Abstract
We investigated the effects of domain-general processing capacity (fluid ability such as working memory), domain-general knowledge (crystallized ability such as vocabulary), and domain-specific health knowledge for two of the most commonly used measures of health literacy (S-TOFHLA and REALM). One hundred forty six community-dwelling older adults participated; 103 had been diagnosed with hypertension. The results showed that older adults who had higher levels of processing capacity or knowledge (domain-general or health) performed better on both of the health literacy measures. Processing capacity interacted with knowledge: Processing capacity had a lower level of association with health literacy for participants with more knowledge than for those with lower levels of knowledge, suggesting that knowledge may offset the effects of processing capacity limitations on health literacy. Furthermore, performance on the two health literacy measures appeared to reflect a different weighting for the three types of abilities. S-TOFHLA performance reflected processing capacity as well as general knowledge, whereas performance on the REALM depended more on general and health knowledge than on processing capacity. The findings support a process-knowledge model of health literacy among older adults, and have implications for selecting health literacy measures in various health care contexts.
Health literacy, defined as the capacity to obtain, understand, and use information and services needed to make health decisions (U.S. DHHS, Healthy People 2010), has been linked to many patient behaviors and health outcomes, especially among older adults with chronic illness (Berkman et al., 2011; DeWalt, Berkman, Sheridan, Lohr, & Pignone, 2004; Nielsen-Bohlman, Panzer, & Kindig, 2004; Paasche-Orlow, Parker, Gazmararian, Nielsen-Bohlman, & Rudd, 2005). Health literacy is often viewed functionally as the match between patients’ abilities and the demands imposed on these abilities by health tasks (Baker, 2006; Nielsen-Bohlman et al., 2004), yet we know little about the component abilities critical to functional health literacy that are deployed to accomplish even rudimentary health tasks.
A starting point for identifying these components is to investigate abilities that are associated with measures that have been found to predict health behaviors and outcomes. Although it is generally agreed that there are nomeasures that adequately cover the broad definition of functional health literacy (Berkman, Davis, & McCormack, 2010), there are two that are commonly used to assess this construct (Paasche-Orlow et al., 2005): the Rapid Estimate of Adult Literacy in Medicine (REALM; Davis et al., 1993) and the Short Test of Functional Health Literacy in Adults (S-TOFHLA; Baker, Williams, Parker, Gazmararian, & Nurss, 1999). These instruments measure some of the reading and literacy skills that are prerequisites for self-care (DeWalt & Pignone, 2005) and are associated with performance on tasks that reflect health-information seeking and comprehension (e.g., Chin, Fu, & Kannampallil, 2009; Davis et al., 2006), as well as self-care behaviors and health outcomes (Berkman et al., 2011). Therefore, the S-TOFHLA and REALM have been interpreted as proxy measures for a broadly defined set of activities that link health literacy and health outcomes (e.g., DeWalt et al., 2004; Nielsen-Bohlman et al., 2004).
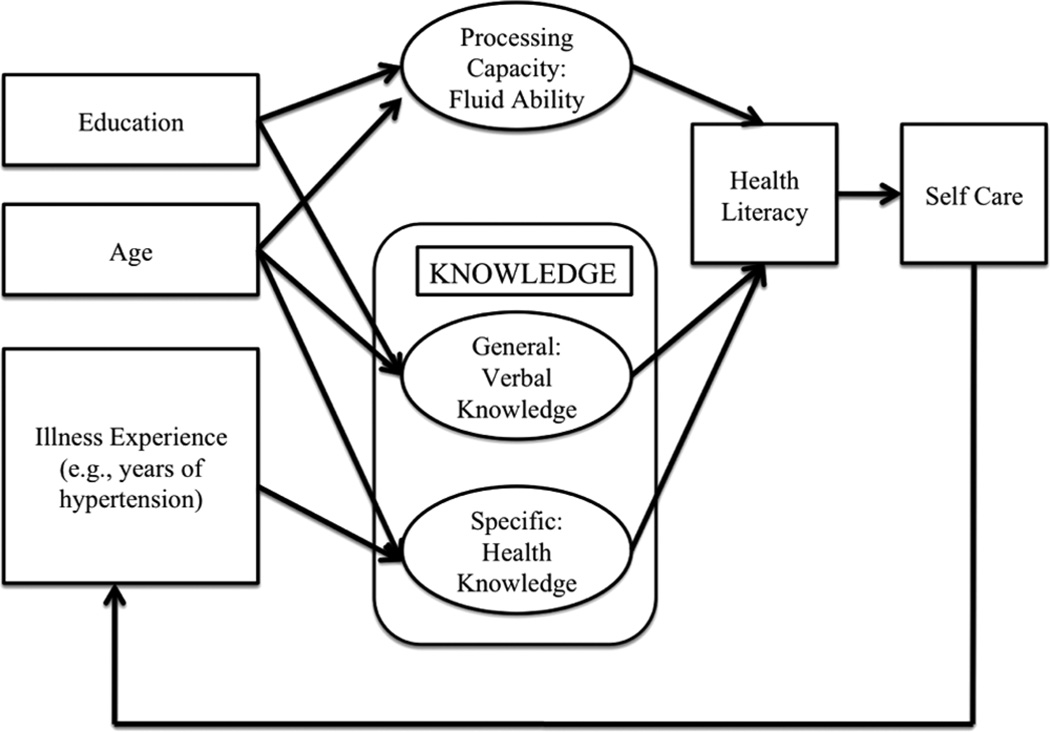
Our investigation of abilities that are related to these proxy measures of literacy activities was guided by what we call the Process-Knowledge model (P-K model). This framework posits three fundamental components of health literacy among older adults: processing capacity (fluid ability such as working memory), general knowledge (crystallized ability such as vocabulary), and specific health knowledge. We focus on processing capacity and knowledge as components of health literacy among older adults because they are central to reading comprehension (Kintsch, 1998) and have distinct trajectories across the life span (Baltes, 1997). Guided by this model, our goal is to examine how these components contribute to performance on the S-TOFHLA and REALM. It is important to distinguish sources of variance in health literacy that are caused by processing capacity and knowledge because (a) trade-offs between processing capacity and knowledge can impact health literacy in particular contexts; (b) health literacy limitations caused by either limited processing capacity or lack of knowledge suggest distinct interventions; and (c) the development of processing capacity and knowledge across the life span varies as a function of health, educational background, and experience with particular diseases, implying that “health literacy” during the adult years does not develop as a single construct. We explored the components of health literacy among older adults with hypertension, one of the most common age-related chronic illnesses (American Heart Association, 2010).
Our framework (see Figure 1) integrates current health literacy models (Baker, 2006; Nielsen-Bohlman et al., 2004) with life span theories of cognition (Baltes, 1997; Beier & Ackerman, 2005) and comprehension (Stine-Morrow, Miller, & Hertzog, 2006). As in other models, health literacy is conceptualized as a competency used to meet the demands imposed by the need to understand health information for self-care. Our focus in the present study was on the internal structure of health literacy as a multifaceted capacity critical for comprehension, planning, and decision-making (Morrow et al., 2006).
Figure 1.
The process-knowledge model of health literacy.
Aging, Cognition, and Comprehension
Language comprehension requires the coordination of mental processes such as recognizing words, combining conceptual representations of words into ideas, and linking ideas to construct a representation of the meaning of the text (textbase). Readers elaborate on this textbase based on their knowledge to create a situation model, which represents events and states implied by the text (Kintsch, 1998). Whereas the textbase depends on general processing capacity that constrains how efficiently novel information is processed (Stine & Wingfield, 1990), knowledge can support word recognition, conceptual integration, and situation model construction so as to reduce reliance on processing capacity (Miller, 2009).
