Abstract
Background
Patients with tibial plateau fractures are believed to have an increased risk for posttraumatic arthritis that may require reconstructive surgery. The incidence of this problem is, however, unknown. We sought to determine the average 10-year incidence of posttraumatic arthritis necessitating reconstructive surgery following tibia plateau fractures.
Methods
We used data from our orthopedic trauma database to identify patients with operatively treated tibia plateau fractures. Their cases were cross-referenced with the data from our province’s administrative health database and tracked over time for the performance of reconstructive knee surgery. The average follow-up was 10 years.
Results
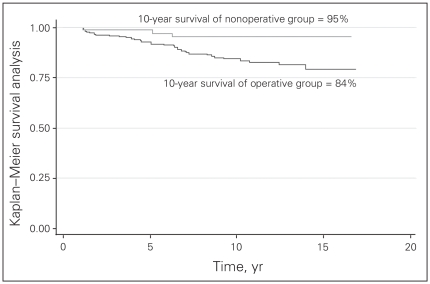
There were 311 tibial plateau fractures treated at our institution between 1987 and 1994. The 10-year Kaplan–Meier survival analysis for the primary outcome of endstage arthritis was 96%. Analysis of the secondary outcome measure, specifically surgeries for what was thought to be “minor arthritis,” revealed a 10-year Kaplan–Meier survival of 87%.
Conclusion
Our findings may be used to counsel patients who require surgical treatment of tibia plateau fractures about the long-term risk of requiring reconstructive knee surgery for endstage arthritis in the knee.
Abstract
Contexte
On croit que les patients atteints d’une fracture du plateau tibial risquent davantage de souffrir d’arthrite post-traumatique pouvant nécessiter une chirurgie reconstructive. L’incidence de ce problème est toutefois inconnue. Nous avons cherché à déterminer l’incidence moyenne à 10 ans de l’arthrite post-traumatique nécessitant une chirurgie reconstructive à la suite d’une fracture du plateau tibial.
Méthodes
Nous avons utilisé des données tirées de notre base de données sur les traumatismes orthopédiques pour trouver des patients qui avaient subi une fracture du plateau tibial réduite chirurgicalement. Ces cas ont été reliés aux données tirées de la base de données administratives sur la santé de notre province et nous les avons suivis dans le temps pour voir le résultat de la chirurgie reconstructive du genou. Le suivi moyen était de 10 ans.
Résultats
Notre rétablissement a traité 311 fractures du plateau tibial entre 1987 et 1994. L’analyse de Kaplan–Meier sur la survie à 10 ans, pour une issue principale d’arthrite au stade ultime, a donné un résultat de 96 %. L’analyse de Kaplan–Meier de la mesure de l’issue secondaire, et plus précisément des chirurgies pour ce que l’on considérait comme une « arthrite mineure », a révélé un taux de survie à 10 ans de 87 %.
Conclusion
Nos constatations pourraient servir à conseiller les patients qui ont besoin d’un traitement chirurgical d’une fracture du plateau tibial au sujet du risque à long terme d’avoir besoin d’une chirurgie reconstructive du genou pour une arthrite du genou au stade ultime.
Displaced intra-articular fracture is considered to be a major risk factor for posttraumatic osteoarthritis. Intra-articular fracture of a major weight-bearing joint of the lower extremity, such as a tibial plateau fracture, is thought to carry an even higher risk. In counselling patients with tibial plateau fractures, an important topic to discuss is the long-term incidence of osteoarthritis. Patients want to know if they are at risk for posttraumatic osteoarthritis, and if so, they want to know about how long it takes for symptomatic arthritis to develop and how long before it becomes severe enough to require major surgical intervention.
The sparse literature on this topic reports an incidence of posttraumatic arthritis following tibia plateau fracture of 23%–44%.1–3 Some of these studies had small cohorts, with as few as 21 individuals. Some of the studies involved surgical techniques that are no longer employed. For example, a complete open meniscectomy was performed for patients who had an associated meniscal tear. Most importantly, none of the studies performed a survival analysis.
In view of these limitations, the long-term risk of end-stage posttraumatic arthritis remains unclear. A potential solution is to use an administrative database in the setting of a universal socialized health care system — a strategy that improves the potential to investigate a large cohort. We sought to determine the long-term incidence of end-stage arthritis following tibial plateau fractures and the expected time delay until necessary surgical intervention.
