Abstract
Recent isolation of a novel swine-origin influenza A H3N2 variant virus [A(H3N2)v] from humans in the United States has raised concern over the pandemic potential of these viruses. Here, we analyzed the virulence, transmissibility, and receptor-binding preference of four A(H3N2)v influenza viruses isolated from humans in 2009, 2010, and 2011. High titers of infectious virus were detected in nasal turbinates and nasal wash samples of A(H3N2)v-inoculated ferrets. All four A(H3N2)v viruses possessed the capacity to spread efficiently between cohoused ferrets, and the 2010 and 2011 A(H3N2)v isolates transmitted efficiently to naïve ferrets by respiratory droplets. A dose-dependent glycan array analysis of A(H3N2)v showed a predominant binding to α2-6–sialylated glycans, similar to human-adapted influenza A viruses. We further tested the viral replication efficiency of A(H3N2)v viruses in a relevant cell line, Calu-3, derived from human bronchial epithelium. The A(H3N2)v viruses replicated in Calu-3 cells to significantly higher titers compared with five common seasonal H3N2 influenza viruses. These findings suggest that A(H3N2)v viruses have the capacity for efficient replication and transmission in mammals and underscore the need for continued public health surveillance.
Seasonal epidemics and periodic pandemics are an ever-present international public health burden. During seasonal epidemics, the risk for hospitalization and death are highest among persons at either end of the age spectrum as well as for individuals with underlying medical conditions (1, 2). Although the overall impact of the 2009 influenza pandemic, caused by an H1N1 virus [A(H1N1)pdm09] was more modest than those of prior pandemics, the disproportionate disease burden among children and younger adults distinguished this pandemic from seasonal influenza (3–5). The A(H1N1)pdm09 virus emerged from swine, with a unique constellation of genes from human, avian, and swine influenza viruses not previously observed in nature. Swine represent a unique host because of their ability to be infected by influenza viruses from multiple species and serve as a reservoir for specific subtypes of influenza capable of infecting humans (6–8). Triple-reassortant swine (TRS) H1N1 viruses, which share host gene-lineage origins with A(H1N1)pdm09 viruses, have been responsible for sporadic human cases since 2005 (9, 10). The emergence of the A(H1N1)pdm09 virus, to which the majority of children and younger adults had little preexisting immunity, highlights the public health threat posed by other swine-origin influenza virus subtypes.
H3N2 viruses have circulated in humans since their pandemic emergence in 1968 and are generally associated with uncomplicated disease in young healthy adults. However, epidemics caused by H3N2 viruses have been more severe than those caused by seasonal H1N1 or influenza B viruses (11, 12). In 1997–1998, human H3N2 viruses infected swine and spread widely in North American swine (6–8). In particular, TRS H3N2 viruses with a human lineage polymerase subunit polymerase basic 1 (PB1) gene, avian lineage PB2 and polymerase acidic (PA) genes, and swine lineage nucleoprotein (NP), matrix (M), and nonstructural (NS) genes, referred to as the triple-reassortant internal gene (TRIG) constellation, have been isolated widely in pigs throughout the United States (6–8, 13). From the late 1990s to 2009, these novel variants of H3N2 viruses [A(H3N2)v] were limited to transmission among swine, with only occasional detections of transmission to humans (14). However, between September and November 2010, five cases of human infection with the novel swine-origin A(H3N2)v were reported (15). Although all five recovered fully from their illness, two of the five cases were hospitalized. In 2011, 12 additional human cases were documented in the United States, with limited human-to-human transmission in some cases (15–17). The 2011 A(H3N2)v viruses are similar to other A(H3N2)v viruses isolated from previous human infections over the past 2 y but are unique in that the M gene is derived from the A(H1N1)pdm09 virus. Antigenic characterization showed that the A(H3N2)v viruses are distinct from current seasonal H3N2 viruses but exhibit a low degree of serologic cross-reactivity with human H3N2 viruses that circulated in the early 1990s (6, 8, 13), suggesting that children born after this time period may be particularly susceptible to infection.
The use of the ferret model has become indispensable for understanding the virulence and transmission of influenza viruses (18–20), partly because ferrets and humans share similar lung physiology as well as because human and avian influenza viruses exhibit similar patterns of binding to sialic acids, the receptor for influenza viruses distributed throughout the respiratory tract in both species (21, 22). In this study, we used glycan microarrays to determine the receptor-binding preference of the A(H3N2)v viruses isolated from humans. The culture model of bronchial epithelial Calu-3 cells was used to assess viral replication, and the ferret model was used to assess pathogenicity and transmissibility. Notably, the 2010 and 2011 swine-origin H3N2 viruses replicated even more efficiently than human seasonal influenza viruses in human airway Calu-3 cells and exhibited efficient respiratory-droplet (RD) transmission in ferrets. These findings suggest that swine-origin H3N2 viruses have the potential to cause additional human disease.
Results
Pathogenesis of A(H3N2)v Influenza Viruses in Ferrets.
