Abstract
Background
Despite the considerable impact of migraine, the use of preventive medication in primary care is limited. Only about 5% of migraine patients who qualify for prophylaxis actually receive it, and adherence is far from optimal.
Aim
To explore the opinions of GPs regarding preventive medication for migraine.
Design and setting
A qualitative focus group study in Dutch general practice.
Method
Four focus groups (six GPs each) were formed. GPs were purposively sampled to acquire a range of participants, reflecting the more general GP population.
Results
GPs perceived patients' concerns about the impact of migraine and the potential benefits of prophylaxis. However, some were hesitant to start prescribing prophylaxis due to doubts about effectiveness, potential side effects, and the risk of developing drug dependency. GPs' decisions were often based on considerations other than those presented in national guidelines, for example, the patient's need to control their own problem. Many GPs placed responsibility for initiating prophylaxis with the patient.
Conclusion
Various considerations hamper GPs from managing migraine with preventive medication, and various patient-related concerns cause GPs to deviate from national headache guidelines.
Keywords: general practice, headache, migraine disorders, physician-patient relations, primary health care, qualitative research, secondary prevention
INTRODUCTION
Migraine is a common and disabling brain disorder, and many patients with migraine have severe and debilitating attacks.1 Primary care is an important setting for the management of migraine; for example, in the Netherlands, 95% of triptans are prescribed in primary care.2
Prophylactic therapy is an option for patients with frequent or long-lasting migraine, where treatment can reduce attack frequency by 50% and also reduce attack severity.3–5 Suggested thresholds for starting prophylactic therapy range from attacks twice a month to twice a week.3,4,6 Dutch headache guidelines for GPs recommend discussing prophylactic therapy in patients who have (on average) at least two attacks each month.7 In Dutch general practice, beta-blockers are the most frequently prescribed preventive migraine medication, together with anti-epileptic drugs and other anti-hypertensive drugs.8
Preventive therapy is probably indicated in about one-third of patients with migraine, and a broad range of pharmaceutical and non-pharmaceutical options are available.1 However, despite the fact that prophylaxis is a safe and effective intervention,9–11 only 5–13% of patients with migraine who qualify for prophylaxis actually receive it.8,12 In many countries a substantial proportion of those who might benefit from prevention do not receive it.12,13 Moreover, the adherence to prophylaxis is modest.9 In addition, although many patients express a wish for prophylaxis (even for infrequent headache),14 GPs and patients are often reluctant to exploit its possibilities.14 Little is known about the opinions of GPs and patients regarding prophylaxis or about the considerations involved in making a decision about prophylaxis.
To reduce the unmet needs of patients with migraine, it is important to elucidate why GPs do not prescribe preventive medication and why many patients do not ask for it.14 Therefore, this study explores GPs' decision making regarding prophylactic migraine therapy.
METHOD
Recruitment
Because little is known about how GPs deal with preventive treatment of migraine and their underlying motivations, qualitative methods were used for this study. It was expected that, in a focus group, the GPs would prompt one another to a more profound discussion on preventive treatment than might occur during an individual interview.
The aim was to recruit a sample of GPs that reflects a mix of urban/rural practitioners with a range of age, experience, sex, and type and size of practice. ‘Theoretical sampling’ was used and it was expected that data saturation would be reached with three to four focus groups.15 GPs who appeared to have a special interest in headache were excluded. Four groups of GPs (two urban and two rural) were recruited. The GPs were targeted as existing regional groups and all the GPs of the four groups received (via e-mail) an invitation and an answer form.
How this fits in
Preventive treatment of migraine is a cost-effective intervention, generally using medication commonly used in primary care. However, GPs offer the intervention too infrequently, due to low expectations about its effectiveness, worries about side effects, or their perceived views on patients' wishes. Elucidating the underlying opinions and motivations of GPs may facilitate greater use of prophylactic drugs and a subsequent reduction in the burden of migraine.