The cognitive abilities underlying comprehension have different life span trajectories (Horn & Hofer, 1992). Processing capacity tends to decline, which helps explain why older adults are generally less successful than younger adults at creating and retaining the textbase when comprehension imposes heavy demands on working memory (Johnson, 2003). More positively, general knowledge (Stanovich, West, & Harrison, 1995), domain-specific knowledge (Krampe & Charness, 2006; Morrow, Leirer, Altieri, & Fitzsimmons, 1994), and health knowledge (Chin, D’Andrea, et al., 2009; Gazmararian, Williams, Peel, & Baker, 2003), tend either to remain unchanged or to increase with age, reflecting age-related experience from work, illness, and other factors. Knowledge-related gains in efficiency of processing may reduce comprehension demands on processing capacity. For example, older domain experts effectively deploy their knowledge despite processing capacity limits to support high levels of comprehension for domain-relevant text (Miller, Stine-Morrow, Kirkorian, & Conroy, 2004; Morrow et al., 1994).
Aging and Health Literacy
Our framework suggests that health literacy depends on the interplay among processing capacity, general knowledge, and health knowledge. The REALM (Davis et al., 1993) and the S-TOFHLA (Baker et al., 1999), as commonly used proxies for health literacy, provide single scores but arguably depend on all three of these components. Indeed, performance on these measures among older adults with chronic illness has been found to be associated with processing capacity, which explains many of the age-related differences in performance (Baker et al., 2007; Levinthal et al., 2008; Morrow et al., 2006). These findings converge with evidence that performance on measures of general literacy is associated with cognitive function among older adults (Barnes, Tager, Satariano, & Yaffe, 2004).
Even though the contribution of processing capacity to health literacy is clear (e.g., Morrow et al., 2006), little is known about the role of knowledge. Health and general knowledge may counter limitations on comprehension associated with processing capacity for several reasons. First, older adults tend to know more than younger adults about health (Beier & Ackerman, 2005). Second, older adults with chronic illness tend to learn more about their illness over time, perhaps by taking classes or by self-directed learning from TV, the web, or other sources (Beier & Ackerman, 2005; Gazmararian et al., 2003). Patients reporting having had hypertension for a longer period of time have been found to know more about their illness despite having lower levels of processing capacity (Chin, D’Andrea, et al., 2009). Finally, the aging and comprehension literature suggests that older adults may leverage their knowledge to support comprehension despite age-related declines in processing capacity (e.g., Miller, 2009). However, despite the theoretical and practical importance of investigating how knowledge supports health literacy, no studies have examined relationships among general knowledge, health knowledge, and processing capacity as components of health literacy, even though illness knowledge is associated with health literacy (Gazmararian et al., 2003).
The Present Study
We investigated how processing capacity, general knowledge, and health knowledge relate to performance on the two most commonly used measures of health literacy: the REALM (Davis et al., 1993) and the S-TOFHLA (Baker et al., 1999). We expected older adults with higher levels of both processing capacity and knowledge to perform better on both measures. Most important, we expected knowledge to offset limitations imposed by processing capacity on both measures, such that participants high in knowledge would perform well regardless of level of processing capacity, while the contribution of processing capacity would be greater for participants with low knowledge.
Method
Participants
Participants were recruited from Champaign-Urbana and Peoria, Illinois. They were screened for normal vision, motor skills, native English-language proficiency, and normal cognitive function (MMSE > 23; Mini-Mental State Exam; Folstein, Folstein, & McHugh, 1975). They were also screened to ensure that they had not had a stroke or cancer treatments in the previous 3 years, which might impair cognitive function. No participants were screened out of the study based on these criteria. Participants with hypertension were identified by self-reported physician diagnosis and use of medications prescribed for high blood pressure, for example, “Have you ever been told by a doctor or other health professional that you have high blood pressure?” (Centers for Disease Control and Prevention, 2007; Nelson, Holtzman, Bolen, Stanwyck, & Mack, 2001). We also asked them to report how long they have been diagnosed with hypertension.
Measures
Table 1 summarizes the health literacy, cognitive, and knowledge measures. For all measures, higher scores indicated better performance.
Table 1.
Summary of measures
| Construct | Instrument | Source | Internal consistency reliability |
|---|---|---|---|
| Health Literacy | |||
| Medical-related reading | S-TOFHLA | Baker et al., 1999 | 0.90 |
| Medical vocabulary pronunciation | REALM | Davis et al., 1993 | 0.91 |
| Process | |||
| Processing speed | Letter Comparison | Salthouse, 1991 | 0.73~0.84 |
| Pattern Comparison | Salthouse, 1991 | 0.73~0.84 | |
| Finding As | Ekstrom et al., 1976 | 0.73~0.74 | |
| Identical Pictures | Ekstrom et al., 1976 | 0.81~0.87 | |
| Working memory | Letter Number Sequencing | Wechsler, 1997 | |
| Inductive reasoning | Letter Sets Test | Ekstrom et al., 1976 | 0.74~0.84 |
| Everyday Problem Solving | Marsiske & Willis, 1995 | ||
| Visual spatial ability | Card Rotation | Ekstrom et al., 1976 | 0.86~0.89 |
| Hidden Patterns | Ekstrom et al., 1976 | 0.81~0.91 | |
| Knowledge | |||
| General (vocabulary) | Advanced Vocabulary | Ekstrom et al., 1976 | 0.79 |
| Extended Range Vocabulary | Ekstrom et al., 1976 | 0.81~0.84 | |
| North American Adult Reading Test | Uttl, 2002 | 0.93 | |
| Author Recognition Test | Stanovich et al., 1995 | ||
| Specific (health) | Hypertension Knowledge Questionnaire | Modified in Chin, D’Andrea et al., 2009 | 0.90 |
Health Literacy
Health literacy was measured by the S-TOFHLA (Baker et al., 1999) and REALM (Davis et al., 1993), which have been shown to predict health-related behaviors (Nielsen-Bohlman, Panzer & Kindig, 2004) and outcomes (DeWalt et al., 2004). In the S-TOFHLA, participants read two brief health care documents, such as a consent form for x-rays. They completed 36 cloze items in which a word is deleted from the text and they choose the best of four options to complete the sentence. To better understand what types of knowledge were needed to accomplish this task, two people independently coded each cloze item for whether it required health knowledge (e.g., Your doctor has sent you to have a ____x-ray. a. stomach, b. diabetes, c. stitches, d. germs) or linguistic (semantic or grammatical) knowledge (e.g., Do not eat _____. a. appointment, b. walk-in, c. breakfast, d. clinic). Fewer than 10% of the items required health knowledge (inter-rater agreement was acceptable, Kappa = .85).
In the REALM, participants pronounced 66 medical words varying in length and frequency of occurrence. Higher health literacy is indicated by correct pronunciation of more words, which may occur either because people have more medical knowledge related to these words, or better general verbal abilities, including phonological rules for pronouncing the words. In short, compared with the S-TOFHLA, better performance on the REALM more likely reflects health and general knowledge than processing capacity.
