Abstract
Objectives
To estimate the rates of stress urinary incontinence (SUI) surgery from 2000-2009 by type of procedure, year, age, and region of the country.
Methods
We utilized data between 2000 and 2009 from a database containing healthcare claims data from employer-based plans in the United States. We analyzed data for all women aged 18-64 years, identifying all SUI procedures in this population. Rates per 100,000 person-years and 95% confidence intervals (CI) were calculated each year by procedure type, age and region.
Results
The study population included 32.9 million women aged 18-64 years observed for 74,007,937 person-years between 2000 and 2009. During that time, there were 182,110 SUI procedures for a rate of 246.1 per 1100,000 person-years (95%CI: 239.7, 252.6). The most common SUI surgery was sling (198.3 per 1100,000 person-years, 95%CI: 192.8, 203.9) followed by Burch (25.9 per 100,000 person-years, 95%CI 24.8, 27.2). There was a dramatic increase in slings with a corresponding decrease in Burch procedures from 2000-2009. Other SUI surgeries had lower rates. Although this trend was evident across all regions, the Northeast had the lowest rate of SUI surgery, while rates in the West, Midwest and South were 1.44, 1.76, and 2.09 times higher, respectively.
Conclusions
In a dramatic shift over the last decade, slings have become the dominant procedure for stress urinary incontinence among women aged 18-64 years. Although this trend was seen across the U.S., considerable variability exists in the SUI surgery rates by region.
INTRODUCTION
Stress urinary incontinence (SUI) is a highly prevalent condition affecting approximately 13% of women aged 19-44 years and 22% of women aged 45-64 years.(1) These women suffer from unpredictable episodes of urinary leakage, which profoundly impairs their quality of life.(2-4) In addition, the economic costs are substantial, totaling over $20 billion per year in the United States,(4, 5) with 50-75% of these costs due to routine care from incontinence pads, diapers, laundry, dry cleaning, odor control, bed pads and skin care products.
The number of SUI surgeries has increased substantially since the mid 1990's with increases in both outpatient (6) and inpatient (7, 8) surgical procedures. It is not known if this increase in the number of procedures simply reflects an increase in the size of the population overall, a shift in the age distribution as a result of aging ‘baby boomers’, or an actual increase in the rate at which SUI is managed surgically.
Anecdotally, clinicians believe that there has also been a shift from the Burch procedure to the midurethral sling, since 1998 when the first midurethral sling was Food and Drug Administration (FDA)-approved.(9) Recent studies based on the National Hospital Discharge Survey (NHDS)(7) and the Nationwide Inpatient Sample (NIS) (8) have used International Classification of Diseases, 9th revision (ICD9) procedure codes to identify SUI surgeries, but these codes are not sufficiently specific. For example, in 2004, 74% of SUI surgeries, which represented more than 77,000 procedures, were coded as ICD9 code 59.79 “other repair of SUI”.(7) While the authors speculate that surgeries coded as “other repair of SUI” were midurethral slings, no definitive conclusions can be made without more specific codes. Another limitation is that these national databases include either inpatient (7, 8) or outpatient procedures,(6) limiting the ability of investigators to study overall trends in surgical management of SUI in a single, nationally representative sample. Detailed information regarding the trends in SUI surgery, by type of procedure, location of surgery (inpatient versus outpatient) as well as the impact of age and region of the U.S., would provide valuable insight into the public health burden of SUI, identify changes in clinical practice and whether these changes correlate to evidence regarding effectiveness, and stimulate future research.
In light of these limitations in the existing literature, the objectives of this study were 1) to estimate the rates of SUI surgery (overall and by type of procedure) for the years 2000-2009 and 2) to estimate the impact of age on these surgical rates, and 3) to identify regional differences, if any, in the rates of SUI surgery.
MATERIALS AND METHODS
Data Source
This analysis is based on the Thomson Reuters MarketScan Commercial Claims and Encounters (CC&E) database from 2000-2009 (copyright © 2010 Thomson Healthcare Incorporated Inc. All rights reserved). This database contains de-identified, individual-specific clinical utilization and enrollment claims data for inpatient, outpatient and prescription drug services from approximately 100 payers in the United States. Although the data are de-identified, unique individuals can be followed over time using encrypted identification numbers. The database provides information on approximately 3.7 million individuals in 2000 and increases to 40.0 million in 2009. These data represent the medical experience of insured employees, their spouses and their dependents until 65 years of age when they become eligible for Medicare. Of note, in 2006, 57% of the total U.S. population had employer-based insurance, and a detailed analysis of the database has shown that it is representative of the non-elderly population with employer-based insurance in terms of gender, age, and region of the U.S.(11) This study was determined to be exempt from further review by the Institutional Review Board at the University of North Carolina at Chapel Hill.