Of the 32 invited GPs, 24 attended the focus group meetings, with (on average) six GPs per group. Their mean age was 48 years (range 31–59 years) and there were 10 females and 14 males. This distribution broadly reflects the Dutch situation.8,14 Of the 24 GPs, 11 worked in a group practice, 3 in a two-handed practice, and 10 in a single-handed practice. Of the 24 participating GPs, 18 had ≥10 years' experience and 22 worked full-time in general practice. Of all GPs, three experienced infrequent migraine themselves, and two experienced frequent migraine attacks.
Data generation
Each focus group meeting was chaired by an independent health scientist experienced in moderating headache focus groups. The moderator conducted the group meetings using an interview guide compiled by two of the researchers. To facilitate discussion, the themes ‘general attitudes towards migraine’ (such as feeling comfortable in consultations with patients with migraine),16 and ‘scenarios for treatment goals and prophylactic treatment’, were used, supported by a range of questions and statements. Each session lasted about 2 hours and was digitally recorded. The audiorecordings were transcribed.
Analysis
The recordings were analysed independently by three researchers. Because the DVD recordings provided the most detailed information on both verbal and non-verbal communication, these served as the primary data source.17–19 The researchers used regular DVD-reading software with good on-screen forward/backward and other search possibilities. The DVDs allowed both verbal and non-verbal indications to support an opinion given by others in the group.
The three investigators independently identified ‘themes’ on preventive treatment, emerging from the data. These themes were written in text form and then organised into categories and (sub-) themes according to the rules of thematic analysis.19–21 The subsequent draft analytical framework was discussed and decided upon with the other members of the team. In the case of disagreement between the researchers, the theme was analysed again by those involved; in the case of a persisting discrepancy, consensus was sought and reached between the researchers. Using this framework, an interpretative analysis of the data enabled identification of several related, but separate, topics of experience and reasoning regarding prophylactic treatment for migraine, and a tentative model to elucidate GPs' considerations regarding preventive migraine treatment.
RESULTS
Analysis of the data revealed six main themes, which are discussed in turn.
GPs' general views on migraine
In the present study, many GPs believed that even when acute treatment was optimal, patients with migraine with frequent attacks still had a ‘serious’ health problem. Of the 24 GPs, 17 stated that patients with migraine need as much attention as patients with, for example, chronic obstructive pulmonary disease (COPD) or diabetes, but patients with migraine did not receive any form of chronic disease monitoring:
‘Why is so little attention paid to migraine? We're expected to go along with the hype that diabetes is a really nasty disease, asthma is a really nasty disease, but with migraine we just have to accept the lack of attention for it.’ (group 3, GP 2)
However, a minority of GPs believed that the patient is to blame for the high attack frequency, or that the decision to consult the GP should be left to the patient without actively offering follow-up.
GPs felt positive about patients with migraine and their search for help, valued migraine consultations because they challenged their knowledge, believed that migraine is a treatable disease, and regarded their own treatment as sufficiently patient centred. Those GPs with migraine themselves (at least one in each focus group) claimed a greater understanding of the significance of the impact of migraine. Almost all GPs were able to describe the patients' (or recall exceptional) stories about the severity of migraine attacks.