We characterized four A(H3N2)v viruses isolated in 2009, 2010, and 2011 from patients with uncomplicated upper respiratory tract illness. A/Kansas/13/2009 (KS/09) was isolated from a 12-y-old male who presented with fever, cough, and sore throat after contact with healthy-appearing swine while attending a county fair (14). A/Minnesota/11/10 (MN/10) virus was isolated from a 37-y-old male who reported exposure to pigs, whereas A/Pennsylvania/14/10 (PA/10) virus was isolated from a 45-y-old male with no known swine exposure (15). A/Indiana/08/11 (IN/11) virus was isolated from a male child <5 y old who may have been indirectly exposed through his caregiver (16). We first compared the pathogenesis of the A(H3N2)v viruses in ferrets inoculated with 106 pfu of virus. For each virus group, three ferrets were observed for clinical signs of illness and also served as inoculated animals for transmission studies. Ferrets inoculated with each of the A(H3N2)v viruses exhibited moderate weight loss, with the mean maximum loss ranging from 8.3% to 10.8% and a maximum mean body temperature increase of ∼1.4 °C (Table 1). All four viruses replicated efficiently in the upper respiratory tract; high viral titers (≥5.2 log10 pfu/mL) were measured in nasal wash samples. Mild lethargy was observed among all inoculated ferrets only during peak times of viral shedding [1–5 d postinoculation (dpi)], and all animals recovered fully from the infection.
Table 1.
Clinical symptoms of ferrets infected with A(H3N2)v influenza viruses
| Virus exposure | No. with weight loss (mean maximum weight loss, %) | No. with fever (mean maximum temperature increase, °C) | Lymphopenia at 3 dpi,* % | No. with virus detection (peak titer, log10 pfu/mL) | No. with seroconversion (HI geometric mean titer) |
| IN/11 | |||||
| Inoculated | 3/3 (10.8) | 3/3 (1.3) | 16.6 | 3/3 (7.1) | 3/3 (1280) |
| DC contact | 3/3 (2.8) | 3/3 (1.2) | ND | 3/3 (5.3) | 3/3 (1280) |
| RD contact | 3/3 (2.9) | 3/3 (1.2) | ND | 3/3 (5.2) | 3/3 (1280) |
| MN/10 | |||||
| Inoculated | 3/3 (8.3) | 3/3 (1.1) | 23.8 | 3/3 (5.9) | 3/3 (403) |
| DC contact | 3/3 (6.9) | 3/3 (0.9) | ND | 3/3 (5.5) | 3/3 (403) |
| RD contact | 3/3 (15.9) | 3/3 (1.3) | ND | 3/3 (5.5) | 3/3 (254) |
| PA/10 | |||||
| Inoculated | 3/3 (10.3) | 3/3 (1.5) | 19.0 | 3/3 (6.1) | 3/3 (806) |
| DC contact | 3/3 (11.5) | 3/3 (1.4) | ND | 3/3 (5.5) | 3/3 (640) |
| RD contact | 3/3 (10.8) | 3/3 (1.2) | ND | 3/3 (6.7) | 3/3 (640) |
| KS/09 | |||||
| Inoculated | 3/3 (9.1) | 3/3 (1.6) | 13.2 | 3/3 (5.2) | 3/3 (1015) |
| DC contact | 3/3 (1.5) | 3/3 (0.5) | ND | 3/3 (5.9) | 3/3 (806) |
| RD contact | 2/3 (16.5) | 2/3 (0.5) | ND | 2/3 (4.5) | 2/3 (453) |
ND, not determined.
*Mean percentage decrease in lymphocytes determined at 3 dpi compared with baseline measurements.
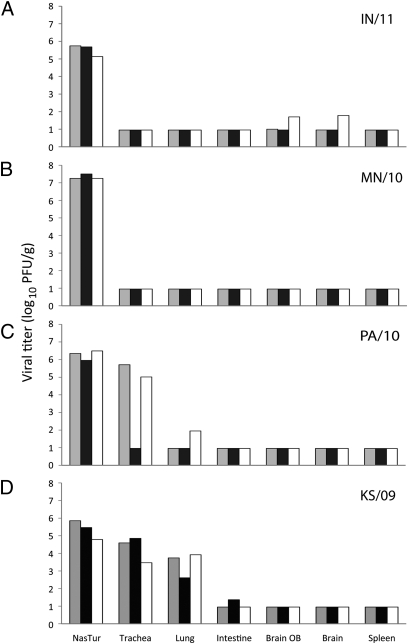
Three additional inoculated ferrets were humanely euthanized on 3 dpi for determination of viral titers in the respiratory tract (nasal turbinates, trachea, and lungs), brain tissue (and olfactory bulbs), intestinal tract (duodenum, jejunum, and descending colon), and spleen. High viral titers were detected in nasal turbinates from ferrets inoculated with each of the 2010–2011 A(H3N2)v viruses; mean titers ranged from 5.5 to 7.3 log10 pfu/mL (Fig. 1 A–C). Although IN/11 and MN/10 viruses were not detected in trachea or lungs, PA/10 virus was detected in the trachea of two of three ferrets (mean 5.4 log10 pfu/g) and in lung tissue of one ferret (1.95 log10 pfu/g). In contrast to the more recent A(H3N2)v viruses, the 2009 (KS/09) virus replicated efficiently throughout the respiratory tract in all three ferrets (Fig. 1D). With the exception of trace amounts of virus (5–6 pfu/g) detected in the brain and intestinal tissues of a single ferret (Fig. 1), no infectious virus was recovered from extrapulmonary tissues, suggesting a general lack of systemic spread of A(H3N2)v viruses in ferrets.
