Abstract
Background
Religious involvement has been associated with improved health outcomes but greater obesity in older adults. No longitudinal study of young adults has examined the prospective association of religious involvement with incident cardiovascular risk factors (RFs) and subclinical disease (subCVD).
Methods
We included 2433 participants of the CARDIA study, aged 20 to 32 in 1987 when religiosity was assessed, who were followed for 18 years. Multivariable-adjusted regression models were fitted to assess prospective associations of frequency of religious participation at baseline with incidence of RFs and prevalence of subCVD after 18 years’ follow up.
Results
High frequency of religious participation was associated with a significantly greater incidence of obesity in unadjusted models (RR 1.57, 95% CI 1.14 – 1.73) and demographic-adjusted models (RR 1.34, 95% CI 1.09 – 1.65) but not after additional adjustment for baseline RFs (RR 1.17, 95% CI 0.97 – 1.41). When religious participation was treated dichotomously, any religious participation, compared with none, was associated with significantly lower subCVD.
Conclusions
Frequent religious participants are more likely to become obese between young adulthood and middle age; this association is confounded by demographic and other factors. Nonetheless, young adults with frequent participation may represent an opportunity for obesity prevention.
Keywords: Religion, Cardiovascular Disease, Obesity, Epidemiology, Prevention
INTRODUCTION
Religious involvement is associated with improved general health practices and outcomes. Lower rates of smoking (Strawbridge, W.J. et al, 1997; Lapane, K.L, et al, 1997; Whooley, M.A. et al, 2002) and all-cause mortality (Strawbridge, W.J. et al, 1997; Koenig, H.G. et al, 1999; Hummer, R.A. et al, 1999) have been found among those with frequent religious service attendance in longitudinal and cross-sectional studies. Review articles and meta-analyses have confirmed the positive relationship between religiosity and general health status (McCullogh, M.E. et al, 2000; Powell, L.H. et al, 2003; Chida, Y. et al, 2009).
Religious involvement has also been associated with lower cardiovascular disease (CVD)-related morbidity and mortality (Hummer, R.A. et al, 1999; Obisesan, T. et al, 2006; Oman, D. et al, 2002; Goldbourt, U. et al, 1999). However, the relationships between religiosity and CVD-related risk factors (RFs) are somewhat less clear, and few studies have examined longitudinal associations between religiosity and RFs. Religiosity has been associated with significantly greater body weight and/or obesity in numerous cross-sectional analyses (Lapane, K.L. et al, 1997; Ferraro, K.F., 1998; Feinstein, M. et al, 2010; Cline, K.M. & Ferraro, K., 2006), though some analyses have found no significant association between religiosity and overweight/obesity (Roff, L.L. et al, 2005; Ellis, L. & Biglione, D., 2000). While some studies have suggested that religious involvement and/or spirituality are cross-sectionally associated with lower blood pressure (Gillum, R.F. & Ingram, D.D., 2006), some have found no significant cross-sectional (Fitchett, G. & Powell, L.H., 2009) or longitudinal (Krause, N. et al, 2002) associations between religiosity/spirituality and blood pressure. In a recent cross-sectional analysis of a nationally representative, multi-ethnic sample of older adults, we found that religious involvement was associated with greater obesity (Feinstein, M. et al, 2010). However, no longitudinal community-based study of young adults has examined the association of religious involvement with incident CVD RFs and sub-clinical CVD (subCVD), despite evidence that CVD RFs and significant subCVD develop in the first decades of life.
In the present study, we sought to better understand the temporal nature of the association between religiosity and obesity. Thus, the objective of this study was to examine longitudinal associations of religious participation with development of CVD RFs, particularly obesity, and subCVD from young adulthood to middle age.
