Abstract
We report 20 episodes of infection caused by acquired echinocandin-resistant Candida spp. harboring diverse and new Fksp mutations. For 12 patients, initial isolates (low MIC, wild-type Fksp sequence) and subsequent isolates (after caspofungin treatment, high MIC, mutated Fksp) were genetically related.
Keywords: caspofungin, echinocandins, FKS mutation, Candida albicans, Candida glabrata, Candida krusei, treatment failure, clinical isolates, genotyping, drug resistance, fungi, France
Echinocandins are effective in patients with invasive candidiasis and recommended as first-line therapy, especially for patients with severe sepsis or those previously exposed to azoles or infected with Candida glabrata (1). Fewer than 50 persons infected with echinocandin-resistant species that are usually susceptible, such as C. albicans, C. glabrata, C. tropicalis, and C. krusei, have been described in limited series or case reports (2–4). All species were found in patients preexposed to echinocandins. The major mechanism of resistance is related to mutations in FKS genes coding for β-1,3-glucan-synthase (5), with almost 20 known FKS mutations. We describe the characteristics of infections from caspofungin-resistant Candida spp. isolates belonging to usually susceptible species recorded in France (2004–2010) and analyze their FKS mutations and effect on echinocandin susceptibility.
The Study
Isolates received at the French National Reference Center for Mycoses and Antifungals (NRCMA) are identified to the species level by standard mycologic procedures and routinely tested for susceptibility to caspofungin, micafungin, and anidulafungin by using European Committee for Antimicrobial Susceptibility Testing (EUCAST) methods (6) and AM3 medium (7). In addition, RPMI 1640 medium was used here for selected isolates and reference strains. For the clinical isolates with caspofungin MIC >0.5 µg/mL in AM3, nucleotide sequences of hot spot (HS) 1 and 2 regions of the FKS1 gene for C. albicans and C. krusei and of HS1 region of FKS1, FKS2, and FKS3 genes for C. glabrata were determined (7,8).
The resulting protein sequences were aligned with the BioloMics software (BioloMics, BioAware SA, Hannut, Belgium) and compared with reference strains (C. albicans, ATCC32354; C. krusei, ATCC6258; and C. glabrata, ATCC2001). Genetic relatedness of C. albicans and C. glabrata paired isolates was studied by using microsatellite-length polymorphism analysis (9–11). The Wilcoxon signed-rank test was used to compare echinocandin MICs of paired isolates. Surveillance for mycoses by the NRCMA has been approved by the Institut Pasteur Internal Review Board and by the Commission Nationale de l’Informatique et des Libertés.
During September 2004–April 2010, twenty proven infections caused by C. albicans (n = 10), C. glabrata (n = 8), or C. krusei (n = 2) with caspofungin MIC >0.5 µg/mL and a mutation in the target enzyme were reported to the NRCMA (Table 1). Nineteen of the isolates were recovered after caspofungin treatment for a median duration of 27 days (range 10–270 days; 13 of 19 patients received caspofungin at the time the resistant isolate was recovered). Caspofungin was prescribed for 14 patients with proven Candida spp. infection, 1 patient with proven invasive aspergillosis, and 2 patients with febrile neutropenia; for 2 persons with hematologic malignancies, caspofungin was prescribed prophylactically.
Table 1. Characteristics of 20 patients with infections caused by a non–parapsilosis/guilliermondii Candida spp. Fks mutation, France, 2004–2010*.
