Abstract
Objectives
To evaluate the efficacy and safety of 2.5 mg and 5 mg mifepristone during 3 months for the treatment of uterine fibroids before surgery.
Design
Multicenter randomized clinical trial.
Locations
Eusebio Hernández Hospital, Havana, Cuba and the Alemán Hospital, Managua, Nicaragua.
Subjects
Included in the study were 146 women with symptomatic uterine fibroids.
Treatment
Group I: half a tablet of 5 mg (2.5 mg) mifepristone taken orally every 24 hours, and Group II: one tablet of 5 mg mifepristone taken orally every 24 hours over a period of 3 months in both groups. Two endometrial biopsies were performed.
Variables to evaluate efficacy
Increase in average hemoglobin, changes in fibroid and uterine volume, and symptomatic improvement.
Results
The average hemoglobin at the end of treatment was 0.6 g/dL greater in the 5 mg mifepristone group (P = 0.033). In both groups there were similar reductions in fibroid volumes. Clinical improvement was more significant in the 5 mg group.
Conclusion
The dose to be used should be 5 mg.
Keywords: mifepristone, leiomyoma, fibroid, antiprogestins
Introduction
Approximately half of women aged 35–49 years have uterine fibroids and almost half of them have heavy bleeding often causing severe anemia.1,2 Every year more than 200,000 hysterectomies due to uterine myomas are performed in the United States.3 The absence of an efficient and safe medication capable of being administered repeatedly contributes to the increase in the number of surgical interventions.
At one time it was thought that only estrogens played a part in the development of uterine myomas, now we know that progesterone also plays its part in their growth and that mifepristone, by inhibiting the latter, influences this development.4–6
Many studies show the efficacy of mifepristone in doses of 50, 25, or 10 mg for the treatment of uterine fibroids, both with respect to reducing the fibroid size and/or improving their symptoms.7–15
There is enough existing scientific evidence to show that low doses of only 5 mg mifepristone are as efficient and safe as those of 10 mg.9,14,16–20
Eisinger et al,21 in a pilot study with only 17 cases and using doses of 2.5 mg, obtained results notably inferior in some respects to those obtained with 5 mg and in other lesser variables results which are similar or close in effectiveness.21 Doses of 2 mg and 5 mg mifepristone were used for contraception by Baird et al.22
The aim of this study was to facilitate surgery by improving hematological conditions and reducing the volume of any such surgery.
Material and methods
Design
This is a multicenter randomized clinical trial to evaluate the efficacy and safety of daily doses of 2.5 mg and 5 mg mifepristone over a 3-month period for treating uterine fibroids before surgery. The clinical trial was carried out in the Eusebio Hernández Hospital in Havana, Cuba and in the Alemán Hospital in Managua, Nicaragua. The study protocol was approved by the respective research committees at each hospital. All subjects gave their informed consent to participate in the study.
The clinical trial was performed in accordance with the revised version of the Declaration of Helsinki (2004) and adhered to good clinical practice standards. The trial began in November 2009 and the last subject included was evaluated in May 2011.
The use of a placebo group was discarded so as not to deprive the subjects of any therapeutic opportunity as there is published evidence that mifepristone in low doses reduces fibroid size, produces relief of associated symptomatology, and improves the general condition of the subject prior to surgery. Subjects were recruited from the hospital gynecological classification consultancies.
Subjects
Women of childbearing age with symptomatic uterine fibroids requiring treatment to improve their general condition before undergoing hysterectomy or myomectomy were eligible for the trial. The inclusion criteria was: (a) symptomatic uterine leiomyomas, (b) indication for surgery (hysterectomy or myomectomy), and (c) agreement to record on a monthly basis all vaginal bleeding episodes, mifepristone side effects, and to have ultrasound examinations at every evaluation session. The exclusion criteria was: (a) pregnancy or the desire to get pregnant, (b) breastfeeding, (c) hormonal contraception or any hormonal therapy in the last 3 months, (d) signs or symptoms of pelvic inflammation, (e) adnexal tumors, (f) suspicion or diagnosis of cervical–uterine or ovarian cancer, (g) signs or symptoms of mental illness, (h) unexplained genital bleeding, (i) anemia due to sickle-cell disease, (j) suffering from a serious illness, and (k) antiprogesterone contraindications. After evaluation of inclusion and exclusion criteria and gathering and submitting all the information needed to participate in the trial, the subjects signed the informed consent.
Treatment
Group I (2.5 mg mifepristone)
Oral administration of half a 5 mg tablet (2.5 mg) of mifepristone every 24 hours for 3 months.
Group II (5 mg mifepristone)
Oral administration of one tablet of 5 mg mifepristone every 24 hours for 3 months.
The mifepristone was supplied by Litaphar Laboratories (Azpeitia, Spain), in individual 5 mg tablets. Treatment began in both groups between the second and fourth days of menstruation. At every evaluation session the subjects were given a phial containing the medication they required up until the next visit and this continued until the end of treatment.
Treatment assignment
The subjects satisfying all requirements were included in the trial in the order they joined it and were assigned to one or other of the treatment groups by means of a random computer-generated list. Centralized in Havana, staff not directly involved in the trial prepared for both participant centers, opaque and sequentially numbered sealed envelopes, each one containing a card indicating “mifepristone 2.5 mg” or “mifepristone 5 mg.” Once the subject had been included, the envelope corresponding to her trial inclusion number was opened and she was assigned to the treatment indicated on the card contained within.