Processing Capacity
We used several standard measures of processing capacity. Processing speed was measured by the Letter Comparison and Pattern Comparison tests (Salthouse, 1991), in which participants judged within 30 seconds whether two letter strings or two patterns were the same. Speed of visual processing was measured by the Finding As test and the Identical Pictures test (Ekstrom, French, Harmon, & Dermen, 1976). In the former, participants needed to circle the letter “a” in a list of words, in 2 minutes. In the latter, participants were given a target picture and needed to identify the corresponding identical picture from a set of distracter pictures. Spatial ability was measured by the Card Rotation and the Hidden Pattern test (Ekstrom et al., 1976). These timed tests require participants to perform mental rotation or spatial search operations.
Working memory capacity was measured by the Letter Number Sequencing (Wechsler, 1997). Participants first heard a combination of letters and numbers, and then recalled the letters and numbers in order immediately. Inductive reasoning was measured by the Letter Sets test (Ekstrom et al., 1976) and Everyday Problem Solving (Marsiske & Willis, 1995). In the Letter Sets test, participants were told to identify a letter string from other letter strings based on its composition rule. The Everyday Problem Solving measured reasoning abilities in the contexts of daily life problems, such as reading a nutrition label or understanding a recipe.
General Knowledge
General knowledge, or crystallized ability, was measured by the Advanced Vocabulary Task, Extended Range Vocabulary Task (Ekstrom et al., 1976), North American Adult Reading Test (NAART; Uttl, 2002) and the Author Recognition Test (Stanovich et al., 1995). The first two mainly measured verbal ability, while the latter two measured general literacy. In the Author Recognition Test, participants chose the names of real authors from a list of nonauthor names. Higher scores are interpreted as reflecting more reading experience and better literacy (Stanovich et al., 1995).
Health Knowledge
Our measure of health knowledge focused on hypertension because the majority of participants in our study were diagnosed with this illness. Hypertension knowledge was considered a facet of broader health domain knowledge (Beirer & Ackerman, 2005). We created a questionnaire with 33 true/false questions and four multiple-choice questions to measure the hypertension knowledge of participants. These questions probed knowledge of several aspects of hypertension, such as the definition, causes and consequences, risk factors, self-care, as well as heart structures and functions. Twenty-five of the T/F questions were from Gazmararian and colleagues (2003) and focused on hypertension’s definition, consequences, and self-care. For example, “Exercising every day may make blood pressure go down.” To extend the breadth of questions and balance the T/F ratio of Gazmararian’s set of questions, we added eight T/ F questions modified from the materials on the American Heart Association (2007) website and from a previous study (Oliveria et al., 2005). An example of a false item was, “For a blood pressure reading of 120/80, the number 80 is the systolic blood pressure.” The four multiple-choice questions were from Miller and colleagues (2004) and measured patients’ understanding of the heart structures and functions. For example, “During systole, (a) the heart relaxes; (b) the mitral valve opens; (c) the heart contracts; (d) the bicuspid valve opens.”
Health Status
Health status was measured by two widely used tests, SF-36 (Ware & Sherbourne, 1992) and the self-report version of the Charlson Comorbidity Index (Katz, Chang, Snagha, Fossel, & Bates, 1996). The SF-36 included a physical functioning subscale (10 items) and a mental health subscale (five items). Each item was scaled from 0 to 100, with higher scores indicating better self-reported health. The unweighted Comorbidity Index score was used to estimate illness in terms of number of conditions, with higher mortality connected to higher comorbidity. Besides health status measures, a “years of hypertension” variable was created by asking participants to self-report how long they had been diagnosed with hypertension. The healthy participants (no diagnosis of hypertension or other chronic illness) were assigned a zero for this variable, which was log transformed to address the skewed distribution.
Procedure
The study consisted of two sessions conducted on separate days in order to reduce the risk of fatigue. Participants first provided informed consent in the first session. Next, their blood pressure was measured by an electronic monitor (HEM-711DLX) twice (15 minutes between readings). Both readings of systolic and diastolic blood pressure were recorded. All participants were administered the cognitive and knowledge measures in the same order, using standard instructions in a quiet room. The remaining measures were administered during the second session. At the end of this session, participants were debriefed and compensated.
Plan of Analysis
We first replaced missing data and created composite scores for some measures. Missing data (some tests were not completed, possibly due to fatigue) and outliers (values more than three standard deviations above or below the mean with the mean scores) were replaced with mean of the condition. Less than 1% of the data was replaced. Two cognitive ability composite scores were created based on the large amount of literature showing that processing capacity and general knowledge measures form distinct clusters (e.g., Beier& Ackerman, 2005). Scores for the 13 cognitive measures were standardized (z-transformed). A processing capacity composite score was created by summing standardized scores for Letter Comparison, Pattern Comparison, Finding As, Identical Picture, Letter Number Sequencing, Letter Sets, Everyday Problem Solving, Card Rotation, and Hidden Pattern tests. This composite variable had acceptable reliability (Cronbach’s alpha = .83). A general knowledge composite score was created by combining standardized scores for Advanced Vocabulary, Extended Vocabulary, Author Recognition Test, and North American Adult Reading Test (Cronbach’s alpha = .87).
The next step was to correlate the two cognitive ability composite scores, the health knowledge measure, and education with the two health literacy measures. Guided by these correlational results, we conducted multivariable regression models in order to investigate the separate and interacting effects of processing capacity and knowledge on S-TOFHLA and REALM while controlling age, education, and years of illness. The significant interaction effects were analyzed by the slope analysis to explore the compensatory effects of knowledge on the health literacy for the decline in processing capacities.
Results
Health Literacy, Demographic, and Ability Variable Correlations
Of the 148 participants, two discontinued due to fatigue. Data from the remaining 146 participants (60–87 years old; mean age = 69.6, SD = 6.7) were used in the study. Eighty-eight (60.3%) were female and 58 (34.9%) had a high school level of education or less (see Table 2). Over two thirds were diagnosed with hypertension (N = 103, 70.5%), and the rest had no chronic illness diagnosis. Among the hypertensive participants, mean duration of their illness was 9 years (range, 1–40 years) (see Table 2). Our sample had high levels of health literacy (only 7% had inadequate or marginal literacy on the S-TOFHLA and REALM), reflecting the generally high level of education of the sample. Nonetheless, there was a wide range of scores for the S-TOFHLA (mean = 32.8, min = 6, max = 36) and REALM (mean = 63.6, min = 3, max = 66), enabling us to investigate relationships among health literacy and participants’ abilities. All the participants completed the S-TOFHLA within 7 minutes, suggesting that performance on this timed test was not constrained by the time limits.
Table 2.
Characteristics of participants
| Variable (N = 146) | |
|---|---|
| Female, n (%) | 88 (60.3) |
| Age, M (SD) | 69.6 (6.7) |
| Education, n (%) | |
| Less than high school | 20 (8.9) |
| High school graduated | 38 (26) |
| More than high school | 88 (65.1) |
| S-TOFHLA, M (SD) | 32.79 (4.94) |
| REALM, M (SD) | 63.55 (6.92) |
S-TOFHLA = Short Test of Functional Health Literacy in Adults (Baker et al., 1999).
REALM = Rapid Estimate of Adult Literacy in Medicine (Davis et al., 1993).
We also explored whether including participants without chronic illness as well as with hypertension in our sample increased variability in potential variables associated with health literacy by comparing the two subsamples on these variables. Compared with participants who had hypertension, the healthy participants showed better performance on the physical (692.09 vs. 835.77, t(144) = −3.31, p < .001) and mental (381.81 vs. 415.19, t(144) = −2.29, p < .05) health SF-36 subscales, as well as the processing capacity composite (−0.86 vs. 2.07, t(144) = −2.83, p < .005). There was no group difference in systolic blood pressure (mean across the two BP readings; hypertensive group: 134, healthy group: 131, t(144) = 0.53, p = .60) or diastolic blood pressure (mean = 80 for both groups).