| Patient no. | Age, y/sex | Underlying condition | Neutropenia | Species | Site of infection | Duration of caspofungin exposure, d† | Outcome at 30 d‡ |
|---|---|---|---|---|---|---|---|
| 1 | 34/M | HIV positive | No | C. albicans | Esophagus | 21 | Alive |
| 2 | 20/M | Hematologic malignancy: familial lymphohistiocytosis | Yes | C. albicans | Blood | 17 | Dead |
| 3 | 77/M | Hematologic malignancy: AML | Yes | C. albicans | Blood | 25 | Alive |
| 4 | 46/M | Hematologic malignancy: AML | Yes | C. albicans | Blood, peritoneum, pleural fluid | 26 | Dead |
| 5 | 34/F | Liver transplant: cirrhosis | No | C. albicans | Hepatic abscess, peritoneum | 60 | Alive |
| 6 | 64/F | Hematologic malignancy: AML; breast cancer | No | C. albicans | Blood | 25 | Alive at 17 d |
| 7 | 59/M | Teratocarcinoma | No | C. albicans | Pharynx | 35 | Dead |
| 8 | 28/M | Chronic mucocutaneous candidiasis | No | C. albicans | Pharynx, nails | 270 | Alive |
| 9 | 14/F | Hematologic malignancy: ALL | Yes | C. krusei | Lung | 45 | Alive |
| 10 | 79/M | Hematologic malignancy: non-Hodgkin lymphoma | Yes | C. krusei | Blood | 10 | Dead |
| 11 | 46/M | Hematologic malignancy: Burkitt lymphoma; HSCT | Yes | C. glabrata | Blood | None | Dead |
| 12 | 85/M | Gastric ulcer; CVC | No | C. glabrata | Blood | 32 | Alive |
| 13 | 28/M | Hematologic malignancy: non-Hodgkin lymphoma; HSCT | No | C. glabrata | Palate§ | 135 | Alive |
| 14 | 48/M | Esophageal cancer | No | C. glabrata | Blood | 12 | Alive |
| 15 | 41/M | Liver transplant: fulminant hepatitis | No | C. glabrata | Blood, peritoneum | 37 | Dead |
| 16 | 38/F | Hematologic malignancy; AML; HSCT | Yes | C. glabrata | Blood | 51 | Dead |
| 17 | 60/M | Acute pancreatitis; GI tract surgery | No | C. glabrata | Bile | 34 | Alive |
| 18 | 39/M | Hematologic malignancy: AML; HSCT | No | C. glabrata | Sinus§ | 15 | Alive |
| 19 | 55/F | Lock-in syndrome; neurogenic bladder | No | C. glabrata | Urine¶ | 27 | Alive |
| 20 | 63/M | Colon cancer | Yes | C. glabrata | Blood | 14 | Alive |
*AML, acute myelogenous leukemia; ALL, acute lymphoblastic leukemia; HSCT, hematopoietic stem cell transplantation; CVC, central venous catheter; GI, gastrointestinal. †Duration of caspofungin exposure before isolation of the first resistant Candida isolate. ‡Outcome 30 d after isolation of the first resistant Candida isolate. §From a biopsy specimen. ¶With sepsis.
The geometric mean MIC for C. glabrata and C. albicans were 2.8 and 1.7 µg/mL for caspofungin, 0.4 and 0.7 µg/mL for micafungin, and 0.2 and 0.09 µg/mL for anidulafungin, respectively (Table 2). Of the 20 mutated isolates found resistant to caspofungin in AM3 by using the EUCAST method, 19 also were resistant to caspofungin (1 intermediate), 18 to micafungin (1 intermediate and 1 susceptible), and 9 to anidulafungin (5 intermediate and 6 susceptible) according to Clinical Laboratory Standards Institute (CLSI) breakpoints and RPMI 1640 medium (Table 2). According to EUCAST breakpoints, 19 isolates also were resistant to anidulafungin, and 1 isolate was almost resistant (MIC 0.03 µg/mL). We thus showed discrepancies between CLSI and EUCAST regarding anidulafungin susceptibility (www.srga.org/eucastwt/MICTAB/EUCAST%20clinical%20MIC%20breakpoints%20-%20antimicrobials%20for%20Candida%20infections.htm [V 3.0 2011–4-27]) (12,13).