Examinations performed
Complete gynecological examination with pregnancy test, Pap test, and abdominal or vaginal ultrasound examination of the uterus prior to commencement and every 30 days until termination of treatment. Fibroid volume was calculated using the formula: 0.523 × ABC where A, B, and C are the fibroid diameters in each of the three planes and volume is expressed in cubic centimeters.8 If the subject had more than one myoma, measurement was taken of the biggest myoma and its variations were used to evaluate the effect of mifepristone on the fibroid. The total volume of the uterus was calibrated using the previously mentioned formula. Endometrial thickness in millimeters was also measured by ultrasound. All ultrasound calibrations were performed using ultrasound diagnostic equipment (SSD-4000; Aloka Co, Ltd, Mitaka-shi, Tokyo, Japan) and carried out by two ultrasound medical specialists. Measurements taken in the various follow-up periods were carried out without the specialists knowing the results of previous calibrations, they only knew the location of the myoma they had to measure if the subject had more than one fibroid.
Blood samples were taken for hematological studies and liver function at the first visit and every 30 days until termination of treatment. It was decided beforehand that any subject presenting transaminase alterations of values over three times their normal maximum limit, in line with US Food and Drug Administration (FDA) recommendations, would be eliminated from the trial.23
Given the climate of estrogenic predominance stimulated by mifepristone due to the elimination of gestagen action, the risk of endometrial hyperplasias appearing was considered to be greater. To control this phenomenon and/or the appearance of what Mutter et al and Horne and Blithe call “endometrial changes associated to progesterone receptor modulators (PAECs),”24,25 endometrial biopsies were performed before and after treatment only on those subjects who decided not to have surgery for whatever reason. We report the result of the anatomopathological study of the endometrium performed on the subjects’ surgically-removed uterus. An endometrial biopsy was taken during surgery from subjects undergoing myomectomy.
Once treatment was terminated the subjects underwent surgery between 3 and 10 days later. At each visit the subjects were given a form where they were to record bleeding episodes, side effects of mifepristone, and any other relevant information; these forms were handed in at the following visit.
Variables to evaluate efficacy
The main variable for evaluating efficacy was the average hemoglobin (g/dL) at the end of treatment in the 2.5 mg and 5 mg mifepristone groups. It was measured at the beginning and every 30 days until termination of treatment. As secondary variables of efficacy, measurement of the changes registered in the fibroid and uterus dimensions was performed using ultrasound at each evaluative consultancy. Other variables measured were: (a) changes in the prevalence and intensity of pelvic pain and hypermenorrhea, both calibrated by a visual analog scale from 0 to 10 in which 0 represented the absence of symptoms and 10 their maximum value and determined by the subject herself; these symptoms were evaluated prior to commencement of treatment and every 30 days until termination, and (b) changes in the prevalence of pelvic pressure, urinary alterations, rectal and/or lumbar pain, and metrorrhagia which were measured at the beginning of treatment and every 30 days until termination.
We consider metrorrhagia to be the bleeding that occurs between menstrual periods; we consider hypermenorrhea to be menstruation lasting a few days with the subject suffering a greater than normal blood loss. “Pelvic pressure” is the term used by most authors to define a sensation of pressure or something tightening or occupying the pelvis; “irregular bleeding” is considered to be the bleeding incurred during treatment in the form of spotting or bleeding heavier than spotting.
Variables to evaluate safety
The variables to evaluate safety were (a) changes in endometrial thickness measured by ultrasound (mm), (b) side effects of mifepristone: amenorrhea, hot flushes, nausea, dizziness, vomiting, and fatigue, (c) changes in liver transaminase levels: aspartate aminotransferase (AST) and alanine aminotransferase (ALT); these three parameters were evaluated every month until termination of treatment, and (d) frequency of histological endometrial anomalies at the end of treatment.
Number of patients to be included
In administering 5 mg mifepristone over 3 months the average hemoglobin was expected to be 1.0 g/dL higher at the end of treatment in subjects taking 5 mg mifepristone than in those taking 2.5 mg. It was assumed the variances were similar and these were considered equal to 1.6 g/dL, based on other trials with mifepristone in the treatment of uterine fibroids. Working on previous suppositions and so as to guarantee a power of 90% in a two-tailed test with a significance level of 0.05, a minimum sample size of 55 subjects in each treatment group was required.26 The total sample size was increased by approximately 20% (140 patients in all, 70 subjects in each group) in order to counter subject dropouts during treatment.
Statistical analysis
To evaluate the homogeneity of the two participant centers and the treatment groups, use was made of the one-way analysis of variance, the t-test, Pearson’s chi-square test, and the normal approximation for proportions. Analysis of hemoglobin changes was performed using the t-test for independent samples (comparison between the treatment groups) and the t-test for paired samples (comparisons within each mifepristone group). Differences between the treatment groups regarding fibroid and uterine volumes and endometrial thickness in each evaluative period were analyzed by t-test. The t-test was used to analyze pelvic pain and hypermenorrhea in only those subjects who had symptoms prior to treatment. Side effects of mifepristone are presented in descriptive statistical graphs and normal approximation for proportions was used in comparing treatments. In all cases P < 0.05 was considered significant. The data was processed using SPSS software (v. 11.5; SPSS Inc, Chicago, IL).
Results
Inclusion and compliance with the treatment
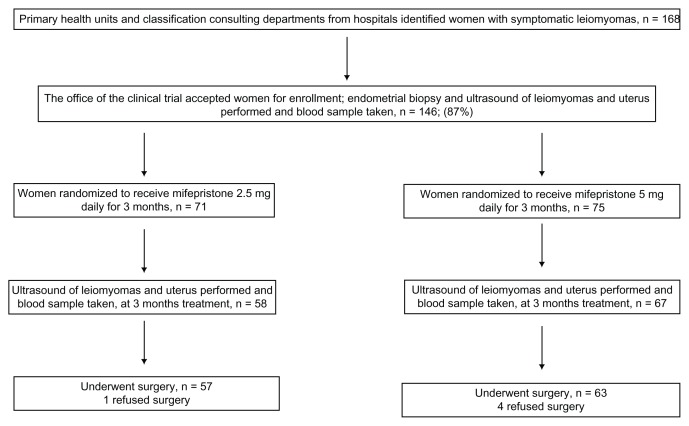
In all, 168 subjects in both centers were referred to the trial, 22 of them failed to satisfy the inclusion criteria. One hundred forty-six of 168 (86.9%) subjects were included, with 71 and 75 in the 2.5 mg and 5 mg mifepristone groups, respectively (see Figure 1).