Fig. 1.
Comparison of A(H3N2)v influenza virus titers recovered from ferret tissues. Three ferrets were inoculated by the i.n. route with 106 pfu of IN/11 virus (A), MN/10 virus (B), PA/10 virus (C), or KS/09 virus (D), and tissues were collected 3 dpi. Titers are expressed as log10 pfu per gram of tissue; the limit of detection was 1.0 log10 pfu/g or mL. Nasal turbinate virus titers are expressed as log10 pfu/mL Each bar represents one ferret.
Transient mild lymphopenia has been reported previously after infection of ferrets with seasonal influenza viruses, whereas infection with highly pathogenic avian influenza viruses can result in a substantial reduction in lymphocytes (>20% from baseline levels) (23, 24). To assess the impact of novel A(H3N2)v virus infection on the lymphohemopoetic system, we performed complete blood counts taken before infection, 3 dpi, and 21 dpi. Compared with baseline levels, a significant decrease in the total percentage of lymphocytes (13–24% reduction, P < 0.004) was detected on 3 dpi in ferrets infected with all A(H3N2)v viruses (Table 1). In all virus groups, the lymphopenia observed at 3 dpi resolved by 21 dpi, with leukocyte parameters returning to preinoculation (baseline) levels.
Transmissibility of A(H3N2)v Viruses.
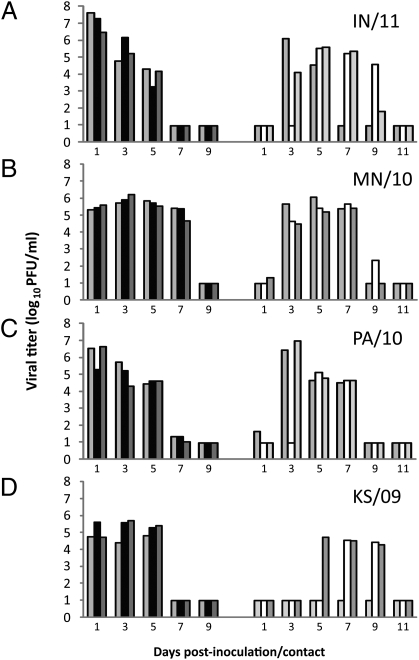
To evaluate the transmissibility of A(H3N2)v viruses, both RD and direct-contact (DC) transmission experiments were performed. For the DC transmission model, a naïve contact ferret was introduced into the same cage as each inoculated ferret 1 d after inoculation. For RD transmission experiments, naïve ferrets were placed in adjacent cages with modified walls containing perforations to allow for air exchange while restricting physical contact between animals (25). RD transmission is a more stringent test of virus transmissibility because it requires virus to be transmitted only through the exchange of air containing virus particles. Transmission was assessed by titration of infectious virus in nasal washes and measurement of hemagglutination inhibition (HI) titers in convalescent sera of contact ferrets. All four A(H3N2)v viruses transmitted efficiently in the DC model; virus was detected in nasal washes in all contact ferrets as early as 1 d postcontact (dpc) (Fig. S1), and seroconversion was confirmed in all animals (Table 1).
The 2010–2011 A(H3N2)v viruses, MN/10, PA/10, and IN/11, transmitted efficiently by RD to three of three RD contact ferrets as early as 1 dpc, and all contact ferrets shed virus and seroconverted at levels similar to those of inoculated animals (Table 1 and Fig. 2 A–C). A repeat experiment was performed with MN/10 virus to confirm efficient RD transmission, and similar results held for both 100% transmission (three of three positive-contact ferrets) and early (1–3 dpc) spread of virus to RD contact ferrets. The 2009 H3N2 virus, KS/09, spread to only two of three RD contact ferrets, and the kinetics of transmission was delayed by 5 or more dpc (Fig. 2D). In general, RD contact ferrets exhibited similar symptoms of fever and lethargy compared with A(H3N2)v-inoculated ferrets (Table 1). Altogether, these data demonstrate that the 2010–2011 A(H3N2)v viruses replicated efficiently in ferrets and readily transmitted in both the DC and RD models, whereas the 2009 A(H3N2)v virus exhibited efficient DC transmission but less efficient RD transmission.
Fig. 2.
Transmissibility of A(H3N2)v influenza viruses among ferrets in the RD model. Three ferrets each were inoculated i.n. with 106 pfu of IN/11 virus (A), MN/10 virus (B), PA/10 virus (C), or KS/09 virus (D); a naïve ferret was placed in an adjacent cage at 24 h after inoculation to initiate contact. Nasal washes were collected from inoculated (dark bars) and contact (light bars) ferrets, and titers are expressed as log10 pfu/mL. Values for individual ferrets are shown.
Glycan Binding Properties of MN/10, PA/10, and KS/09 Viruses.