Reluctance to start prescribing prophylaxis
GPs frequently mentioned that patients were reluctant to take medication for preventive purposes, even when they understood its benefit. Many GPs found that the disadvantages often outweigh the benefits of preventive therapy. For example, four GPs were concerned about the ‘medicalising’ effects of preventing migraine, or thought that the patient's concerns about this hampered the initiation of prevention:
‘With migraine there's a price to pay every single day for effective prevention, it's the same with epilepsy.’ (group 2, GP 4)
‘In my estimation, about half of the patients who qualify for prophylaxis don't really want it.’ (group 1, GP 6)
GPs believed that patients did take any downside of preventive treatment into account, such as adverse reactions and drug dependency. GPs said that they often heard from patients about their fear of drug dependency. These downsides of medication could make patients less positive toward preventive therapy. GPs understood and accepted this reluctance; this sometimes made them unwilling to initiate treatment and/or convince the patient about the benefits of prophylaxis:
‘Whenever I offer prophylaxis for migraine I feel as though I'm adding another problem to the patient's already existing health problems.’ (group 4, GP 1)
‘Patients see prophylaxis as a heavy form of therapy — that's the way they experience it. And that's an important reason to decline prophylactic treatment.’ (group 4, GP 4)
‘In the case of prophylaxis, patients receive a huge leaflet full of instructions and warnings — this means that the medication prescribed by GPs is a serious matter.’ (group 4, GP 4)
Second, GPs felt that when patients used a lot of medication to treat acute attacks, the patients would sometimes be more reluctant to consider further/more medication, even when it was for prevention purposes. Third, GPs thought that patients had many concerns about the side effects of prophylaxis; on this topic, GPs thought they shared the concerns with their patients:
‘In the case of migraine, the side effects of beta-blockers weigh much more heavily [compared with hypertension].’ (group 2, GP 5)
Although some GPs were pessimistic about changing the health behaviour of patients with migraine, the majority believed that when the goals and benefits of preventive therapy were adequately explained, it should be possible to reduce the burden of migraine:
‘The unpredictability of the attacks makes migraine a serious problem; you can't ignore that … and as a doctor you have to do something about it.’ (group 2, GP 4)
Initiating prophylactic medication
A recurring theme was that the trigger to initiate prophylaxis was not a simple sum of migraine frequency plus duration. If acute attacks are treated successfully, patients are less likely to ask for other types of migraine treatment. However, in the GPs' opinion, many patients experienced insufficient relief from acute medication, whether or not prescribed by a specialist. GPs believed that patients often did not realise that their care was less than optimal:
‘You often hear: “I'm satisfied, I don't need daily treatment myself”.’ (group 2, GP 3)
‘Migraine patients come to the GP's office only for that “stronger” cure that they really hope is available.’ (group 2, GP 2)
GPs found that the threshold to instigate preventive medication in migraine was less clear than in other diseases, such as asthma. However, in migraine, two factors were important. First, the patient's feelings of being in control of the headache played an important role in determining whether they were satisfied with their therapy, a goal that was not always achieved with acute treatment only. Second, the functional impact on regular activities (work, school, and so on) was also important. About 50% of the GPs reported that if they, personally, experienced two or more attacks each month, they would accept preventive treatment.
Taking the initiative for prophylaxis — patient or physician?
GPs felt reluctant to initiate or explore prophylactic treatment for some patients, even when they noticed a high frequency of migraine attacks. Generally, they responded to questions or cues coming from the patient. An important cue was when the patient expressed that they were unable to cope with their migraine. Some GPs (especially those who monitored attack medication) noticed the need for prophylaxis at an earlier stage, for example, in the case of an excessive use of triptans.
The approachability of the physician was considered to be an important factor in exploring or initiating preventive medication:
‘If a GP is open and approachable, then it's also the patient's responsibility whether or not to start taking prophylactic treatment. Patients don't need to be assertive when the doctor is approachable.’ (group 3, GP 2)
GPs acknowledged the impact of medication overuse and its importance as a marker for possible preventive therapy. However, it was felt that this was an area that was not well recognised:
‘When practice assistants identify triptan overuse, this is a clear warning that the patient needs preventive treatment.’ (group 1, GP 4)
