Abstract
We report on three out of 270 consecutive patients (1.1%) suffering from coronary artery obstruction or occlusion at the end of transcatheter aortic valve implantation (TAVI). The partial or total obstruction of the coronary artery seen in the post-implantation aortography was accompanied by haemodynamic instability and electrocardiographic changes typical for myocardial ischaemia. Immediate percutaneous coronary intervention with stent implantation was successful in two cases, while in the third case it was not possible to cross the occluded right coronary artery. Emergency coronary artery bypass grafting was performed resulting in uneventful myocardial recovery. All patients were discharged home. These cases highlight the awareness of this rare, life-threatening complication of TAVI, which is in need of a dedicated heart team involved not only in decision-making, but also in the procedure itself.
Keywords: Transcatheter aortic valve implantation, Complication, Coronary occlusion, Aortic stenosis
INTRODUCTION
Nowadays, transcatheter aortic valve implantation (TAVI) is an accepted treatment option for high-risk patients with severe aortic stenosis (AS) not amenable for conventional aortic valve replacement [1]. One prerequisite for TAVI is decision-making in a heart team to offer an individualized treatment option (aortic valve replacement versus TAVI) and appropriate approach (transfemoral versus transapical) [2] for each patient. The procedure should be performed within the heart team to (i) assure an optimal procedure and (ii) to successfully treat possible complications. One of these is obstruction or occlusion of coronary arteries [3]. We report three out of 270 consecutive TAVI procedures (1.1%) suffering from obstruction or occlusion of a coronary ostium.
MATERIAL AND METHODS
Since August 2008, 270 consecutive patients (mean age 82.5 ± 5.3 years, mean logistic EuroSCORE 29.5 ± 16%) underwent TAVI for severe AS. The decision to treat a patient by TAVI was made by a ‘heart team’ consisting of an interventional cardiologist and a cardiac surgeon as suggested by common recommendations [2]. Presence of severe AS was confirmed via echocardiography according to the ACC/AHA valve guidelines (aortic jet velocity >4 m/s, mean gradient >40 mmHg, AVA <1.0 cm2). TAVI was proposed only in patients with severe AS at high risk or with contraindications for surgery, who presented with symptoms. The decision whether a patient was at high risk for surgery was made by clinical judgement in combination with the assessment of the logistic EuroSCORE.
RESULTS
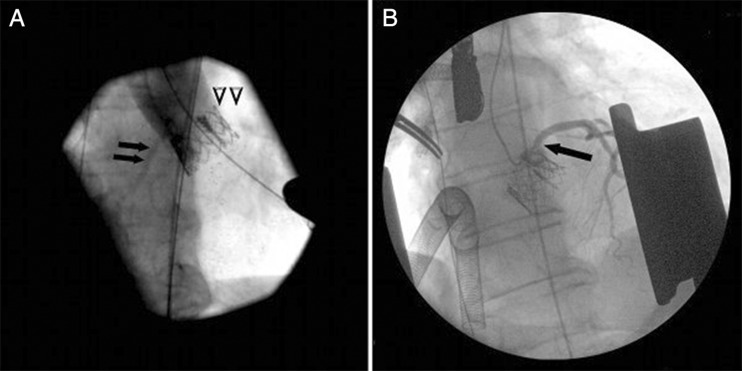
In three out of 270 TAVI procedures (1.1%), a life-threatening coronary obstruction or occlusion of a coronary ostium occurred. The first case was a symptomatic 81-year old female with a logistic EuroSCORE of 21% who underwent transapical TAVI for severe AS. Six days prior to TAVI, the patient underwent percutaneous coronary intervention of a left anterior descending stenosis. Transapical TAVI was performed in a standard manner under general anaesthesia. Under rapid pacing, balloon dilation of the native aortic valve was followed by aortography (20 ml of contrast agent, 20 ml/s). Rapid pacing was started after haemodynamic recovery. Final positioning of a 26 mm Edwards SAPIEN prosthesis (Edwards SAPIEN THV, Edwards Lifesciences, Irvine, CA, USA) was performed with aortography and the valve slowly deployed. When the balloon was deflated and rapid pacing was stopped, the patient did not recover as expected and had impaired left ventricular function determined by direct vision. Final angiographic check by aortography revealed trivial aortic insufficiency, prompt filling of the right coronary artery (RCA) but delayed filling of the left coronary system (Fig. 1A). There was severe ST-segment elevation on leads I and aVL. Haemodynamic status deteriorated rapidly and cardiopulmonary resuscitation (CPR) was initiated after closure of the apex access. After sternotomy, cardiopulmonary bypass (CPB) was established under CPR. Coronary angiography disclosed subtotal occlusion of the left main coronary artery (Fig. 1B). The subtotal occlusion was crossed with a Balance Middleweight Universal guidewire (Abbott Vascular) and stenting was performed with a Driver bare-metal stent (Medtronic Inc.). The patient's haemodynamics normalized and she was weaned from uncomplicated CPB. The patient was discharged to rehab on the 13th postoperative day.