METHODS
Study Participants
The Coronary Artery Risk Development in Young Adults (CARDIA) study is an NHLBI-sponsored study designed to examine the prevalence and progression of coronary RFs and atherosclerosis in young people. The study design of CARDIA has been described in detail previously (Friedman, G.D. et al, 1988). A cohort of 5115 black and white adults aged 18-30 at the time of enrollment and balanced by sex, education, and age was recruited in 1985-1986 from four sites: Chicago, IL; Minneapolis, MN; Oakland, CA; and Birmingham, AL. Exams were conducted at years 0 (1985), 2, 5, 7, 10, 15, and 20. Follow-up contact has been maintained in 91% of CARDIA participants. This study used data from the CARDIA year 2 (baseline) and year 20 exams. Year 2 was used as baseline because it was the only exam in which religiosity was ascertained.
Religious Participation
Religious participation was measured based on participant responses to a questionnaire given at CARDIA exam 2 (which began in 1987). Frequency of participation in religious activities was determined by responses (more than once a week, every week, regularly but not every week, only on special occasions, never) to the question: “How frequently do you participate in religious activities?” Based on responses to this question, participants were grouped as having high (more than once a week, every week), medium (regularly but not every week), low (only on special occasions), or no (never) frequency of religious participation.
Risk Factors
For each participant, resting blood pressure, blood chemistries, anthropometric measures, as well as self-reported histories of smoking and medication use were obtained at the year 2 and year 20 exams according to methods described previously (Friedman, G.D. et al, 1988); the year 2 exam was performed concurrently with the questionnaires on religiosity. Obesity was defined as a BMI ≥30 kg/m2. Hypertension was defined as a systolic blood pressure of ≥140 mmHg, a diastolic blood pressure of ≥90 mmHg, or use of medication prescribed for hypertension. Hypercholesterolemia was defined as a total cholesterol ≥240 mg/dL, or use of medication for hyperlipidemia. Diabetes was defined at year 2 as self-reported diabetes, and at year 20 as self-reported, fasting glucose ≥126 mg/dL, or use of anti-diabetic medication.
Subclinical CVD
Coronary artery calcium (CAC) and common carotid intima-media thickness (CC-IMT) were obtained at the year 20 exam. Each of these measures is associated with different manifestations of vascular pathology; CAC associates most closely with coronary atherosclerosis and coronary risk, and CC-IMT is a measure of atherosclerosis that associates most closely with stroke risk (Folsom, A.R. et al, 2008). CAC was measured by electron-beam or multi-detector computed tomography (CT) scans; scans were sent to a central CARDIA Reading Center, where radiologists used image-processing software to determine calcific foci and calculate calcium scores. Images of the left and right common carotid arteries were obtained using high-resolution B-mode ultrasound and read centrally; CC-IMT values were determined using previously described methods (Polak, J.F. et al, 2010).
Statistical Analyses
All analyses were performed using SAS version 9.2 (SAS Institute Inc, Cary, NC). Participants were classified by self-reported levels of participation in religious activity (never, low, medium, or high). Baseline characteristics were compared across these groups using general linear models for continuous variables and chi-square tests for categorical variables. Logistic regression models were fitted to assess prospective associations of frequency of religious participation (at year 2) with incidence of cardiovascular risk factors (at year 20): obesity, hypertension, hypercholesterolemia, diabetes and smoking. Three sequential models were developed for each outcome of interest: unadjusted (Model 1); adjusted for age, sex, race, education and income at year 2 (Model 2); and additionally adjusted for clinical covariates at year 2: systolic and diastolic blood pressure, body mass index, total cholesterol, triglycerides, high-density lipoprotein, diabetes and smoking status (Model 3). All regressions were performed using the religiosity level of “never” as the reference group. Similar analyses were performed examining the association of religiosity levels (at year 2) with subCVD (at year 20): coronary artery calcium score>0 and CC-IMT>90th percentile. A 2-tailed p<0.05 was considered statistically significant. Participants were excluded from logistic regression models assessing incidence of each RF if they did not answer the religiosity questionnaire, did not attend the year 20 exam, or already had the RF under analysis (obesity, hypertension, hypercholesterolemia, diabetes, or smoking) prevalent at year 2. Participants were excluded from logistic regression models assessing prevalence of subCVD if they did not answer the religiosity questionnaire, did not attend the year 20 exam, or did not have subCVD assessed. There were modest differences between those who were excluded and those who were included with regard to prevalence of never participating in religious activities at year 2 (20.0% for those who did not attend year 20 vs. 13.8% in those without subCVD measured vs. 16.3% in those with complete covariates).