Methods
Study design
This is a retrospective cohort study that uses an institutional research trauma registry in conjunction with a governmental medical administrative database.
Study population and databases
The study population included all patients with a tibial plateau fracture who had been treated at the Vancouver General Hospital under the care of the orthopedic trauma team. Because the study population consisted of a finite and manageable number, all of the elements of this group were sampled.
We used the computerized trauma database at our institution to identify all patients with a tibial plateau fracture treated before 1995. This cohort was cross-referenced with British Columbia’s linked health database (BCLHD) at the Centre for Health Services and Policy Research (CHSPR; www.chspr.ubc.ca/), which is a provincial administrative health database that may be used to track all of an individual’s interactions with the health care system. The BCLHD was transitioned to Population Data BC (www.popdata.bc.ca) in 2009. The combination of these 2 databases facilitated measuring the duration of clinical follow-up and identifying the primary and secondary outcome measures. Because a patient’s Medical Services Plan (MSP) number is necessary to cross-reference them among different databases, patients whose MSP numbers could not be identified were excluded from the study.
We received no external funding for this study. The University of British Columbia’s Clinical Research Ethics Board approved our study protocol.
Databases
Hospital orthopedic trauma database
We used our hospital’s orthopedic trauma database — a repository of prospectively collected data that generates a case for each admitted individual who has been treated for orthopedic traumatic injuries at our institution. Each week, the database administrative staff, in conjunction with the surgeons, validate admission–discharge–transfer (ADT) data uploaded from the hospital’s information system and add clinical information. Tibia plateau fractures had been classified based on the Mason–Hohl classification system (Box 1).4 The condition of the skin had also been recorded in the database, differentiating open and closed fractures. The Gustilo–Anderson classification was used to grade open fractures.5
Box 1. Mason–Hohl tibia plateau fracture classification.
Type I (undisplaced split)
Type II (local compression)
Type III (split depression)
Type IV (condylar compression)
Type V ( split coronal)
Type VI (comminuted)
British Columbia linked health database
The BCLHD was developed as a cooperative effort of the province’s Ministry of Health and the CHSPR at the University of British Columbia. Person-specific information is linked across administrative data files dating back to April 1985. The following databases are linked:
the MSP database, which records dated fee-for-service claims and payments to physicians and alternative providers related to an individual;
the hospital separations database, which details all hospital admissions with respect to dates, admitting diagnosis, comorbidities, procedures and discharge disposition for the individual;
the home and facility-based continuing care database, which records the living arrangement of the patient on admission and discharge from acute care facilities and any housing or social support provided by the province;
the PharmaCare database, which provides pharmaceutical data related to patients’ prescriptions; and
the vital statistics database, which provides information on individual-specific births and deaths for the province.
Although the linkage is not perfect, the BCLHD was able to link more than 95% of records in all program areas in all years during the study period.
Outcome measures
Primary outcome measure
The primary outcome measure of this study was endstage osteoarthritis, which is defined as arthritis severe enough to require reconstructive surgery, such as total knee arthroplasty, unicompartmental knee arthroplasty, high tibial osteotomy, knee arthrodesis or revision knee arthroplasty (Table 1). The code for revision knee arthroplasty was included because a total knee arthroplasty following a previous tibial plateau fracture is a more complex reconstructive procedure, and our strategy therefore accounted for differing billing practices as the procedures were identified using the MSP billing codes/fee items.
Table 1.
List of procedures and billing codes used as the primary outcome measure of endstage knee arthritis requiring reconstructive surgery
| Procedure and billing code after 1996/97 fiscal year | Procedure and billing code prior to 1996/97 fiscal year |
|---|---|
| 56662 Total knee arthroplasty | 5519 Knee prosthesis |
| 56661 Unicompartmental knee arthroplasty | 5520 Arthroplasty knee |
| 56664 Revision knee arthroplasty | 5524 Knee revision (arthroplasty) |
| 56602 High tibial osteotomy | 5461 Osteotomy, major bones |
| 56603 Osteotomy tibia shaft | 5530 Arthrodesis knee, shoulder, elbow, ankle |
| 56810 Knee arthrodesis |
Secondary outcome measure
The secondary outcome measure was symptomatic arthritis that required medical or minor surgical intervention. Based on existing surgical billing codes, one group of procedures was arbitrarily created. All patients who had an arthroscopic débridement of the knee, a diagnostic knee arthroscopy or an intra-articular knee injection were considered to have minor arthritis (Table 2). We acknowledge that knee arthroscopy and débridement are no longer indicated for arthritis in the knee.