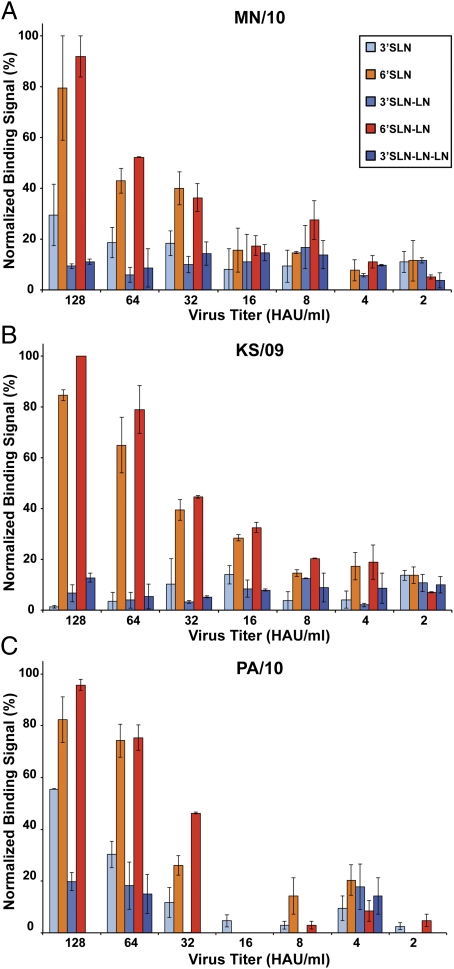
A comparison of the critical amino acid residues constituting the HA receptor-binding site (RBS) between MN/10, KS/09, and PA/10 viruses showed that they were very similar (Table S1). The RBS of these viruses was composed of characteristic residues found in other human-adapted seasonal H3N2 viruses, including Asp190, a hydrophobic amino acid (such as Val/Ile/Leu) at 226 instead of Gln (typically found in avian viruses), and Ser228, which are known to be critically involved in binding to α2-6–sialylated glycans. However, in comparison with seasonal and 1968 pandemic H3N2 viruses, MN/10, KS/09, and PA/10 viruses possessed differences in other residues that contact the glycan receptor, including 156, 137, 193, and 225 (Table S1).
To investigate the glycan receptor-binding properties of MN/10, KS/09, and PA/10 viruses, we analyzed the binding of these viruses in a dose-dependent fashion to representative α2-3– and α2-6–sialylated glycans on a glycan array platform (Fig. 3). All three viruses showed similar predominant binding to α2-6–sialylated glycans in comparison with α2-3–sialylated glycans, indicating that their HA had characteristic binding properties of human-adapted seasonal influenza viruses. The predominant binding to α2-6–sialylated glycan receptors by these viruses is consistent with the characteristic amino acids in the 190, 226, and 228 positions in the RBS that are typically found in HA from human-adapted seasonal viruses (26, 27). The binding characteristics exhibited by the A(H3N2)v viruses as tested in this glycan array system suggest that these viruses would replicate efficiently in the upper respiratory tract of humans, where α2-6 sialic acid linkages are more abundant (21, 22).
Fig. 3.
Binding preference of A(H3N2)v influenza viruses. Dose-dependent direct glycan array binding of MN/10 (A), KS/09 (B), and PA/10 (C) viruses. 3′SLN, 3′SLN-LN, and 3′SLN-LN-LN are representative avian receptors, and 6′SLN and 6′SLN-LN are representative human receptors. The binding signals were determined based on the HRP activity by using the Amplex Red Peroxidase Assay (Invitrogen) according to the manufacturer's instructions. The assays were done in triplicate, and appropriate negative controls were included.
A(H3N2)v Viruses Replicate Efficiently in Human Airway Epithelial Cells.
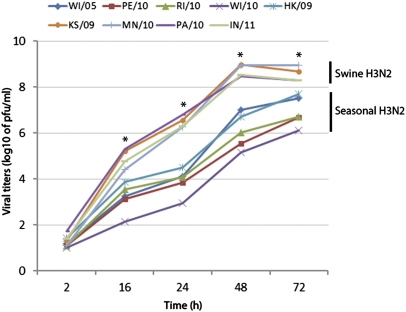
Because the airway epithelium is the primary site of influenza virus replication in humans, we investigated the replication efficiency of the A(H3N2)v viruses in Calu-3 cells, derived from human bronchial epithelium. Grown on transwell inserts, the Calu-3 cell line forms polarized monolayers that resemble the in vivo airway epithelium (28). We compared the replication kinetics of five selected seasonal H3N2 viruses to those of the four A(H3N2)v viruses. Calu-3 monolayers were inoculated with each virus at a multiplicity of infection (MOI) of 0.01, and supernatants were collected at the times indicated and titered for the presence of infectious virus (Fig. 4). With all viruses tested, titers of progeny virus progressively increased during the first 48 h postinoculation (hpi) Notably, all four A(H3N2)v viruses exhibited a 26- to 2,600-fold increase in replication at 48 hpi compared with seasonal H3N2 viruses (P < 0.004). These data demonstrate that the A(H3N2)v viruses replicate efficiently and to high titers in a model of human airway epithelial cells.
Fig. 4.