When patients asked about preventive treatments, the GPs were of the opinion that they had already explored other therapies, including dietary approaches and complementary therapies. GPs considered it important to offer prophylaxis at the most appropriate moment. This was not necessarily the moment of diagnosis, and was influenced by patients' realisation of the impact of the problem:
‘When considering prophylaxis, you have to choose the right moment to present this option to the patient.’ (group 2, GP 1)
Starting prescribing and managing prophylaxis
GPs felt that their role differed from that of specialists, for example, they differed in their motives for starting prophylaxis and its management. GPs were of the opinion that specialists simply carried out their protocols (often personal protocols), whereas GPs also took comorbidity and other health-related circumstances into account, and GPs thought they gave more notice to the complexity of the context in which prescribing took place:
‘If migraine is combined with some other diseases, then you're much more likely to give a beta-blocker [when indicated].’ (group 3, GP 4)
‘When you think about the individual tailoring of prophylaxis, GPs handle a lot more comorbidity than specialists.’ (group 3, GP 5)
‘Migraine therapy actually involves quite a lot of creativity.’ (group 4, GP 3)
‘Migraine management is more a medical art than just medicine itself.’ (group 2, GP 1)
There was no consensus among GPs as to how to manage prophylaxis. Some scheduled regular appointments, whereas others had contact only at the start of prophylaxis and considered the patients to be responsible for their own subsequent treatment:
‘If the aim of the prophylaxis is achieved, your patients don't come back again. If you compare migraine to diseases like asthma, the control policy is much more structured in those other diseases.’ (group 2, GP 2)
‘Because starting preventive treatment is generally at the patient's wish, then the moment to stop should also be the patient's decision — I can accept that.’ (group 4, GP 4)
For participating GPs, the first choice for prophylactic therapy was beta-blockers, and about 50% of the GPs thought that the use of beta-blockers would result in an additional cardiovascular health benefit. Less than 25% prescribed anti-epileptic medication. GPs reported that they were honest and open-minded with their patients about the claims made for prophylaxis in relation to the frequency and reduction in severity of attacks. Non-compliance was seen as a common problem, but the GPs were not particularly worried about this.
Expectations of the benefit of prophylaxis
GPs differed in their expectations regarding benefit. Some suggested that prophylaxis should make migraine disappear, some accepted the evidence-based expectation of a 50% reduction in attack frequency and attack severity, and others had a low expectation because of lack of efficacy or because of patients' reluctance to accept regular medication. This low expectation was reflected in a reluctance to instigate prophylactic treatment:
‘The ultimate aim of prophylactic therapy (“to be free of migraine attacks”) can never really be reached.’ (group 1, GP 6)
‘Sometimes it's very difficult to give prophylaxis, especially when the patients keep coming back without good results.’ (group 4, GP 3)
‘If a patient has suffered from migraine for the past 30 years, then he'll also suffer for the next 30 years.’ (group 3, GP 2)
‘Even after preventive treatment, you don't leave the surgery whistling, you know that you're still in deep water.’ (group 1, GP 4)
GPs felt that patients also differed in their appreciation of the benefits of prophylaxis. In the perception of GPs, some patients were satisfied with only small benefits, while others expected total resolution of their headache. If patients had a long history of migraine, small benefits were often welcome. GPs emphasised that there is no gold standard or endpoint for measuring the effects of prophylaxis in the individual patient.
DISCUSSION
Summary
When considering preventive treatment for migraine, GPs related several facilitating and inhibiting factors influencing their actions (Figure 1). GPs understood their patient's concerns about the impact of migraine. Although the benefits of prophylaxis were appreciated, they were hesitant about advising their patients, not because of lack of knowledge or lack of interest, but because of doubts about its effectiveness, and fear of side effects.
Figure 1.
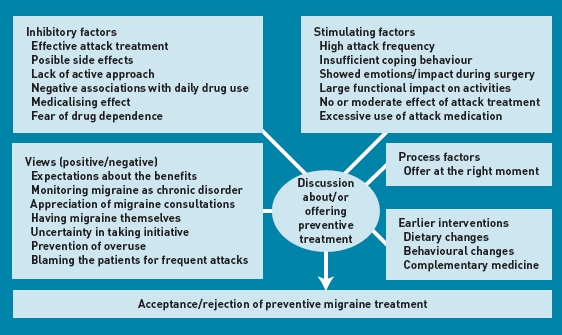
GP considerations and arguments for and against preventive therapy.
It is not a simple matter to decide whether GPs sufficiently comply with the current guideline on headache. In the Netherlands, most GPs generally tend to comply with their guidelines.22 However, in the present study the responders deviate from the guidelines on the above-mentioned points, indicating that for GPs prophylaxis is not simply induced by multiplying duration by frequency. Other guidelines also tend to neglect the above-mentioned factors when discussing the decision whether or not to start preventive treatment.12,23–29 Some guidelines refer to the patient's wishes or preferences;12,23,27 however, even when these are mentioned, they are not further specified.
