Abstract
Thyroidectomy is a safe procedure often performed either for benign or malignant thyroid diseases. Complication rate is low and tracheal injury associated with thyroidectomy is rarely described. The trachea may be perforated or lacerated intraoperatively; nevertheless, damage is usually recognized and directly repaired with reduced patient morbidity. We review a case of a 45-year-old male with a history of non-invasive thyroid cancer who underwent a total thyroidectomy with a tracheal necrosis and a subsequent rupture presenting 4 days following surgical operation. At home, while coughing, the patient experienced rapid swelling of neck, face and upper part of the chest. Computed tomography scan images demonstrated extensive subcutaneous emphysema and a defect in cervical trachea, confirmed also by bronchoscopy. The patient, without delay, underwent an exploration of the neck with a debridement of laceration. In view of the fact that a local infection was present, only a right pre-thyroid muscle flap was stitched on the defect. The patients recovered uneventfully.
Keywords: Total thyroidectomy, Tracheal injury, Virtual bronchoscopy
INTRODUCTION
Thyroidectomy is a safe procedure often performed either for benign or malignant thyroid diseases. Complication rate is low and includes vocal fold paresis or paralysis, hypoparathyroidism, hypocalcaemia, hematoma and wound infection [1]. Tracheal injury associated with thyroidectomy is rare. The trachea may be perforated or lacerated intraoperatively; the damage is usually recognized and repaired at once with little or no patient morbidity. However, unrecognized injury, or delayed rupture secondary to tracheal necrosis, can present up to 2 weeks postoperatively. We review a case of tracheal necrosis with subsequent rupture, which presented 4 days following total thyroidectomy.
CASE REPORT
A 45-year-old male with a history of non-invasive thyroid cancer underwent a total thyroidectomy. Past medical history was uneventful. Patient had not received any radiation therapy before surgery. After oro-tracheal intubation, a formal thyroidectomy and lymph node dissection was performed using electro-cautery and bipolar cautery forceps. No intraoperative complication occurred. Estimated intraoperative blood loss was negligible. The patient was discharged on postoperative day 2 in good condition. The histology demonstrated a papillary cancer of the thyroid with metastasis at bilateral recurrent lymph nodes. On postoperative day 4, the patient (while coughing) felt a sudden pop in his neck and experienced rapid swelling of his neck, face and upper part of the chest. A chest X-ray showed subcutaneous emphysema but no pneumothorax. Computed tomography (CT) image demonstrated extensive subcutaneous emphysema and a defect in cervical trachea (Fig. 1a). Virtual bronchoscopy (Fig. 1b) demonstrated an elliptic defect in right antero-lateral tracheal wall (black arrow) at the level of the fourth tracheal ring. The patient was taken to the operating room and, after a bronchoscopic confirmation of the tracheal lesion, an exploration of the neck through the original thyroidectomy wound was performed. A 6-mm longitudinal elliptic laceration was visualized in the right antero-lateral tracheal wall between two tracheal rings. The wound was debrided and irrigated. Since a local infection was present, the laceration was not primarily closed; a right pre-thyroid muscle flap was stitched with an absorbable suture on the defect. Aspirative drains were placed into the neck and into the anterior mediastinum. The patient was immediately extubated. Broad-spectrum antibiotics were administered. Cultures obtained from the neck wound intraoperatively grew colonies of Staphylococcus aureus. A bronchoscopy obtained in postoperative day 6 demonstrated an irregular 5-mm surface with fibrin edges at the level of the fourth tracheal ring (Fig. 2). The patients recovered uneventfully.