Replication kinetics of A(H3N2)v influenza viruses in polarized human airway epithelial cells. The seasonal H3N2 viruses are abbreviated as follows: WI/05, A/Wisconsin/67/2005; PE/10, A/Perth/16/2009; RI/10, A/Rhode Island/01/2010; WI/10, A/Wisconsin/13/2010; and HK/09, A/Hong Kong/34341/2009. Calu-3 cells cultured for 1 wk were inoculated with virus at an MOI of 0.01. Culture supernatants were collected at the times indicated, and virus titers were determined by standard plaque assay. The titer value represents the average for three independent wells. Asterisks indicate statistically significant difference between seasonal H3N2 viruses and four A(H3N2)v viruses at 16, 24, 48, and 72 h, based on Mann–Whitney test (each was P < 0.004).
Discussion
The recent cases of human infection by the A(H3N2)v viruses have raised public health concerns and highlight the need to better understand the potential of these viruses to spread and cause disease in humans. In this study, we characterized four A(H3N2)v influenza viruses that were isolated from humans in 2009, 2010, and 2011. In cultured human respiratory epithelial cells, we observed that the A(H3N2)v viruses replicated to higher levels than seasonal H3N2 influenza viruses did, suggesting that these viruses have the ability to efficiently infect cells of the human airway. We found that the 2010 and 2011 virus isolates, MN/10, PA/10, and IN/11, replicated efficiently in ferrets, caused morbidity, and transmitted efficiently to contact ferrets. These novel swine-origin A(H3N2)v viruses were also found to possess human-like (α2-6–linked) receptor-binding properties consistent with the efficient RD transmission displayed by the 2010 and 2011 virus isolates. These findings underscore the need for continued surveillance and characterization of these viruses because they resemble viruses with pandemic potential.
The ferret model recapitulates the efficient transmission of seasonal influenza viruses and the poor transmission of avian influenza viruses in humans (25, 29–31). The transmission kinetics and efficient RD transmission of the 2010 and 2011 A(H3N2)v viruses is comparable to that observed with seasonal influenza viruses in ferrets (23, 29, 32, 33). The high titers of virus shedding observed (peak mean titers 5.2–7.1 log10 pfu/mL) in ferret nasal washes correlated with the high-growth phenotype of A(H3N2)v viruses in human airway epithelial cells. The significantly higher release of progeny virus from A(H3N2)v-infected Calu-3 cells reached levels previously observed in Calu-3 cell cultures infected with the 1918 pandemic virus (34). The A(H3N2)v viruses induced morbidity in ferrets (mean maximum weight loss of >8%) and lymphopenia to levels comparable to the 2009 pandemic and TRS H1N1 viruses (24, 35–37) but substantially less than those observed with avian H5N1 viruses (23, 38–40).
The binding preference of influenza viruses for receptors on cells of the airway epithelium is likely a determinant of efficient RD transmission (21, 27, 32). Human-adapted seasonal influenza H1 and H3 HA demonstrate high specificity for α2-6–sialylated glycans, and it has been postulated that efficient and sustained human-to-human transmission of influenza viruses requires an α2,6 sialic acid receptor-binding preference (21, 22, 27, 30, 32, 41). Bateman et al. demonstrated that TRS H3N2 viruses isolated in the late 1990s bound exclusively to α2-6–sialylated glycans (42). The A(H3N2)v viruses tested here have retained a human receptor-binding affinity for α2-6–linked sialic acids, similar to human seasonal H3N2 viruses (43) despite distinct evolutionary pathways of these viruses since the introduction of this subtype into the pig population in the late 1990s (6, 8, 13).
Identification of the genetic determinants that govern efficient replication and transmission of A(H3N2)v viruses are needed to understand the factors that may lead to the emergence of future swine-origin pandemic influenza viruses. In comparison with the 2010–2011 A(H3N2)v viruses, the 2009 H3N2 (KS/09) virus possessed a distinct phenotype in ferrets that included a greater tropism for lung tissue and reduced RD transmission efficiency. Previous studies with different subtypes of influenza A viruses have suggested that the major determinants for viral replication, pathogenesis, and/or transmission are located in the HA: polymerase subunit proteins PB2 and PB1-F2 (30, 32, 44, 45). KS/09 HA and neuraminidase (NA) proteins are phylogenetically distinct from the 2010–2011 A(H3N2)v viruses, with amino acid divergence of ∼5% and 5–6% from the 2010–2011 A(H3N2)v viruses, respectively. The amino acid changes seen in the HA1 subunit are mostly mapping to antigenic sites, with only one amino acid change located in a receptor-binding region (13) (at amino acid position 154). As observed in our glycan binding experiments, none of these changes appear to affect sialic acid binding pattern, which would suggest a change in virus binding to cell types in the respiratory tract.
The greatest identity among the A(H3N2)v viruses are in the proteins PB1 (98–99%), PB2 (99%), and PA (98–99%) as well as in NP (99–100%) and NS1/nuclear export protein (NEP) (99–100%) genes. Interestingly, with the exception of the 2011 (IN/11) virus, the M protein shares 100% identity among the viruses tested in this study. Genetic analysis of IN/11 virus, as well as the other 11 2011 A(H3N2)v viruses, revealed that the M gene was inherited from the A(H1N1)pdm09 virus (16, 17). Although it has been suggested that the M segment of the A(H1N1)pdm09 virus is important for enhancing RD transmission in the guinea pig model (36), the IN/11 virus displayed a similar transmission phenotype to that of the 2010 A(H3N2)v viruses in ferrets. Thus, it is unclear whether the acquisition of the M gene from A(H1N1)pdm09 virus enhanced the ability of A(H3N2)v virus to spread in pigs and infect humans.