Table 2.
List of procedures and billing codes used as the secondary outcome measure of minor arthritis in the knee, necessitating surgery
| Procedure and billing code after 1996/97 fiscal year | Procedure and billing code prior to 1996/97 fiscal year |
|---|---|
| 11600 Knee arthroscopy | 0713 Arthroscopic examination general anesthetic |
| 56405 Knee injection | 0014 Injection, intra-articular |
| 0015 Injection, intra-articular | |
| 56330 Arthroscopic abrasion/débridement | 5509 Arthroscopic débridement of joints (hip, knee, ankle, shoulder) |
Demographic and trauma information
We used the hospital trauma registry to determine patient age and the injury severity.
Statistical analysis
We performed a descriptive analysis to characterize the cohort. The cohort was reviewed to ensure that all participants had at least 2 years of adequate follow-up after the initial tibia plateau fracture. The likelihood of the primary or secondary outcome measures developing was quantified using nonparametric Kaplan–Meier survival analysis. To calculate the survival analysis, we “right censored” patients if they died before reaching the clinical end point. We also “right censored” patients if they had a significant absenteeism from MSP registration, precluding them from adequate follow-up. Furthermore, survival analysis required designation of end points, which are outlined in Tables 1 and 2.
Primary outcome measure
To address the complicated issue of individual absenteeism from MSP registration, we used an arbitrary set of guidelines to determine inclusion/exclusion of each participant. With regards to the primary outcome of endstage arthritis, it was decided that patients with less than 2 years of follow-up would be eliminated from the cohort unless they had already undergone a secondary procedure. Anyone who had reached the primary end point (i.e., undergone one of the reconstructive procedures) less than 2 years after the tibia plateau fracture were individually reviewed to determine whether they should be included in the cohort. One of us (R.M.) reviewed each of these cases to determine how long after the tibia plateau fracture the reconstructive surgery had been performed. A dichotomous group was observed whereby some patients experienced the primary outcome shortly after the injury, whereas others reached the primary outcome shortly before the 2-year cutoff.
Secondary outcome measure
We used a different set of guidelines to evaluate the secondary outcome measure as the end point for the survival analysis. Any member of the cohort who had less than 1 year of adequate follow-up was excluded from the study; therefore, the final cohort used for survival analysis of the secondary outcome measure was different than that used for the survival analysis of the primary outcome measure.
Bias
Being a level 1 trauma institution, our hospital may have treated an above-average proportion of patients with complex tibial plateau fractures, which may not have been representative of the distribution of the severity of fractures at other sites. This may have yielded an artificially inflated incidence of endstage arthritis. Another potential source of bias was that the surgeries were performed by a group of expert fracture surgeons.