Pearson correlations showed that the two health literacy measures were moderately correlated (see Table 3). Both were significantly correlated with processing capacity, general knowledge, education, and health knowledge. Consistent with our predictions, the S-TOFHLA had a higher correlation with processing capacity and a lower correlation with health knowledge than the REALM. Age and the comorbidity measure were negatively associated with S-TOFHLA but not with the REALM (the comorbidity measure also correlated with S-TOFHLA scores in simple but not multivariable regression analyses in Levinthal et al., 2008; and Morrow et al., 2006). Gender and the SF-36 measure were not correlated with either health literacy measure. Therefore, we excluded the health and gender measures from the regression analysis. However, age was included in the analyses because it is central to theoretical analyses of cognition across the life span, and because of the well-established negative association between health literacy and age in the previous study (Baker, Gazmararian, Sudano, & Patterson, 2000).
Table 3.
Correlations among age, education, health literacy, processing capacity and knowledge measures
| 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | S-TOFHLA | .52** | .16* | −.18* | .37** | −.21* | .58** | .46* | −.24** | .15 | .10 |
| 2. | REALM | – | .32** | .03 | .37** | −.06 | .33** | .43** | −.13 | .15 | .12 |
| 3. | Health knowledge | – | .04 | .27** | .18* | .24** | .33** | −.11 | .09 | .08 | |
| 4. | Age (years) | – | .03 | .15 | −.29** | .06 | .17* | −.12 | .05 | ||
| 5. | Education | – | −.08 | .40** | .49** | −.20* | .25** | .08 | |||
| 6. | Years of Hypertension | – | −.24** | −.14 | .37** | −.26** | −.15 | ||||
| 7. | Processing capacity | – | .53** | −.41** | .27** | .21* | |||||
| 8. | General knowledge | – | −.23** | .10 | .14 | ||||||
| 9. | Comorbidity index | – | −.46** | −.26** | |||||||
| 10. | SF36-physical | – | .30** | ||||||||
| 11. | SF36-mental | – |
Note:
p<.05;
p<.01.
Regression Models of Health Literacy Correlates
Guided by the simple correlations of potential correlates with health literacy and the P-K model, we conducted multivariable regression models for each health literacy measure. Variables were entered in the following order: (1) Age, (2) Education and Years of Hypertension, (3) Processing capacity, (4) General knowledge and health knowledge. In the final step, we explored possible trade-offs between knowledge (crystallized ability and health knowledge) and processing capacity by entering the interaction terms—processing capacity × general knowledge and processing capacity × health knowledge—after controlling for the main effects of processing capacity and knowledge. We first centered the scores on processing capacity, general, and health knowledge in order to reduce possible effects of multicollinearity (Smith & Sasaki, 1979). Then, we computed the product of the processing capacity and general-knowledge variables to create the processing capacity × general-knowledge interaction term (the processing capacity × health knowledge term was similarly created).
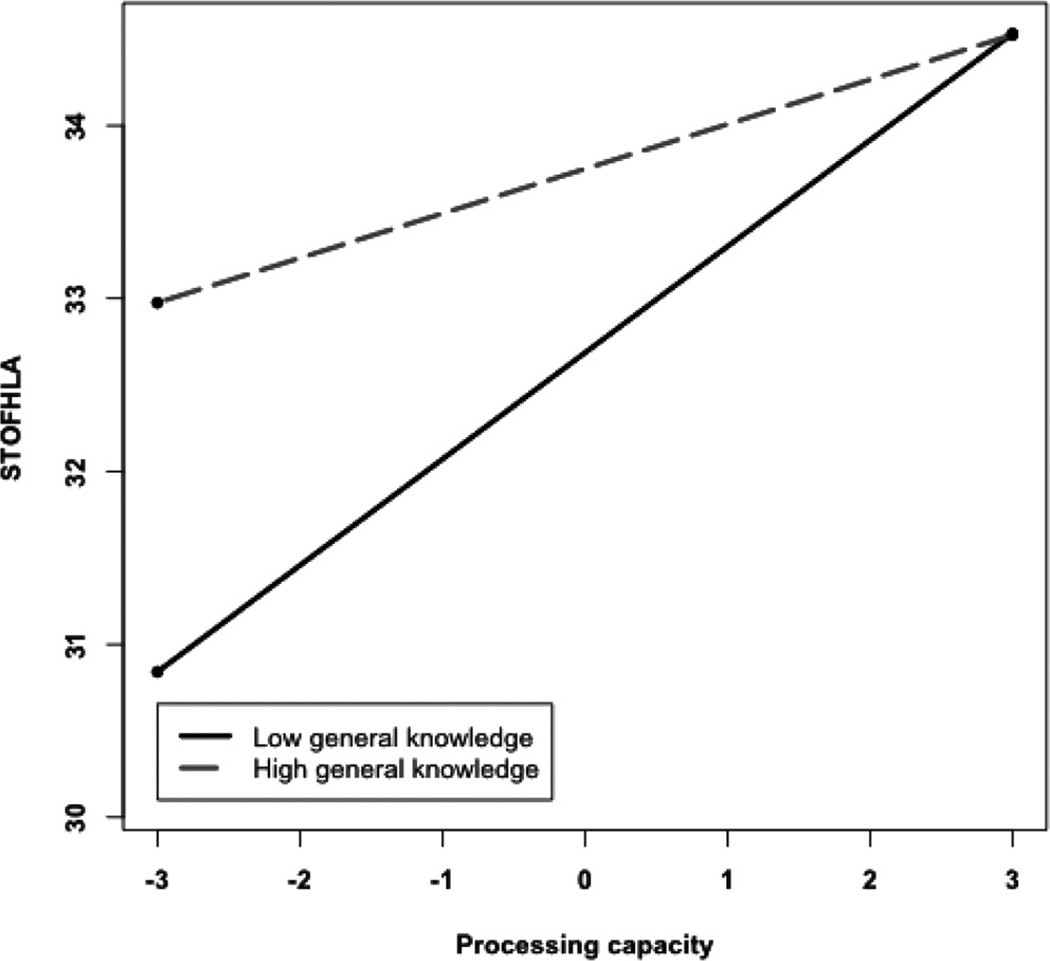
Table 4 shows that better performance on the S-TOFHLA was associated with younger age (Step 1) and higher education (Step 2), but the effects of age and more than half of the education-related variance was explained by processing capacity (Step 3; also see Morrow et al., 2006). General knowledge, but not health knowledge, also explained variance in health literacy (Step 4). Most interesting, the processing capacity × general-knowledge interaction term was significant in the final step. To analyze the relationship between processing capacity and general knowledge, we did a median split on the general-knowledge variable and investigated the relationship between processing capacity and S-TOFHLA performance for participants who were higher or lower in general knowledge. Figure 2 suggests that processing capacity was associated with S-TOFHLA performance for the low but not high general-knowledge participants.
Table 4.
Regression model examining correlates of S-TOFHLA (Standardized Beta coefficients are listed in each step)
| Variable | Step 1 | Step 2 | Step 3 | Step 4 | Step 5 |
|---|---|---|---|---|---|
| Model R2 | 2.4%* | 16.6%** | 34.4%** | 36.1%** | 42.0%** |
| Age | −0.18* | −0.17* | −0.02 | −0.06 | −0.11 |
| Education | 0.39** | 0.18* | 0.14 | 0.13 | |
| Years of Hypertension | −0.12 | −0.09 | −0.10 | −0.09 | |
| Processing capacity | 0.49** | 0.41** | 0.36** | ||
| General knowledge | 0.20* | 0.16 | |||
| Health knowledge | −0.06 | −0.08 | |||
| Processing capacity × General knowledge | −0.26** | ||||
| Processing capacity × Health knowledge | −0.04 |
Note:
p<.05;
p<.01.