RESULTS
Study Sample and Baseline Characteristics
Baseline characteristics of the 2433 CARDIA participants who had complete data are shown in Table 1, stratified by frequency of religious participation. Participants with medium and high frequencies of religious participation were more likely than those with little or none to be female and black. Those with more religious participation also had higher BMI, were more likely to have diabetes, and were less likely to smoke.
Table 1.
Descriptive Statistics at Baseline (1987) of Participants by Frequency of Religious Participation (N=2433)*
| None (N=396) | Low (N=954) | Medium (N=562) | High (N=521) | P Value | |
|---|---|---|---|---|---|
| Age (yrs) | 27.3 | 27.2 | 27.3 | 27.3 | .97 |
|
| |||||
| % Female | 53.8 | 51.8 | 62.5 | 63.0 | <.01 |
|
| |||||
| Race (%) | <.01 | ||||
| White | 76.5 | 64.5 | 45.0 | 49.1 | |
| Black | 23.5 | 35.5 | 55.0 | 50.9 | |
|
| |||||
| Income (%) | .11 | ||||
| Low (<$25,000/yr) | 36.6 | 31.3 | 36.3 | 34.7 | |
| Medium ($25,000-49,999/yr) | 35.9 | 39.1 | 39.0 | 41.1 | |
| High (>=$50,000/yr) | 27.5 | 29.6 | 24.7 | 24.2 | |
|
| |||||
| Education (%) | <.01 | ||||
| High School | 32.6 | 32.6 | 33.3 | 26.9 | |
| College | 57.3 | 52.4 | 57.3 | 60.6 | |
| Graduate School | 10.1 | 15.0 | 9.4 | 12.5 | |
|
| |||||
| Systolic Blood Pressure, mmHg | 106.6 | 107.3 | 107.4 | 107.0 | .63 |
|
| |||||
| Diastolic Blood Pressure, mmHg | 67.1 | 67.4 | 67.5 | 67.6 | .83 |
|
| |||||
| Triglycerides, mg/dL | 82.9 | 80.5 | 75.1 | 71.6 | <.01 |
|
| |||||
| LDL Cholesterol, mg/dL | 112.8 | 113.7 | 114.2 | 112.8 | .87 |
|
| |||||
| Total Cholesterol, mg/dL | 184.1 | 184.5 | 184.4 | 182.4 | .68 |
|
| |||||
| Treated for Hypertension, % | 2.0 | 1.8 | 3.9 | 2.7 | .07 |
|
| |||||
| Diabetes, % | 0.5 | 0.8 | 1.4 | 1.5 | .33 |
|
| |||||
| Smoking, % | 26.3 | 27.6 | 26.5 | 13.6 | <.01 |
|
| |||||
| Body Mass Index, kg/m2 | 24.2 | 24.9 | 25.1 | 25.3 | <.01 |
Includes CARDIA participants who attended exam years 2 and 20 and had complete religiosity, RF, and subCVD data
Incidence of RFs by frequency of religious participation
The incidence of new CVD RFs among CARDIA participants initially free of each respective RF at baseline is shown in Table 2 and Figure 1. In unadjusted logistic regression, each frequency of participation (low, medium, and high) was associated with a significantly greater likelihood of incident obesity than no participation, and the highest frequency of participation was associated with the greatest likelihood of incident obesity (Table 3). Meanwhile, those with medium and high frequencies of religious participation were significantly more likely than those with none to become hypertensive by year 20 (Table 3).
Table 2.