Results
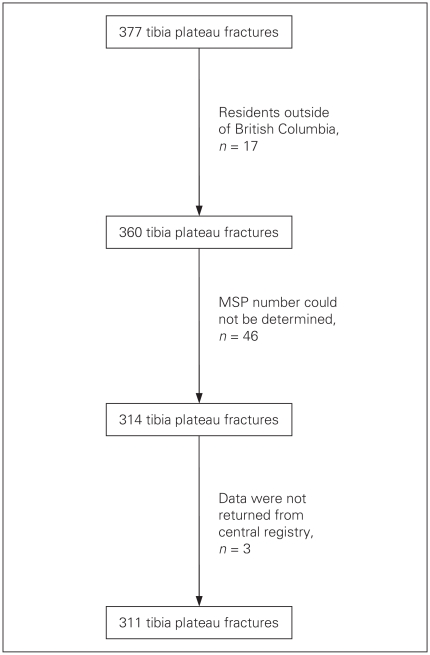
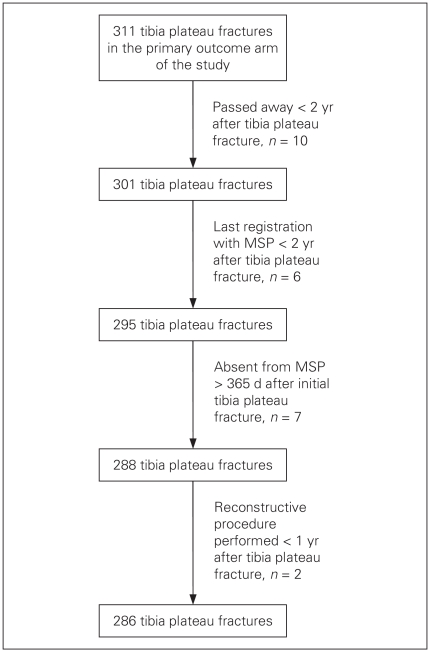
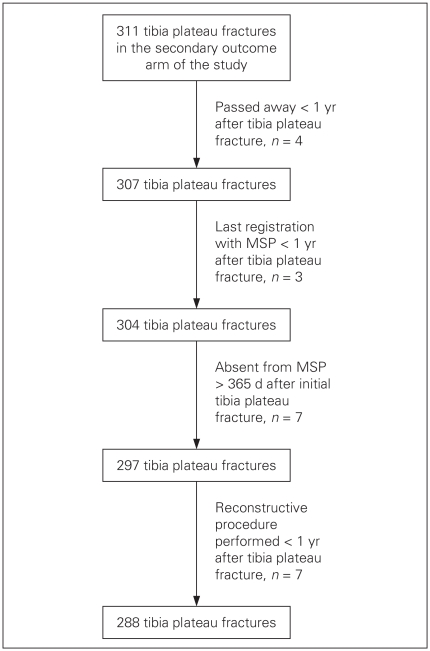
Between 1987 and 1994, 377 patients with tibia fractures were treated at our institution. About 44% of the patients were female and 56% were male. We excluded 17 patients from our analysis because they resided outside of the province, and we excluded 46 because their MSP numbers could not be identified (7 were Workman’s Compensation Board (WCB) patients and 1 was affiliated with the military). After evaluating the data from CHSPR, it became apparent that they had missed 3 individuals; no information regarding their MSP was available. There were 311 patients for whom data were available for analysis (Fig. 1). After applying the exclusion criteria outlined previously, 286 patients remained in the primary outcome cohort, and 288 remained in the secondary outcome cohort (Figs. 2 and 3).
Fig. 1.
Initial cohort. MSP = Medical Services Plan.
Fig. 2.
Cohort for primary outcome measure. MSP = Medical Services Plan.
Fig. 3.
Cohort for secondary outcome measure. MSP = Medical Services Plan.
The final study cohort used to analyze the primary outcome of endstage arthritis necessitating reconstructive surgery consisted of 286 patients with tibial plateau fractures, of whom 77% were initially treated operatively and 23% were managed nonoperatively. The mean age of the operative group was 44 (standard deviation [SD] 17, range 14–87) years, whereas the mean age of the nonoperative group was 52 (SD 19, range 18–87) years. Using the Mason–Hohl classification, the types of tibia plateau fractures was calculated for the operative and nonoperative groups. The nonoperative group had a larger proportion of type-I and type-II injuries. The cumulative frequency of type-I and type-II fractures was 60% in the nonoperative group compared with 17% in the operative group. The mechanisms of injury are outlined in Table 3. In the entire cohort, the 3 most common causes of injury were pedestrian–motor vehicle crashes (31%), fall < 1 meter (3 feet) (13%) and motor vehicle crashes (11%). Most injuries were closed fractures (85%), and only 5% of injuries were associated with severe open soft tissue damage (Table 4).
Table 3.