Figure 1.
Flow chart for the trial.
In Havana, of the 47 subjects included in the 2.5 mg mifepristone group there were nine dropouts: four did not attend the first evaluative consultation, one underwent surgery due to fibroid necrobiosis before completing the first month of treatment, three abandoned treatment in the first month prior to surgery, and one abandoned treatment at the end of the second month. Of the 48 included in the 5 mg group there were two dropouts: one due to surgery for fibroid necrobiosis before completing the first month and the other abandoned the trial in the second month of treatment.
In Managua, of the 24 subjects included in the 2.5 mg group there were three dropouts: two abandoned treatment between the second and third month and one dropped out due to heavy bleeding during the first month of treatment with mifepristone. Of the 27 included in the 5 mg group there were two dropouts: one due to fibroid expulsion in the first month and one due to elevated transaminases after 1 month of treatment (60 and 72 IU of AST and ALT), respectively. In total, in the two centers there were twelve of 71 (16.9%) and four of 75 (5.3%) dropouts in the 2.5 mg and 5 mg groups, respectively (P = 0.01). Data was processed in an “intention-to-treat basis” and the information on patients who abandoned the trial is included in the results in the evaluative periods in which they took mifepristone.
Initial variables and comparison between treatment groups
Table 1 shows the general characteristics of all the subjects included in the clinical trial. There were no significant differences between the treatment groups for any of them. Nor were there significant differences between the centers save for two exceptions; there were significantly (P < 0.001) less black subjects in Managua, two of 51 (3.9%), than in Havana, 34 of 95 (35.8%); the fibroid volumes in the subjects in Managua were 2.1 times less than in the patients in Havana (P = 0.003); and there were no significant differences in the average uterine volumes between the participant centers, nor between the mifepristone groups. No subject was diagnosed with fibroid-associated sterility. There were 15 of 71 (21.1%) and 19 of 75 (25.3%) subjects with only one myoma in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.274), and no significant differences between the participant centers (P > 0.05). In total, the fibroids studied were made up as follows: 30 of 146 (20.6%) subserous, six of 146 (4.1%) submucous, and 110 of 146 (75.3%) intramural, and there were no significant differences between the mifepristone groups (P = 0.165).
Table 1.
Subject characteristics by mifepristone group
| Characteristics | 2.5 mg (n = 71) | 5 mg (n = 75) |
|---|---|---|
| Age | 42.3 ± 5.8 | 42.0 ± 6.7 |
| Body mass index (kg/m2) | 26.2 ± 4.5 | 27.2 ± 4.8 |
| Gravidity | 3.3 ± 1.9 | 3.1 ± 1.8 |
| Parity | 2.0 ± 1.1 | 2.1 ± 1.4 |
| Abortion | 1.8 ± 1.8 | 1.8 ± 1.3 |
| Fibroids volume (mL) | 106 ± 156 | 115 ± 114 |
| Uterine volume (mL) | 426 ± 323 | 527 ± 373 |
| Endometrial thickness (mm) | 6.7 ± 2.1 | 7.3 ± 2.7 |
| Aspartate aminotransferase (IU) | 22.6 ± 8.7 | 20.5 ± 9.8 |
| Alanine aminotransferase (IU) | 21.7 ± 10.1 | 20.2 ± 10.9 |
| Hemoglobin (g/dL) | 10.7 ± 2.2 | 10.9 ± 1.6 |
| Hemoglobin (<10.0 g/dL) | 23 (32.4) | 18 (24.0) |
| Race | ||
| White | 23 (32.4) | 18 (24.0) |
| Black | 18 (25.4) | 18 (24.0) |
| Afro-Cuban | 30 (42.0) | 39 (52.0) |
Note: Data presented as averages ± standard deviation+ or n(%).
Once treatment was over, surgery was refused by four of 63 (6.3%) of the 5 mg group in Havana and one of 24 (4.2%) of the 2.5 mg group in Managua (P = 0.348).
Efficacy
The average hemoglobin levels at the end of treatment were 11.3 ± 1.7 and 11.9 ± 1.1 g/dL in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.033). In the 2.5 mg group the initial hemoglobin average was 10.7 ± 2.2 g/dL and the final one was 11.3 g/dL (P = 0.03); in the 5 mg group the initial hemoglobin average was 10.9 g/dL and the final average was 11.9 ± 1.1 g/dL (P < 0.001).
Prior to treatment the percentages of subjects with hemoglobin < 10.0 g/dL were 23 of 71 (32.4%) and 18 of 75 (24.0%) in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.13); there were no significant differences between the centers and treatment groups. Thirty days after beginning treatment there were 20 of 59 (33.9%) and 15 of 65 (23.1%) subjects with hemoglobin < 10.0 g/dL in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.091). Two months into treatment the subjects with hemoglobin <10.0 g/dL were 14 of 54 (24.6%) and ten of 65 (15.4%) in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.077).
At the end of treatment, there were seven of 50 (14%) and three of 63 (4.8%) subjects with hemoglobin < 10.0 g/dL in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.043). In the 2.5 mg group, the percentage of subjects with <10.0 g/dL hemoglobin levels was significantly reduced by the end of treatment (P = 0.011), and in the 5 mg mifepristone group it was very significant (P < 0.001). At the end of treatment, the proportion of subjects with hemoglobin > 10.0 g/dL in the 5 mg group in Nicaragua was significantly greater than in the 2.5 mg group in Havana (P = 0.013); in the remaining comparisons there were no significant differences.
Tables 2 and 3 compare the dimensional changes in fibroid and uterine volumes during the trial evaluative periods for the subjects with the relevant observations. Three months into treatment fibroid volume was not reduced, compared to its initial value, in six of 48 (12.5%) and five of 60 (8.3%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.238). At the end of treatment, compared to pretreatment values, uterine volume was not reduced in 14 of 48 (29.2%) and 16 of 60 (26.7%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.387).