Incidence of Risk Factors and Prevalence of Subclinical Cardiovascular Disease by year 20 (2005)*
| Condition | Number of participants without condition at baseline† | Participants without condition at baseline with incident RF or prevalent SubCVD by year 20 (%) |
|---|---|---|
| Obesity | 2826 | 28.7 |
| Smoking | 2465 | 5.2 |
| Hypercholesterolemia | 3027 | 12.8 |
| Diabetes | 3294 | 9.0 |
| Hypertension | 3200 | 21.5 |
| CAC > 0 | 2721 | 18.3 |
| IMT > 90th Percentile | 2721 | 10.0 |
RF incidence analysis includes CARDIA participants who attended exam years 2 and 20 and had complete religiosity data. SubCVD prevalence analysis includes CARDIA participants who attended exam years 2 and 20, had complete religiosity data, and had subCVD measured.
SubCVD was not assessed at baseline.
Figure 1.
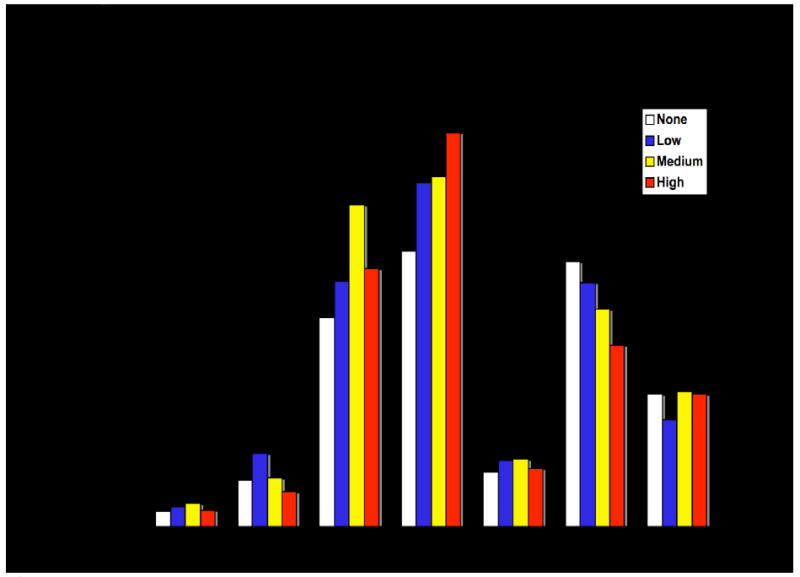
Incidence of RFs and Year 20 (2005) Prevalence of Subclinical Atherosclerosis by Frequency of Participation in Religious Activities at Baseline (1987)
Table 3.
Rate Ratios for Incidence of Risk Factors and Odds Ratios for Prevalence of Subclinical Cardiovascular Disease by year 20 (2005) by Frequency of Religious Participation at Baseline (1987)*
| Frequency of participation | ||||
|---|---|---|---|---|
| Model 1: Unadjusted | ||||
| None | Low | Medium | High | |
| Obesity | Referent | 1.29 (1.06, 1.57)† | 1.40 (1.14, 1.73)† | 1.57 (1.28, 1.93)† |
| Smoking | Referent | 1.78 (1.01, 3.15)† | 1.60 (.87, 2.94) | 0.84 (.43, 1.64) |
| Hypercholesterolemia | Referent | 1.10 (.83, 1.46) | 0.95 (.69, 1.30) | 0.94 (.69, 1.29) |
| Diabetes | Referent | 1.05 (.75, 1.48) | 1.24 (.87, 1.78) | 1.18 (.82, 1.71) |
| Hypertension | Referent | 1.23 (.98, 1.54) | 1.61 (1.28, 2.02)† | 1.32 (1.03, 1.68)† |
| CAC > 0 | Referent | 0.89 (.68, 1.18) | 0.79 (.58, 1.07) | 0.63 (.46, .87)† |
| IMT > 90th Percentile | Referent | 0.80 (.55, 1.15) | 0.94 (.64, 1.40) | 0.96 (.65, 1.44) |
| Model 2: Adjusted for year 2 demographics (age, sex, race, education, and income) | ||||
| Obesity | Referent | 1.24 (1.02, 1.51)† | 1.12 (.90, 1.39) | 1.34 (1.09, 1.65)† |
| Smoking | Referent | 1.81 (.99, 3.27) | 1.62 (.86, 3.07) | 0.87 (.43, 1.75) |
| Hypercholesterolemia | Referent | 1.13 (.85, 1.50) | 1.09 (.79, 1.50) | 1.10 (.80, 1.52) |
| Diabetes | Referent | 1.02 (.71, 1.45) | 1.05 (.72, 1.54) | 1.04 (.71, 1.52) |
| Hypertension | Referent | 1.13 (.90, 1.42) | 1.22 (.96, 1.54) | 1.03 (.81, 1.32) |
| CAC > 0 | Referent | 0.89 (.66, 1.21) | 0.89 (.63, 1.27) | 0.72 (.50, 1.04) |
| IMT > 90th Percentile | Referent | 0.67 (.45, 0.99)† | 0.68 (.44, 1.05) | 0.81 (.52, 1.25) |
| Model 3: Adjusted for year 2 demographics and RFs (SBP, DBP, BMI, triglycerides, total cholesterol, HDL cholesterol, diabetes and smoking) | ||||
| Obesity | Referent | 1.11 (.93, 1.32) | 1.02 (.84, 1.23) | 1.17 (0.97, 1.41) |