Table 2. In vitro susceptibility and Fksp mutations of 20 echinocandin-resistant Candida spp. isolates, France, 2004–2010.
| Patient no. |
Strain |
Species |
MIC, µg/m, AM3/RPMI 1640 medium |
|
Fksp mutation | |||
|---|---|---|---|---|---|---|---|---|
| Caspofungin |
Micafungin |
Anidulafungin |
Gene |
Mutation |
||||
| 1* | 05BL1-38 | C. albicans | 1/2 | 0.25/1 | 0.06/0.125 | FKS1 (HS1) | F641S | |
| 2* | ODL13-1254 | C. albicans | 1/2 | 1/1 | 0.5/0.5 | FKS1 (HS1) | S645Y | |
| 3† | 06BL2-127 | C. albicans | 2/2 | 1/0.5 | 0.125/0.125 | FKS1 (HS1) | F641S‡ + S645P‡ | |
| 4 | ODL19-1894 | C. albicans | 4/2 | 2/2 | 0.125/0.25 | FKS1 (HS1) | S645P | |
| 5* | 08BL1-94 | C. albicans | 2/4 | 0.25/1 | 0.06/0.5 | FKS1 (HS2) | R1361G§ | |
| 6* | 08BL2-143 | C. albicans | 8/4 | 4/2 | 0.25/0.5 | FKS1 (HS1) | S645P | |
| 7* | 09BL1-43 | C. albicans | 1/2 | 0.25/1 | 0.06/0.25 | FKS1 (HS1) | F641S | |
| 8* | 09BL1-77 | C. albicans | 0.5/0.5 | 0.5/0.25 | 0.015/0.03 | FKS1 (HS1) | R647G§ | |
| 9 | 06BL1-34 | C. krusei | 4/8 | 2/4 | 1/2 | FKS1 (HS1) | L648W§,¶ | |
| 10* | 10BL1-50 | C. krusei | 2/4 | 1/2 | 0.06/1 | FKS1 (HS1) | F645L§,¶ | |
| 11 | ODL7-647 | C. glabrata | 8/8 | 0.5/1 | 0.25/0.125 | FKS2 | DelF658# | |
| 12* | 07BL2-157 | C. glabrata | 4/1 | 1/0.5 | 0.25/0.5 | FKS2 | DelF658# | |
| 13* | 06BL1-33 | C. glabrata | 8/8 | 4/8 | 2/2 | FKS2 | S663P | |
| 14* | ODL21-2028 | C. glabrata | 1/1 | 0.25/0.25 | 0.25/0.25 | FKS1 | S629P | |
| 15* | ODL22-2183 | C. glabrata | 8/2 | 0.25/0.25 | 0.25/1 | FKS2 | S663P | |
| 16 | ODL23-2221 | C. glabrata | 1/4 | 0.06/2 | 0.06/0.25 | FKS1 + FKS2 | F625I§ (FKS1) + P667T§ (FKS2) | |
| 17* | 08BL2-142 | C. glabrata | 1/4 | 0.25/2 | 0.25/2 | FKS2 | S663P | |
| 18 | 09BL1-55 | C. glabrata | 8/4 | 2/4 | 0.5/0.5 | FKS2 | S663P | |
| 19 | 10BL1-19 | C. glabrata | 0.5/4 | 0.06/0.5 | 0.06/1 | FKS2 | F659S + L664V§ | |
| 20 | 10BL1-67 | C. glabrata | 4/4 | 0.5/1 | 0.125/1 | FKS2 | DelF658# | |
*Parentage of initial isolate available. †In this patient, another isolate with reduced susceptibility to echinocandin was retrieved. This isolate harbored an S645P mutation in FKS1. ‡Heterozygous mutation. §Mutations not already described (13). ¶Strains had also an L701M mutation. #Deletion.
Of the 10 caspofungin-resistant C. glabrata isolates, 8 harbored a mutation in Fks2p only, 1 isolate had a mutation in Fks1p, and 1 had mutations in Fks1p and Fks2p (Table 2). Of the 8 caspofungin-resistant C. albicans isolates, 1 had a missense mutation in HS2, and 1 had a combination of 2 heterozygous mutations in HS1. The other 6 isolates harbored 4 different mutations in HS1 (Table 2). Finally, the 2 C. krusei isolates had 2 different mutations in HS1 region. Of the 20 mutated isolates, 6 harbored 7 mutations not yet described in the literature (Table 2) (13).