SUI Surgery Rates
The study population included all women aged 18-64 years from 2000-2009. Rates were calculated by dividing the total number of surgeries (including repeat surgeries) by the total person-time at risk. In order to calculate person-time at risk, we summed all periods of time when eligible women were enrolled in a contributing health plan. For the numerator, we identified SUI procedures among eligible women based on the following CPT codes: 57288 for sling; 51840, 51841 or 51851 for Burch colposuspension; 51715 for endoscopic injection of implant material into the submucosal tissue of the urethra, which we will refer to as “collagen”; 57220 for Kelly plication; 51845 or 57289 for needle suspension; 51990 or 51992 for laparoscopic urethral suspension or laparoscopic sling operation, respectively, which we will refer to as “laparoscopic”; and 58267 or 58293 for total vaginal hysterectomy (TVH) with colpo-urethrocystopexy.”
If multiple CPT codes were recorded on the same service date, we utilized a prioritization scheme in order to identify only one SUI procedure for each date of service. The prioritization for SUI surgeries was the following: Burch followed by a laparoscopic SUI surgery, TVH+colpo-urethrocystopexy, sling, needle suspension, collagen injection and then Kelly plication. This hierarchy was utilized to avoid double counting, as it would be uncommon to undergo two different SUI procedures on the same date of service. If both an inpatient and outpatient procedure claim occurred on the same service date, we preferentially included the inpatient procedure, again in order to avoid double counting. However, if a woman underwent several SUI procedures on different service dates, each SUI procedure would be counted in this analysis.
Statistical Analysis
We estimated the rate of SUI surgery overall as well as procedure and location (inpatient vs outpatient) specific, procedure and calendar-year specific, age and calendar-year specific, and age and region specific rates for SUI surgery. We estimated 95% confidence intervals (CIs) based on the Poisson distribution. Rates and CIs are reported per 100,000 person-years (100Kpy). In order to adjust for differences in the age distribution over calendar time and across regions, we estimated age-adjusted rate ratios (adjRR) using Poisson regression by including age as a 5-level categorical variable plus a linear term to account for residual variation within age levels. Wald chi-square statistics were used to test the significance of independent predictors with a two-sided alpha=0.05. All confidence intervals were estimated and statistical tests were conducted using Poisson regression with the dispersion parameter empirically estimated by the Pearson chi-square divided by the degrees of freedom to account for overdispersion.(12) Analyses were performed using SAS, v9.2 (SAS Institute, Cary, NC).
RESULTS
The study population included 32.9 million women aged 18-64 years in the database from 2000-2009. Table 1 lists the person-time contribution for the population at-risk of all women aged 18-64 years, divided by age group (18-24, 25-34, 35-44, 45-54, 55-64 years), calendar year, and region of the U.S. These women contributed a total of 74,007,937 person-years of observation with a median person-time of 1.75 years (interquartile range (IQR) 0.9, 3.0 years, range 0.003-10.0 years). The shorter median person-time contribution reflects the higher person-time contribution in the later years, such as 2009 (13.4 million person-years) when compared to earlier years such as 2000 (1.3 million person-years) (Table 1).
Table 1.