| Smoking | Referent | 1.86 (.99, 3.45) | 1.58 (.82, 3.04) | 0.89 (.43, 1.84) |
| Hypercholesterolemia | Referent | 1.10 (.84, 1.43) | 1.09 (.80, 1.49) | 1.11 (.82, 1.51) |
| Diabetes | Referent | 0.86 (.61, 1.21) | 0.98 (.67, 1.41) | 0.85 (.58, 1.25) |
| Hypertension | Referent | 1.11 (.88, 1.39) | 1.19 (.94, 1.50) | 0.98 (.77, 1.26) |
| CAC > 0 | Referent | 0.83 (.60, 1.14) | 0.81 (.56, 1.17) | 0.72 (.49, 1.06) |
| IMT > 90th Percentile | Referent | 0.56 (.37, .85)† | 0.58 (.37, 0.93)† | 0.70 (.44, 1.11) |
RF incidence analysis includes CARDIA participants who attended exam years 2 and 20 and had complete religiosity data. SubCVD prevalence analysis includes CARDIA participants who attended exam years 2 and 20, had complete religiosity data, and had subCVD measured.
P<0.05. Unless otherwise indicated, results are nonsignificant
After adjustment for year 2 demographic covariates (including age, sex, race, education, and income), a high frequency of participation was still associated with a significantly greater likelihood of incident obesity by year 20, while the associations of all levels of religious participation with incident hypertension were attenuated to non-significance (Table 3). After further adjustment for all baseline RFs, a high frequency of religious participation was still associated with a greater risk of incident obesity, although this association was no longer statistically significant (Table 3). After additional adjustment for CARDIA field center in a secondary analysis, associations between religious participation and obesity were not significantly different from the model adjusted for demographics and RFs only; the association between a high frequency of religious participation and obesity before (RR 1.17, 95% CI 0.97, 1.41) and after (RR 1.16, 95% CI 0.96, 1.41) additional adjustment for field center were essentially the same.
A secondary analysis treating religious participation dichotomously (any frequency of religious participation vs. none) revealed significant associations of religious participation with obesity in unadjusted (RR 1.56, 95% CI 1.23 – 1.98) and demographic-adjusted (RR 1.34, 95% CI 1.04-1.73) models, but not in models adjusted additionally for all RFs. When the dichotomous model was stratified by race, no statistically significant associations were found between religious involvement and incident RFs for white or black participants (with lower power to detect significant associations). Likewise, an interaction term for race and participation was not statistically significant. When we combined the “never” and “low” participation groups in another secondary analysis, the demographic-adjusted relative risk for obesity in the high versus this combined lowest participation group was 1.14 (95% CI 0.99-1.31), indicating a similar but somewhat weaker association.
