Depression is an inflammatory disease, but cell-mediated immune activation is the key component of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:664–675. doi: 10.1016/j.pnpbp.2010.06.014. [DOI] [PubMed] [Google Scholar]
- Paz-Filho G, Licinio J, Wong ML. Pathophysiological basis of cardiovascular disease and depression: a chicken-and-egg dilemma. Revista brasileira de psiquiatria. 2010;32:181–191. doi: 10.1590/s1516-44462010000200015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12:204–212. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- Petaja J. Inflammation and coagulation. An overview. Thromb Res. 2011;127 (Suppl 2:S34–S37. doi: 10.1016/S0049-3848(10)70153-5. [DOI] [PubMed] [Google Scholar]
- Sasayama D, Hori H, Iijima Y, Teraishi T, Hattori K, Ota M, et al. Modulation of cortisol responses to the DEX/CRH test by polymorphisms of the interleukin-1beta gene in healthy adults. Behav Brain Functions: BBF. 2011;7:23. doi: 10.1186/1744-9081-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malpas SC. Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev. 2010;90:513–557. doi: 10.1152/physrev.00007.2009. [DOI] [PubMed] [Google Scholar]
- Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010;67:1067–1074. doi: 10.1016/j.biopsych.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Shimokawa H. Primary endothelial dysfunction: atherosclerosis. J Mol Cell Cardiol. 1999;31:23–37. doi: 10.1006/jmcc.1998.0841. [DOI] [PubMed] [Google Scholar]
- Rybakowski J, Wykretowicz A, Heymann-Szlachcinska A, Wysocki H. Impairment of endothelial function in unipolar and bipolar depression. Biol Psychiatry. 2006;60:889–891. doi: 10.1016/j.biopsych.2006.03.025. [DOI] [PubMed] [Google Scholar]
- Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol. 2002;22:1065–1074. doi: 10.1161/01.atv.0000051384.43104.fc. [DOI] [PubMed] [Google Scholar]
- Cooper DC, Tomfohr LM, Milic MS, Natarajan L, Bardwell WA, Ziegler MG, et al. Depressed mood and flow-mediated dilation: a systematic review and meta-analysis. Psychosom Med. 2011;73:360–369. doi: 10.1097/PSY.0b013e31821db79a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajagopalan S, Brook R, Rubenfire M, Pitt E, Young E, Pitt B. Abnormal brachial artery flow-mediated vasodilation in young adults with major depression. Am J Cardiol. 2001;88:196–198. doi: 10.1016/s0002-9149(01)01623-x. [DOI] [PubMed] [Google Scholar]
- Sherwood A, Hinderliter AL, Watkins LL, Waugh RA, Blumenthal JA. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J Am Coll Cardiol. 2005;46:656–659. doi: 10.1016/j.jacc.2005.05.041. [DOI] [PubMed] [Google Scholar]
- Huang TL, Lee CT. T-helper 1/T-helper 2 cytokine imbalance and clinical phenotypes of acute-phase major depression. Psychiatry Clin Neurosci. 2007;61:415–420. doi: 10.1111/j.1440-1819.2007.01686.x. [DOI] [PubMed] [Google Scholar]
- Kaestner F, Hettich M, Peters M, Sibrowski W, Hetzel G, Ponath G, et al. Different activation patterns of proinflammatory cytokines in melancholic and non-melancholic major depression are associated with HPA axis hyperactivity. J Affect Dis. 2005;87:305–311. doi: 10.1016/j.jad.2005.03.012. [DOI] [PubMed] [Google Scholar]