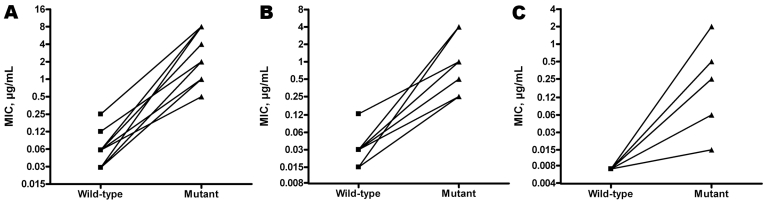
Prior initial isolates available for 12 patients had the wild-type sequence for the HS regions that were mutated in the paired resistant isolate. All initial isolates were susceptible to anidulafungin and to micafungin and anidulafungin according to EUCAST and CLSI, respectively (data not shown). According to CLSI caspofungin breakpoints, 5 of 6 initial isolates of C. albicans were susceptible, and 1 was intermediate; 4 of 5 C. glabrata isolates were resistant (0.5 µg/mL), and 1 was intermediate; and the C. krusei isolate was resistant (1 µg/mL). For each of the 12 pairs, MICs increased significantly (from 3 to 8 dilutions for caspofungin and micafungin and from 1 to 8 dilutions for anidulafungin) between the wild-type and the mutant isolate (Figure; p<0.001). Genetic relatedness was demonstrated for all C. albicans and C. glabrata paired isolates.
Figure.
Corresponding caspofungin (A), micafungin (B), and anidulafungin (C) MICs in 12 Fksp mutant Candida spp. isolates and their wild-type parent isolates, France, 2004–2010. Susceptibility testing was performed by using the European Committee for Antimicrobial Susceptibility Testing method (6) and AM3 medium (7).
Conclusions
We demonstrated that recent exposure to caspofungin altered the distribution of species causing Candida bloodstream infections (14), and that caspofungin exposure was independently associated with fungemia associated with intrinsically less-susceptible species in hematology (15). Echinocandin resistance in Candida spp. is still uncommon (4,13). Through our surveillance program, we estimated the incidence of decreased susceptibility to caspofungin associated with FKS mutations among C. albicans, C. glabrata, and C. krusei isolates responsible for candidemia in children and adults in Paris at 6 (0.4%) of 1,643 (NRCMA, unpub. data). We report proven caspofungin-resistant Candida spp. infections with none of the isolates belonging to the intrinsically less-susceptible species C. parapsilosis or C. guilliermondii.
We determined antifungal susceptibility testing by the EUCAST technique using AM3 because it enables better discrimination between susceptible wild-type and resistant mutant isolates (7). All isolates with high caspofungin MIC (>0.5 µg/mL) had mutation in the HS1 and/or HS2 region of FKS genes. The mutations were not restricted to a given position but were diverse, especially for C. albicans with 6 different mutations among the 8 resistant isolates; 5 different mutations were observed among the 10 C. glabrata resistant isolates. Most mutations in C. glabrata isolates were in Fks2p. Two mutations in C. albicans, 2 patterns of mutation in C. glabrata, and 1 mutation in C. krusei had not been reported before, highlighting the great mutation diversity that could be responsible for echinocandin resistance (13).
All but 1 patient had received caspofungin (70 mg on day 1, then 50 mg/d) before recovery of the resistant isolate, with a variable duration of exposure (<10 days to >8 months), in agreement with the literature (5 [3] to 420 days). In addition, 13 of 19 patients received caspofungin at the time of recovery of the resistant isolate. Most patients had malignancy, but 7 intensive care unit hospitalizations also were recorded. Echinocandins MICs between the wild-type parent and the subsequent mutant isolate increased by up to 8 log2 dilutions (Figure). The source of the resistant isolate is not unequivocal; it was acquired from the environment as an already resistant isolate or from the patient’s own flora under drug pressure. Our genotyping results favor the second hypothesis. This study suggests in France the emergence of infections from acquired echinocandin resistance in usually susceptible Candida spp. in patients preexposed to caspofungin, which highlights the need for careful species identification, antifungal drug susceptibility testing, and evaluation of prior drug exposure before antifungal drug prescription.