Table 2.
Changes in fibroid measurements (cm3) by treatment groups
| Evaluation | Group | n | Mean ± standard deviation | 95% confidence interval for mean | Cumulative reduction+ | P* |
|---|---|---|---|---|---|---|
| Before treatment | 2.5 mg | 48 | 119 ± 107 | 87–150 | 0.402 | |
| 5 mg | 60 | 140 ± 144 | 103–177 | |||
| 1 month treatment | 2.5 mg | 48 | 87 ± 95 | 59–114 | 26.7% | 0.917 |
| 5 mg | 60 | 85 ± 102 | 60–112 | 39.3% | ||
| 2 months treatment | 2.5 mg | 48 | 75 ± 75 | 54–97 | 36.9% | 0.853 |
| 5 mg | 60 | 72 ± 90 | 50–96 | 48.6% | ||
| 3 months treatment | 2.5 | 48 | 73 ± 82 | 49–96 | 38.7% | 0.556 |
| 5 mg | 60 | 64 ± 76 | 44–84 | 54.3% |
Notes:
t-test (analysis of variance);
concerning value before treatment in the same group.
Table 3.
Changes in uterine measurements (cm3) by treatment groups
| Evaluation | Group | n | Mean ± standard deviation | 95% confidence interval for mean | Cumulative reduction+ | P* |
|---|---|---|---|---|---|---|
| Before treatment | 2.5 mg | 48 | 384 ± 246 | 313–456 | 0.019 | |
| 5 mg | 60 | 538 ± 390 | 437–639 | |||
| 1 month treatment | 2.5 mg | 48 | 377 ± 297 | 292–464 | 1.8% | 0.228 |
| 5 mg | 60 | 449 ± 314 | 368–530 | 16.5% | ||
| 2 months treatment | 2.5 mg | 48 | 359 ± 375 | 286–504 | 6.5% | 0.866 |
| 5 mg | 60 | 369 ± 233 | 308–429 | 31.4% | ||
| 3 months treatment | 2.5 mg | 48 | 347 ± 267 | 270–425 | 9.6% | 0.295 |
| 5 mg | 60 | 407 ± 357 | 314–499 | 24.3% |
Notes:
t-test (analysis of variance);
concerning value before treatment in the same group.
Table 4 shows the changes in fibroid symptom prevalence before treatment and at each evaluative period. Tables 5 and 6 show the changes in the prevalence and intensity of pelvic pain and hypermenorrhea.
Table 4.
Prevalence of fibroid symptoms before, after 30, 60, and 90 days treatment by groups
| Treatment | P* | ||
|---|---|---|---|
|
|
|||
| 2.5 mg | 5 mg | ||
| Pelvic pain | |||
| Before treatment | 56 (83.1) | 60 (80.0) | 0.315 |
| 30 days after | 29 (48.3) | 35 (52.2) | 0.330 |
| 60 days after | 23 (41.8) | 24 (36.9) | 0.292 |
| 90 days after | 19 (38.0) | 13 (21.3) | 0.023 |
| Pelvic pressure | |||
| Before treatment | 46 (64.8) | 48 (64.0) | 0.460 |
| 30 days after | 30 (50.0) | 23 (34.3) | 0.037 |
| 60 days after | 20 (36.4) | 13 (20.0) | 0.023 |
| 90 days after | 16 (32.0) | 14 (23.0) | 0.143 |
| Urinary symptoms | |||
| Before treatment | 45 (63.4) | 47 (62.7) | 0.464 |
| 30 days after | 30 (50.0) | 34 (50.7) | 0.467 |
| 60 days after | 23 (41.8) | 20 (30.8) | 0.104 |
| 90 days after | 11 (22.0) | 13 (21.3) | 0.465 |
| Lumbar pain | |||
| Before treatment | 56 (78.9) | 52 (69.3) | 0.095 |
| 30 days after | 28 (46.7) | 35 (52.2) | 0.265 |
| 60 days after | 25 (45.5) | 22 (33.8) | 0.097 |
| 90 days after | 20 (40.0) | 15 (24.6) | 0.041 |
| Rectal pain | |||
| Before treatment | 30 (42.2) | 28 (37.3) | 0.272 |
| 30 days after | 13 (21.7) | 10 (16.7) | 0.162 |
| 60 days after | 10 (18.2) | 5 (7.7) | 0.042 |
| 90 days after | 5 (10.0) | 2 (3.3) | 0.074 |
| Dispareunia | |||
| Before treatment | 35 (49.3) | 35 (46.7) | 0.375 |
| 30 days after | 15 (25.0) | 21 (31.3) | 0.214 |
| 60 days after | 11 (20.0) | 11 (16.9) | 0.332 |
| 90 days after | 8 (16.0) | 2 (3.3) | 0.009 |
| Hypermenorrhea | |||
| Before treatment | 61 (85.9) | 63 (84.0) | 0.373 |
| 30 days after | 28 (46.7) | 26 (38.8) | 0.186 |
| 60 days after | 11 (20.0) | 5 (7.7) | 0.024 |
| 90 days after | 4 (8.0) | 5 (8.2) | 0.485 |
| Metrorrhagia | |||
| Before treatment | 24 (33.8) | 35 (46.7) | 0.057 |
| 30 days after | 7 (11.7) | 12 (17.9) | 0.162 |
| 60 days after | 3 (5.5) | 2 (3.1) | 0.258 |
| 90 days after | 4 (8.0) | 1 (1.6) | 0.054 |
Notes: Data presented as n(%);
Normal approximation for proportions.
Table 5.