Another difference between the actions of the GPs in this study and the Dutch GP guideline7 involves taking the initiative for prophylaxis. On this issue some GPs were much more reluctant than advised in the guideline, because they felt that the responsibility for initiating prophylaxis should lie with the patient. Therefore, prophylaxis was not always promoted in an active way; this finding warrants further exploration.
A parallel study on patients with migraine shows that some elements in the decision-making process are similar between GPs and patients, whereas differences also occur.30 For example, GPs more often mention the inability to cope with migraine attacks as a reason to start taking preventive treatment. It would be worthwhile to further quantify these differences between GPs and patients.
GPs indicated that they are more respectful of other patient-related conditions and comorbidity than specialists. Contextual factors have a large influence on medical care as delivered by GPs. Further exploration of differences between GPs and specialists in the consideration of contextual factors needs further research.31
Most GPs show realistic expectations, although in each focus group one or two were pessimistic. This might be due to the discrepancy between the ‘ideal’ of a total relief of migraine in contrast to a sometimes moderate or absent effect in actual practice. Because GPs and/or patients often have a too-positive vision of prevention in advance, it is important to discuss this issue in postgraduate training and patient education.
In the present study, the GPs expressed a fear regarding drug dependency, but it is unclear whether they were referring to fear of actual addiction, such as with benzodiazepines. Also, the GPs seemed to refer to a broader negative association with the daily use of medication, such as when patients use (too) many drugs.
GPs occasionally felt that patients were suggesting that they did not take migraine seriously. The GPs did not agree with this and sincerely believed that they always paid adequate attention to migraine headaches. The patients were told to be aware that, even with optimal attack treatment, patients with migraine with frequent attacks had a ‘serious’ health problem. GPs' approach to migraine as a health problem was not different from other diseases and some GPs regarded headache as an interesting problem because it challenges their own knowledge and skills. The lack of regular follow-up was seen as being unlike other chronic conditions in which preventive medication is used.
Strengths and limitations
Although the composition of the focus groups broadly reflects the characteristics of GPs in the Netherlands, the study GP group may have reflected those with a particular interest in headache. In the fourth focus group, no new themes or additional information on those themes were raised, so it is unlikely that any important themes were missed.
A weakness of the study was that all meetings were conducted in the Dutch language and are reported here in English. Qualitative studies aim to capture meaning from the narrative of the responders and some distortion may have occurred in the translation process. The text was corrected by two native English speakers, with the Dutch text at hand, and verified by a physician headache expert.
Comparison with existing studies
Although migraine has a complex biopsychosocial context, few qualitative studies on this topic are available. Reports have included patients' perceptions of migraine and chronic daily headache,32,33 the needs of patients with migraine,34,35 migraine-related decision making,36–38 the burden of migraine and impact on quality-of-life,39,40 patients' experience, and the expectations of management.16,41,42 One of these latter studies addressed prophylaxis,42 but the setting was a specialised care clinic and the study aim was different from that of the present study. The latter study focuses on whether the physician involves the patient in choosing a preventive agent when the decision to start this was already made, not on the decision making in starting preventive therapy as in the present study. A questionnaire study provided information on the extent to which patients accept the side effects of preventive treatment, which is consistent with the findings in the present study.43 Another study addressed how GPs treated themselves and close relatives;44 one study explored physicians' understanding of patients with migraine;45 and another study reports clinical determinants of preventive therapy in primary care.46
Implications for practice and research
Appropriate prophylaxis is an important factor in the aim to improve the quality of care of patients with migraine by reducing attack frequency and duration, improving functioning and productivity, reducing use of acute medication, and preventing medication overuse. The present study has elucidated some factors that prevent GPs from adequately managing migraine from this perspective, and might inform the development of educational strategies to improve migraine prophylaxis in general practice. The results also highlight the difficulties GPs experience in translating guidelines into practice and the need to develop guidelines that realistically reflect the context in which they are applied.
