Abstract
Background
More than 140 000 new cases of cancer are diagnosed annually in Canada, nearly half of which metastasize to bone. The implications for orthopedic oncology services are potentially huge. We reviewed the experience in a major Canadian orthopedic trauma centre treating long bone metastases. The primary aim was to quantify the caseload, and the secondary aim was to report on the methods of fixation.
Methods
We conducted a retrospective review of all patients treated for pathologic lesions or fracture secondary to metastatic disease over a 20-year period from July 1987 to March 2007.
Results
The mean number of cases treated annually was 13. Most patients came from the local oncology centre. The median length of stay in hospital was 11 days. Inhospital mortality was 14%. The fatal pulmonary embolus rate was 5% for femoral lesions. The revision rate for the operative intervention was 3%.
Conclusion
The caseload was much lower than anticipated, likely owing to under-referring from oncology services. The high mortality rate may reflect delay in seeking orthopedic opinion, but overall the fixation methods appeared durable.
Abstract
Contexte
Chaque année, au Canada, plus de 140 000 nouveaux cas de cancer sont diagnostiqués, dont près de la moitié se propagent aux os. Les conséquences pour l’oncologie orthopédique peuvent être énormes. Nous avons passé en revue l’expérience enregistrée dans un grand centre de traumatologie orthopédique canadien qui traite les métastases osseuses. L’objectif principal était d’évaluer quantitativement le volume de cas et l’objectif secondaire était de faire état des méthodes de fixation.
Méthodes
Nous avons procédé à une analyse rétrospective de tous les dossiers de patients traités pour des lésions pathologiques ou des fractures secondaires à la maladie métastatique sur une période de 20 ans, de juillet 1987 à mars 2007.
Résultats
Le nombre moyen de cas traités annuellement était de 13. La plupart des patients étaient adressés par des centres d’oncologie. La durée médiane du séjour hospitalier était de 11 jours. La mortalité perhospitalière était de 14 %. Le taux d’embolie pulmonaire fatale était de 5 % dans le cas des lésions fémorales. Le taux de révision des interventions chirurgicales était de 3 %.
Conclusion
Le volume de cas a été beaucoup moindre que prévu, probablement parce que les centres d’oncologie adressent relativement peu de patients. Le taux de mortalité élevé témoigne peut-être du retard à consulter en orthopédie, mais dans l’ensemble, les méthodes de fixation ont semblé durables.
There were 143 466 new cases of cancer diagnosed in Canada in 2007.1 Bone-seeking tumours (lung, breast, multiple myeloma, renal and prostate) accounted for 45% of these cases, and it was estimated that half of these patients would present with bone metastases during the course of their disease. A further 25% of these new cancers had the potential to metastasize to bone. These figures appear formidable to those in orthopedic service, but the British experience suggests that the orthopedic services are underutilized.2
The aim of this paper was to evaluate the long bone metastatic caseload in a major trauma centre. The secondary aim was to comment on the morbidity and durability of the techniques used.
Methods
We reviewed the cases of all patients treated for pathologic lesions or fracture secondary to metastatic disease over a 20-year period from July 1987 to March 2007. Most referrals of patients with metastatic lesions came from the regional oncology service as part of a program to control their symptoms. The trauma and oncology services provide care for a local population of about 1 million and tertiary support for a population of about 3.5 million.
Patient demographic characteristics, including diagnosis and treatment, were retrieved from the trauma unit’s prospectively accumulated database. We included all patients with a pathologic fracture or impending fracture in the appendicular skeleton secondary to metastatic disease who were admitted with the intention of operative management. Those patients with a pathologic fracture or impending fracture secondary to a benign neoplasm or a primary bone tumour were excluded.
Treatment of an impending fracture was undertaken in conjunction with the oncology service for symptoms not controlled by radiotherapy and radiographic evidence suggesting critical loss of osseous architecture. In addition to consulting the database, we contacted the patients’ family physicians to confirm the date of death and that there had been no revision surgery in other centres that had not been recorded in the local database.