- Maes M, Mihaylova I, Kubera M, Ringel K. Activation of cell-mediated immunity in depression: association with inflammation, melancholia, clinical staging and the fatigue and somatic symptom cluster of depression. Prog Neuropsychopharmacology Biol Psychiatry. 2012;36:169–175. doi: 10.1016/j.pnpbp.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Marques-Deak AH, Neto FL, Dominguez WV, Solis AC, Kurcgant D, Sato F, et al. Cytokine profiles in women with different subtypes of major depressive disorder. J Psychiatr Res. 2007;41:152–159. doi: 10.1016/j.jpsychires.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Rothermundt M, Arolt V, Peters M, Gutbrodt H, Fenker J, Kersting A, et al. Inflammatory markers in major depression and melancholia. J Affect Dis. 2001;63:93–102. doi: 10.1016/s0165-0327(00)00157-9. [DOI] [PubMed] [Google Scholar]
- Erdem M, Celik C, Cayci T, Ozdemir B, Kurt YG, Akgul EO, et al. Serum haptoglobin levels in patients with melancholic and nonmelancholic major depression. Prog Neuropsychopharmacology Biol Psychiatry. 2011;35:944–947. doi: 10.1016/j.pnpbp.2011.01.009. [DOI] [PubMed] [Google Scholar]
- Schlatter J, Ortuno F, Cervera-Enguix S. Lymphocyte subsets and lymphokine production in patients with melancholic versus nonmelancholic depression. Psychiatry Res. 2004;128:259–265. doi: 10.1016/j.psychres.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Nelson JC, Davis JM. DST studies in psychotic depression: a meta-analysis. Am J Psychiatry. 1997;154:1497–1503. doi: 10.1176/ajp.154.11.1497. [DOI] [PubMed] [Google Scholar]
- Maes M, Van der Planken M, Van Gastel A, Desnyder R. Blood coagulation and platelet aggregation in major depression. J Affect Dis. 1996;40:35–40. doi: 10.1016/0165-0327(96)00044-4. [DOI] [PubMed] [Google Scholar]
- Yoon HK, Kim YK, Lee HJ, Kwon DY, Kim L.Role of cytokines in atypical depression Nordic J Psychiatryadvance online publication, 22 September 2011 (e-pub ahead of print). [DOI] [PubMed]
- Anisman H, Ravindran A, Griffiths J, Merali Z. Endocrine and cytokine correlates of major depression and dysthymia with typical or atypical features. Mol Psychiatry. 1999;4:182–188. doi: 10.1038/sj.mp.4000436. [DOI] [PubMed] [Google Scholar]
- Gecici O, Kuloglu M, Atmaca M, Tezcan AE, Tunckol H, Emul HM, et al. High serum leptin levels in depressive disorders with atypical features. Psychiatry Clin Neurosci. 2005;59:736–738. doi: 10.1111/j.1440-1819.2005.01445.x. [DOI] [PubMed] [Google Scholar]
- Ravindran AV, Griffiths J, Merali Z, Anisman H. Circulating lymphocyte subsets in major depression and dysthymia with typical or atypical features. Psychosom Med. 1998;60:283–289. doi: 10.1097/00006842-199805000-00013. [DOI] [PubMed] [Google Scholar]
- Zaharia MD, Ravindran AV, Griffiths J, Merali Z, Anisman H. Lymphocyte proliferation among major depressive and dysthymic patients with typical or atypical features. J Affect Dis. 2000;58:1–10. doi: 10.1016/s0165-0327(99)00100-7. [DOI] [PubMed] [Google Scholar]
- Yoshimura R, Umene-Nakano W, Hoshuyama T, Ikenouchi-Sugita A, Hori H, Katsuki A, et al. Plasma levels of brain-derived neurotrophic factor and interleukin-6 in patients with dysthymic disorder: comparison with age- and sex-matched major depressed patients and healthy controls. Hum Psychopharmacol. 2010;25:566–569. doi: 10.1002/hup.1155. [DOI] [PubMed] [Google Scholar]
- Kim JM, Stewart R, Kim SW, Shin IS, Kim JT, Park MS, et al. Associations of cytokine gene polymorphisms with post-stroke depression World J Biol Psychiatryadvance online publication, 27 July 2011 (e-pub ahead of print). [DOI] [PubMed]
- Thomas AJ, Morris C, Davis S, Jackson E, Harrison R, O'Brien JT. Soluble cell adhesion molecules in late-life depression. Int Psychogeriatr. 2007;19:914–920. doi: 10.1017/S1041610206004728. [DOI] [PubMed] [Google Scholar]
- Thomas AJ, Davis S, Morris C, Jackson E, Harrison R, O'Brien JT. Increase in interleukin-1beta in late-life depression. Am J Psychiatry. 2005;162:175–177. doi: 10.1176/appi.ajp.162.1.175. [DOI] [PubMed] [Google Scholar]