Common to all A(H3N2)v viruses, as well as classical swine viruses, is the glutamic acid (E) at position 627 in PB2, aspartic acid at position 701, and the serine/arginine (SR) polymorphism at positions 590/591. The lack of lysine at position 627 and asparagine at position 701, reported as markers of virus adaptation to mammals, replication, and transmissibility, are compensated by the SR polymorphism at positions 590/591 (44). This change is also present in PB2 of the A(H1N1)pdm09 viruses (10). The greatest genetic difference between the KS/09 and 2010–2011 A(H3N2)v is found in PB1-F2. The two 2010 A(H3N2)v viruses are predicted to produce a full-length 90-aa protein, and, even though IN/11 produces a truncated 79-aa protein, presumably it is still functional and localizes to the mitochondria (46). On the other hand, KS/09 produces a truncated, nonfunctional 57-aa protein similar to seasonal human viruses. Full-length PB1-F2 has been shown to have proapoptotic function (47) and has been related to delayed virus clearance from lungs, whereas the absence of this protein has been reported to reduce mortality in mice (48). Because TRS viruses have a unique genetic combination, additional studies are needed to fully understand the molecular correlates A(H3N2)v virus virulence and transmission.
Genetic variation attributable to the gradual accumulation of HA mutations or genetic reassortment of influenza A viruses in pigs is unpredictable and may lead to the generation of novel influenza viruses against which a subset of the population lacks serologic immunity. In North America, there are multiple combinations of TRS influenza viruses that have been isolated from healthy-appearing swine, and A(H3N2)v viruses are one of the most common subtypes circulating in this species (6–8, 13). The evolution of antigenically distinct H3N2 viruses in pigs may pose a threat to humans lacking cross-reactive serologic immunity. The A(H3N2)v viruses have retained some antigenic properties of human seasonal influenza viruses that circulated in the mid-1990s, but they are antigenically distinct from the contemporary human seasonal H3N2 vaccine virus, A/Perth/16/2009, and would not be well covered by the current trivalent vaccine (13). The data presented in this study suggest that A(H3N2)v viruses have the capacity for efficient replication and transmission in mammals and underscore the need for continued public health surveillance of this emerging virus.
Materials and Methods
Viruses.
The stocks of IN/11 and MN/10 virus were grown in Madin–Darby canine kidney cells as previously described (28). PA/10, KS/09, and seasonal human H3N2 viruses used in the study were grown in the allantoic cavities of 10-d-old embryonated hens’ eggs at 37 °C for 48 h (34, 39). The identities of virus genes of virus stocks were confirmed by the Centers for Disease Control and Prevention Influenza Sequencing Activity, and genetic analysis was performed with BioEdit 7.0.9.0 (49) and Mega 5.04 programs (50). To determine a pfu titer, stocks of virus were titrated in Madin–Darby canine kidney cells by using standard plaque assay methods (28). All experiments were performed in negative-pressure biosafety level 3 laboratories with enhancements (BSL3+) as outlined in Biosafety in Microbiological and Biomedical Laboratories (51).
Ferret Pathogenesis and Transmission Experiments.
Animal research was conducted under the guidance of the Centers for Disease Control and Prevention's Institutional Animal Care and Use Committee in an Association for Assessment and Accreditation of Laboratory Animal Care International-accredited animal facility. Male Fitch ferrets (Triple F Farms) at 6 mo of age and serologically negative by HI assay for currently circulating influenza viruses were used (33). After intranasal (i.n.) inoculation of 106 pfu in 1 mL, the pathogenesis of each virus was determined (39). RD and DC virus transmission models were performed as previously described (25). Nasal washes were collected from ferrets every other dpi or dpc and titered by plaque assay. Statistical significance of virus titers in nasal washes was determined by Student's t test. Convalescent serum was collected from inoculated and contact animals at 21 dpi to assess seroconversion to virus by HI assay (52). Ferret complete blood count analyses were performed on blood collected at 0, 3, and 21 dpi as previously described (24).
Dose-Dependent Direct Binding of H3N2 Virus by Glycan Array.
A streptavidin plate array comprising representative biotinylated α2-3– and α2-6–sialylated glycans as described in Table S2 was used for the analysis (27, 45). 3′SLN, 3′SLN-LN, and 3′SLN-LN-LN are representative avian receptors, and 6′SLN and 6′SLN-LN are representative human receptors (Table S2). The viruses (hemagglutination units HAU titers indicated) were diluted to 250 μL with 1× PBS + 1% BSA. Diluted virus in 50 μL was added to each of the glycan-coated wells and incubated overnight at 4 °C. The primary and secondary antibodies used to detect binding were ferret anti–MN/10 antisera (1:500 diluted in 1× PBS + 1% BSA) and anti–ferret HRP-conjugated antibody (1:500 diluted in 1× PBS + 1% BSA, respectively). After each step, the wells were washed thrice with 1× PBST (1× PBS + 0.1% Tween-20) followed by 1× PBS. The wells were blocked with 1× PBS + 1% BSA for 2 h at 4 °C before adding antibodies. The binding signals were determined based on the HRP activity determined by using the Amplex Red Peroxidase Assay (Invitrogen) according to the manufacturer's instructions. The assays were done in triplicate, and appropriate negative controls were included.