Results
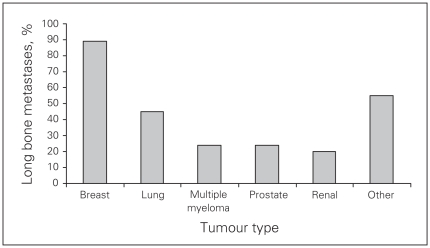
In all, we included 257 patients treated between July 1987 and March 2007 in our analysis, representing an annual mean of 13 patients. Of the 257 patients, 26 were still alive at the time of data retrieval (range 0–6579 d from index procedure). For 33 patients, no information on survival and no record of death could be traced. The sites of the pathologic lesions or fractures were as follows: 182 femur (50 impending), 56 humerus (9 impending), 7 radius, 11 tibia (3 impending) and 1 ulna. The median length of stay in hospital was 11 days (8 d for patients with humerus lesions or fractures and 12 d for those with femur lesions or fractures). Figure 1 illustrates the percentage of long bone metastases among patients with the main 5 tumour types. Patients with breast tumours represented the bulk of referrals. Four patients with fractures were treated palliatively without operation.
Fig. 1.
Percentage of long bone metastases among patients with the main 5 tumour types.
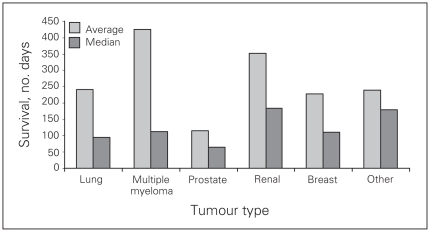
Figure 2 summarizes survival among patients with the 5 main tumour types and femoral metastases. In the femoral metastasis group, 24 patients (14%) did not survive to discharge. Two of the deaths occurred before the planned operative intervention, 2 occurred in the hemiarthroplasty group, and the remaining 20 occurred in the osteosynthesis group. These numbers reflect that the patients had been referred for a palliative procedure and include those who were then treated in hospital until death as part of their oncology care. Cardiorespiratory problems were the most common cause of death in the immediate postoperative period. Six patients had radiographically proven pulmonary emboli (PE), and 5 of them died in the immediate postoperative days. Six people had severe cardiorespiratory compromise of unspecified cause, and 1 of them died. Pulmonary embolic phenomena were suspected clinically in all patients. The rate of PE after treatment of the femoral lesion was 12 out of 175 cases (7%), and that of fatal PE was 6 of 175 (3%). Fatal PE occurred predominantly in the patients treated with intramedullary nailing.
Fig. 2.
Survival after orthopedic fixation of femoral metastases.
Table 1 lists the orthopedic interventions used in patients with femoral metastases. We had no meaningful way of comparing the techniques used as they represented different fracture types, and the choice of intervention depended on the character of the lesion and patient. The overall rate of major complications among patients with femoral metastases was 11%. In the osteosynthesis group it was 15 of 145 (10%) compared with 4 of 30 (13%) in the hemiarthroplasty group. Revision of femoral fixation was required in 5 patients, and 1 patient required 2 revisions. Of these, 1 patient was revised to a tumour endoprosthesis after an initial cephalomedullary nail. The remaining patients were revised to cephalomedullary nails, 2 with bone grafting to the initial pathologic site. There were no cases of catastrophic failure of the implants. All revisions were performed owing to increasing pain or concern that the implant was in jeopardy of fatiguing. Cement augmentation was employed for 1 patient with a femoral lesion in this series. No patients in the hemiarthroplasty group underwent revision. There were 2 major wound problems requiring a return to the operating room and 1 case of systemic sepsis. Three patients treated for a femoral lesion had an additional lesion treated during the same admission.
Table 1.
Orthopedic intervention used in the management of femoral metastases, n = 182*
| Fixation type | No. | Complications | Survival, median (range), d | Revision |
|---|---|---|---|---|
| Gamma | 96 | 10 | 112 (0–6234) | 2 |
| Hemiarthroplasty | 30 | 4 | 87 (0–778) | 0 |
| Antegrade nail | 25 | 3 | 46 (0–651) | 1 |
| Dynamic hip screw | 10 | None recorded | 131 (0–194) | 1 |
| Retrograde nail | 3 | 1 | 34 (0–229) | 0 |
| Other | 11 | 1 | 176 (0–2256) | 1 |
Six patients were treated nonoperatively (2 died in hospital before surgery and 4 were discharged to palliative care, all with fractures), and no data were available for 1 patient.
