Abstract
Background:
Organophosphorus (OP) poisoning is a major health problem all over the world, particularly in the developing countries.
Aim:
The present study aims to explore the clinical and epidemiological features found in patients presenting with OP poisoning.
Materials and Methods:
A 1-year cross-sectional study was conducted on patients presenting with clinical features of OP poisoning in a tertiary care medical college.
Results:
A total of 968 patients presented during the study period. Poisoning with suicidal intent (82.02%) was more common than the accidental one (17.98%). Majority of the patients were housewives (42%) followed by farmers, shopkeepers, laborers, students. Methyl parathion was the most common poison consumed by the patients (35.74%) followed by diazinon, chlorpyriphos, dimicron. Nausea and vomiting (85.02%) was the most common symptom while miosis was the most common sign observed in 91.94% patients. A total of 56 patients of OP poisoning died (5.78%) with respiratory failure being the primary cause of death followed by CNS depression, cardiac arrest, and septicaemia.
Conclusion:
The present study showed that majority of the patients were of young age with females outnumbering males. Poisoning with suicidal intent was more common than accidental. Nausea and vomiting was the most common symptom reported by the patients while miosis was the most common sign observed by the treating physicians of the research team.
Keywords: Clinico-epidemiological characteristics, organophosphorus poisoning, study
Introduction
Poisoning with organophosphorus compounds (OP) is a global problem. World Health Organization estimates that one million serious unintentional poisonings occur every year and an additional two million people are hospitalized for suicide attempts with pesticides.[1] India is a predominantly agrarian country where pesticides are routinely used for farming. According to data available from National Poison Information Centre India, suicidal poisoning with house-hold agents (OPs, carbamates, pyrethrinoids, etc.) is the most common modality of poisoning.[2] Recent data from National crime bureau of India shows suicide by consumption of pesticides account for 19.4% and 19.7% of all cases of suicidal poisoning in the year 2006 and 2007 respectively.[3]
OP compounds inhibit acetylcholinesterase resulting in accumulation of acetylcholine (Ach) and overstimulation of cholinergic synapses. Patients die mostly from respiratory failure and lung injury, although there is variability in the clinical symptoms and signs depending on nature of compounds, amount consumed, severity, time gap between exposure, and presentation in the hospital.[4] Common clinical features of OP poisoning include the following:
Muscarinic manifestations[5]
Respiratory: Increased bronchial secretions, bronchospasm, chest tightness, dyspnoea, cough
Eyes: Blurred vision, conjunctival injection, dimness of vision, miosis
Gastrointestinal: Cramping, diarrhea, nausea, vomiting
Urinary: Incontinence
Cardiovascular: Bradycardia, hypotension
Exocrine glands: Hyperamylesia, increased salivation
Nicotinic manifestations[5]
Muscle fasciculation, cramping, weakness, diaphragmatic paralysis, respiratory failure, tachycardia, hypertension.
Thus we can appreciate that a patient with OP poisoning presents with a variety of signs and symptoms. In India, unconscious patients are often brought by their relatives and neighbors who are unable to provide correct information regarding the nature of the particular poison to which the patient was exposed. In such cases the diagnosis of OP poisoning is based on clinical features as observed by the treating physicians. The clinical features also help to determine the severity of poisoning which is of prognostic importance.
A literature search was conducted which consisted of a Medical Literature Analysis and Retrieval System Online (MEDLINE) database search (accessed on 16.4.2009) and a World Wide Web search (Search engine: Google, accessed on 16.4.2009) using the following keywords: “Organophosphorus poisoning, clinico-epimiological features, study”. The search revealed that only a few studies have considered the clinical and epidemiological features of OP poisoning.[6–11] Our study was conducted in this backdrop to explore the clinical features and epidemiological characteristics of patients presenting with OP poisoning.
Materials and Methods
Study setting
The study was conducted in a tertiary care medical college and hospital in West Bengal, India.
Ethics
The study was approved by institutional ethics committee.
Study design
A cross-sectional, study was conducted to address the study objective. All consecutive patients presenting in the emergency department of the hospital with history and clinical evidence of OP poisoning during the study period were considered eligible for participation in the study.
Study procedure
Patients attending the emergency department with history of exposure to OP compounds were initially evaluated and resuscitated for maintaining airway, breathing, and circulation. Informed consent was obtained from eligible patients/legally authorized representatives (if the patient was unconscious). After completing the medicolegal formalities careful history was taken from the patients/legally authorized representatives (in case the patient was unconscious) following which clinical examination was carried out to determine the common clinical features of OP poisoning.