Figure 1:
Panel (a) shows the angiographic check after valve deployment with prompt filling of the right coronary artery (black arrows) but sparse filling of the left coronary system (open arrows). Panel (b) shows the selective coronary angiography with the subtotal occlusion of the left main coronary artery (black arrow) after sternotomy with retractor in place and establishment of cardiopulmonary bypass.
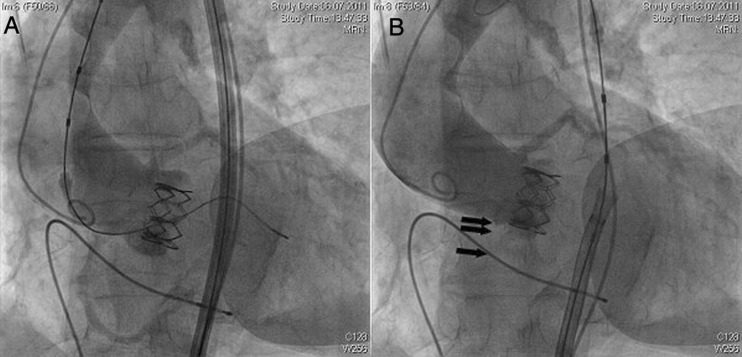
The second case was a symptomatic 85-year old lady with a logistic EuroSCORE of 23.8% who underwent transfemoral TAVI for severe AS. Balloon dilation of the native valve and deployment of a 23 mm Edwards SAPIEN XT prosthesis were uneventful. The aortography revealed no coronary obstruction but moderate aortic insufficiency (Fig. 2A). Therefore, a second balloon dilation of the valve was performed under rapid pacing. The final aortography showed trivial aortic insufficiency, excellent filling of the left coronary artery but occlusion of the RCA (Fig. 2B). There was severe ST-segment elevation on leads II, III and aVF. Haemodynamic status deteriorated slowly. Attempts to intubate the RCA failed with different guide catheters and the decision was made to perform emergency coronary artery bypass grafting (CABG) with CPB. On the 12th postoperative day, the patient was discharged to rehab.
Figure 2:
Panel (a) shows angiographic check after valve deployment with prompt coronary filling. Panel (b) shows angiographic check after second balloon dilation. Occlusion of the right coronary artery (black arrows) was obvious.
The third case was a symptomatic 80-year old male with a logistic EuroSCORE of 31% who underwent transapical TAVI for severe AS. Immediately after implantation of a 29 mm Edwards SAPIEN XT prosthesis, the patient became hypotensive. ST-segment elevations were noted on the inferior leads. The aortography revealed a competent aortic valve, but ostial occlusion of the RCA and prompt filling of the left coronary system. The haemodynamic status deteriorated rapidly and a brief period of CPR was necessary. Catheter manipulation alone led to reopening of the RCA without further obstruction. With restoration of blood flow, haemodynamic, wall motion and ECG normalized. The patient was discharged to rehab on the 14th postoperative day.
DISCUSSION
TAVI is a therapeutic option for patients with AS who are deemed not suitable for conventional aortic valve replacement. In recent years, this technique has been rapidly propagated for high-risk patients [4]. However, the incidence of severe complications is not insignificant. A life-threatening complication is coronary artery stenosis or occlusion with a reported incidence of 0.6–7% [5–7]. Rapid diagnosis and a staged management are mandatory. In our three cases, haemodynamic deterioration despite high doses of inotropic drugs accompanied by ECG changes typical for ischaemia was suspicious for coronary occlusion. In case 1, the necessary cardiac massage was not sufficient to support the perfusion of the body. Therefore, we did not hesitate to perform a sternotomy and supported the patient with CPB. Thereafter, we confirmed the diagnosis of subtotal left main occlusion by aortography and we were able to recover the left main. The other two cases had occlusion of the RCA. Both patients seemed to tolerate this condition with high doses of inotropic drugs. We went on to recover the RCA occlusion. In case 2, this was not possible. The next stage was to perform emergency CABG to restore myocardial blood supply.