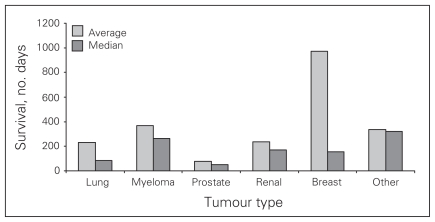
Survival among patients with the 5 main tumour types and humeral metastases is shown in Figure 3. Three of these 56 patients (5%) did not survive to discharge.
Fig. 3.
Survival after orthopedic fixation of humeral metastases.
Table 2 outlines the interventions used in patients with humeral lesions. The overall complication rate among patients with humeral metastases was 9%. There was 1 PE and 1 subclavian thrombus, but both of these patients survived past discharge. There were 2 wound problems requiring a return to the operating room. There were 2 revisions in this group. In both cases a nail was revised to a plate because of fatigue of the initial implant. Both patients had bone grafting to the pathologic site and underwent bone cement augmentation.
Table 2.
Orthopedic intervention used in the management of humeral metastases, n = 55
| Fixation type | No. | Complications | Survival, median (range), d | Revision |
|---|---|---|---|---|
| Intramedullary nail | 44 | 2 | 147 (0–4255) | 2 |
| Plate | 9 | 2 | 141 (0–1153) | 0 |
| Other | 2 | 1 | 230 (0–459) | 0 |
Discussion
The estimated number of patients with cancer who would have bone-seeking tumours and present with bone metastases present a daunting picture for planning orthopedic oncology services. However, the experience outlined in the present paper suggests that the actual numbers are not as overwhelming as initially anticipated, the annual case-load being on average 13 patients. The referral population for our study is difficult to define because most of the referrals came from the regional oncology centre based on the same site. The local population served is about 1 million, and the regional population is 3.5 million. We had anticipated that the workload would be greater than we have reported, and this seems to be the view held in many similar units. However, in the published literature, even the largest centres report an annual caseload of only about 20 patients.3,4 It may be that the literature reflects under-reporting, and it is likely that it under-represents patients amenable to improvement with orthopedic intervention.
Wilkinson and colleagues5 reviewed the management of bone metastases, discussing predominantly the associated pain. They reported that half of all patients with metastatic tumours will present with pain originating from bone lesions. Given that there are more than 140 000 new cases of cancer diagnosed in Canada annually and that our centre represents about one-tenth of the country’s population,6 we had anticipated a much greater orthopedic burden. Radiotherapy can provide some pain relief in up to 80% of patients, but pain relief is not complete in all patients. Wilkinson and colleagues outlined the risk factors for fracture, as reported by Healy and Brown,7 but unfortunately they did not elaborate on when to seek an orthopedic opinion. It seems there is reluctance to consider surgery or ignorance of what additional benefit orthopedics can offer.2 Prompt surgical management can be highly cost effective. The median length of stay in hospital of 11 days among patients in our study is better than that for the hip fracture population.2,7 This suggests that engaging with oncologists to consider available orthopedic interventions might provide more effective overall care in patients with metastatic disease in the long bones.
Operative procedures are not without risk,7 and this may explain some of the reluctance to refer patients to orthopedics. In this study we report a rate of fatal PE of 3.5% for patients with femoral lesions. Our in-hospital mortality rate was 14%, mainly in patients with a pathologic fracture. The mortality rate does seem high, but the procedures were undertaken as palliative interventions and as part of a multi-disciplinary approach, which in many circumstances was part of the patients’ final care. This confirms Tillman’s comment in the British Orthopaedic Association guidelines2 that failure to seek a timely surgical opinion may contribute to some of the poor outcomes reported.