Changes in pelvic pain intensity during evaluation
| Treatment | ||||
|---|---|---|---|---|
|
|
||||
| Start | 30 days | 60 days | 90 days | |
| n | (n = 60; n = 59) | (n = 44; n = 52) | (n = 44; n = 52) | (n = 44; n = 52) |
| 2.5 mg | 6.9 ± 2.9 | 3.6 ± 3.9 | 2.4 ± 3.5 | 2.0 ± 3.0 |
| Reduction (%) | – | 47.8 | 65.2 | 71.0 |
| 5 mg | 7.0 ± 2.5 | 2.9 ± 3.1 | 2.1 ± 3.1 | 1.0 ± 2.3 |
| Reduction (%) | – | 58.6 | 70.0 | 85.7 |
| P* | 0.813 | 0.325 | 0.564 | 0.079 |
Note:
corresponds to comparison between treatment groups.
Table 6.
Changes in hypermenorrhea intensity during evaluation
| Treatment | ||||
|---|---|---|---|---|
|
|
||||
| Start | 30 days | 60 days | 90 days | |
| n | (n = 43; n = 55) | (n = 43; n = 55) | (n = 43; n = 55) | (n = 43; n = 55) |
| 2.5 mg | 8.5 ± 2.5 | 3.4 ± 4.0 | 1.5 ± 3.1 | 0.5 ± 1.9 |
| Reduction (%) | – | 60.0 | 82.4 | 94.1 |
| 5 mg | 8.8 ± 2.0 | 3.2 ± 3.9 | 0.3 ± 1.2 | 0.3 ± 1.1 |
| Reduction (%) | – | 63.6 | 96.6 | 96.6 |
| P* | 0.454 | 0.866 | 0.024 | 0.455 |
Note:
corresponds to comparison between treatment groups.
Side effects of mifepristone
There was amenorrhea in 28 of 60 (46.7%) and 35 of 67 (52.2%), 39 of 55 (70.1%) and 54 of 65 (83.1%), 42 of 50 (84.0%) and 58 of 63 (92.0%), subjects in the 2.5 mg and 5 mg groups at the consultations after 30, 60, and 90 days (P = 0.265, P = 0.056, and P = 0.091), respectively.
Hot flushes were reported at least once during treatment by 14 of 24 (51.9%) and ten of 27 (37.0%) subjects in the 2.5 mg and 5 mg groups in Managua, respectively (P = 0.064); hot flushes were reported in the three evaluative consultations by 14 subjects, seven in each mifepristone group.
Hot flushes were reported at least once during treatment by nine of 38 (23.6%) and six of 42 (14.3%) in the 2.5 mg and 5 mg groups in Havana, respectively (P = 0.141). Hot flushes were reported in the three evaluative consultations by one subject in the 2.5 mg group and by none in the 5 mg group.
In total, in both centers hot flushes were reported at least once during treatment by 23 of 62 (37.1%) and 16 of 69 (23.2%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.041); hot flushes were reported in the three evaluative consultations by eight and seven subjects in the 2.5 mg and 5 mg mifepristone groups, respectively.
At some point during treatment the following side effects of mifepristone were reported: (a) nausea by four of 50 (8.0%) and four of 63 (6.3%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.367); (b) vomiting by two of 50 (4.0%) and two of 63 (3.2%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.42); (c) feeling of fatigue by twelve of 50 (24.0%) and seven of 63 (11.1%) subjects in the 2.5 mg and 5 mg groups, respectively (P = 0.034).
During the treatment period there were four of 71 (5.6%) subjects in the 2.5 mg mifepristone group with elevated liver transaminase levels: between 47 and 78 IU for AST and between 51 and 62 IU for ALT, (reference levels 46 and 49 for AST and ALT, respectively). In the 5 mg group there were six of 75 (8.1%) elevated transaminases: between 51 and 72 IU for AST and between 53 and 62 for ALT.
Table 7 shows changes in endometrial thickness during treatment.
Table 7.
Changes in endometrial thickness (mm) by treatment groups
| Evaluation | Group | n | Mean ± standard deviation | Increment+ | P* |
|---|---|---|---|---|---|
| Before treatment | 2.5 mg | 48 | 6.8 ± 2.0 | 0.098 | |
| 5 mg | 60 | 7.6 ± 2.8 | |||
| 1 month treatment | 2.5 mg | 48 | 7.8 ± 3.0 | 14.7% | 0.873 |
| 5 mg | 60 | 7.9 ± 3.4 | 3.9% | ||
| 2 months treatment | 2.5 mg | 48 | 8.5 ± 2.9 | 25.0% | 0.001 |
| 5 mg | 60 | 10.9 ± 3.8 | 43.4% | ||
| 3 months treatment | 2.5 | 48 | 9.4 ± 3.7 | 38.2% | 0.267 |
| 5 mg | 60 | 10.3 ± 4.5 | 35.5% |
Notes:
t-test (analysis of variance);
concerning value before treatment in the same group.
Between the beginning and end of treatment, irregular vaginal bleeding at some time was reported by 19 of 63 (30.1%) and eleven of 67 (16.4%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.032); the average number of days was: 6.3 ± 5.1 and 5.4 ± 4.1 in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.601). Over the 3 months of treatment some spotting was reported by 29 of 63 (46.0%) and 20 of 67 (29.8%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.029); the average number of days was: 8.0 ± 7.1 and 6.3 ± 5.9 in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.599). In total, there was irregular bleeding (spotting and/or blood) in 32 of 63 (50.8%) and 21 of 67 (31.3%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.012); the average duration was 11.0 ± 10.6 and 8.8 ± 8.9 days in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.437).
Endometrial biopsy
In the endometrial biopsies before and after treatment there was no diagnosis of simple hyperplasia, atypical or not, nor was any other pathology found and there were no significant differences between the two mifepristone groups. In the posttreatment endometrial biopsies eleven of 125 (8.8%) were found to be of no diagnostic use; in the 114 with valid results there were 16 of 56 (28.6%) and 14 of 58 (24.1%) PAECs in the 2.5 mg and 5 mg groups, respectively (P = 0.296). The remaining diagnoses in both groups were compatible with secretory or proliferating endometria.