Infection of Calu-3 Human Airway Epithelial Cells.
Calu-3 cells were grown in Eagle's MEM and seeded onto semipermeable membrane transwell inserts as previously described (28). Briefly, after confirming transepithelial resistance, apical inoculation of influenza viruses at an MOI of 0.01 was performed. Aliquots of culture supernatant taken postinoculation from triplicate cultures were titrated for the presence of infectious virus by standard plaque assay. The statistical significance of virus titer data were determined by using Student's t test and unpaired two-tailed Mann–Whitney test.
Supplementary Material
Acknowledgments
This work was supported in part by National Institutes of Health (GM 57073) and Singapore-MIT Alliance for Research and Technology awarded to R.S.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1119945109/-/DCSupplemental.
References
- 1.Barker WH, Mullooly JP. Impact of epidemic type A influenza in a defined adult population. Am J Epidemiol. 1980;112:798–811. doi: 10.1093/oxfordjournals.aje.a113052. [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 3.Dawood FS, et al. Novel Swine-Origin Influenza A (H1N1) Virus Investigation Team Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–2615. doi: 10.1056/NEJMoa0903810. [DOI] [PubMed] [Google Scholar]
- 4.Louie JK, et al. California Pandemic (H1N1) Working Group Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302:1896–1902. doi: 10.1001/jama.2009.1583. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Padilla R, et al. INER Working Group on Influenza Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N Engl J Med. 2009;361:680–689. doi: 10.1056/NEJMoa0904252. [DOI] [PubMed] [Google Scholar]
- 6.Olsen CW. The emergence of novel swine influenza viruses in North America. Virus Res. 2002;85:199–210. doi: 10.1016/s0168-1702(02)00027-8. [DOI] [PubMed] [Google Scholar]
- 7.Landolt GA, Karasin AI, Phillips L, Olsen CW. Comparison of the pathogenesis of two genetically different H3N2 influenza A viruses in pigs. J Clin Microbiol. 2003;41:1936–1941. doi: 10.1128/JCM.41.5.1936-1941.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richt JA, et al. Pathogenic and antigenic properties of phylogenetically distinct reassortant H3N2 swine influenza viruses cocirculating in the United States. J Clin Microbiol. 2003;41:3198–3205. doi: 10.1128/JCM.41.7.3198-3205.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shinde V, et al. Triple-reassortant swine influenza A (H1) in humans in the United States, 2005–2009. N Engl J Med. 2009;360:2616–2625. doi: 10.1056/NEJMoa0903812. [DOI] [PubMed] [Google Scholar]
- 10.Garten RJ, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palese P, Shaw ML. Orthomyxoviridae: The viruses and their replication. In: Knipe DM, Howley PM, editors. Fields Virology. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 1647–1689. [Google Scholar]
- 12.Simonsen L, et al. The impact of influenza epidemics on mortality: Introducing a severity index. Am J Public Health. 1997;87:1944–1950. doi: 10.2105/ajph.87.12.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shu B, et al. Genetic analysis and antigenic characterization of swine origin influenza viruses isolated from humans in the United States, 1990–2010. Virology. 2012;422:151–160. doi: 10.1016/j.virol.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 14.Cox CM, et al. Swine influenza virus A (H3N2) infection in human, Kansas, USA, 2009. Emerg Infect Dis. 2011;17:1143–1144. doi: 10.3201/eid1706.101488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anonymous; Centers for Disease Control and Prevention (CDC) Update: Influenza activity—United States, 2010–11 season, and composition of the 2011–12 influenza vaccine. MMWR Morb Mortal Wkly Rep. 2011;60:705–712. [PubMed] [Google Scholar]
- 16.Anonymous; Centers for Disease Control and Prevention (CDC) Swine-origin influenza A (H3N2) virus infection in two children—Indiana and Pennsylvania, July–August 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1213–1215. [PubMed] [Google Scholar]
- 17.Anonymous; Centers for Disease Control and Prevention (CDC) Limited human-to-human transmission of novel influenza A (H3N2) virus—Iowa, November 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1615–1617. [PubMed] [Google Scholar]
- 18.Belser JA, Szretter KJ, Katz JM, Tumpey TM. Use of animal models to understand the pandemic potential of highly pathogenic avian influenza viruses. Adv Virus Res. 2009;73:55–97. doi: 10.1016/S0065-3527(09)73002-7. [DOI] [PubMed] [Google Scholar]
- 19.Smith H, Sweet C. Lessons for human influenza from pathogenicity studies with ferrets. Rev Infect Dis. 1988;10:56–75. doi: 10.1093/clinids/10.1.56. [DOI] [PubMed] [Google Scholar]
- 20.Maher JA, DeStefano J. The ferret: An animal model to study influenza virus. Lab Anim (NY) 2004;33(9):50–53. doi: 10.1038/laban1004-50. [DOI] [PubMed] [Google Scholar]