Prevalence of subCVD at year 20, by frequency of religious participation
The prevalence at year 20 of CAC>0 or CC-IMT>90th percentile is shown in Table 2 and Figure 1. Although high religious involvement was associated with a significantly lower year 20 prevalence of CAC in unadjusted logistic regression, this association became non-significant after adjustment for demographics and baseline RFs (Table 3). Low religious participation was associated with a significantly lower risk of CC-IMT >90th percentile after adjustment for demographics, and both low and medium religious participation were associated with significantly lower risks of CC-IMT >90th percentile after additional adjustment for RFs (Table 3). When religious participation was treated dichotomously, any religious participation was associated with a significantly lower risk of CC-IMT >90th percentile after adjustment for baseline demographics and RFs (OR 0.56, 95% CI 0.38 – 0.83). When the dichotomous model was stratified by race, any religious involvement among white participants was associated with a significantly lower risk of CC-IMT >90th percentile than no religious involvement among white participants, after adjustment for baseline demographics and RFs (OR 0.38, 95% CI 0.22-0.68); this association was not significant in blacks (OR 0.77, 95% CI, 0.42-1.44).
DISCUSSION
Principal Findings
A high frequency (at least once per week) of religious involvement was associated with an elevated risk of incident obesity in unadjusted analyses and after adjustment for demographics. Further adjustment for all baseline RF levels revealed an association of borderline significance. Any level of religious participation was associated with a lower year 20 prevalence of CC-IMT >90th percentile in adjusted analyses, particularly among white participants.
Religious Participation and Obesity
Study participants with a high frequency of religious involvement were more likely than those with none to become obese between young adulthood and middle age, even after accounting for demographics. After additional adjustment for RFs during young adulthood, a high frequency of religious involvement remained associated with a greater incidence of obesity by middle age, but this association was borderline statistically significant. In light of previous studies demonstrating a greater prevalence of obesity among older adults, the findings of the present study suggest that development of obesity among religious people between young adulthood and middle age may partially explain the persistent association between religiosity and obesity through middle age and older adulthood.
Numerous theories have been proposed to explain the finding that greater religiosity is associated with a greater risk of obesity. One longitudinal analysis suggested that religious individuals are more likely to become obese because religious organizations rarely address dietary over-consumption and religious gatherings often center around food and drink (Krause, N. et al, 2002). It is also possible that religiosity leads to obesity to a lesser extent than obesity leads to religiosity, as religious organizations may offer a welcoming environment for those who are obese and seek protection from social stigma (Cline, K.M. & Ferraro, K., 2006). However, the latter explanation does not appear to be primarily responsible for the association between religiosity and obesity in light of our longitudinal finding that religious participation associates prospectively with incident obesity.
The presence of a significant longitudinal association between religiosity and obesity even after adjustment for demographics highlights a need for anti-obesity interventions targeted specifically at religious groups. Numerous faith-based preventive health programs have arisen over the last two decades in an attempt to capitalize on the relative accessibility and pre-existing infrastructure of religious populations, with promising results (Dehaven, M.J. et al, 2004). Nevertheless, these initiatives have been somewhat limited in scope and duration, and obesity has remained a prevalent yet unaddressed problem in many religious communities. That nearly 30% of younger adults with any religious participation may become obese over the ensuing two decades may represent an important opportunity to target obesity prevention.
Religious Participation and Hypertension
Religious involvement was associated with a significantly greater incidence of hypertension in unadjusted analysis, but was attenuated to non-significance after adjustment for demographics. Regression analysis demonstrated a particularly strong, statistically significant association of race and sex with hypertension. Given the especially high number of black females in the medium and high religious involvement groups and the known high prevalence of hypertension among black females (Cutler, J.A. et al, 2008), it is likely that the association between medium religious involvement and hypertension was strongly confounded by sex and race.