Surgery
In all, hysterectomies were performed with or without double adnexectomy on 51 of 57 (89.5%) and 59 of 63 (93.7%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.204). In six of 57 (10.5%) and four of 63 (6.3%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively, myomectomies were performed. In the subjective evaluation of intraoperative bleeding this was considered to be “less than usual” in 20 of 57 (35.1%) and 30 of 63 (47.6%) in the cases in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.082).
The surgeons considered surgery to be “easier than usual” in eight of 57 (14.0%) and 23 of 63 (36.5%) subjects in the 2.5 mg and 5 mg mifepristone groups, respectively (P = 0.002). The average postoperative stay in hospital for subjects in Cuba was 3.4 ± 5.4 and 1.4 ± 0.8 days in the 2.5 mg and 5 mg groups, respectively (P = 0.046). In those in Nicaragua, the average postoperative stay in hospital was 2.5 ± 1.8 and 3.3 ± 2.8 days in the 2.5 mg and 5 mg groups, respectively (P = 0.345). In Table 8 we have presented some surgery data according to mifepristone groups.
Table 8.
Some surgery data by mifepristone group
| Surgery data | Group | n | Mean | Standard deviation | Min | Max | P |
|---|---|---|---|---|---|---|---|
| Postsurgery stay in hospital | 2.5 mg | 57 | 2.1 | 3.8 | 1 | 24 | 0.712 |
| 5 mg | 63 | 1.9 | 1.9 | 1 | 11 | ||
| Hemoglobin before surgery | 2.5 mg | 57 | 11.4 | 1.5 | 8.0 | 14.0 | 0.404 |
| 5 mg | 63 | 11.6 | 1.1 | 9.0 | 14.5 | ||
| Hemoglobin after surgery | 2.5 mg | 57 | 10.9 | 1.4 | 7.0 | 14.0 | 0.436 |
| 5 mg | 63 | 11.1 | 1.4 | 8.0 | 14.5 | ||
| Length of surgery (min) | 2.5 mg | 57 | 95.5 | 35.4 | 43 | 178 | 0.173 |
| 5 mg | 63 | 87.4 | 29.2 | 35 | 148 | ||
| Intraoperative bleeding (mL) | 2.5 mg | 57 | 500 | 216 | 100 | 1000 | 0.981 |
| 5 mg | 63 | 499 | 239 | 100 | 1000 |
Note: Data presented as averages ± standard deviation.
Discussion
This multicenter trial presents some differences in the subjects included: (1) the size of the fibroids is 2.2 times smaller in Nicaragua, and (2) the percentage of black subjects is much less in Nicaragua. In the latter study the subject age is on average 3 years older than in our previous studies.16–19
Despite the difference in the final hemoglobin levels between both groups being significant, it is only 0.5 g/dL, which, from a clinical point of view, is not especially important when the data is interpreted together, but it is important when analyzed separately: for example, the more serious anemic subjects with less than 10 g/dL. In that subgroup the improvement is much greater and faster than in the 5 mg group (P = 0.04).
Doubtlessly, this improvement is related to the percentages of amenorrhea in each group which, although not presenting significant differences, except in the second month, when at the limit of statistical significance (P = 0.056), do observe a tendency towards greater percentages of amenorrhea in the 5 mg group, which might be significant with greater sample sizes. Our percentages of amenorrhea are superior to those obtained by Eisenger et al in the only study carried out to date with 2.5 mg which reaches only 65% after 3 months of treatment.21
This tendency is also observed to an even greater degree in the percentage of subjects having irregular bleeding (blood + spotting) which is always significantly less in the 5 mg group (P = 0.012). And although the difference is not significant the average duration of days with bleeding is also less (P = 0.437).
Table 4 shows that the 5 mg group as a whole experiences a significantly greater clinical improvement at the end of treatment, this greater clinical efficacy can be seen particularly in pelvic pressure, rectal pain, and hypermenorrhea; that is to say, the subjects in the 5 mg group improve faster even when this clinical improvement levels out in both treatment groups in only one part of their symptoms. The same thing happens with the intensity in hypermenorrhea in the second month of treatment which is significantly lower in the 5 mg group (P = 0.02) (Table 6).
These differences are probably behind the greater number of dropouts in the 2.5 mg group (twelve of 71, 16.9%) compared with (four of 75, 5.3%) in the 5 mg group (P = 0.01). This is similar to the results obtained by Eisinger et al who also reports a high level of dropouts (26%) when using a 2.5 mg dosage.21
A greater efficacy in the 5 mg mifepristone group may also be indicated by the submucous fibroid being expelled at the end of the first month of treatment as well as by the greater number of cases that refused to undergo surgery.
The same is not the case with other secondary variables: fibroid volume, to name one, since the percentages in fibroid volume reduction in both treatment groups do not differ significantly at the end of treatment (P = 0.55), although there is a marked tendency in major fibroid volume reductions in the 5 mg group which would probably become significant were the sample size increased. The same applies to uterine volume (P = 0.34).