Mechanism of injury
| Mechanism | Frequency, no. (%) |
|---|---|
| Pedestrian–motor vehicle crash | 90 (31.47) |
| Fall < 1 m or 3 feet | 37 (12.94) |
| Not specified | 34 (11.89) |
| Motor vehicle–motor vehicle crash | 17 (5.94) |
| Motor vehicle | 13 (4.55) |
| Motorcycle–motor vehicle crash | 16 (5.59) |
| Fall 1–3 m or 3–20 feet | 14 (4.90) |
| Motorcycle | 12 (4.20) |
| Bicycle | 13 (4.55) |
| Twisting injury | 10 (3. 50) |
| Fall > 6 m or 20 feet | 8 (2.80) |
| Blow | 6 (2.10) |
| Fall from unspecified height | 4 (1.40) |
| All terrain vehicle crash | 3 (1.05) |
| Aircraft injury | 2 (0.70) |
| Shotgun | 2 (0.70) |
| Crushing injury | 1 (0.35) |
| Electrical | 1 (0.35) |
| Explosion | 1 (0.35) |
| Motor vehicle NFS | 1 (0.35) |
| Watercraft injury | 1 (0.35) |
| Total | 286 (100.00) |
NFS = need for speed.
Table 4.
Skin condition
| Condition | Frequency, no. (%) |
|---|---|
| Normal | 288 (91.71) |
| Open — type I: small wound | 4 (1.27) |
| Open — type II: moderate | 8 (2.55) |
| Open — type IIIA: > 10 cm, high energy | 5 (1.59) |
| Open — type IIIB: > 10 cm, high energy | 6 (1.91) |
| Open —- type IIIC: > 10 cm, associated vascular injury | 3 (0.96) |
| Total | 314 (100.00) |
Primary outcome
The average follow-up for the entire group was 11 (SD 3.7, range 2–17) years. Of all patients with tibia plateau fractures, 13 (4.5%) underwent one of the reconstructive procedures for endstage arthritis. Of these, 8 required a knee arthroplasty. In this cohort, endstage arthritis occurred at a mean delay of 4.6 (SD 3.7, range 1.4–11.1) years following the tibia plateau fracture.
In the nonoperative group, 4 patients (6.0%) underwent one of the reconstructive procedures, 3 of whom required a knee arthroplasty. Endstage arthritis occurred at a mean delay of 4 (SD 3.8, range 1.9–9.8) years following the initial injury. In the operative group, 9 patients (3.5%) underwent one of the reconstructive procedures, 5 of whom required a knee arthroplasty. Endstage arthritis occurred at a mean delay of 5 (SD 3.9, range 1.4–11.1) years.
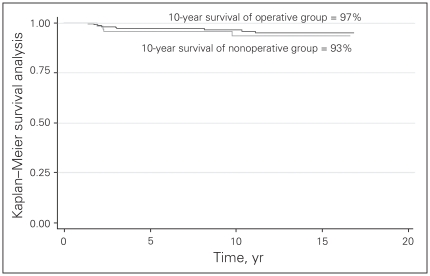
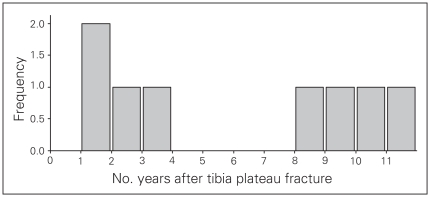
The 10-year Kaplan–Meier survival analysis demonstrated that 96% of patients with tibia plateau fractures had not required reconstructive surgery (total or unicompartmental knee arthroplasty, knee arthrodesis, realignment osteotomy) for endstage arthritis. The 10-year Kaplan–Meier survival for the operative group was 97%, whereas for the nonoperative group it was 93% (Fig. 4). However, it is important to note that patients in the operative and non-operative groups had different types of fractures so their results cannot be compared. In contrast, if the analysis was limited to those who required a total knee arthroplasty, the 10-year Kaplan–Meier survival analysis demonstrated that 98% of patients had not required knee arthroplasty. Limiting our analysis to total knee arthroplasty as the end point, 8 patients had required this procedure. There was a bimodal distribution of the need for this procedure (Fig. 5), with 1 group undergoing knee arthroplasty about 2 years after tibia plateau fracture repair and the second group requiring knee arthroplasty 10 years after tibia plateau fracture repair.
Fig. 4.
Kaplan–Meier survival analysis of primary outcome measure.
Fig. 5.
Time from initial tibia fracture to reconstructive knee surgery.