The present study reports on a variety of techniques, all of which are commonly used in any institute with an orthopedic trauma service. As far as we are aware, all patients in whom there are suspected problems with the hardware or potential failure are referred back to orthopedics. Our revision rate of about 3% for femoral and humeral lesions is therefore likely to be an accurate estimate. Therefore, hardware issues or failure are not major problems even without augmentation measures, such as the use of bone cement.3,8 The optimal orthopedic intervention has been debated, but there are no meaningful comparative studies.4,9,10 It is likely that the technique used is a combination of the patient and lesion characteristics and local expertise.11,12 Failure or imminent failure of the initial implant, while not a major problem, does not preclude revision with either endoprosthetic or osteosynthetic methods.9
Conclusion
The metastatic oncology population does not represent a major service burden, but there may be considerable underutilization of orthopedic interventions. The standard techniques available from an orthopedic trauma service appear durable and effective.
Footnotes
Competing interests: M. Kelly declares having received travel support from Stryker. None declared for P. Clarkson, M. Lee and P.J. O’Brien.
Contributors: All authors designed the study. M. Lee, P. Clarkson and P. O’Brien acquired the data, which M. Kelly and M. Lee analyzed. M. Kelly wrote the article, which all authors reviewed and approved for publication.
References
- 1.Canadian Cancer Statistics 2007. Ottawa (ON): Canadian Cancer Society, National Cancer Institute of Canada, Statistics Canada, Provincial/Territorial Cancer Registries, Public Health Agency Of Canada; 2007. [accessed 2012 Mar. 2]. Available: http://bit.ly/szS3BQ. [Google Scholar]
- 2.Tillman RM. Metastatic bone disease: a guide to good practice. London: British Orthopaedic Association and the British Orthopaedic Oncology Society; 2001. [Google Scholar]
- 3.Yazawa Y, Frassica FJ, Chao EY, et al. Metastatic bone disease. A study of the surgical treatment of 166 pathologic humeral and femoral fractures. Clin Orthop Relat Res. 1990;(251):213–9. [PubMed] [Google Scholar]
- 4.Wedin R, Bauer HCF. Surgical treatment of skeletal metastatic lesions of the proximal femur: Endoprosthesis or reconstruction nail? J Bone and Joint Surg Br. 2005;87:1653–7. doi: 10.1302/0301-620X.87B12.16629. [DOI] [PubMed] [Google Scholar]
- 5.Wilkinson AN, Viola R, Brundage MD. Managing skeletal related events resulting from bone metastases. BMJ. 2008;337:a2041. doi: 10.1136/bmj.a2041. [DOI] [PubMed] [Google Scholar]
- 6.Canada’s population estimates. Ottawa (ON): Statistics Canada; 2009. [accessed 2009 Sept. 29]. Available: www.statcan.gc.ca/daily-quotidien/090929/dq090929b-eng.htm. [Google Scholar]
- 7.Healey JH, Brown HK. Complications of bone metastases: surgical management. Cancer. 2000;88(Suppl):2940–51. doi: 10.1002/1097-0142(20000615)88:12+<2940::aid-cncr10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 8.Jacofsky DJ, Haidukewych GJ. Management of pathologic fractures of the proximal femur: state of the art. J Orthop Trauma. 2004;18:459–69. doi: 10.1097/00005131-200408000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Eckardt JJ, Kabo JM, Kelly CM, et al. Endoprosthetic reconstructions for bone metastases. Clin Orthop Relat Res. 2003;(15 Suppl):S254–62. doi: 10.1097/01.blo.0000093044.56370.94. [DOI] [PubMed] [Google Scholar]
- 10.Wedin R, Bauer HCF, Wersall P. Failures after operation for skeletal metastatic lesions of long bones. Clin Orthop Relat Res. 1999;358:128–39. [PubMed] [Google Scholar]
- 11.Park DH, Jaiswal PK, Al-Hakim W, et al. The use of massive endopros-theses for the treatment of bone metastases. Sarcoma. 2007;2007:62151. doi: 10.1155/2007/62151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fuchs B, Trousdale RT, Rock MG. Solitary bony metastasis from renal cell carcinoma: significance of surgical treatment. Clin Orthop Relat Res. 2005;431:187–92. doi: 10.1097/01.blo.0000149820.65137.b4. [DOI] [PubMed] [Google Scholar]