Demographic Characteristics of Women Aged 18-64 in the Database Population, Women Having Any Type of Stress Urinary Incontinence (SUI) Surgery, and Women Having One of Seven Specific SUI Surgeries
| Person-Years* (n=74,007,937) |
All Surgeries (n=182,110) |
Sling (n=146,748) | Burch (n=19,190) |
Collagen (n=8,266) |
Laparoscopic (n=4,315) |
TVH (n=1,709 |
Needle (n=1,355) |
Kelly (n=527) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Age | ||||||||||||||||||
| 18–24 | 8,815,790 | 11.9 | 350 | 0.2 | 219 | 0.2 | 27 | 0.1 | 82 | 1.0 | 9 | 0.2 | 8 | 0.5 | 2 | 0.2 | 3 | 0.6 |
| 25–34 | 13,490,039 | 18.2 | 9,659 | 5.3 | 7,523 | 5.1 | 1,263 | 6.6 | 331 | 4.0 | 285 | 6.6 | 148 | 8.7 | 66 | 4.9 | 43 | 8.2 |
| 35–44 | 17,322,910 | 23.4 | 47,032 | 25.8 | 37,577 | 25.6 | 6,107 | 31.8 | 1,112 | 13.5 | 1,277 | 29.6 | 559 | 32.7 | 291 | 21.5 | 109 | 20.7 |
| 45–54 | 19,591,600 | 26.5 | 71,486 | 39.3 | 57,900 | 39.5 | 7,914 | 41.2 | 2,662 | 32.2 | 1,719 | 39.8 | 585 | 34.2 | 515 | 38.0 | 191 | 36.2 |
| 55–64 | 14,787,598 | 20.0 | 53,583 | 29.4 | 43,529 | 29.7 | 3,879 | 20.2 | 4,079 | 49.4 | 1,025 | 23.8 | 409 | 23.9 | 481 | 35.5 | 181 | 34.4 |
| Calendar Year | ||||||||||||||||||
| 2000 | 1,292,297 | 1.7 | 2,710 | 1.5 | 1,012 | 0.7 | 1,101 | 5.7 | 232 | 2.8 | 108 | 2.5 | 121 | 7.1 | 121 | 8.9 | 15 | 2.9 |
| 2001 | 2,039,122 | 2.8 | 4,176 | 2.3 | 1,911 | 1.3 | 1,483 | 7.7 | 299 | 3.6 | 171 | 4.0 | 158 | 9.3 | 122 | 9.0 | 32 | 6.1 |
| 2002 | 3,754,618 | 5.1 | 7,964 | 4.4 | 4,425 | 3.0 | 2,288 | 11.9 | 501 | 6.1 | 344 | 8.0 | 205 | 12.0 | 159 | 11.7 | 42 | 8.0 |
| 2003 | 5,669,279 | 7.7 | 12,014 | 6.6 | 7,812 | 5.3 | 2,671 | 13.9 | 628 | 7.6 | 393 | 9.1 | 242 | 14.2 | 207 | 15.3 | 61 | 11.6 |
| 2004 | 7,519,076 | 10.2 | 16,384 | 9.0 | 12,052 | 8.2 | 2,663 | 13.9 | 772 | 9.3 | 446 | 10.3 | 216 | 12.6 | 162 | 12.0 | 73 | 13.9 |
| 2005 | 8,298,578 | 11.2 | 19,607 | 10.8 | 15,716 | 10.7 | 2,115 | 11.0 | 908 | 11.0 | 458 | 10.6 | 222 | 13.0 | 145 | 10.7 | 43 | 8.2 |
| 2006 | 9,293,200 | 12.6 | 24,275 | 13.3 | 20,342 | 13.9 | 2,049 | 10.7 | 1,103 | 13.3 | 470 | 10.9 | 153 | 9.0 | 118 | 8.7 | 40 | 7.6 |
| 2007 | 9,290,854 | 12.6 | 25,198 | 13.8 | 21,768 | 14.8 | 1,713 | 8.9 | 997 | 12.1 | 473 | 11.0 | 98 | 5.7 | 101 | 7.5 | 48 | 9.1 |
| 2008 | 13,496,934 | 18.2 | 34,199 | 18.8 | 30,006 | 20.5 | 1,739 | 9.1 | 1,394 | 16.9 | 713 | 16.5 | 145 | 8.5 | 115 | 8.5 | 87 | 16.5 |
| 2009 | 13,353,981 | 18.0 | 35,583 | 19.5 | 31,704 | 21.6 | 1,368 | 7.1 | 1,432 | 17.3 | 739 | 17.1 | 149 | 8.7 | 105 | 7.8 | 86 | 16.3 |
| US Region | ||||||||||||||||||
| Northeast | 7,973,109 | 10.8 | 11,119 | 6.1 | 9,169 | 6.3 | 693 | 3.6 | 768 | 9.3 | 205 | 4.8 | 147 | 8.6 | 77 | 5.7 | 60 | 11.4 |
| Midwest | 18,580,278 | 25.1 | 46,344 | 25.5 | 37,825 | 25.8 | 4,205 | 21.9 | 2,351 | 28.4 | 1,022 | 23.7 | 499 | 29.2 | 326 | 24.1 | 116 | 22.0 |
| South | 33,736,415 | 45.6 | 97,422 | 53.5 | 78,214 | 53.3 | 11,061 | 57.6 | 4,068 | 49.2 | 2,484 | 57.6 | 717 | 42.0 | 627 | 46.3 | 251 | 47.6 |
| West | 13,315,993 | 18.0 | 26,474 | 14.5 | 20,935 | 14.3 | 3,160 | 16.5 | 1,047 | 12.7 | 583 | 13.5 | 334 | 19.5 | 321 | 23.7 | 94 | 17.8 |
| Unknown | 402,142 | 0.5 | 751 | 0.4 | 605 | 0.4 | 71 | 0.4 | 32 | 0.4 | 21 | 0.5 | 12 | 0.7 | 4 | 0.3 | 6 | 1.1 |
TVH, transvaginal hysterectomy.