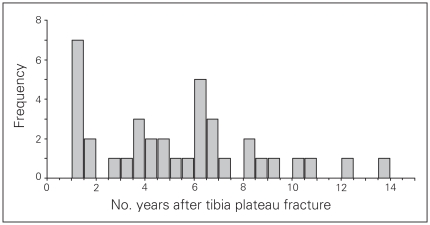
Secondary outcome measure
Analyzing the cohort with regards to the secondary outcome measure, 37 (12.8%) individuals had undergone arthroscopic surgery or had an injection at an average time of 5.5 (SD 3.3, range 1.1–14.0) years following the repair of the initial tibia plateau fracture (Fig. 6). The 10-year Kaplan–Meier survival for this end point was 87%. However, there was a significant difference between the operative and nonoperative groups. Of all the patients who received operative care for their tibia plateau fracture, 16% had one of the elective operative procedures for minor arthritis (intra-articular injection, arthroscopic examination, arthroscopic débridement/abrasion) within 10 years following the initial injury. On the other hand, only 5% of the nonoperative group underwent one of these elective procedures during this period (Fig. 7).
Fig. 6.
Time from initial tibia fracture to secondary outcome measure.
Fig. 7.
Kaplan–Meier survival analysis of secondary outcome measure.
Internal validation of registry data
We attempted to determine the accuracy of the BCLHD data using 2 different analyses. First, we used the Vancouver General Hospital’s trauma registry to identify patients who had undergone operative and nonoperative treatment. Similarly, the BCLHD, in conjunction with appropriate billing codes, was used to identify whether operative or nonoperative treatment had been administered. Next, we matched the data for each individual and constructed a 2-way table. About 74% of the operative group was matched between the 2 groups, whereas 82% of the nonoperative group was matched. Ideally, one would want 100% agreement between the Vancouver General Hospital’s trauma registry and the BCLHD.
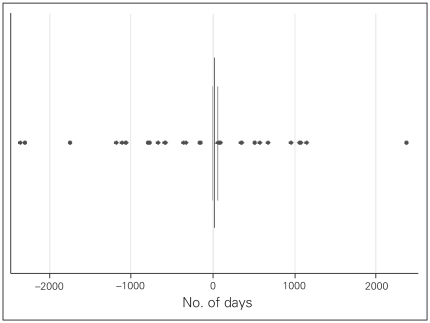
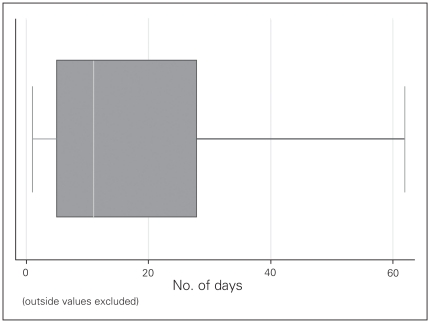
The second means of evaluating the accuracy of the BCLHD was to determine the difference between the hospital discharge date, as recorded in the Vancouver General Hospital’s trauma registry, and the date of the treatment for the tibia plateau fracture, as recorded in the BCLHD. The average difference between the 2 dates was 6 days. When depicted visually in a box plot (Figs. 8 and 9), it appears that most dates were closely matched.
Fig. 8.
Box plot of difference in dates of inital tibia plateau fracture between the Vancouver General Hospital trauma registry and the British Columbia linked health database.
Fig. 9.
Box plot of difference in dates of initial tibia plateau fracture between the Vancouver General Hospital trauma registry and the British Columbia linked health database, with outside values excluded.
Discussion
Tibial plateau fractures are intra-articular fractures that are thought to be associated with long-term risk for posttraumatic arthritis. Although patients with this injury are often advised that they will eventually have endstage arthritis necessitating reconstructive surgery, the actual incidence of this problem is unknown. Other authors have tried to study this question; however, they have been limited by an inadequate number of patients with a long enough clinical follow-up of contemporary surgical treatment.
Rademakers and colleagues6 evaluated 109 patients with tibia plateau fractures who had an average follow-up period of 14 years to determine the long-term functional outcome of operatively treated tibia plateau fractures. The authors also reported complications, one of which was secondary osteoarthritis. They reported a 5% incidence of secondary osteoarthritis that necessitated reconstructive surgery (total knee arthroplasty, realignment osteotomy, knee arthrodesis). However, it is uncertain how long after the initial injury that these secondary reconstructive surgeries were performed.