The 9.6% reduction in uterine volume obtained in the 2.5 mg group in this trial is similar to the 11% obtained by Eisinger et al21 in their study with 2.5 mg, but quite a lot lower than the average percentages in reduction obtained with a 5 mg dosage in other studies.16–19 There cannot be said to be a direct linear causal relationship between reduction in fibroid size and clinical improvement as, for example, in our previous trials there are approximately 20% of cases whose fibroids do not decrease and nevertheless do experience a clinical improvement and the same thing happens in the present trial.13–17,19 Something similar occurs in the study by Engman et al.8
With regard to safety, the elevated transaminases are low percentage-wise and of minimum clinical significance since the levels never rise above 100 IU at most. These percentages are similar to other studies.8,9,14,16–20
The side effects produced by mifepristone are similar in both groups, including the hot flushes which are the only substantial mifepristone side effect. It should be pointed out that the high prevalence of hot flushes (24% and 21.3% in the 2.5 mg and 5 mg groups, respectively) obtained in this trial is basically due to their greater incidence in the subjects in Nicaragua, hovering around the 50% mark, given that in the subjects in Cuba it is the same as in previous trials, around 10%. We believe that there is some bias in collecting data on this symptom in the Nicaraguan center. Although the intensity of hot flushes has never been studied, the impression the researchers have is that they are of an intensity, duration, and frequency much greater than those of the physiological menopause or those brought on by gonadotropin-releasing hormone analogs. Moreover, in none of our four clinical trials published,16–19 which included around 400 subjects, has there been a single case of dropout from treatment due to hot flushes nor has treatment for such been requested.
The increase in endometrial thickness derived from the estrogenic predominance triggered by mifepristone shows no significant differences between the two treatment groups (P = 0.26), the average end-of-treatment values not being excessively over the permitted physiological limit of 8 mm.
When analyzing the surgical data of the Cuba subgroup, one is struck by the significant differences in the average postoperative hospital stay (P = 0.046). With regard to surgical variables logically, there were no differences between the various surgical parameters studied since these could only have been evident had they been compared to a group that did not receive mifepristone, ie, a placebo group. In this case significant differences would certainly have been observed between the sizes of the removed fibroid or uterus, ease of surgery, or blood loss.
The results of the posttreatment endometrial biopsies do not include any simple hyperplasia, atypical or not, being within the classical diagnostic categories or those recently established by Mutter and Horne, or PAECs24,25 for endometria under the effect of progesterone receptor modulators like mifepristone. There are no significant differences between the two treatment groups. The percentages of histological changes of the PAEC type are similar to those obtained by Fiscella et al.27 This could represent a threshold effect; perhaps differences in features would appear at doses lower than 2.5 mg. The histological changes found in the present trial are similar to those observed with other progesterone receptor modulators like CDB-4124.28
When compared with other progesterone receptor modulators like ulipristal that have proved their efficacy in this field, our results are similar to those obtained with this medicine.29,30
So, therefore, this new therapeutic technique for uterine fibroids offers us an ongoing medical (as opposed to surgical) treatment. A treatment cycle administered periodically according to the subject’s individual response until the onset of the menopause. The data obtained in other studies indicate that this therapeutic technique could be viable.7–21
One of the weak points of this trial is not evaluating the impact on quality of life which is shown to have increased in the study by Eisinger with a dosage of 2.5 mg mifepristone.21 As this trial ended with hysterectomies and there was no plan to repeat treatment in the foreseeable future, it was not deemed important to evaluate this aspect.
By way of conclusion we could say that: (1) the difference in efficacy between the two doses is not huge, since both achieve reductions in fibroid and uterine volumes, symptomatic improvement, and have minimal side effects, and (2) the 5 mg dose presents the following advantages: (a) slightly greater symptomatic improvement, (b) greater speed in the onset of this improvement, (c) significant difference in the normalization of hemoglobin levels, (d) significantly less irregular bleeding, and (e) significantly lower number of dropouts from treatment. Part (c) is particularly important when the subject finally comes to surgery as it enables her to undergo an operation in better hematological shape thus decreasing the chances of blood transfusions. Therefore, for these reasons, in our opinion, the dose to be used in future should be 5 mg.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Day BD, Dunson DB, Hill MC, Coousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1):100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 2.Wegienka G, Baird DD, Hertz-Piccioto I, et al. Self-reported heavy bleeding associated with uterine leiomyomata. Obstet Gynecol. 2003;101(3):431–437. doi: 10.1016/s0029-7844(02)03121-6. [DOI] [PubMed] [Google Scholar]
- 3.Wilcox LS, Koonin LM, Pokras R, Strauss LT, Xia Z, Peterson HB. Hysterectomy in the United States, 1988–1990. Obstet Gynecol. 1994;83(4):549–555. doi: 10.1097/00006250-199404000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Wilson EA, Yang F, Reese E. Estradiol and progesterone binding in uterine leiomyomata and in normal uterine tissues. Obstet Gynecol. 1980;55(1):20–24. [PubMed] [Google Scholar]