Figure 2.
Relationship between S-TOFHLA and processing capacity for high and low general knowledge groups.
To further analyze this pattern, we conducted separate regressions for the high and low general-knowledge participants with the following variables for S-TOFHLA performance: (1) Age, (2) Education and Years of Hypertension, and (3) Processing capacity. The beta coefficient for processing capacity was higher for the low-general-knowledge group (β = .54) than high-general-knowledge group (β = .17) (t(136) = 5.51, p < .001), providing more direct evidence that processing capacity had less influence on S-TOFHLA performance for participants with higher general knowledge. This finding suggests that general knowledge compensated for lower processing capacity in supporting S-TOFHLA performance.
In addition to the significant difference in the association between processing capacity and S-TOFHLA in low- and high-general-knowledge groups, we used simple slope techniques (Preacher, Curren, & Bauer, 2006) to visualize the interaction effect between processing capacity and general knowledge. The interaction term was decomposed into a simple regression of S-TOFHLA onto processing capacity for lower and higher general knowledge (Figure 2) instead of testing group differences. Results showed that processing capacity was positively associated with S-TOFHLA for both lower and higher general-knowledge groups (t(142) = 7.05 and 2.73 respectively, ps < .01) despite the difference between slopes (β = .62, β = .23 for lower and higher general-knowledge group, respectively; see Figure 2).
Table 5 shows that better performance on the REALM was associated with more education (Step 2), processing capacity (Step 3), as well as general and health knowledge (Step 4). Consistent with the simple correlations, processing capacity appeared to play a smaller role in explaining the variance in REALM compared to S-TOFHLA performance (β = .25 vs. .49), which was largely explained by the knowledge measures. Together, processing capacity and general knowledge also explained the education-related effects (Step 4).
Table 5.
Regression model examining correlates of REALM (standardized beta coefficients are listed in each step)
| Variable | Step 1 | Step 2 | Step 3 | Step 4 | Step 5 |
|---|---|---|---|---|---|
| Model R2 | −0.01% | 11.8%** | 16.1%** | 22.6%** | 31.9%** |
| Age | 0.03 | 0.03 | 0.10 | 0.03 | −0.03 |
| Education | 0.37** | 0.27** | 0.15 | 0.14 | |
| Years of Hypertension | −0.02 | −0.004 | 0.06 | 0.11 | |
| Processing capacity | 0.25** | 0.12 | 0.09 | ||
| General knowledge | 0.23* | 0.18 | |||
| Health knowledge | 0.19* | 0.13 | |||
| Processing capacity × General knowledge | −0.21** | ||||
| Processing capacity × Health knowledge | −0.21** |
Note:
p<.05;
p<.01.
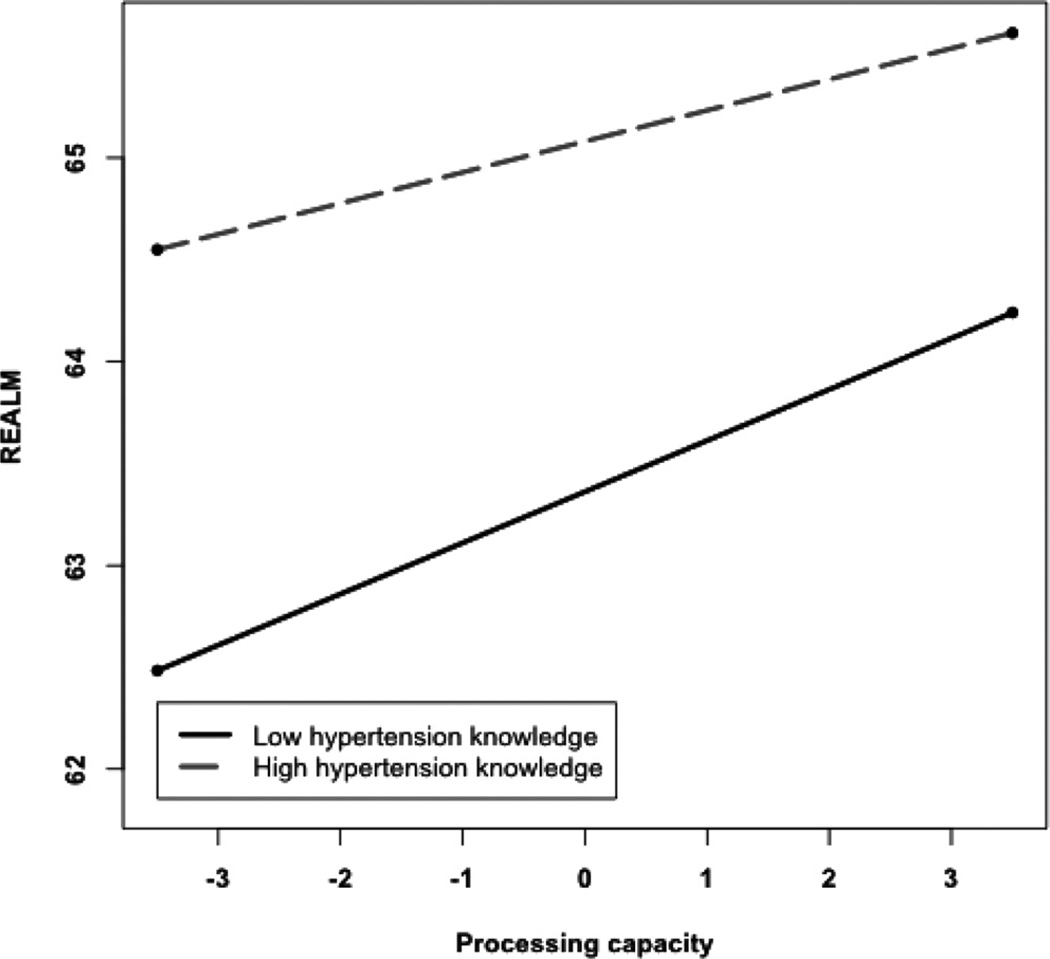
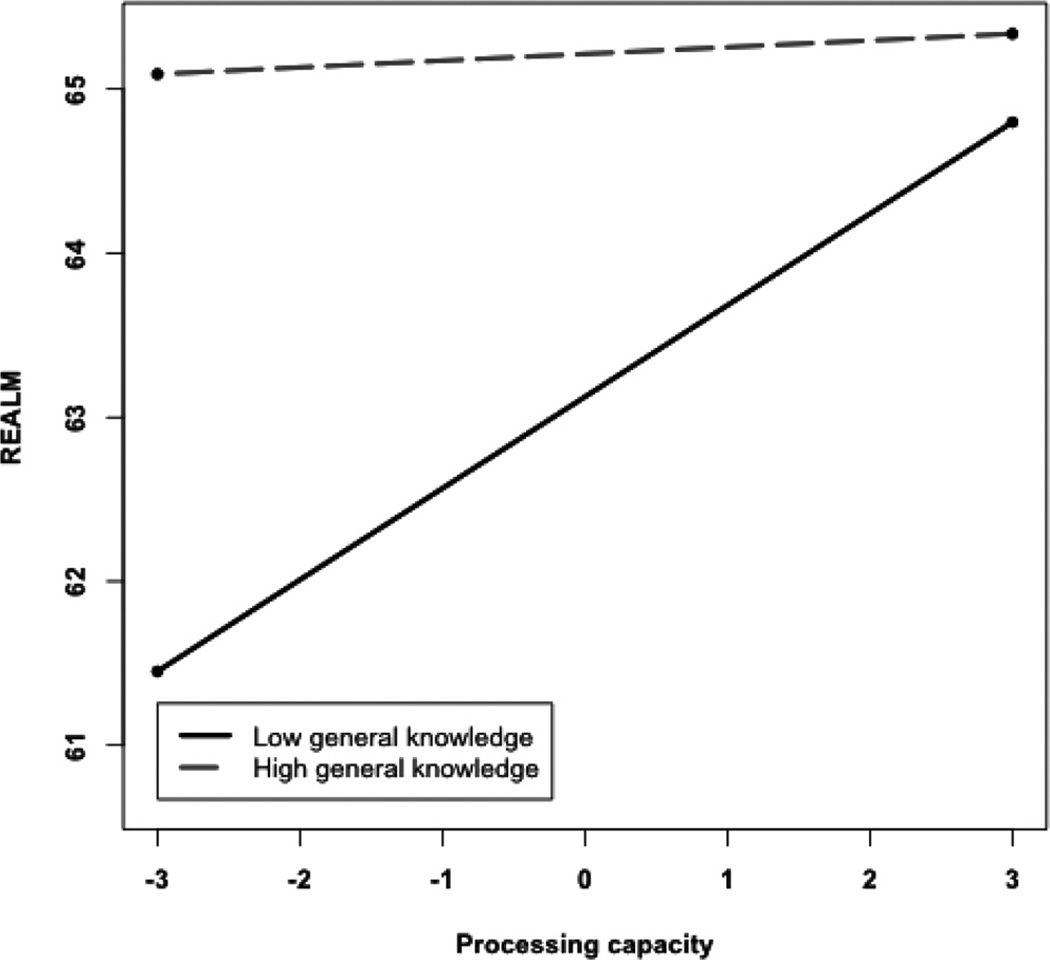
Most important, both the processing capacity × health-knowledge interaction and the processing capacity × general-knowledge terms were significant (Step 5). These interactions were analyzed in the same way as the S-TOFHLA regression. Processing capacity was associated with REALM performance for lower but not higher health knowledge (Figure 3). As before, we analyzed this pattern by conducting separate regressions for participants who were high or low in health knowledge (based on median split) with the following variables: (1) Age, (2) Education and Years of Hypertension, and (3) Processing capacity. The beta coefficient for processing capacity was larger for the low health-knowledge group (β = .40) than for the high health-knowledge group (β = .09) (t(136) = 2.90, p < .005). A similar pattern occurred for the low- (β = .41) vs. high-general-knowledge groups (β = .04). These findings suggest that REALM performance is limited by processing capacity primarily for older adults with lower general knowledge or lower health knowledge, but not for older adults with higher levels of knowledge. The simple slope technique (Preacher et al., 2006) was again used to visualize the interaction effects between processing capacity and health knowledge on REALM (Figure 3). Results showed that processing capacity was positively associated with REALM in the lower health-knowledge group (β = .25, t(142) = 2.75, p < .01), but not in the higher health-knowledge group (β = .15, t(142) = 1.52, p = .13). For the processing capacity × general-knowledge interaction, the simple slope technique also showed that processing capacity was positively associated with REALM performance in the lower general knowledge group (β = .56, t(142) = 4.00, p < .001), but not in the higher general knowledge group (β = .04, t(142) = 0.27, p = .78; Figure 4).
Figure 3.
Relationship between REALM and processing capacity for high and low hypertension knowledge groups.
Figure 4.
Relationship between REALM and processing capacity for high and low general knowledge groups.