- 21.Shinya K, et al. Avian flu: Influenza virus receptors in the human airway. Nature. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- 22.van Riel D, et al. H5N1 virus attachment to lower respiratory tract. Science. 2006;312:399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- 23.Gustin KM, et al. Influenza virus aerosol exposure and analytical system for ferrets. Proc Natl Acad Sci USA. 2011;108:8432–8437. doi: 10.1073/pnas.1100768108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Belser JA, et al. Pathogenesis and transmission of triple-reassortant swine H1N1 influenza viruses isolated before the 2009 H1N1 pandemic. J Virol. 2011;85:1563–1572. doi: 10.1128/JVI.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maines TR, et al. Lack of transmission of H5N1 avian–human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci USA. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kumari K, et al. Receptor binding specificity of recent human H3N2 influenza viruses. Virol J. 2007;4:42. doi: 10.1186/1743-422X-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Srinivasan A, et al. Quantitative biochemical rationale for differences in transmissibility of 1918 pandemic influenza A viruses. Proc Natl Acad Sci USA. 2008;105:2800–2805. doi: 10.1073/pnas.0711963105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zeng H, et al. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type I interferon response in polarized human bronchial epithelial cells. J Virol. 2007;81:12439–12449. doi: 10.1128/JVI.01134-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herlocher ML, et al. Ferrets as a transmission model for influenza: Sequence changes in HA1 of type A (H3N2) virus. J Infect Dis. 2001;184:542–546. doi: 10.1086/322801. [DOI] [PubMed] [Google Scholar]
- 30.Van Hoeven N, et al. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc Natl Acad Sci USA. 2009;106:3366–3371. doi: 10.1073/pnas.0813172106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roberts KL, Shelton H, Scull MA, Pickles RJ, Barclay WS. Lack of transmission of a human influenza virus with avian receptor specificity between ferrets is not due to decreased virus shedding but rather a lower infectivity in vivo. J Gen Virol. 2011;92:1822–1831. doi: 10.1099/vir.0.031203-0. [DOI] [PubMed] [Google Scholar]
- 32.Tumpey TM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 33.Maines TR, et al. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science. 2009;325:484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tumpey TM, et al. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;310:77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 35.Munster VJ, et al. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chou YY, et al. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol. 2011;85:11235–11241. doi: 10.1128/JVI.05794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Itoh Y, et al. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature. 2009;460:1021–1025. doi: 10.1038/nature08260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zitzow LA, et al. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J Virol. 2002;76:4420–4429. doi: 10.1128/JVI.76.9.4420-4429.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maines TR, et al. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yen HL, et al. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol. 2007;81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chandrasekaran A, et al. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat Biotechnol. 2008;26:107–113. doi: 10.1038/nbt1375. [DOI] [PubMed] [Google Scholar]
- 42.Bateman AC, et al. Glycan analysis and influenza A virus infection of primary swine respiratory epithelial cells: The importance of NeuAcα2-6 glycans. J Biol Chem. 2010;285:34016–34026. doi: 10.1074/jbc.M110.115998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stevens J, et al. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 44.Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 2009;5:e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jayaraman A, et al. A single base-pair change in 2009 H1N1 hemagglutinin increases human receptor affinity and leads to efficient airborne viral transmission in ferrets. PLoS ONE. 2011;6:e17616. doi: 10.1371/journal.pone.0017616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zell R, Krumbholz A, Wutzler P. Influenza A virus PB1-F2 gene. Emerg Infect Dis. 2006;12:1607–1608, author reply 1608–1609. doi: 10.3201/eid1210.060511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen W, et al. A novel influenza A virus mitochondrial protein that induces cell death. Nat Med. 2001;7:1306–1312. doi: 10.1038/nm1201-1306. [DOI] [PubMed] [Google Scholar]
- 48.Zamarin D, Ortigoza MB, Palese P. Influenza A virus PB1-F2 protein contributes to viral pathogenesis in mice. J Virol. 2006;80:7976–7983. doi: 10.1128/JVI.00415-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hall TA. BioEdit: A user-friendly biological sequence alignment. analysis program for Windows 95/98/NT. Nucl Acids Symp Ser. 1999;41:95–98. [Google Scholar]
- 50.Kumar S, Tamura K, Nei M. MEGA3: Integrated software for Molecular Evolutionary Genetics Analysis and sequence alignment. Brief Bioinform. 2004;5:150–163. doi: 10.1093/bib/5.2.150. [DOI] [PubMed] [Google Scholar]
- 51.Richmond JY, McKinney RW. Biosafety in Microbiological and Biomedical Laboratories. 5th Ed. Atlanta, GA: Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 52.Stephenson I, Wood JM, Nicholson KG, Charlett A, Zambon MC. Detection of anti-H5 responses in human sera by HI using horse erythrocytes following MF59-adjuvanted influenza A/Duck/Singapore/97 vaccine. Virus Res. 2004;103:91–95. doi: 10.1016/j.virusres.2004.02.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.