Two reported cases of coronary occlusion [3, 8] and our cases showed that coronary blood flow restoration was life-saving. The staged treatment of this complication consisted of haemodynamic stabilization by inotropic drugs and if necessary CPB, and confirmation of diagnosis by aortography followed by percutaneous recanalization. If percutaneous recanalization was impossible, CABG was performed immediately.
Several conditions might predispose to coronary occlusion. A low-lying coronary ostium, bulky native leaflets, a narrow root, an excessively enlarged valve leaflet or the new valve prosthesis might result in coronary occlusion [9]. Therefore, we use angiographic visualization of the aortic root to position and slowly deploy the new valve. In all our cases, the distance from the basal leaflet insertion to the coronary ostium was >12 mm.
We conclude that haemodynamic instability of a patient after TAVI might be suspicious for coronary artery obstruction or occlusion. The only treatment option after diagnosis is immediate re-establishment of blood flow by percutaneous techniques or CABG. In some cases, a cardiopulmonary support is necessary. These cases highlight the need for a heart team involved not only in decision-making, but also in the procedure itself.
Conflict of interest: R.G.S. and W.S. are proctors for Edwards Lifesciences.
References
- 1.Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. PARTNER Trial Investigators. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187–98. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 2.Vahanian A, Alfieri OR, Al-Attar N, Antunes MJ, Bax J, Cormier B, et al. Transcatheter valve implantation for patients with aortic stenosis: a position statement from the European Association of Cardio-Thoracic Surgery (EACTS) and the European Society of Cardiology (ESC), in collaboration with the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur J Cardiothorac Surg. 2008;34:1–8. doi: 10.1016/j.ejcts.2008.04.039. [DOI] [PubMed] [Google Scholar]
- 3.Crimi G, Passerone G, Rubartelli P. Trans-apical aortic valve implantation complicated by left main occlusion. Catheter Cardiovasc Interv. 2011;78:656–9. doi: 10.1002/ccd.23026. [DOI] [PubMed] [Google Scholar]
- 4.Gummert JF, Funkat AK, Beckmann A, Ernst M, Hekmat K, Beyersdorf F, et al. Cardiac surgery in Germany during 2010: a report on behalf of the German Society for Thoracic and Cardiovascular Surgery. Thorac Cardiovasc Surg. 2011;59:259–67. doi: 10.1055/s-0030-1271191. [DOI] [PubMed] [Google Scholar]
- 5.Thomas M, Schymik G, Walther T, Himbert D, Lefèvre T, Treede H, et al. Thirty-day results of the SAPIEN aortic Bioprosthesis European Outcome (SOURCE) Registry: a European registry of transcatheter aortic valve implantation using the Edwards SAPIEN valve. Circulation. 2010;122:62–9. doi: 10.1161/CIRCULATIONAHA.109.907402. [DOI] [PubMed] [Google Scholar]
- 6.Rodés-Cabau J, Webb JG, Cheung A, Ye J, Dumont E, Feindel CM, et al. Transcatheter aortic valve implantation for the treatment of severe symptomatic aortic stenosis in patients at very high or prohibitive surgical risk: acute and late outcomes of the multicenter Canadian experience. J Am Coll Cardiol. 2010;55:1080–90. doi: 10.1016/j.jacc.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 7.Zierer A, Wimmer-Greinecker G, Martens S, Moritz A, Doss M. The transapical approach for aortic valve implantation. J Thorac Cardiovasc Surg. 2008;136:948–53. doi: 10.1016/j.jtcvs.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 8.Bartorelli AL, Andreini D, Sisillo E, Tamborini G, Fusari M, Biglioli P. Left main coronary artery occlusion after percutaneous aortic valve implantation. Ann Thorac Surg. 2010;89:953–5. doi: 10.1016/j.athoracsur.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 9.Webb JG. Coronary obstruction due to transcatheter valve implantation. Catheter Cardiovasc Interv. 2009;73:973. doi: 10.1002/ccd.22105. [DOI] [PubMed] [Google Scholar]