- Pivac N, Jakovljevic M, Muck-Seler D, Brzovic Z. Hypothalamic-pituitary-adrenal axis function and platelet serotonin concentrations in depressed patients. Psychiatry Res. 1997;73:123–132. doi: 10.1016/s0165-1781(97)00120-0. [DOI] [PubMed] [Google Scholar]
- Contreras F, Menchon JM, Urretavizcaya M, Navarro MA, Vallejo J, Parker G. Hormonal differences between psychotic and non-psychotic melancholic depression. J Affect Dis. 2007;100:65–73. doi: 10.1016/j.jad.2006.09.021. [DOI] [PubMed] [Google Scholar]
- Gomez RG, Fleming SH, Keller J, Flores B, Kenna H, DeBattista C, et al. The neuropsychological profile of psychotic major depression and its relation to cortisol. Biol Psychiatry. 2006;60:472–478. doi: 10.1016/j.biopsych.2005.11.010. [DOI] [PubMed] [Google Scholar]
- Keller J, Flores B, Gomez RG, Solvason HB, Kenna H, Williams GH, et al. Cortisol circadian rhythm alterations in psychotic major depression. Biol Psychiatry. 2006;60:275–281. doi: 10.1016/j.biopsych.2005.10.014. [DOI] [PubMed] [Google Scholar]
- Belanoff JK, Kalehzan M, Sund B, Fleming Ficek SK, Schatzberg AF. Cortisol activity and cognitive changes in psychotic major depression. Am J Psychiatry. 2001;158:1612–1616. doi: 10.1176/appi.ajp.158.10.1612. [DOI] [PubMed] [Google Scholar]
- Posener JA, DeBattista C, Williams GH, Chmura Kraemer H, Kalehzan BM, Schatzberg AF. 24-Hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Arch Gen Psychiatry. 2000;57:755–760. doi: 10.1001/archpsyc.57.8.755. [DOI] [PubMed] [Google Scholar]
- Cubells JF, Price LH, Meyers BS, Anderson GM, Zabetian CP, Alexopoulos GS, et al. Genotype-controlled analysis of plasma dopamine beta-hydroxylase activity in psychotic unipolar major depression. Biol Psychiatry. 2002;51:358–364. doi: 10.1016/s0006-3223(01)01349-x. [DOI] [PubMed] [Google Scholar]
- Su KP, Leu SJ, Yang YY, Shen WW, Chou YM, Tsai SY. Reduced production of interferon-gamma but not interleukin-10 in bipolar mania and subsequent remission. J Affect Disord. 2002;71:205–209. doi: 10.1016/s0165-0327(01)00369-x. [DOI] [PubMed] [Google Scholar]
- Liu HC, Yang YY, Chou YM, Chen KP, Shen WW, Leu SJ. Immunologic variables in acute mania of bipolar disorder. J Neuroimmunol. 2004;150:116–122. doi: 10.1016/j.jneuroim.2004.01.006. [DOI] [PubMed] [Google Scholar]
- Kim YK, Jung HG, Myint AM, Kim H, Park SH. Imbalance between pro-inflammatory and anti-inflammatory cytokines in bipolar disorder. J Affect Disord. 2007;104:91–95. doi: 10.1016/j.jad.2007.02.018. [DOI] [PubMed] [Google Scholar]
- O'Brien SM, Scully P, Scott LV, Dinan TG. Cytokine profiles in bipolar affective disorder: focus on acutely ill patients. J Affect Disord. 2006;90:263–267. doi: 10.1016/j.jad.2005.11.015. [DOI] [PubMed] [Google Scholar]
- Kapczinski F, Dal-Pizzol F, Teixeira AL, Magalhaes PV, Kauer-Sant'Anna M, Klamt F, et al. Peripheral biomarkers and illness activity in bipolar disorder. J Psychiatr Res. 2011;45:156–161. doi: 10.1016/j.jpsychires.2010.05.015. [DOI] [PubMed] [Google Scholar]
- Barbosa IG, Huguet RB, Mendonca VA, Sousa LP, Neves FS, Bauer ME, et al. Increased plasma levels of soluble TNF receptor I in patients with bipolar disorder. Eur Arch Psychiatry Clin Neurosci. 2011;261:139–143. doi: 10.1007/s00406-010-0116-z. [DOI] [PubMed] [Google Scholar]
- Hope S, Melle I, Aukrust P, Steen NE, Birkenaes AB, Lorentzen S, et al. Similar immune profile in bipolar disorder and schizophrenia: selective increase in soluble tumor necrosis factor receptor I and von Willebrand factor. Bipolar Disord. 2009;11:726–734. doi: 10.1111/j.1399-5618.2009.00757.x. [DOI] [PubMed] [Google Scholar]