Acknowledgments
Additional members of the French Mycoses Study Group who contributed data: Gilles Blasco (Besançon); Claire Bouges-Michel, Guilene Barnaud, Charikleia Kelaidi (Bobigny); X. Baumgartner (Béziers); Guy Galeazzi, Jean Damien Ricard, Didier Dreyfus (Colombes); Anne-Lise Bienvenu, Claude Guerin, Michèle Gérard-Boncompain, Mauricette Michallet, Giovanna Cannas (Lyon); Jacques Reynes (Montpellier); Vanessa Chanteperdrix, Claude Lenoir (Nevers); Michel Attal (Toulouse); Edith Mazars, Philippe Lecocq (Valenciennes); Liliana Mihaila, Faouzi Saliba (Villejuif); Elisabeth Chachaty, Jean-Henri Bourhis (Villejuif); and Armelle Mathonnet, Julien Charpentier, Stéphane Bonacorsi, Karima Yacouben, André Baruchel, Jean-Hugues Dalle, Christophe Piketty, Annick Datry, Damien Roos-Weil, Jean-Louis Poirot, Harry Sokol, Anne-Sophie Leguern (Paris).
We thank Karine Stibon for managing the database and Dorothée Raoux and Damien Hoinard for technical assistance. We thank the sequencing facility (PF-8, Genotyping of Pathogens and Public Health, Institut Pasteur). We also thank Merck, Astellas, and Pfizer, respectively, for caspofungin, micafungin, and anidulafungin.
Institut Pasteur and Institut de Veille Sanitaire provided financial support for this study. E.D. has received funds for speaking from Merck and Schering; for consultancy from Merck and Astellas; and for travel from Merck, Schering, Gilead, and Astellas. O.L. has been a consultant for Gilead Sciences and Astellas and a member of the speaker’s bureau of Pfizer, MSD, Astellas, and Gilead Sciences. S.B. has been a consultant for Gilead Sciences and has received speaking honoraria from Gilead Sciences. F.G. has received funds for speaking from Merck and Schering.
Biography
Mr Dannaoui is associate professor at Paris Descartes University and Georges Pompidou European Hospital in Paris, France. His main research focuses on evaluation of antifungal drugs in vitro and in vivo in animal models of invasive fungal infections.
Footnotes
Suggested citation for this article: Dannaoui E, Desnos-Ollivier M, Garcia-Hermoso D, Grenouillet F, Cassaing S, Baixench M-T, et al. Candida spp. with acquired echinocandin resistance, France, 2004–2010. Emerg Infect Dis [serial on the Internet]. 2012 Jan [date cited]. http://dx.doi.org/10.3201/eid1801.110556
This work was presented in part at the 20th European Congress of Clinical Microbiology and Infectious Diseases, Vienna, Austria, April 10–13, 2010 (abstract no. O346).
These authors contributed equally to this article.
Additional members of the French Mycoses Study Group who contributed data are listed at the end of this article.