Figure 1:
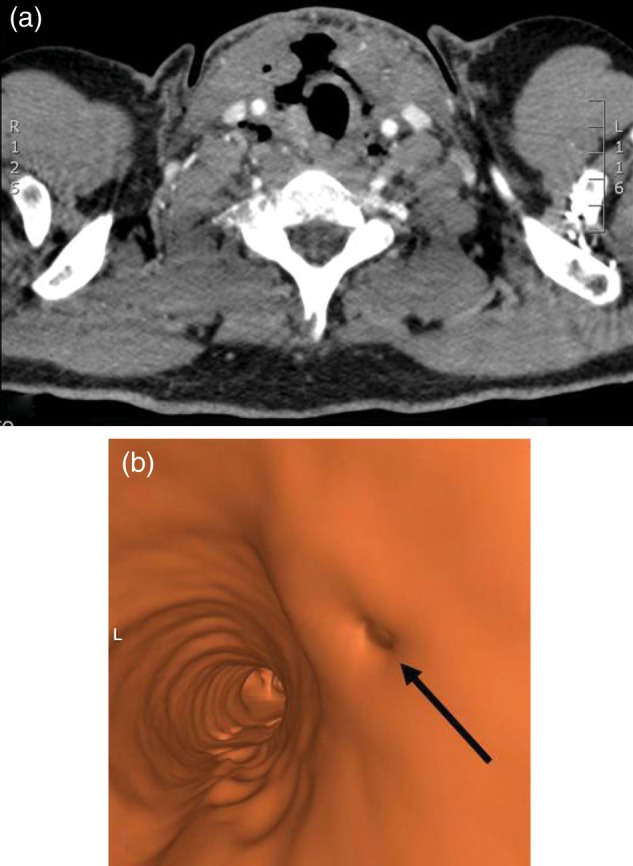
(a) CT image demonstrate extensive subcutaneous emphysema and the defect in cervical trachea. (b) Virtual bronchoscopy demonstrates an elliptic defect in right antero-lateral tracheal wall (black arrow) at the level of the fourth tracheal ring (L = left).
Figure 2:
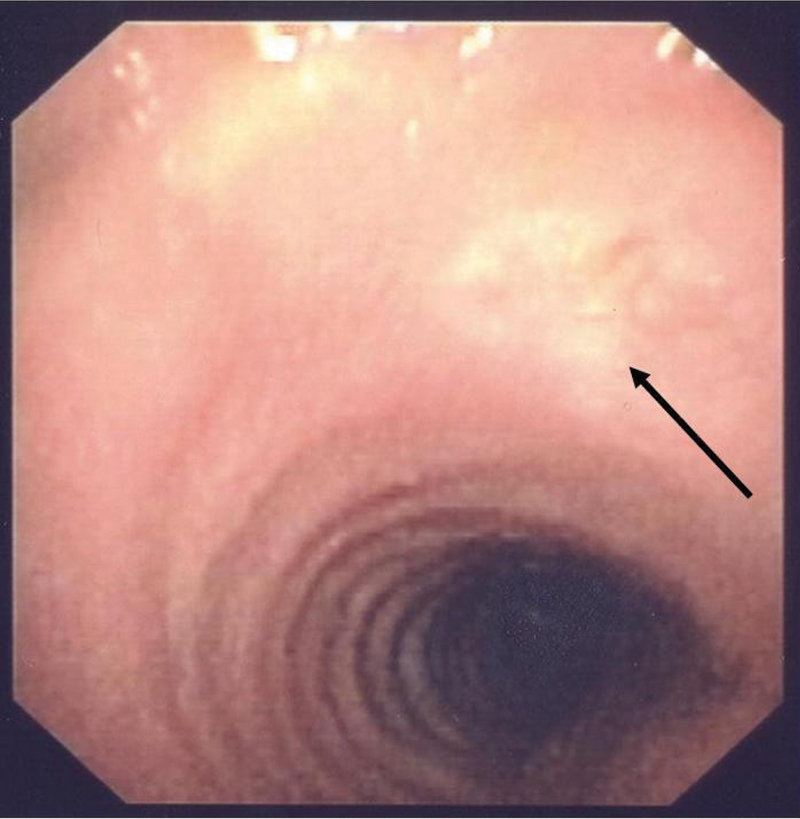
Bronchoscopy in postoperative day 6 demonstrates an irregular 5-mm surface with fibrin edges at the level of the fourth tracheal ring.