- Brietzke E, Stertz L, Fernandes BS, Kauer-Sant'anna M, Mascarenhas M, Escosteguy Vargas A, et al. Comparison of cytokine levels in depressed, manic and euthymic patients with bipolar disorder. J Affect Disord. 2009;116:214–217. doi: 10.1016/j.jad.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Knijff EM, Breunis MN, Kupka RW, de Wit HJ, Ruwhof C, Akkerhuis GW, et al. An imbalance in the production of IL-1beta and IL-6 by monocytes of bipolar patients: restoration by lithium treatment. Bipolar Disord. 2007;9:743–753. doi: 10.1111/j.1399-5618.2007.00444.x. [DOI] [PubMed] [Google Scholar]
- Huang TL, Lin FC. High-sensitivity C-reactive protein levels in patients with major depressive disorder and bipolar mania. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:370–372. doi: 10.1016/j.pnpbp.2006.09.010. [DOI] [PubMed] [Google Scholar]
- Kauer-Sant'Anna M, Kapczinski F, Andreazza AC, Bond DJ, Lam RW, Young LT, et al. Brain-derived neurotrophic factor and inflammatory markers in patients with early- vs. late-stage bipolar disorder. Int J Neuropsychopharmacol. 2009;12:447–458. doi: 10.1017/S1461145708009310. [DOI] [PubMed] [Google Scholar]
- Rapaport MH, Guylai L, Whybrow P. Immune parameters in rapid cycling bipolar patients before and after lithium treatment. J Psychiatr Res. 1999;33:335–340. doi: 10.1016/s0022-3956(99)00007-2. [DOI] [PubMed] [Google Scholar]
- Tsai SY, Chen KP, Yang YY, Chen CC, Lee JC, Singh VK, et al. Activation of indices of cell-mediated immunity in bipolar mania. Biol Psychiatry. 1999;45:989–994. doi: 10.1016/s0006-3223(98)00159-0. [DOI] [PubMed] [Google Scholar]
- Rapaport MH. Immune parameters in euthymic bipolar patients and normal volunteers. J Affect Disord. 1994;32:149–156. doi: 10.1016/0165-0327(94)90012-4. [DOI] [PubMed] [Google Scholar]
- Hung YJ, Hsieh CH, Chen YJ, Pei D, Kuo SW, Shen DC, et al. Insulin sensitivity, proinflammatory markers and adiponectin in young males with different subtypes of depressive disorder. Clin Endocrinol (Oxf) 2007;67:784–789. doi: 10.1111/j.1365-2265.2007.02963.x. [DOI] [PubMed] [Google Scholar]
- Drexhage RC, Hoogenboezem TH, Versnel MA, Berghout A, Nolen WA, Drexhage HA. The activation of monocyte and T cell networks in patients with bipolar disorder. Brain Behav Immun. 2011;25:1206–1213. doi: 10.1016/j.bbi.2011.03.013. [DOI] [PubMed] [Google Scholar]
- Kunz M, Cereser KM, Goi PD, Fries GR, Teixeira AL, Fernandes BS, et al. Serum levels of IL-6, IL-10 and TNF-alpha in patients with bipolar disorder and schizophrenia: differences in pro- and anti-inflammatory balance. Rev Bras Psiquiatr. 2011;33:268–274. doi: 10.1590/s1516-44462011000300010. [DOI] [PubMed] [Google Scholar]
- Guloksuz S, Cetin EA, Cetin T, Deniz G, Oral ET, Nutt DJ. Cytokine levels in euthymic bipolar patients. J Affect Disord. 2010;126:458–462. doi: 10.1016/j.jad.2010.04.027. [DOI] [PubMed] [Google Scholar]
- Dickerson F, Stallings C, Origoni A, Boronow J, Yolken R. Elevated serum levels of C-reactive protein are associated with mania symptoms in outpatients with bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:952–955. doi: 10.1016/j.pnpbp.2007.02.018. [DOI] [PubMed] [Google Scholar]
- Kim YK, Suh IB, Kim H, Han CS, Lim CS, Choi SH, et al. The plasma levels of interleukin-12 in schizophrenia, major depression, and bipolar mania: effects of psychotropic drugs. Mol Psychiatry. 2002;7:1107–1114. doi: 10.1038/sj.mp.4001084. [DOI] [PubMed] [Google Scholar]