Statistical analysis
Data collected were analyzed in computer by using the Statistical Package for Social Sciences (SPSS) program version 10. Data analysis was done by using descriptive and inferential statistical methods: frequency, percentage, means, standard deviation (S.D.). A two-tailed P-value less than 0.05 was considered to be statistically significant.
Results
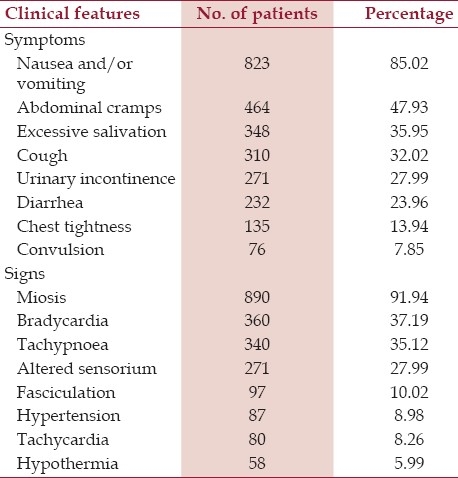
A total of 968 patients presented in the emergency department of the institute during the study period with the clinical features of OP poisoning. The demographic characteristics of the patients are shown in Table 1. Mean age of the persons presenting in the emergency with clinical features of OP poisoning is 34.47 years (Mean±S.D.: 34.47±9.21). The females outnumbered males with male: female ratio of 1:1.38. Poisoning with suicidal intent was more common (82.02%) than the accidental one (17.98%) (P-value < 0.0001). Majority of the patients were housewives (42%) followed by farmers (33.99%), shopkeepers (9.93%), laborers (8.14%), students (6.2%). The mean interval between poison consumption and admission to hospital was 4.4 hours (Mean±S.D.: 4.4±2.29). Regarding the type of poison consumed by the patient, methyl parathion was the most common poison consumed by the patients (35.74%) followed by diazinon (28.62%), chlorpyriphos (19.52%), dimicron (16.12%). The signs and symptoms with which the patients presented are enumerated in Table 2. In the present study, nausea and vomiting is the most common symptom reported by 85.02% of patients followed by abdominal cramps (47.93%), while miosis is the most common sign observed in 91.94% patients. Following admission, a total of 56 (5.78%) patients died during their hospital stay. Respiratory failure was the primary cause of death in 21 patients (37.5%) followed by CNS depression (33.92%), cardiac arrest (21.44%), and septicemia (7.14%).
Table 1.
Baseline demographic parameter of the patients of OP poisoning (n=968)
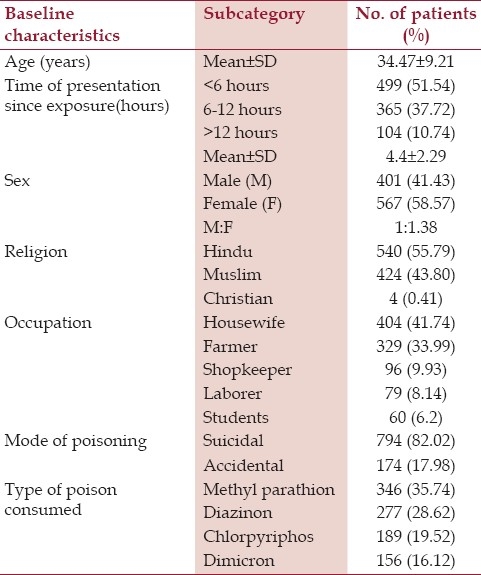
Table 2.
Clinical features of patients suffering from OP poisoning at presentation
Discussion
In the present study, majority of the patients belonged to the young age group (Mean±S.D.: 34.47±9.21). Females show a clear preponderance over male with a male (M): female (F) ratio of 1:1.38. This finding is in agreement with studies conducted in Turkey (M: F=1:1.47),[6] Nepal (M: F=1:2).[7] However, in the study conducted in Chennai by Shivaprasad et al., (2001),[8] male patients (74%) outnumbered female (26%). Majority of the affected patients in our study are housewives (42%) which is at par with the study conducted in Turkey (housewives 47.3% of total sample).[6]
In the present study, poisoning with suicidal intent was more common (82.02%) than the accidental one (P-value< 0.0001). This is in congruence with studies conducted in Nepal,[7] Turkey,[6] Gulbarga[9] where poisoning with suicidal intent accounts for 95.24%, 75.9%, and 97.25% of total cases of OP poisoning respectively. The mean interval between poison consumption and admission to the hospital was 4.4 hours (Mean±S.D.: 4.4± 2.29). In studies conducted at Chennai,[8] maximum patients (89.69%) presented within 6 hours. Regarding the type of poison consumed by the patient, methyl parathion was the most common poison (35.74%) followed by diazinon, chlorpyriphos, dimicron., carbamates. In a study conducted in Nepal,[7] methyl parathion (64.62%) was the most common one followed by Baygon spray, malathion, dichlorvos. Methyl parathion was also the most common poison in studies conducted in Chennai.[8] However, in a study conducted in Turkey,[6] dichlorvos was the most common one. This variation in the type of poison consumed can be attributed to the regional availability of pesticides in different countries.