Because women contributed varying amounts of time to the population at risk, we report the demographic characteristics of the women weighted by the total person-years that they contributed.
From 2000-2009, we identified a total of 182,110 SUI procedures, among which slings contributed 146,748 procedures followed by the Burch at 19,190 and then, in decreasing order, collagen, laparoscopic procedures, TVH+ colpo-urethrocystopexy, needle suspensions and lastly Kelly plication with only 527 procedures (Table 1). Age at the time of surgery, calendar year of surgery, and region for patients who underwent any SUI procedure , as well as each specific SUI procedure are presented in Table 1. The mean age of women at the time of surgery was 39.5 ± 13.3 years.
The overall rate of any SUI surgery was 246.1 per 100Kpy (95%CI 239.7, 252.6) (Table 2). The rate was highest for slings (198.3 per 100Kpy, 95%CI: 192.8, 203.9). The remainder of the SUI procedures had lower rates. The Burch procedure was the next most common with a rate of 25.9 per 100Kpy (95%CI 24.8, 27.2), followed by collagen/endoscopic injections at 11.2 per 100Kpy (95%CI 10.7, 11.7). Laparoscopic SUI procedures, needle suspensions, TVH+colpo-urethrocystopexies and Kelly plications were relatively uncommon (Table 2). The majority of procedures (62.7%) were performed on an outpatient basis (Table 2). Slings and laparoscopic SUI surgeries were more commonly performed on an outpatient basis, while the Burch procedure and TVH+colpo-cystourethropexies were more commonly performed in the inpatient setting.
Table 2.
Rates and 95% Confidence Intervals of Inpatient and Outpatient Stress Urinary Incontinence Procedures From 2000-2009 in Women Aged 18–64 Years
| Inpatient Procedures |
Outpatient Procedures |
Total Procedures |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Type of SUI surgery | n | Rate* | 95% CI | n | Rate* | 95% CI | n | Rate* | 95% CI |
| Sling | 47,853 | 64.7 | 62.9, 66.5 | 98,895 | 133.6 | 129.7 137.7 | 146,748 | 198.3 | 192.8. 203.9 |
| Burch | 16,229 | 21.9 | 20.9, 23.0 | 2,961 | 4.0 | 3.8, 4.2 | 19,190 | 25.9 | 24.8, 27.2 |
| Collagen | 46 | 0.06 | 0.05, 0.08 | 8,220 | 11.1 | 10.6, 11.6 | 8,266 | 11.2 | 10.7, 11.7 |
| Laparoscopic SUI procedures | 1,371 | 1.9 | 1.7, 2.0 | 2,944 | 4.0 | 3.8, 4.2 | 4,315 | 5.8 | 5.6, 6.1 |
| TVH and colpo-urethrocystopexy | 1,328 | 1.8 | 1.7, 1.9 | 381 | 0.5 | 0.5, 0.6 | 1,709 | 2.3 | 2.2, 2.5 |
| Needle suspension | 765 | 1.0 | 0.9, 1.2 | 590 | 0.8 | 0.7, 0.9 | 1,355 | 1.8 | 1.7, 2.0 |
| Kelly plication | 308 | 0.4 | 0.4, 0.5 | 219 | 0.3 | 0.3, 0.3 | 527 | 0.7 | 0.6, 0.8 |
| Total | 67,900 | 91.7 | 89.2, 94.3 | 114,210 | 154.3 | 150.0, 158.8 | 182,110 | 246.1 | 239.7, 252.6 |
SUI, stress urinary incontinence; CI, confidence interval; TVH, total vaginal hysterectomy.