- Lewitus GM, Wilf-Yarkoni A, Ziv Y, Shabat-Simon M, Gersner R, Zangen A, et al. Vaccination as a novel approach for treating depressive behavior. Biol Psychiatry. 2009;65:283–288. doi: 10.1016/j.biopsych.2008.07.014. [DOI] [PubMed] [Google Scholar]
- Schwartz M, Shechter R. Protective autoimmunity functions by intracranial immunosurveillance to support the mind: the missing link between health and disease. Mol Psychiatry. 2010;15:342–354. doi: 10.1038/mp.2010.31. [DOI] [PubMed] [Google Scholar]
- Boufidou F, Nikolaou C, Alevizos B, Liappas IA, Christodoulou GN. Cytokine production in bipolar affective disorder patients under lithium treatment. J Affect Disord. 2004;82:309–313. doi: 10.1016/j.jad.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Schmider J, Lammers CH, Gotthardt U, Dettling M, Holsboer F, Heuser IJ. Combined dexamethasone/corticotropin-releasing hormone test in acute and remitted manic patients, in acute depression, and in normal controls: I. Biol Psychiatry. 1995;38:797–802. doi: 10.1016/0006-3223(95)00064-X. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Ritchie JC, Carroll BJ. Plasma dexamethasone concentration and cortisol response during manic episodes. Biol Psychiatry. 1998;43:747–754. doi: 10.1016/s0006-3223(97)00274-6. [DOI] [PubMed] [Google Scholar]
- Rybakowski JK, Twardowska K. The dexamethasone/corticotropin-releasing hormone test in depression in bipolar and unipolar affective illness. J Psychiatr Res. 1999;33:363–370. doi: 10.1016/s0022-3956(99)00014-x. [DOI] [PubMed] [Google Scholar]
- Jabben N, Nolen WA, Smit JH, Vreeburg SA, Beekman AT, Penninx BW. Co-occurring manic symptomatology influences HPA axis alterations in depression. J Psychiatr Res. 2011;45:1208–1213. doi: 10.1016/j.jpsychires.2011.03.010. [DOI] [PubMed] [Google Scholar]
- Watson S, Gallagher P, Ferrier IN, Young AH. Post-dexamethasone arginine vasopressin levels in patients with severe mood disorders. J Psychiatr Res. 2006;40:353–359. doi: 10.1016/j.jpsychires.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Watson S, Gallagher P, Ritchie JC, Ferrier IN, Young AH. Hypothalamic-pituitary-adrenal axis function in patients with bipolar disorder. Br J Psychiatry. 2004;184:496–502. doi: 10.1192/bjp.184.6.496. [DOI] [PubMed] [Google Scholar]
- Deshauer D, Duffy A, Meaney M, Sharma S, Grof P. Salivary cortisol secretion in remitted bipolar patients and offspring of bipolar parents. Bipolar Disord. 2006;8:345–349. doi: 10.1111/j.1399-5618.2006.00338.x. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. ‘Vascular depression' hypothesis. Arch Gen Psychiatry. 1997;54:915–922. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- O'Brien J, Desmond P, Ames D, Schweitzer I, Harrigan S, Tress B. A magnetic resonance imaging study of white matter lesions in depression and alzheimer's disease. Br J Psychiatry. 1996;168:477–485. doi: 10.1192/bjp.168.4.477. [DOI] [PubMed] [Google Scholar]
- Baldwin R, O'Brien J. Vascular basis of late-onset depressive disorder. Br J Psychiatry. 2002;180:157–160. doi: 10.1192/bjp.180.2.157. [DOI] [PubMed] [Google Scholar]
- Krishnan RRR, Hays JC, Blazer DG. MRI-defined vascular depression. Am J Psychiatry. 1997;154:497–501. doi: 10.1176/ajp.154.4.497. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Helms MJ, Krishnan KRR, Burke GL. Cerebrovascular disease and depression symptoms in the cardiovascular health study. Stroke. 1999;30:2159–2166. doi: 10.1161/01.str.30.10.2159. [DOI] [PubMed] [Google Scholar]
- Ramasubbu R. Relationship between depression and cerebrovascular disease: conceptual issues. J Affect Dis. 2000;57:1–11. doi: 10.1016/s0165-0327(99)00101-9. [DOI] [PubMed] [Google Scholar]