Discussion
Performance on both the S-TOFHLA and REALM measures of health literacy depended on multiple cognitive abilities. Older adults with higher levels of processing capacity and knowledge performed better on the measures. Most important, there was some evidence that higher levels of knowledge offset the impact of limited processing capacity, such that processing capacity was less likely to be associated with performance among the more knowledgeable participants. The processing capacity and knowledge variables also helped to explain the influence of age (S-TOFHLA) and education (both measures) on health literacy performance. Processing capacity may mediate the relationship between education and health literacy in part because less educated elders are perhaps more likely to experience chronic illness (Nielsen-Bohlman et al., 2004), further eroding cognitive function (for hypertension; Kilander, Nyman, Boberg, Hansson, & Lithell, 1998).
Although the two health literacy measures were moderately correlated, successful performance on each measure depended on profiles of abilities that were somewhat different. Processing capacity was most related to S-TOFHLA performance, followed by general knowledge. On the other hand, general and health knowledge were most important for the REALM and accounted for most of the processing capacity effects. General knowledge offset processing capacity on both measures, whereas health knowledge also did so for the REALM. These findings extend earlier work in this area (Federman et al., 2009; Levinthal et al., 2008; Morrow et al., 2006) by showing that general knowledge and health knowledge, as well as processing capacity, explain large amounts of variance in performance of the two most commonly used measures of health literacy, and that high levels of knowledge may reduce the role of processing capacity in performance. These findings have several implications for health literacy models and measures.
Health Literacy Models
The findings support a P-K model of health literacy. Processing capacity may have been important for comprehension (and thus performance on the health literacy measures) because working memory constrains the efficiency of processes, such as integrating concepts into a textbase representation and elaborating the latter into a situation model, which helps explain age-related differences in comprehension (Johnson, 2003). Such age-related limitations in processing capacity would be reflected more in S-TOFHLA performance because the cloze procedure in this test requires participants to keep sentences with missing words in working memory in order to compare them with options for missing words.
General and health knowledge also played important roles in explaining performance on the measures, presumably because knowledge facilitates word recognition and provides relationships among concepts that facilitate comprehension. The importance of general as well as health knowledge for heath literacy performance supports the view that health literacy overlaps with more general literacy skills (Rudd, 2007), while the importance of hypertension knowledge (for REALM performance) suggests that health literacy also builds on more specific knowledge in the health domain (e.g., Gazmararian et al., 2003).
The finding that older adults with more knowledge performed well even if they had lower levels of processing capacity suggests that knowledge may make comprehension processes more efficient and less resource-consuming. The resilience of situation model processes among older adults has been explained in part by age-related accumulation of knowledge relevant to the text topic (Radvansky & Dijkstra, 2007). Evidence that knowledge offsets processing capacity limitations in our study is also consistent with adult learning theories suggesting that for complex, open-ended, knowledge-based tasks, general and domain knowledge are stronger predictors of learning than is processing capacity (Beier & Ackerman, 2005).
Our study suggests that health literacy depends in part on a constellation of general abilities that are important for understanding and reasoning about health information, and that there may be multiple paths to achieving health literacy (also see Wolf et al., 2009). For example, older adults who have had hypertension for many years and have learned about their illness despite processing capacity limits may leverage this knowledge to continue learning about their illness and to develop effective plans for managing their illness (Chin, D’Andrea et al., 2009). Younger adults who have recently been diagnosed, on the other hand, may rely on higher levels of processing capacity to reason about their illness despite sparse knowledge. Other resources that were not investigated in the present study, such as health-related self-efficacy or self-care daily practices, may provide other paths to health literacy.