Rate per 100,000 person-years. TVH, transvaginal hysterectomy.
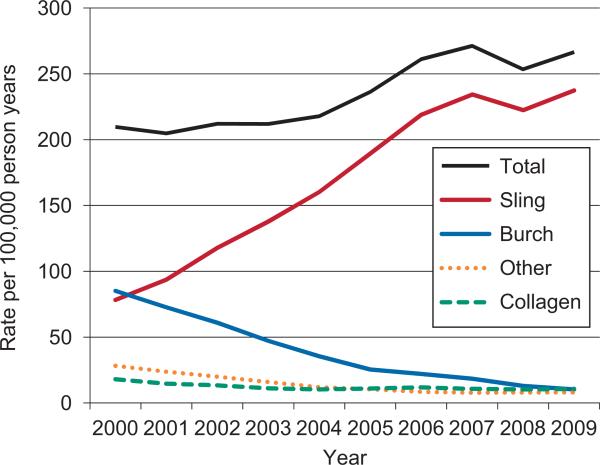
As illustrated in Figure 1, there was a 27% increase in the rate of SUI surgery over the 10-year time period from 209.7 per 100Kpy (95%CI 191.2, 230.0) in 2000 compared to 266.5 per 100Kpy (95%CI 246.0, 288.6) in 2009. This increase in surgeries overall was not the result of a uniform increase in all of the types of procedures but rather an increase in slings in particular. In 2000, the rates for the Burch and sling procedures were comparable (85.2 per 100Kpy [95%CI 76.9, 94.4] and 78.3 per 100Kpy [95%CI 70.1, 87.5], respectively). By 2009, the rate of the Burch had dropped to 10.2 per 100Kpy (95%CI 9.3, 11.3), and the rate for sling had increased to 237.4 per 100Kpy (95%CI 219.1, 257.3). The rates for collagen injection decreased from 18.0 per 100Kpy (95%CI 14.9, 20.7) in 2000 to 10.7 per 100Kpy (95%CI 9.4, 12.2) in 2009. The rate for all other procedures combined (needle suspension, Kelly plication, TVH+ colpo-cystourethrocystopexy and laparoscopic procedures) decreased from 28.2 per 100Kpy (95%CI 25.2, 31.7) in 2000 to 8.1 per 100Kpy (95%CI 7.4, 8.9) in 2009. Thus, in 2009, slings represented 89.1% of all SUI procedures followed by collagen at 4.0%, Burch at 3.8% and all other SUI surgeries combined at 3.0%.
Figure 1.
Annual rates of different types of stress urinary incontinence (SUI) surgery for each year from 2000 to 2009. There was a significant increase in total SUI procedures over the calendar year (P<.001). There was also a significant increase for slings over calendar time (P<.001). For all remaining procedures, there was a significant decrease over calendar time: Burch (P<.001), collagen injection (P=.001), laparoscopic SUI procedures (P<.001), transvaginal hysterectomy with colpo-urethrocystopexy (P<.001), needle suspension (P<.001) and Kelly plication (P<.001).
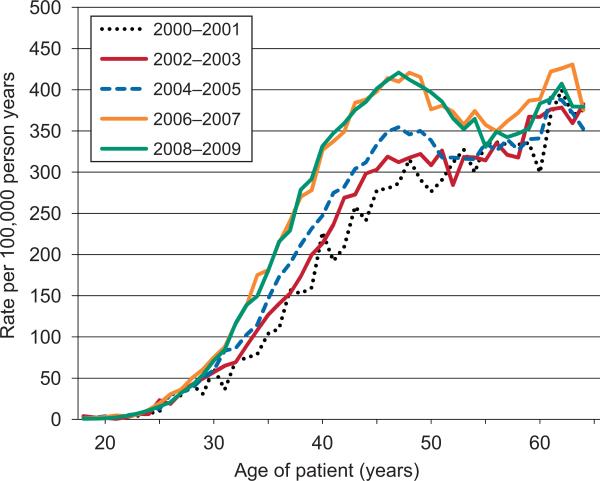
One possible explanation for the observed increase in the total rate of SUI surgery over time was that the population was older, on average, during later time periods and we know that the rate of SUI surgery is higher in older women. To further evaluate whether the increase in the rate for any SUI surgery over time was primarily due to the aging population, we estimated age-adjusted rate ratios (adjRR) comparing each two-year time interval to the rate in 2000-2001. By evaluating the total rate of SUI surgery while controlling for age, we can evaluate the impact of calendar year on surgery rates. After adjusting for age, the rate was not significantly different in 2002-2003 but rates were significantly elevated in each of the subsequent calendar periods. Compared to the rate in 2000-2001, the adjRR in 2002-2003 was 1.06 (95%CI: 0.99, 1.14; p=0.09); the adjRR in 2004-2005 was 1.14 (95%CI: 1.06, 1.22; p=0.0002); the adjRR in 2006-2007 was 1.34 (95%CI: 1.25, 1.43; p<0.0001); and the adjRR in 2008-2009 was 1.31 (95%CI: 1.22,1.39; p<0.0001).