DISCUSSION
Tracheal injury following thyroidectomy is rare. Gosnell et al. [2] identified an incidence of perforation of 0.06%. Risk factors for injury include female gender, thyreotoxic goiter, prolonged intubation with high cuff pressure, use of diathermy (especially with the increased blood loss) and persistent uncontrolled cough in the postoperative period [3]. The trachea may be perforated at the time of the initial surgery or may undergo necrosis in the early postoperative period. Devascularization of the tracheal wall through thermal injury from coagulation is the most likely cause of necrosis. Wound infection may also be a complicating factor. The patient presented in this case had none of the risk factors associated with delayed tracheal perforation.
Acute perforations tend to occur in the lateral trachea in the region of the ligament of Berry [4]. If recognized at the time of the initial surgery, perforation can often be closed primarily with absorbable suture with no morbidity. Strap muscle may also be rotated over the site to further reinforce the repair. A visual inspection of the trachea may, however, miss a small perforation. The placement of drains and the use of postoperative antibiotics are dictated by surgeon preference.
Perforations that are missed initially, or tracheal necrosis that evolves later, may present in the ensuing days as a wound infection, subcutaneous emphysema or progressive respiratory compromise. History may reveal a bout of vigorous coughing prior to the onset of symptoms. Complaints of retrosternal pain are concerning for pneumomediastinum or pneumothorax. Flexible bronchoscopy is the procedure of choice to visualize the site of the perforation. A chest X-ray should be obtained to assess for pneumothorax or pneumomediastinum. A CT of the neck and chest is more sensitive and may help either localize the site of the perforation or detect fluid collections.
Surgery must not be delayed. Airway control should be a priority. Equipment should be on hand for performing an emergent tracheostomy, if necessary. A rapid sequence induction of anaesthesia and orotracheal intubation with placement of the cuff distal to the site of injury is usually sufficient to control the airway. Potential patient morbidity, although uncommon, includes neck abscess, mediastinitis, pneumothorax, cardiac tamponade and tension pneumomediastinum. Mortality has been reported anecdotally [5].
Our patient was subjected to total thyroidectomy. In view of the bilateral neck dissection undertaken, the possibility of ischaemic necrosis of the tracheal wall exists. In our case, inadvertent minor injury to trachea may have ensued during dissection of the thyroid off the trachea which may have gone unnoticed peri-operatively, but a thermal injury was considered improbable due to the use of a bipolar cautery forceps with a very low setting. But, in the postoperative period, this injury, coupled with possible ischaemia, may have led to the tracheal necrosis. Alternatively, an infection of the surgical site might have been the primum movens and have led to the necrosis in a point of relative weakness. The prompt re-exploration of the neck prevented any untoward outcome.
Conflict of interest: none declared.
REFERENCES
- 1.Sosa JA, Udelsman R. Total thyroidectomy for differentiated thyroid cancer. J Surg Oncol. 2006;94:701–7. doi: 10.1002/jso.20695. doi:10.1002/jso.20695. [DOI] [PubMed] [Google Scholar]
- 2.Gosnell JE, Campbell P, Sidhu S, Sywak M, Reeve TS, Delbridge LW. Inadvertent tracheal perforation during thyroidectomy. Br J Surg. 2006;93:55–6. doi: 10.1002/bjs.5136. doi:10.1002/bjs.5136. [DOI] [PubMed] [Google Scholar]
- 3.Iacconi P. Inadvertent tracheal perforation during thyroidectomy. Br J Surg. 2006;93:770–1. doi: 10.1002/bjs.5136. doi:10.1002/bjs.5480. [DOI] [PubMed] [Google Scholar]
- 4.Jacqmin S, Lentschener C, Demirev M, Gueroult S, Herman P, Ozier Y. Postoperative necrosis of the anterior part of the cervical trachea following thyroidectomy. J Anesth. 2005;19:347–8. doi: 10.1007/s00540-005-0330-4. doi:10.1007/s00540-005-0330-4. [DOI] [PubMed] [Google Scholar]
- 5.Chauhan A, Ganguly M, Saidha N, Gulia P. Tracheal necrosis with surgical emphysema following thyroidectomy. J Postgrad Med. 2009;55:193–5. doi: 10.4103/0022-3859.57401. doi:10.4103/0022-3859.57401. [DOI] [PubMed] [Google Scholar]