Religious Participation and Subclinical Carotid Atherosclerosis
We found that religious participation was associated with a significantly lower risk of subclinical carotid atherosclerosis (as measured by CC-IMT >90th percentile) after adjustment for baseline demographics and RFs. This association was particularly strong among white participants. Although these findings were statistically significant, they may not be particularly clinically meaningful; mean CC-IMT varied minimally between religious participation groups and without any clear trend (.79, .79, .81, and .80 mm for those with no, low, medium, and high religious participation, respectively). We did not measure associations between religiosity and CVD events in this analysis because of our young population in whom very few CVD events have occurred to date.
Limitations
Some limitations of our study should be acknowledged. First, our measure of frequency of religious participation may not adequately capture all aspects of religiosity. Religion was measured only once, and self-reported religious involvement at year 2 may not always correspond to religious involvement for the following 18 years. Another limitation of this study is our likely inability to fully account for residual confounding related to geographic and cultural considerations. It is possible that demographic adjustment does not entirely account for regional differences and that distinct regional characteristics are partially responsible for differences in prospective RF development between religiosity groups. Another limitation of our study is that CARDIA participants represent a young volunteer cohort of relatively healthy individuals at inception; accordingly, the external validity of our findings may be limited somewhat.
CONCLUSION
Our study in a well-described, community-based sample confirms a longitudinal link between religious involvement and obesity, independent of demographics. Our finding that religiosity is associated with a slightly lower risk of subclinical carotid atherosclerosis is statistically significant but of uncertain clinical meaning and merits further validation in other cohorts.
Highlights.
We examined associations of religiosity in young adulthood with incident cardiac risk factors.
Frequent religious involvement in young adults is associated with greater obesity by middle age.
This study confirms a longitudinal link between religious involvement and obesity.
Long-term obesity prevention initiatives targeted at religious groups may be warranted.
Acknowledgments
Work on this manuscript was supported by the following contracts: University of Alabama at Birmingham, Coordinating Center, N01-HC-95095;; University of Alabama at Birmingham, Field Center, N01-HC-48047;; University of Minnesota, Field Center, N01-HC-48048;; Northwestern University, Field Center, N01-HC-48049;; Kaiser Foundation Research Institute, N01-HC-48050;; Wake Forest University, N01-HC-45205; New England Medical Center, N01-HC-45204 from the National Heart, Lung and Blood Institute.
Dr. Lloyd-Jones had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
CONFLICT OF INTEREST STATEMENT The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Chida Y, Steptoe A, Powell LH. Religiosity/spirituality and mortality. A systematic quantitative review. Psychother Psychosom. 2002;78:81–90. doi: 10.1159/000190791. [DOI] [PubMed] [Google Scholar]
- Cline KM, Ferraro K. Does religion increase the prevalence and incidence of obesity in adulthood? J Sci Study Relig. 2006;45:269–281. doi: 10.1111/j.1468-5906.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in Hypertension Prevalence, Awareness, Treatment, and Control Rates in United States Adults Between 1988-1994 and 1999-2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- Dehaven MJ, Hunder IB, Wilder L, Walton JW, Berry J. Health programs in faith-based organizations: are they effective? Am J Public Health. 2004;94:1030–6. doi: 10.2105/ajph.94.6.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis L, Biglione D. Religiosity and obesity: are overweight people more religious? Personality and Individual Differences. 2000;28:1119–1123. [Google Scholar]
- Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Burden of Cardiovascular Risk Factors, Subclinical Atherosclerosis, and Incident Cardiovascular Events Across Dimensions of Religiosity: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2010;121:659–666. doi: 10.1161/CIRCULATIONAHA.109.879973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF. Firm believers? Religion, body weight, and well-being. Rev Relig Rsch. 1998;39:224–44. [Google Scholar]
- Fitchett G, Powell LH. Daily Spiritual Experiences, Systolic Blood Pressure, and Hypertension among Midlife Women in SWAN. Ann Behav Med. 2009;37:257–267. doi: 10.1007/s12160-009-9110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folsom AR, Kronmal RA, Detrano RC, O’Leary DH, Bild DE, Bluemke DA, et al. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA) Arch Intern Med. 2008;168:1782. doi: 10.1001/archinte.168.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freidman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- Gillum RF, Ingram DD. Frequency of Attendance at Religious Services, Hypertension, and Blood Pressure: The Third National Health and Nutrition Examination Survey. Pyschosomatic Med. 2006;68:382–385. doi: 10.1097/01.psy.0000221253.90559.dd. [DOI] [PubMed] [Google Scholar]
- Goldbourt U, Yaari S, Medalie J. Factors predictive of long-term coronary heart disease mortality among 10,059 male Israeli civil servants and municipal employees. Cardiology. 1999;82:100–121. doi: 10.1159/000175862. [DOI] [PubMed] [Google Scholar]
- Hummer RA, Rogers R, Nam C, Ellison C. Religious Involvement and US Adult Mortality. Demography. 1999;36:273–285. [PubMed] [Google Scholar]
- Koenig HG, Hays J, Larson D, George L, Cohen H, McCullough M, et al. Does religious attendance prolong survival? A six-year follow-up study of 3968 older adults. J Gerontol A Biol Sci Med. 1999;54:M370–M376. doi: 10.1093/gerona/54.7.m370. [DOI] [PubMed] [Google Scholar]
- Krause N, Liang J, Shaw BA, Sugisawa H, Kim HK, Sugihara Y. Religion, death of a loved one, and hypertension among older adults in Japan. J Gerontol Soc Sci. 2002;57B:S96–S107. doi: 10.1093/geronb/57.2.s96. [DOI] [PubMed] [Google Scholar]
- Lapane KL, Lasater T, Allan C, Carleton R. Religion and cardiovascular disease risk. J Relig Health. 1997;36:155–63. [Google Scholar]
- McCullough ME, Larson DB, Hoyt WT, Koenig HG, Thoresen C. Religious involvement and mortality: a meta-analytic review. Healthy Psychology. 2000;19:211–22. doi: 10.1037//0278-6133.19.3.211. [DOI] [PubMed] [Google Scholar]
- Obisesan T, Livingston I, Trulear HD, Gillum F. Frequency of attendance at religious services, cardiovascular disease, metabolic risk factors and dietary intake in Americans: an age-stratified exploratory analysis. Int J Psychiatry Med. 2006;36:435–48. doi: 10.2190/9W22-00H1-362K-0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oman D, Kurata J, Strawbridge W, Cohen R. Religious attendance and cause of death over 31 years. Int J Psychiatry Med. 2002;32:69–89. doi: 10.2190/RJY7-CRR1-HCW5-XVEG. [DOI] [PubMed] [Google Scholar]
- Polak JF, Person SD, Wei GS, Godreau A, Jacobs DR, Harrington A, et al. Segment-Specific Associations of Carotid Intima-Media Thickness with Cardiovascular Risk Factors. Stroke. 2010;41:9–15. doi: 10.1161/STROKEAHA.109.566596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LH, Shahabi L, Thoresen CE. Religion and Spirituality: Linkages to Physical Health. Am Psych. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- Roff LL, Klemmack D, Parker M, Koenig H, Sawyer-Baker P, Allman R. Religiosity, smoking, exercise, and obesity among southern, community-dwelling older adults. J App Gerontol. 2005;24:337–354. [Google Scholar]
- Strawbridge WJ, Cohen R, Sherma S, Kaplan G. Frequent attendance at religious services and mortality over 28 years. Am J Pub Health. 1997;87:957–961. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whooley MA, Boyd AL, Gardin JM, Williams DR. Religious Involvement and Cigarette Smoking in Young Adults: The CARDIA Study. Arch Intern Med. 2002;162:1604–1610. doi: 10.1001/archinte.162.14.1604. [DOI] [PubMed] [Google Scholar]