Figure 2 illustrates the age-specific rates by two-year time interval, which is a graphical means of depicting the rate of SUI surgery for women at every specific age and how these rates change from 2000 to 2009. In this figure, we see evidence of the increase in the rate of SUI surgery with age and the increase across calendar time. This figure also indicates that there was a particularly large increase over calendar time in the rate among women aged 35 to 50. For example, between 2000 and 2009, the rate for a 28, 38, 48, and 58 year old changed by - 0.9, 126.2, 96.8, and 13.3 per 100Kpy, respectively.
Figure 2.
Age-specific rates for all of stress urinary incontinence (SUI) surgeries from 2000 to 2009 stratified by two-year intervals. The increase in SUI surgery rate after adjusting for age is not statistically significant when 2002-2003 is compared to 2000-2001 (P=.09). For all subsequent two-year time intervals, there is a significant increase in the SUI surgery rate compared with 2000-2001 (2004-2005, P<.001; 2006-2007, P<.001; 2008-2009, P<.001).
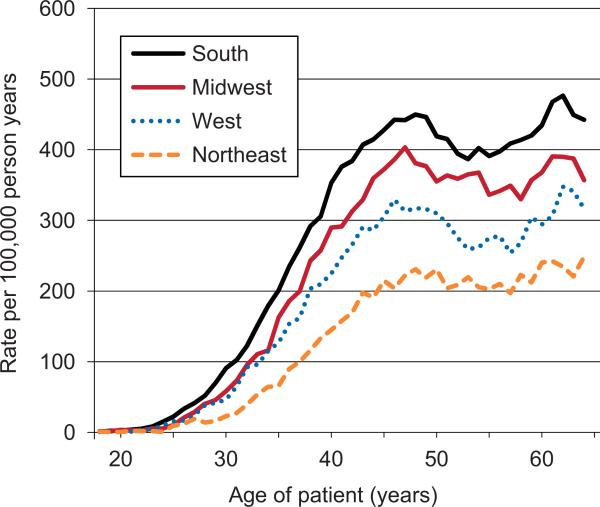
We also observed overall differences in SUI surgery by region of the U.S. In order to assess whether this was driven by differences in the age distribution among the regions, we estimated age-adjusted rate ratios (adjRR) comparing each region to the rate in the Northeast. The age-adjusted rates were significantly elevated in each of the other regions. Compared to the Northeast, the adjRR in the West was 1.44 (95%CI: 1.38, 1.51; p<0.0001); the adjRR in the Midwest was 1.76 (95% CI: 1.68, 1.83; p<0.0001); and the adjRR in the South was 2.09 (95%CI: 2.01, 2.18; p<0.0001). Figure 3 illustrates that the rate was highest in the South and lowest in the Northeast across all ages.
Figure 3.
Age-specific rates for of stress urinary incontinence (SUI) surgery for 2000-2009 stratified by region of the country. After adjusting for age, all regions have significantly higher rates of SUI surgery when compared to the Northeast (P<.001).
DISCUSSION
In women aged 18 to 64, there has been a 27% increase in the rate of surgical management of SUI since 2000. This increase has been accompanied by widespread adoption of the sling, which now dominates all other SUI procedures. Less effective SUI procedures like the Kelly plication (13, 14) and needle suspensions (15) are rarely performed.