References
- 1.Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35. 10.1086/596757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baixench MT, Aoun N, Desnos-Ollivier M, Garcia-Hermoso D, Bretagne S, Ramires S, et al. Acquired resistance to echinocandins in Candida albicans: case report and review. J Antimicrob Chemother. 2007;59:1076–83. 10.1093/jac/dkm095 [DOI] [PubMed] [Google Scholar]
- 3.Pfeiffer CD, Garcia-Effron G, Zaas AK, Perfect JR, Perlin DS, Alexander BD. Breakthrough invasive candidiasis in patients on micafungin. J Clin Microbiol. 2010;48:2373–80. 10.1128/JCM.02390-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sun HY, Singh N. Characterisation of breakthrough invasive mycoses in echinocandin recipients: an evidence-based review. Int J Antimicrob Agents. 2010;35:211–8. 10.1016/j.ijantimicag.2009.09.020 [DOI] [PubMed] [Google Scholar]
- 5.Perlin DS. Resistance to echinocandin-class antifungal drugs. Drug Resist Updat. 2007;10:121–30. 10.1016/j.drup.2007.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Subcommittee on Antifungal Susceptibility Testing (AFST) of the ESCMID European Committee for Antimicrobial Susceptibility Testing. (EUCAST). EUCAST definitive document EDef 7.1: method for the determination of broth microdilution MICs of antifungal agents for fermentative yeasts. Clin Microbiol Infect. 2008;14:398–405. 10.1111/j.1469-0691.2007.01935.x [DOI] [PubMed] [Google Scholar]
- 7.Desnos-Ollivier M, Bretagne S, Raoux D, Hoinard D, Dromer F, Dannaoui E. Mutations in the fks1 gene in Candida albicans, C. tropicalis, and C. krusei correlate with elevated caspofungin MICs uncovered in AM3 medium using the method of the European Committee on Antibiotic Susceptibility Testing. Antimicrob Agents Chemother. 2008;52:3092–8. 10.1128/AAC.00088-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katiyar S, Pfaller M, Edlind T. Candida albicans and Candida glabrata clinical isolates exhibiting reduced echinocandin susceptibility. Antimicrob Agents Chemother. 2006;50:2892–4. 10.1128/AAC.00349-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foulet F, Nicolas N, Eloy O, Botterel F, Gantier JC, Costa JM, et al. Microsatellite marker analysis as a typing system for Candida glabrata. J Clin Microbiol. 2005;43:4574–9. 10.1128/JCM.43.9.4574-4579.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia-Hermoso D, Cabaret O, Lecellier G, Desnos-Ollivier M, Hoinard D, Raoux D, et al. Comparison of microsatellite length polymorphism and multilocus sequence typing for DNA-based typing of Candida albicans. J Clin Microbiol. 2007;45:3958–63. 10.1128/JCM.01261-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia-Hermoso D, MacCallum DM, Lott TJ, Sampaio P, Serna MJ, Grenouillet F, et al. Multicenter collaborative study for standardization of Candida albicans genotyping using a polymorphic microsatellite marker. J Clin Microbiol. 2010;48:2578–81. 10.1128/JCM.00040-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arendrup MC, Park S, Rodriguez-Tudela JL, Hope W, Lass-Flörl C, Donnelly PJ, et al. EUCAST susceptibility testing of Candida species to echinocandins: improved separation between wild type isolates and fks mutants by supplementation of BSA to the test medium. 21st European Congress of Clinical Microbiology and Infectious Diseases 27th International Congress of Chemotherapy; 2011; Milan, Italy. [Google Scholar]
- 13.Pfaller MA, Diekema DJ, Andes D, Arendrup MC, Brown SD, Lockhart SR, et al. Clinical breakpoints for the echinocandins and Candida revisited: integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drug Resist Updat. 2011;14:164–76. 10.1016/j.drup.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 14.Lortholary O, Desnos-Ollivier M, Sitbon K, Fontanet A, Bretagne S, Dromer F. Recent exposure to caspofungin or fluconazole influences the epidemiology of candidemia: a prospective multicenter study involving 2,441 patients. Antimicrob Agents Chemother. 2011;55:532–8. 10.1128/AAC.01128-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blanchard E, Lortholary O, Boukris-Sitbon K, Desnos-Ollivier M, Dromer F, Guillemot D, et al. Prior caspofungin exposure in patients with haematological malignancies is a risk factor for subsequent fungemia due to decreased susceptible Candidda spp.: a case-control study in Paris, France. Antimicrob Agents Chemother. 2011;55:5358–61. 10.1128/AAC.00690-11 [DOI] [PMC free article] [PubMed] [Google Scholar]