- 5.Andersen J. Factors in fibroid growth. Baillieres Clin Obstet Gynaecol. 1998;12(2):225–243. [PubMed] [Google Scholar]
- 6.Reim MS, Barbier RL, Friedman AJ. Progesterone: a critical role in the pathogenesis of uterine myoma. Am J Obstet Gynecol. 1995;172(1 Pt 1):14–18. doi: 10.1016/0002-9378(95)90077-2. [DOI] [PubMed] [Google Scholar]
- 7.Steinauer J, Pritts EA, Jackson R, Jacoby A. Systematic review of mifepristone for the treatment of uterine leiomyomata. Obstet Gynecol. 2004;103(6):1331–1336. doi: 10.1097/01.AOG.0000127622.63269.8b. [DOI] [PubMed] [Google Scholar]
- 8.Engman M, Granber S, Williams AR, Meng CX, Lalitkumar PG, Gemzell-Danielsson K. Mifepristone for treatment of uterine leiomyoma. A prospective randomized placebo controlled trial. Hum Reprod. 2009;24(8):1870–1879. doi: 10.1093/humrep/dep100. [DOI] [PubMed] [Google Scholar]
- 9.Eisinger SH, Meldrum S, Fiscella K, le Roux HD, Guzick DS. Low-dose mifepristone for uterine leiomyomata. Obstet Gynecol. 2003;101(2):243–250. doi: 10.1016/s0029-7844(02)02511-5. [DOI] [PubMed] [Google Scholar]
- 10.Alvarez-Murphy AA, Kettel LM, Morales AJ, Roberts VJ, Yen SS. Regression of uterine leiomyomata in response to the antiprogesterone RU 486. J Clin Endocrinol Metabol. 1993;76(2):513–517. doi: 10.1210/jcem.76.2.8432797. [DOI] [PubMed] [Google Scholar]
- 11.Reinsch RC, Murphy AA, Morales AJ, Yen SS. The effects of RU 486 and leuprolide acetate on uterine artery blood flow in the fibroid uterus: a prospective, randomized study. Am J Obstet Gynecol. 1994;170(6):1623–1628. [PubMed] [Google Scholar]
- 12.Yang Y, Zheng S, Li K. Treatment of uterine leiomyomata by two different doses of mifepristone. Zhonghua Fu Chan Ke Za Zhi. 1996;31(10):624–626. Chinese. [PubMed] [Google Scholar]
- 13.Zeng C, Gu M, Huang H. A clinical control study on the treatment of uterine leiomyomata with gonadotropin releasing hormone agonist or mifepristone. Zhonghua Fu Chan Ke Za Zhi. 1998;33(8):490–492. Chinese. [PubMed] [Google Scholar]
- 14.Eisinger SH, Bonfiglio T, Fiscella K, Meldrum S, Guzick D. Twelve-month safety and efficacy of low-dose mifepristone for uterine myomas. J Min Invasiv Gynecol. 2005;12(3):227–233. doi: 10.1016/j.jmig.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 15.Bagaria M, Suneja A, Vaid NB, Guleria K, Mishra K. Low-dose mifepristone in treatment of uterine leiomyoma: a randomized double-blind placebo-controlled trial. Aust NZJ Obstet Gynecol. 2009;49(1):77–83. doi: 10.1111/j.1479-828X.2008.00931.x. [DOI] [PubMed] [Google Scholar]
- 16.Carbonell JL, Acosta R, Heredia B, Pérez Y, Yero MC, Valle A. Mifepristone for the treatment of uterine leiomyomas: a randomized controlled trial. Obstet Gynecol. 2008;112(5):1029–1036. doi: 10.1097/AOG.0b013e31818aa930. [DOI] [PubMed] [Google Scholar]
- 17.Carbonell JL, Quiróz Rámirez GM, Borge A, Castellón Zapata LE, Cuadra Aragón W, Giuseppe Tomasi G. Mifepristone 5 mg versus 10 mg daily for treatment of leiomyoma. Prog Obstet Gynecol. 2009;10:1–8. [Google Scholar]
- 18.Carbonell JL, Acosta R, Heredia B, et al. Evolution of uterine leiomyoma after treatment with mifepristone: a randomized clinical trial. Prog Obstet Ginecol. 2010;53(6):231–236. [Google Scholar]
- 19.Carbonell JL, Acosta R, Heredia B, et al. Mifepristone for treatment of uterine fibroids. Rev Cub Gynecol Salud Reprod. 2010;36(2):236–250. [Google Scholar]
- 20.Fiscella K, Eisinger SH, Meldrum S, et al. Effect of mifepristone for symptomatic leiomyomata on quality of life and uterine size: a randomized controlled trial. Obstet Gynecol. 2006;108(6):1381–1387. doi: 10.1097/01.AOG.0000243776.23391.7b. [DOI] [PubMed] [Google Scholar]
- 21.Eisinger SH, Fiscella J, Bonfiglio T, Meldrum S, Fiscella K. Open-label study of ultra low-dose mifepristone for the treatment of uterine leiomyomata. Eur J Obstet Gynecol. 2009;146(2):215–218. doi: 10.1016/j.ejogrb.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Baird DT, Brown A, Critchley HO, Williams AR, Lin S, Cheng L. Effect of long-term treatment with low-dose mifepristone on the endometrium. Hum Reprod. 2003;18(1):61–68. doi: 10.1093/humrep/deg022. [DOI] [PubMed] [Google Scholar]
- 23.Guidance for Industry. Drug-Induced Liver Injury: Premarketing Clinical Evaluation. US Department of Health and Human Services; Jul, 2009. [Accessed February 13, 2012]. Available from: http://www.ccd.org.cn/ccd/fs/web_edit_file/20090807144518.pdf. [Google Scholar]
- 24.Mutter GL, Bergeron C, Deligdisch L, et al. The spectrum of endometrial pathology induced by progesterone receptor modulators. Mod Pathol. 2008;21(5):591–598. doi: 10.1038/modpathol.2008.19. [DOI] [PubMed] [Google Scholar]
- 25.Horne FM, Blithe DL. Progesterone receptor modulators and the endometrium: changes and consequences. Hum Reprod Update. 2007;13(6):567–580. doi: 10.1093/humupd/dmm023. [DOI] [PubMed] [Google Scholar]
- 26.Faul F. G*Power version 3.0.10. Kiel, Germany: Universitat Kiel; 2008. [Google Scholar]
- 27.Fiscella F, Bonfiglio T, Winters P, Eisinger SH, Fiscella K. Distinguishing features of endometrial pathology after exposure to the progesterone receptor modulator mifepristone. Hum Pathol. 2011;42(7):947–953. doi: 10.1016/j.humpath.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ioffe OB, Zaino RJ, Mutter GL. Endometrial changes from short-term therapy with CDB-4121, a selective progesterone receptor modulator. Mod Pathol. 2009;22(3):450–459. doi: 10.1038/modpathol.2008.204. [DOI] [PubMed] [Google Scholar]
- 29.Levens ED, Potlog-Nahari C, Armstrong A, et al. CDB-2914 for uterine leiomyomata treatment: a randomized controlled trial. Obstet Gynecol. 2008;111(5):1129–1136. doi: 10.1097/AOG.0b013e3181705d0e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nieman LK, Blocker W, Nansel T, et al. Efficacy and tolerability of CDB-2914 treatment for symptomatic uterine fibroids: a randomized, double-blind, placebo-controlled, phase IIb study. Fertil Steril. 2011;95(2):767–772. doi: 10.1016/j.fertnstert.2010.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]