These factors should be addressed in guideline setting and postgraduate education. Finally, some aspects of the findings of this study need further exploration, and some deserve quantification.
Acknowledgments
The authors thank JAG Muller, MSc, moderator, and all participating GPs for their cooperation.
Funding
The study received no external funding.
Ethical approval
This study was approved by the Medical Ethical Committee of the Leiden University Medical Center, Leiden, the Netherlands.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Michel D Ferrari has received unrestricted research grants from, or served as a consultant to, Almirall Prodesfarma, AstraZeneca, Glaxo SmithKline, Merck, Pfizer, Menarini, Johnson & Johnson, and Pharmacia. David Kernick has acted in an advisory capacity to MSD and AstraZeneca. Frans Dekker has received an unrestricted research grant from Janssen-Cilag, with no relation to the present study. All other authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Goadsby PJ, Sprenger T. Current practice and future directions in the prevention and acute management of migraine. Lancet Neurol. 2010;9(3):285–298. doi: 10.1016/S1474-4422(10)70005-3. [DOI] [PubMed] [Google Scholar]
- 2.Dekker F, Wiendels N, de Valk V, et al. Triptan overuse in the Dutch general population: a nationwide pharmaco-epidemiology database analysis in 6.7 million people. Cephalalgia. 2011;31(8):943–952. doi: 10.1177/0333102411408626. [DOI] [PubMed] [Google Scholar]
- 3.D'Amico D, Solari A, Usai S, et al. Improvement in quality of life and activity limitations in migraine patients after prophylaxis. A prospective longitudinal multicentre study. Cephalalgia. 2006;26(6):691–696. doi: 10.1111/j.1468-2982.2005.01094.x. [DOI] [PubMed] [Google Scholar]
- 4.Ramadan NM, Schultz LL, Gilkey SJ. Migraine prophylactic drugs: proof of efficacy, utilization and cost. Cephalalgia. 1997;17(2):73–80. doi: 10.1046/j.1468-2982.1997.1702073.x. [DOI] [PubMed] [Google Scholar]
- 5.Silberstein SD, Winner PK, Chmiel JJ. Migraine preventive medication reduces resource utilization. Headache. 2003;43(3):171–178. doi: 10.1046/j.1526-4610.2003.03040.x. [DOI] [PubMed] [Google Scholar]
- 6.Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalalgia. 2002;22(7):491–512. doi: 10.1046/j.1468-2982.2002.00386.x. [DOI] [PubMed] [Google Scholar]
- 7.Grol MH, Neven AK, Pijnenborg L, Goudswaard AN. [Summary of the practice guideline ‘Headache’ from the Dutch College of General Practitioners] Ned Tijdschr Geneeskd. 2006;150(6):305–309. [PubMed] [Google Scholar]
- 8.Rahimtoola H, Buurma H, Tijssen CC, et al. Incidence and determinants of migraine prophylactic medication in the Netherlands. Eur J Clin Pharmacol. 2002;58(2):149–155. doi: 10.1007/s00228-002-0443-8. [DOI] [PubMed] [Google Scholar]
- 9.Linde M, Jonsson P, Hedenrud T. Influence of disease features on adherence to prophylactic migraine medication. Acta Neurol Scand. 2008;118(6):367–372. doi: 10.1111/j.1600-0404.2008.01042.x. [DOI] [PubMed] [Google Scholar]
- 10.Mulleners WM, Chronicle EP. Anticonvulsants in migraine prophylaxis: a Cochrane review. Cephalalgia. 2008;28(6):585–597. doi: 10.1111/j.1468-2982.2008.01571.x. [DOI] [PubMed] [Google Scholar]
- 11.Victor S, Ryan SW. Drugs for preventing migraine headaches in children. Cochrane Database Syst Rev. 2003;4:CD002761. doi: 10.1002/14651858.CD002761. [DOI] [PubMed] [Google Scholar]