In order to further understand what factors underlie the increase in the rate of SUI surgeries, we also evaluated the influence of age and region of the U.S. The increase in the rate of SUI surgery persists even after adjusting for differences in the age distribution over calendar time. Interestingly, the age-specific rates indicate that there has been a dramatic increase in the rate of SUI surgery specifically in women aged 35 to 50 years from 2006-2009 compared to 2000-2005.
Important regional differences in the rates of SUI surgery were also noted, even after adjusting for age. While there are a number of factors that may explain these regional differences including variation in the prevalence of SUI, the fact that the rate is two times higher in the South compared to the Northeast implies the need for future research to explore the underlying reasons for these differences and to evaluate whether over-treatment or under-treatment exists in certain regions of the U.S.
A major strength of this study is the database used. First, this database provides CPT codes for procedures, which are more informative than ICD9 procedure codes which are utilized by other national databases such as the NIS and NHDS. Prior studies on national SUI surgery trends have reported that the most common SUI procedure is ICD9 code 59.79, which represents “other repair of SUI”, a vague description which does not indicate a specific SUI procedure.(6-8, 16) Second, we had the unique ability to calculate enrollment periods in order to estimate rates for SUI procedures, as data regarding population-based rates are quite limited. Third, we were able to identify both inpatient and outpatient procedures (and thus any procedure) from one data source rather than estimating the rate for all SUI procedures using different databases. Finally, the sample represented in this database has good external validity. Specifically, it is more representative of the female population in the U.S. than data obtained from subspecialty centers or specific institutions, as it represents a very large sample of commercially insured women across the United States,.
While the database has unique strengths, there are also several limitations. Because the data are derived from employer-based insurance plans, we do not have information regarding Medicaid or Medicare patients. Our study population included women aged 18 to 64, and we were not able to examine trends in elderly women aged 65 and older. Based on prior published data, the rate of SUI surgery in elderly women has been shown to be higher than those less than 65 years. For example in 2007, the rate of inpatient SUI surgery in elderly women was 123.4 per 100,000 person-years versus 74.8 per 100,000 person-years in women less than 65 years of age.(8) Given this, the national SUI surgery rates for all women are likely to be significantly higher than what we report; however, we provide novel age and procedure-specific rates for SUI surgery for non-elderly women.
We were also not able to evaluate other factors that might be associated with SUI surgery rates, such as race or body mass index, as these characteristics are not captured by this database. Additionally, CPT codes for SUI surgery do not provide detailed information regarding the sling material and the type of sling performed. For example, we cannot distinguish between a traditional bladder neck sling versus a midurethral sling, nor whether the midurethral sling was a retropubic or transobturator procedure. Lastly, our analysis focused on all SUI surgeries performed from 2000-2009 which includes initial as well as repeat SUI surgeries during this time period. Future research could explore rates of repeat surgery and predictors for reoperation.
While slings have become the predominant procedure for treating SUI, they were only FDA-approved in 1998,(9) thus, long-term data are limited. Furthermore, a recent FDA notification in July 2011 highlighted concerns regarding the safety of vaginally placed mesh for prolapse and also stated that “the FDA continues to evaluate the literature for SUI surgeries using surgical mesh and will report about that usage at a later date.”(18) Thus, it will be critical to evaluate the long-term safety and efficacy of slings, particularly for younger women in whom rates of SUI surgery have increased. The fact that the rate of SUI surgery has increased in women aged 35 to 50 raises questions regarding what factors underlie this trend. Does this increase reflect a heightened awareness of and willingness to pursue surgical management? Is the trend due to a greater number of providers performing SUI surgeries especially after the introduction of the midurethral sling? And what will be the long-term implications of a higher rate of slings in younger women? If the FDA reports concerns regarding midurethral slings, there will be dramatic ramifications patients, surgeons, and trainees, who have limited experience with other types of SUI procedures.
In conclusion, we provide evidence that slings are the primary SUI surgery performed in women aged 18 to 64 years and that all other SUI procedures are relatively uncommon as of 2009. The population-based data presented in this study demonstrate valuable information on current practice patterns and offers important insights for training programs and policymakers. Given the FDA's ongoing investigation into the risks of vaginal mesh for SUI surgery, it will be critically important for future research to carefully evaluate the long-term outcomes of slings compared to other stress incontinence surgeries.
Acknowledgements
The authors thank Rebecca G. Fulton for assistance with formatting the figures and tables.