Health Literacy Measures
Our findings also have implications for measuring health literacy. Performance on the two measures was moderately correlated, suggesting that they measure overlapping abilities (that is, a common construct). However, the regressions identified a different pattern of abilities underlying performance on each, suggesting the tests tap different abilities reflecting different task demands. The S-TOFHLA required patients to understand text and choose the best word to complete sentences, which taxed working memory and required general (language) knowledge rather than health knowledge. To the extent that such tests do not require health knowledge, they may underestimate the capacity of some patients to navigate the health care system and accomplish self-care tasks. Similar issues exist for developing measures of how well older experts perform their jobs: Measures that weight general processing capacity over domain knowledge may underestimate the competence of older experts (Morrow et al., 1994).
Our findings suggest that health literacy measures tap different abilities, so the choice of which measure to use will depend on an analysis of demands imposed by the criterion task. For the purpose of academic research, S-TOFHLA can be used to predict how well patients perform general comprehension and reasoning tasks with minimal support from specific health contexts. On the other hand, the REALM may predict how well patients perform tasks that depend heavily on illness knowledge. For clinical goals such as screening, given that self-care tasks are associated with multiple abilities such as domain-specific knowledge and general processing capability, both S-TOFHLA and REALM will generally predict patients’ health outcomes (DeWalt & Pignone, 2005).
Limitations
Our study has several limitations that influence our ability to generalize and interpret the findings. First, because the study was correlational in design, conclusions about causal relationships among the cognitive variables and performance on the health literacy tests cannot be drawn. For example, health knowledge and health literacy may reciprocally influence one another. As suggested in Figure 1, knowledge can improve comprehension and learning associated with health literacy, while at the same time it is possible that health literacy will also influence health knowledge through self-care and health outcomes.
A second limitation was the use of REALM and S-TOFHLA as proxy measures of health literacy. To study the relationship between cognition and health literacy is difficult because there is no adequate measure of functional health literacy as it has been broadly defined (Berkman et al., 2010). However, the study of the most commonly used health literacy measures, the REALM and the S-TOFHLA, is a reasonable starting point, especially given the well-documented connections between these measures and health outcomes and behaviors (e.g., DeWalt et al., 2004; Nielsen-Bohlman, et al., 2004). An important next step will be to investigate relationships between processing capacity, knowledge, and health outcomes and whether these broad cognitive abilities explain the relationship between health literacy and health outcomes.
Third, the sample in the current study was more highly educated than the general population of older adults. Therefore, we may have underestimated relationships between cognitive abilities and health literacy. However, we note that the patterns of associations between the S-TOFHLA and processing capacity measures found in the present study are similar to those found in previous studies that used more diverse samples in terms of education and health literacy (Levinthal et al., 2008; Morrow et al., 2006). Therefore, the associations among processing capacity, knowledge, and health literacy may generalize to other older populations.
A final limitation relates to our measure of health knowledge, because we used a measure of hypertension knowledge to explain performance on general measures of health literacy, which do not directly require knowledge about hypertension. Our goal was to explore relationships between health knowledge and health literacy. Because there is no available standardized measure of general health knowledge, we used a specific measure of hypertension knowledge; many of our participants were diagnosed with hypertension and interpreted it as an important facet of more general health knowledge. In addition, previous work has found that measures of specific illness knowledge have strong connections with health literacy for patients with the specific illness (Gazmararian et al., 2003). Our study replicated these previous results, suggesting that hypertension knowledge, a facet of the more global health knowledge, is associated with health literacy measures.
A separate issue of interpreting the results related to health knowledge and health literacy is the possible reciprocal relationship between health literacy and health knowledge. According to the P-K model, health knowledge is needed to support health literacy (e.g., by reducing demands of comprehension on processing capacity). However, the model also suggests that health knowledge is influenced by health literacy (Figure 1). Patients should acquire more health knowledge by self-care practice or literacy activities with the support of prior health knowledge (Beier & Ackerman, 2005). Therefore, health knowledge can also be regarded as the outcome of growing health literacy. We plan to investigate these possible reciprocal influences in future research.
Overall, to the extent health literacy can be achieved by multiple paths based on different constellations of component abilities, it may be promoted by different design and training approaches that leverage these abilities. These include redesigning health information to reduce the demands of comprehension on processing capacity, improving text organization to facilitate comprehension (Morrow, Leirer, Andrassy, Tanke, & Stine-Morrow, 1996) and designing the patient-centered education or training programs to accelerate knowledge acquisition. Overall, the connections of health literacy to health knowledge, domain-general knowledge, and processing capacity offer many opportunities to promote patients’ health literacy, which provides a foundation to improve self-care and health outcomes.
Acknowledgments
We thank Brennan Payne, Laura D’Andrea, Maryrose Buttice and research coordinators in OSF Saint Francis Medical Center for their assistance on research. This material is based on work supported by the National Institute of Aging (Grant R01 AG31718). Any opinions, findings, and conclusions or recommendations expressed in this publication are those of the authors and do not necessarily reflect the views of the NIH.
Footnotes
Publisher's Disclaimer: Full terms and conditions of use: http://www.tandfonline.com/page/terms-and-conditions
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan, sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
Portions of the data herein were presented at the 117th Annual Convention of the American Psychology Association, Toronto, Canada, August 2009, and the second Health Literacy Research Conference, Bethesda, October 2010.
Contributor Information
Jessie Chin, University of Illinois, Urbana-Champaign, Urbana, Illinois, USA.
Daniel G. Morrow, University of Illinois, Urbana-Champaign, Urbana, Illinois, USA
Elizabeth A. L. Stine-Morrow, University of Illinois, Urbana-Champaign, Urbana, Illinois, USA
Thembi Conner-Garcia, University of Illinois College of Medicine, Peoria, Illinois, USA.
James F. Graumlich, University of Illinois College of Medicine, Peoria, Illinois, USA
Michael D. Murray, Purdue University and the Regenstrief Institute, West Lafayette, Indiana, USA
References
- American Heart Association. Heart disease and stroke statistics—2010 Update. Dallas, TX: American Heart Association; 2010. [Google Scholar]
- American Heart Association. Test your high blood pressure IQ. [Retrieved on February 18, 2009];2007 from: http://www.americanheart.org/presenter.jhtml?identifier=3021399.