- 12.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 13.Cevoli S, D'Amico D, Martelletti P, et al. Underdiagnosis and undertreatment of migraine in Italy: a survey of patients attending for the first time 10 headache centres. Cephalalgia. 2009;29(12):1285–1293. doi: 10.1111/j.1468-2982.2009.01874.x. [DOI] [PubMed] [Google Scholar]
- 14.Kol CM, Dekker F, Neven AK, et al. Acceptance or rejection of prophylactic medicine in patients with migraine: a cross-sectional study. Br J Gen Pract. 2008;58(547):98–101. doi: 10.3399/bjgp08X264063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008;337:a1035. doi: 10.1136/bmj.a1035. [DOI] [PubMed] [Google Scholar]
- 16.Morgan M, Jenkins L, Ridsdale L. Patient pressure for referral for headache: a qualitative study of GPs' referral behaviour. Br J Gen Pract. 2007;57(534):29–35. [PMC free article] [PubMed] [Google Scholar]
- 17.Heath C, Hindmarsh J, Luff P. Video in qualitative research. London: Sage Publications; 2010. [Google Scholar]
- 18.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joffe H, Yardley L. Content and thematic analysis. In: Marks DF, Yardley L, editors. Research methods for clinical and health psychology. London: Sage Publications; 2003. pp. 56–68. [Google Scholar]
- 21.Chamberlain K, Camic P, Yardley L. Qualitative analysis of experience: grounded theory and case studies. In: Marks DF, Yardley L, editors. Research methods for clinical and health psychology. London: Sage Publications; 2003. pp. 69–89. [Google Scholar]
- 22.Lugtenberg M, Burgers JS, Westert GP. Effects of evidence-based clinical practice guidelines on quality of care: a systematic review. Qual Saf Health Care. 2009;18(5):385–392. doi: 10.1136/qshc.2008.028043. [DOI] [PubMed] [Google Scholar]
- 23.D'Amico D, Tepper SJ. Prophylaxis of migraine: general principles and patient acceptance. Neuropsychiatr Dis Treat. 2008;4(6):1155–1167. doi: 10.2147/ndt.s3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dowson AJ, Lipscombe S, Sender J, et al. New guidelines for the management of migraine in primary care. Curr Med Res Opin. 2002;18(7):414–439. doi: 10.1185/030079902125001164. [DOI] [PubMed] [Google Scholar]
- 25.Evers S, Afra J, Frese A, et al. EFNS guideline on the drug treatment of migraine — report of an EFNS task force. Eur J Neurol. 2006;13(6):560–572. doi: 10.1111/j.1468-1331.2006.01411.x. [DOI] [PubMed] [Google Scholar]
- 26.Lewis D, Ashwal S, Hershey A, et al. Practice parameter: pharmacological treatment of migraine headache in children and adolescents: report of the American Academy of Neurology Quality Standards Subcommittee and the Practice Committee of the Child Neurology Society. Neurology. 2004;63(12):2215–2224. doi: 10.1212/01.wnl.0000147332.41993.90. [DOI] [PubMed] [Google Scholar]
- 27.Modi S, Lowder DM. Medications for migraine prophylaxis. Am Fam Physician. 2006;73(1):72–78. [PubMed] [Google Scholar]
- 28.Pryse-Phillips WE, Dodick DW, Edmeads JG, et al. Guidelines for the diagnosis and management of migraine in clinical practice. Canadian Headache Society. CMAJ. 1997;156(9):1273–1287. [PMC free article] [PubMed] [Google Scholar]
- 29.Tepper SJ, D'Amico D, Baos V, et al. Guidelines for prescribing prophylactic medications for migraine: a survey among headache specialist physicians in different countries. Headache Care. 2004;1(4):267–272. [Google Scholar]