Several other authors have studied the clinical and functional outcomes of tibia plateau fractures. Unfortunately, to our knowledge, none have evaluated the long-term incidence of endstage posttraumatic arthritis requiring reconstructive procedures.3,7–10
Through the use of the Vancouver General Hospital orthopaedic trauma registry in combination with the BCLHD, we were able to determine the likelihood of a patient with an operatively treated tibial plateau fracture eventually having endstage posttraumatic arthritis severe enough to necessitate reconstructive surgery. The 10-year survival of patients with operatively treated tibia plateau fractures was 97%, and the 10-year survival of the nonoperative group was 93%.
Limitations
Our study has several limitations. One criticism may be that our cohort was not a homogeneous group; in fact, about 30% of the injuries were high-grade type-VI tibia plateau fractures, whereas 35% were lower-grade type-III fractures. This is in contrast to rates reported in the study by Weigel and Marsh,8 who found that 88% of patients had Schatzker type-VI fractures. In a series by Barei and colleagues,7 all patients had AO/OTA (Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association) type 41-C3 fractures, which is the equivalent of a Schatzker type-V or type-VI fracture. In a study by Chin and colleagues,9 14 of 18 patients had a Schatzker type-VI fracture and 4 had a type-V fracture.
Another potential limitation is that we were unable to determine whether patients had underlying osteoarthritis in the knee. Older patients may have had underlying osteoarthritis that would have required a total knee arthroplasty regardless of the superimposed injury. It is certainly plausible that high-grade injuries in older patients are more likely to lead to more severe arthritis; however, there were too few cases of the primary outcome measure to carry out stratified statistical evaluation. Furthermore, the amount of fracture displacement could not be determined for either the operative or nonoperative groups. An unanswered question is whether outcome was influenced most by the initial fracture displacement or by how well we were able to reduce them.
Our results are not immune to the shortcomings that limit all administrative databases. The primary and secondary outcome measures of this study were based on the available data in the BCLHD. The clinical criteria employed to perform knee arthroplasty were therefore not available. This is certainly a valid concern as it is unknown how many patients may have had endstage arthritis, but based on their surgeons’ surgical philosophies they may or may not have been offered reconstructive surgeries. Therefore, the incidence of posttraumatic arthritis following a tibia plateau fracture may be greater than that reported in our study.
Conclusion
Despite its hurdles, to our knowledge, the present study is the first to specifically measure the incidence of endstage posttraumatic osteoarthritis following operatively treated tibia plateau fractures, and it represents the largest cohort with the longest follow-up.
Acknowledgement
The authors thank R. Johal for her assistance in acquiring the data, facilitating the ethics approval and being the backbone of the team.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study. R. Mehin, P. O’Brien, H. Broekhuyse and P. Blachut acquired the data. R. Mehin, P. Blachut and P. Guy analyzed the data. R. Mehin wrote the article, which all authors reviewed and approved for publication.
References
- 1.Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma. 1995;9:273–7. doi: 10.1097/00005131-199509040-00001. [DOI] [PubMed] [Google Scholar]
- 2.Volpin G, Dowd GS, Stein H, et al. Degenerative arthritis after intra-articular fractures of the knee. Long-term results. J Bone Joint Surg Br. 1990;72:634–8. doi: 10.1302/0301-620X.72B4.2380219. [DOI] [PubMed] [Google Scholar]
- 3.Stevens DG, Beharry R, McKee MD, et al. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15:312–20. doi: 10.1097/00005131-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Hohl M. Tibial condylar fractures. J Bone Joint Surg Am. 1967;49:1455–67. [PubMed] [Google Scholar]
- 5.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 6.Rademakers MV, Kerkhoffs GM, Sierevelt IN, et al. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21:5–10. doi: 10.1097/BOT.0b013e31802c5b51. [DOI] [PubMed] [Google Scholar]
- 7.Barei DP, Nork SE, Mills WJ, et al. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg Am. 2006;88-8:1713–21. doi: 10.2106/JBJS.E.00907. [DOI] [PubMed] [Google Scholar]
- 8.Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. J Bone Joint Surg Am. 2002;84:1541–51. doi: 10.2106/00004623-200209000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Chin TY, Bardana D, Bailey M, et al. Functional outcome of tibial plateau fractures treated with the fine-wire fixator. Injury. 2005;36:1467–75. doi: 10.1016/j.injury.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Rasmussen PS. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–50. [PubMed] [Google Scholar]