- Hickie I, Scott E. Late-onset depressive disorders: a preventablle variant of cerebrovascular disease. Psychol Med. 1998;28:1007–1013. doi: 10.1017/s0033291797006090. [DOI] [PubMed] [Google Scholar]
- Liao D. Arterial stiffness and the development of hypertension. Ann Med. 2000;32:383–385. doi: 10.3109/07853890008995943. [DOI] [PubMed] [Google Scholar]
- Cockcoroft JR, Wilkinson IB, Webb DJ. Age, arterial stiffness and the endothelium. Age Ageing. 1997;26 (suppl 4:53–60. doi: 10.1093/ageing/26.suppl_4.53. [DOI] [PubMed] [Google Scholar]
- Tiemeir H, Breteler M, Popele NMv, Hofman A, Witteman J. Late life depression is associated with arterial stiffness: a population-based study. J Am Geriatr Soc. 2003;51:1105–1110. doi: 10.1046/j.1532-5415.2003.51359.x. [DOI] [PubMed] [Google Scholar]
- Laurent S, Boutouyroe P, Asmar R, Gautier I, Laloux B, Guize L, et al. Aortic stiffness is an independent predicator of all - cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;15:426–444. doi: 10.1161/01.hyp.37.5.1236. [DOI] [PubMed] [Google Scholar]
- Meaume S, Benetos A, Henry OF, Rudnichi A, Safar ME. Aortic pulse wave velocity predicts cardiovascular mortality in subjects >70 years of age. Arterioscler Thromb Vasc Biol. 2001;21:2046–2050. doi: 10.1161/hq1201.100226. [DOI] [PubMed] [Google Scholar]
- Naidu M, Reddy B, Yashmaina S, Patnaik A, Rani P. Validity and reproducibility of arterial pulse wave velocity measurement using new device with oscillometric technique: a pilot study. Biomed Eng Online. 2005;4:49. doi: 10.1186/1475-925X-4-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons PCG, Algra A, Bots ML, Grobbee DE, van der Graaf Y. Common carotid intima-media thickness and arterial stiffness: indicators of cardiovascular risk in high-risk patients. The SMART Study (second manifestations of ARTerial disease) Circulation. 1999;100:951–957. doi: 10.1161/01.cir.100.9.951. [DOI] [PubMed] [Google Scholar]
- Blacher J, Asmar R, Djane S, London GM, Safar ME. Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999;33:1111–1117. doi: 10.1161/01.hyp.33.5.1111. [DOI] [PubMed] [Google Scholar]
- Oulis P, Kouzoupis A, Kyrkou K, Masdrakis VG, Georgiopoulos G, Karapoulios E, et al. Reversal of increased arterial stiffness in severely depressed women after 6-week antidepressant treatment. J Affect Dis. 2010;122:164–166. doi: 10.1016/j.jad.2009.08.003. [DOI] [PubMed] [Google Scholar]
- Anisman H, Ravindran A, Griffiths J, Merali Z. Interleukin-1β production in dysthymia before and after pharmacotherapy. Biol Psychiatry. 1999;46:1649–1655. doi: 10.1016/s0006-3223(99)00211-5. [DOI] [PubMed] [Google Scholar]
- Owen BM, Eccleston D, Ferrier IN, Young H. Raised levels of plasma interleukin-1β in major and postviral depression. Acta Psychiatrica Scandinavica. 2001;103:226–228. doi: 10.1034/j.1600-0447.2001.00162.x. [DOI] [PubMed] [Google Scholar]
- Dickens C, McGowan L, Percival C, Tomenson B, Cotter L, Heagerty A, et al. Depression is a risk factor for mortality after myocardial infarction: fact or artifact. J Am Coll Cardiol. 2007;49:1834–1840. doi: 10.1016/j.jacc.2007.01.075. [DOI] [PubMed] [Google Scholar]
- Rees K, Bennett P, West R, Smith GD, Ebrahim S. Psychological interventions for coronary heart disease (Review) Cochrane Database of Systematic Rev. 2004. pp. 1–63. [DOI] [PMC free article] [PubMed]
- Lesch KP, Laux G, Schulte HM, Pfüller H, Beckmann H. Corticotropin and cortisol response to human CRH as a probe for HPA system integrity in major depressive disorder. Psychiatry Res. 1988;24:25–34. doi: 10.1016/0165-1781(88)90136-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.