- 30.Dekker F, Knuistingh Neven A, Andriesse B, et al. Prophylactic treatment of migraine; the patient's view, a qualitative study. BMC Fam Pract. 2012 doi: 10.1186/1471-2296-13-13. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiner SJ, Schwartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med. 2010;153(2):69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 32.Peters M, Abu-Saad HH, Vydelingum V, et al. Migraine and chronic daily headache management: a qualitative study of patients' perceptions. Scand J Caring Sci. 2004;18(3):294–303. doi: 10.1111/j.1471-6712.2004.00279.x. [DOI] [PubMed] [Google Scholar]
- 33.Peters M, Huijer Abu-Saad H, Vydelingum V, et al. The patients' perceptions of migraine and chronic daily headache: a qualitative study. J Headache Pain. 2005;6(1):40–47. doi: 10.1007/s10194-005-0144-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belam J, Harris G, Kernick D, et al. A qualitative study of migraine involving patient researchers. Br J Gen Pract. 2005;55(511):87–93. [PMC free article] [PubMed] [Google Scholar]
- 35.Cottrell CK, Drew JB, Waller SE, et al. Perceptions and needs of patients with migraine: a focus group study. J Fam Pract. 2002;51(2):142–147. [PMC free article] [PubMed] [Google Scholar]
- 36.Peters M, Abu-Saad HH, Vydelingum V, et al. Patients' decision-making for migraine and chronic daily headache management. A qualitative study. Cephalalgia. 2003;23(8):833–841. doi: 10.1046/j.1468-2982.2003.00590.x. [DOI] [PubMed] [Google Scholar]
- 37.Ivers H, McGrath PJ, Purdy RA, et al. Decision making in migraine patients taking sumatriptan: an exploratory study. Headache. 2000;40(2):129–136. doi: 10.1046/j.1526-4610.2000.00018.x. [DOI] [PubMed] [Google Scholar]
- 38.Meyer GA. The art of watching out: vigilance in women who have migraine headaches. Qual Health Res. 2002;12(9):1220–1234. doi: 10.1177/1049732302238246. [DOI] [PubMed] [Google Scholar]
- 39.Tenhunen K, Elander J. A qualitative analysis of psychological processes mediating quality of life impairments in chronic daily headache. J Health Psychol. 2005;10(3):397–407. doi: 10.1177/1359105305051425. [DOI] [PubMed] [Google Scholar]
- 40.Ruiz de Velasco I, González N, Etxeberria Y, Garcia-Monco JC. Quality of life in migraine patients: a qualitative study. Cephalalgia. 2003;23(9):892–900. doi: 10.1046/j.1468-2982.2003.00599.x. [DOI] [PubMed] [Google Scholar]
- 41.Moloney MF, Strickland OL, DeRossett SE, et al. The experiences of midlife women with migraines. J Nurs Scholarsh. 2006;38(3):278–285. doi: 10.1111/j.1547-5069.2006.00114.x. [DOI] [PubMed] [Google Scholar]
- 42.Rozen TD. Migraine prevention: what patients want from medication and their physicians (a headache specialty clinic perspective) Headache. 2006;46(5):750–753. doi: 10.1111/j.1526-4610.2006.00429.x. [DOI] [PubMed] [Google Scholar]
- 43.Kowacs PA, Piovesan EJ, Tepper SJ. Rejection and acceptance of possible side effects of migraine prophylactic drugs. Headache. 2009;49(7):1022–1027. doi: 10.1111/j.1526-4610.2009.01431.x. [DOI] [PubMed] [Google Scholar]
- 44.Ducros A, Romatet S, Saint MT, Allaf B. Use of antimigraine treatments by general practitioners. Headache. 2011;51(7):1122–1131. doi: 10.1111/j.1526-4610.2011.01939.x. [DOI] [PubMed] [Google Scholar]
- 45.Lipton RB, Stewart WF. Acute migraine therapy: do doctors understand what patients with migraine want from therapy? Headache. 1999;39(suppl 2):S20–S26. [Google Scholar]
- 46.Valade D, Lanteri-Minet M, Radat F, et al. Clinical determinants of migraine preventive treatment: contribution of SMILE, an observational survey of primary care migraine management in France. Cephalalgia. 2010;30(10):1207–1213. doi: 10.1177/0333102409355661. [DOI] [PubMed] [Google Scholar]