- Baker DW. The meaning and the measure of health literacy. Journal of General Internal Medicine. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. Journal of Gerontology: Social Sciences. 2000;55B:368–374. doi: 10.1093/geronb/55.6.s368. [DOI] [PubMed] [Google Scholar]
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Education and Counseling. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian J, Huang J. Health literacy and mortality among elder persons. Archives of Internal Medicine. 2007;167:1503–1509. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Baltes PB. On the incomplete architecture of human ontogeny: Selection, optimization, and compensation as foundation of developmental theory. American Psychologist. 1997;52:366–380. doi: 10.1037//0003-066x.52.4.366. [DOI] [PubMed] [Google Scholar]
- Barnes DE, Tager IB, Satariano WA, Yaffe K. The relationship between literacy and cognition in well-educated elders. Journal of Gerontology: Medical Sciences. 2004;59A:390–395. doi: 10.1093/gerona/59.4.m390. [DOI] [PubMed] [Google Scholar]
- Beier ME, Ackerman PL. Age, ability and the role of prior knowledge on the acquisition of new domain knowledge. Psychology and Aging. 2005;20:341–355. doi: 10.1037/0882-7974.20.2.341. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Davis TC, McCormack L. Health literacy: What is it? Journal of Health Communication. 2010;15:9–19. doi: 10.1080/10810730.2010.499985. [DOI] [PubMed] [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: An updated systematic review. Rockville, MD: Agency for Healthcare Research and Quality; 2011. (Evidence Report=Technology Assessment No. 199. Prepared by RTI International–University of North Carolina Evidence–based Practice Center under contract No. 290–2007-10056-I. AHRQ Publication Number 11-E006.) [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control, and Prevention (CDC) Behavioral risk factor surveillance system survey questionnaire. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- Chin J, D’Andrea L, Morrow DG, Stine-Morrow EA, Conner-Gercia T, Graumlich JF, Murray MD. Cognition and illness experience are associated with illness knowledge among older adults with hypertension. Proceedings of the 53rd annual meeting of the Human Factors and Ergonomics Society, 2009; Human Factors and Ergonomics Society; Santa Monica, CA. 2009. [Google Scholar]
- Chin J, Fu W-T, Kannampallil T. Adaptive information search: Age-dependent interactions between cognitive profiles and strategies. Proceedings of the 27th ACM conference on human factors in computing systems CHI’09; ACM Press; Boston, MA. 2009. [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine. 1993;25:391–395. [PubMed] [Google Scholar]
- Davis TC, Wolf MS, Bass PF, Middlebrooks M, Kennen E, Baker DW, et al. Low literacy impairs comprehension of prescription drug warning labels. Journal of General Internal Medicine. 2006;21:847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Pignone MP. Reading is fundamental: The relationship between literacy and health. Archives of Internal Medicine. 2005;165:1943–1944. doi: 10.1001/archinte.165.17.1943. [DOI] [PubMed] [Google Scholar]
- Ekstrom RB, French JW, Harmon HH, Dermen D. Manual for the kit of factor-referenced cognitive tests. Princeton, NJ: Educational Testing Service; 1976. [Google Scholar]
- Federman AD, Sano M, Wolf MS, Siu AL, Halm EA. Health literacy and cognitive performance in older adults. Journal of the American Geriatrics Society. 2009;57:1475–1480. doi: 10.1111/j.1532-5415.2009.02347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method of grading the state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Education and Counseling. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- Horn JL, Hofer SM. Major abilities and development in the adult period. In: Sternberg RL, Berg CA, editors. Intellectual development. New York, NY: Cambridge University Press; 1992. pp. 44–99. [Google Scholar]
- Johnson RE. Aging and the remembering of text. Developmental Review. 2003;23:261–346. [Google Scholar]
- Katz JN, Chang LC, Snagha O, Fossel, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Kilander L, Nyman H, Boberg M, Hansson L, Lithell H. Hypertension is related to cognitive impairment: A 20-year follow-up of 999 men. Hypertension. 1998;31:780–786. doi: 10.1161/01.hyp.31.3.780. [DOI] [PubMed] [Google Scholar]
- Kintsch W. Comprehension: A paradigm for cognition. New York, NY: Cambridge University Press; 1998. [Google Scholar]
- Krampe RT, Charness N. Aging and expertise. In: Ericsson KA, Charness N, Feltovich P, Hoffman R, editors. Cambridge handbook of expertise and expert performance. Cambridge, UK: Cambridge Press; 2006. pp. 723–742. [Google Scholar]
- Levinthal BR, Morrow DG, Tu W, Wu J, Young J, Weiner M, Murray MD. Cognition and health literacy in patients with hypertension. Journal of General Internal Medicine. 2008;23:1172–1176. doi: 10.1007/s11606-008-0612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsiske M, Willis SL. Dimensionality of everyday problem solving in older adults. Psychology and Aging. 1995;10:269–283. doi: 10.1037//0882-7974.10.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS. Age differences in the effects of domain knowledge on reading efficiency. Psychology and Aging. 2009;24:63–74. doi: 10.1037/a0014586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LMS, Stine-Morrow EAL, Kirkorian HL, Conroy ML. Adult age differences in knowledge-driven reading. Journal of Educational Psychology. 2004;96(4):811–821. [Google Scholar]
- Morrow DG, Clark D, Tu W, Wu J, Young J, Weiner M, et al. Correlates of health literacy in older adults with chronic heart failure. The Gerontologist. 2006;46:669–767. doi: 10.1093/geront/46.5.669. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Leirer V, Altieri P, Fitzsimmons C. When expertise reduces age differences in performance. Psychology and Aging. 1994;9:134–148. doi: 10.1037//0882-7974.9.1.134. [DOI] [PubMed] [Google Scholar]
- Morrow DG, Leier VO, Andrassy JM, Tanke ED, Stine-Morrow EAL. Age differences in schemes for taking medication. Human Factors. 1996;38:556–573. doi: 10.1518/001872096778827305. [DOI] [PubMed] [Google Scholar]
- Nelson DE, Holtzman D, Bolen J, Stanwyck CA, Mack KA. Reliability and validity of measures from the behavioral risk factor surveillance system (BRFSS) Social and Preventive Medicine. 2001;46:3–42. [PubMed] [Google Scholar]
- Nielsen-Bohlman L, Panzer AM, Kindig DA. Health literacy: A prescription to end confusion (Institute of Medicine Report) Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- Oliveria SA, Chen RS, McCarthy BD, Davis CC, Hill MH. Hypertension knowledge, awareness, and attitudes in a hypertensive population. Journal of General Internal Medicine. 2005;20(3):219–225. doi: 10.1111/j.1525-1497.2005.30353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. Journal of General Internal Medicine. 2005;20:1–10. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Radvansky GA, Dijkstra K. Aging and situation model processing. Psychonomic Bulletin and Review. 2007;14:1027–1042. doi: 10.3758/bf03193088. [DOI] [PubMed] [Google Scholar]
- Rudd R. Health literacy skills of U.S. adults. American Journal of Health Behavior. 2007;31:S8–S18. doi: 10.5555/ajhb.2007.31.supp.S8. [DOI] [PubMed] [Google Scholar]
- Salthouse TA. Mediation of adult age differences in cognition by reductions in working memory and speed of processing. Psychological Science. 1991;2:179–183. [Google Scholar]
- Smith KW, Sasaki MS. Decreasing multicollinearity: A method for models with multiplicative functions. Sociological Methods Research. 1979;8:35–56. [Google Scholar]
- Stanovich KE, West RF, Harrison M. Knowledge growth and maintenance across the life span: The role of print exposure. Developmental Psychology. 1995;31:811–826. [Google Scholar]
- Stine EAL, Wingfield A. How much do working memory deficits contribute to age differences in discourse memory? European Journal of Cognitive Psychology. 1990;2:289–304. [Google Scholar]
- Stine-Morrow EAL, Miller LMS, Hertzog C. Aging and self-regulated language processing. Psychological Bulletin. 2006;132:582–606. doi: 10.1037/0033-2909.132.4.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy People. 2010. 2nd ed. Understanding and improving health and objectives for improving health. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Uttl B. North American adult reading test: Age norms, reliability and validity. Journal of Clinical and Experimental Neuropsychology. 2002;24:1123–1137. doi: 10.1076/jcen.24.8.1123.8375. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Wechsler D. Wechsler adult intelligence test manual. 3rd ed. San Antonio, TX: Psychological Corporation; 1997. [Google Scholar]
- Wolf MS, Wilson AH, Rapp DN, Waite KR, Bocchini MV, Davis TC, Rudd RE. Literacy and learning in health care. Pediatrics. 2009;124:275–281. doi: 10.1542/peds.2009-1162C. [DOI] [PMC free article] [PubMed] [Google Scholar]