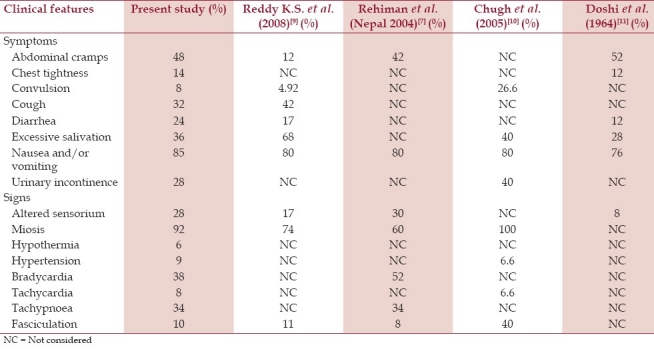
Clinical presentation depends on the specific OP involved, the quantity absorbed, and the type of exposure. In our study nausea and vomiting was the most common symptom (85.02%) while miosis (91.94%) was the most common sign. A comparison between the clinical features as observed in our study with earlier studies has been listed in Table 3. The mortality rate in our study was 5.78% which is comparable to the study done in Turkey (9.1%).[6]
Table 3.
Comparison of the clinical features observed in the present study with the studies held before
Conclusion
The present study showed that majority of the patients were of young age with females outnumbering males. Poisoning with suicidal intent was more common than accidental. Nausea and vomiting was the most common symptom reported by the patients while miosis was the most common sign observed by the treating physicians of the research team.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: Systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srivastava A, Peshin SS. An epidemiological study of poisoning cases reported to the National Poisons Information centre, All India Institute of Medical Sciences, New Delhi. Hum Exp Toxicol. 2005;24:279–85. doi: 10.1191/0960327105ht527oa. [DOI] [PubMed] [Google Scholar]
- 3.Accidental deaths and suicides in India, National Crime Records Bureau, Ministry of Home affairs, Government of India. [Accessed April 6, 2010]. at: http://ncrb.nic.in/adsi2008/suicides-08.pdf .
- 4.Eddleston M. The pathophysiology of organophosphorus pesticide self-poisoning is not so simple. Neth J Med. 2008;66:146–8. [PubMed] [Google Scholar]
- 5.Paudyal BP. Organophosphorus poisoning. J Nepal Med Assoc. 2008;47:251–8. [PubMed] [Google Scholar]
- 6.Yurumez Y, Durukan P, Yavuz Y, Ikizceli I, Avsarogullari L, Ozkan S, et al. Acute organophosphate poisoning in university hospital emergency room patients. Intern Med. 2007;46:965–9. doi: 10.2169/internalmedicine.46.6304. [DOI] [PubMed] [Google Scholar]
- 7.Rehiman S, Lohani SP, Bhattarai MC. Correlation of serum cholinesterase level, clinical score at presentation and severity of organophosphorous poisoning. J Nepal Med Assoc. 2008;47:47–52. [PubMed] [Google Scholar]
- 8.Shivakumar S, Rajan SK, Madhu CR, Doss P, Pasupathy S, Dhandapani E, et al. Profile of acute poisoning in Chennai: A two year experience in Stanley Medical College and Hospital (1999-2000) J Assoc Physicians India. 2002;50:206. [Google Scholar]
- 9.Gannur DG, Maka P, Reddy N. Organophosphorus compound poisoning in Gulbargaregion - A five year study. Indian J Forensic Med Toxicol. 2008. [Accessed December 15, 2011]. at: http://www.indmedica.com/journals. php?journalid = 11andissueid = 120andarticleid = 1596andaction=article .
- 10.Chugh SN, Aggarwal N, Dabla S, Chhabra B. Comparative evaluation of atropine alone and atropine with pralidoxime (PAM) in the management of organophosphorus poisoning. J Indian Acad Clin Med. 2005;6:33–7. [Google Scholar]
- 11.Doshi JC, Katakia MK, Baxamusa HM. Organophosphorus poisoning.A review with a study of 25 cases. J Postgrad Med. 1964;11:62–78. [PubMed] [Google Scholar]