Supported by grant number K02HS017950 from the Agency for Healthcare Research and Quality (AHRQ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. Dr. Wu is supported by K23HD068404, Eunice Kennedy Shriver National Institute of Child Health & Human Development.
Footnotes
Financial Disclosure: The authors did not report any potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Shamliyan T, Wyman J, Bliss DZ, Kane RL, Wilt TJ. Prevention of urinary and fecal incontinence in adults. Evid Rep Technol Assess (Full Rep) 2007 Dec;(161):1–379. [PMC free article] [PubMed] [Google Scholar]
- 2.Tennstedt SL, Fitzgerald MP, Nager CW, Xu Y, Zimmern P, Kraus S, et al. Quality of life in women with stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2007 May;18(5):543–9. doi: 10.1007/s00192-006-0188-5. [DOI] [PubMed] [Google Scholar]
- 3.Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Quality of life and seeking help in women with urinary incontinence. Acta Obstet Gynecol Scand. 2001 Nov;80(11):1051–5. [PubMed] [Google Scholar]
- 4.Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstet Gynecol. 2008 Apr;111(4):899–907. doi: 10.1097/AOG.0b013e31816a1e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001 Sep;98(3):398–406. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 6.Erekson EA, Lopes VV, Raker CA, Sung VW. Ambulatory procedures for female pelvic floor disorders in the United States. Am J Obstet Gynecol. 2010 Aug 24; doi: 10.1016/j.ajog.2010.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliphant SS, Wang L, Bunker CH, Lowder JL. Trends in stress urinary incontinence inpatient procedures in the United States, 1979-2004. Am J Obstet Gynecol. 2009 May;200(5):521, e1–6. doi: 10.1016/j.ajog.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC. Trends in inpatient urinary incontinence surgery in the USA, 1998-2007. Int Urogynecol J. 2011 Nov;22(11):1437–43. doi: 10.1007/s00192-011-1509-x. [DOI] [PubMed] [Google Scholar]
- 9.FDA [November 14, 2011]; 510(K) Number K974098. Jan 28, 1998. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/PMNSimpleSearch.cfm?db=PMN&ID=K974098.
- 10. [December 28, 2011];Thomson Reuters MarketScan® Commercial Claims and Encounters Database, 2000-2009. Source: RED BOOK® and MarketScan® are registered trademarks of Thomson Reuters (Healthcare) Inc. Available from: http://thomsonreuters.com/products_services/healthcare/healthcare_products/pharmaceuticals/mktscan_res_db.
- 11.Pickens G, Moldwin E, Marder WD. [December 28, 2011];Healthcare Spending Index for Private Insurance: Methodology and Baseline Results (White Paper) 2010 November; Available from: http://healthcare.thomsonreuters.com/indexes/assets/HPAYEMP10119145HSI-PIWP_web.pdf.
- 12.McCullagh P, Nelder JA. Generalized Linear Models. Second ed. Chapman and Hall/CRC.; Boca Raton, FL: 1989. [Google Scholar]
- 13.Glazener CM, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database Syst Rev. 2001;(1):CD001755. doi: 10.1002/14651858.CD001755. [DOI] [PubMed] [Google Scholar]
- 14.Bergman A, Elia G. Three surgical procedures for genuine stress incontinence: five-year follow-up of a prospective randomized study. Am J Obstet Gynecol. 1995 Jul;173(1):66–71. doi: 10.1016/0002-9378(95)90171-x. [DOI] [PubMed] [Google Scholar]
- 15.Glazener CM, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database Syst Rev. 2004;(2):CD003636. doi: 10.1002/14651858.CD003636.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Boyles SH, Weber AM, Meyn L. Procedures for urinary incontinence in the United States, 1979-1997. Am J Obstet Gynecol. 2003 Jul;189(1):70–5. doi: 10.1067/mob.2003.376. [DOI] [PubMed] [Google Scholar]
- 17.Subak LL, Richter HE, Hunskaar S. Obesity and urinary incontinence: epidemiology and clinical research update. J Urol. 2009 Dec;182(6 Suppl):S2–7. doi: 10.1016/j.juro.2009.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.FDA Safety Communication [November 14, 2011];Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse (July 13, 2011) doi: 10.1007/s00192-011-1581-2. Available from: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm262435.htm. [DOI] [PubMed]