Abstract
Background
Improvements in prevention have led to declines in incidence and mortality of MI in selected populations. However, no studies have examined regional differences in recent trends in MI incidence, and few have examined whether known regional disparities in MI care have narrowed over time.
Methods and Results
We compared trends in incidence rates of MI, associated procedures and mortality for all U.S. Census Divisions (regions) in Medicare fee-for-service patients between 2000 and 2008 (292,773,151 patient-years). Two-stage hierarchical models were used to account for patient characteristics and state-level random effects. To assess trends in geographical disparities, we calculated changes in between-state variance for outcomes over time. While the incidence of MI declined in all regions (P < 0.001 for trend for each) between 2000 and 2008, adjusted rates of decline varied by region (annual declines ranging from 2.9% to 6.1%). Widening geographical disparities, as measured by percent change of between-state variance from 2000 to 2008, were observed for MI incidence (37.6% increase, P = 0.03) and PCI rates (31.4% increase, P = 0.06). Significant declines in risk-adjusted 30-day mortality were observed in all regions, with the fastest declines observed in states with higher baseline mortality rates.
Conclusions
In a large contemporary analysis of geographic trends in MI epidemiology, the incidence of MI and associated mortality declined significantly in all U.S. Census Divisions between 2000 and 2008. While geographical disparities in MI incidence may have increased, regional differences in MI-associated mortality have narrowed.
Keywords: myocardial infarction, Medicare, trends, disparities
Acute myocardial infarction (MI) remains one of the leading causes of morbidity and mortality in the United States. 1 However, over the previous decade, a number of primary and secondary prevention strategies for MI have been adopted, resulting in better control of cardiovascular risk factors. 2–4 Several studies suggest that these improvements are coincident with, and perhaps responsible for, recent declines in the incidence of MI in several populations.5–7
However, geographic variation in the prevalence of coronary risk factors, health care utilization, and coronary disease-related mortality are well known. 8–11 As strategies to prevent MIs have become more widely adopted, understanding whether declines in the incidence of MI have occurred similarly across populations and whether geographic disparities in cardiovascular care have narrowed serves as an important measure of equity in our healthcare system. To date, no studies have examined regional differences in recent trends in MI incidence.
As a large national dynamic cohort of patients for whom demographic and clinical information is collected, Medicare beneficiaries make up one of the few populations that permits an accurate comparison of trends in cardiovascular disease burden across geographic regions. 12, 13 We estimated and compared temporal trends in the incidence of MI, rates of revascularization, and short-term mortality in the Medicare fee-for-service population across geographic regions during the last decade. We sought to examine 1) whether there have been significant regional disparities in MI incidence, treatment and outcomes during this time period and 2) whether these regional disparities have changed over time.
Methods
Study sample
We examined data on individuals enrolled in Medicare fee-for-service (FFS) from the Medicare beneficiary denominator file between January 1, 2000 and December 31, 2008. We identified 394,194,478 beneficiaries totaled over all years of the study. Of these, only beneficiaries older than age 65 at the beginning of each year residing within the 50 states and the District of Columbia were included in the analysis (n = 292,825,626). We calculated person-years of follow-up for each beneficiary to account for new enrollment, disenrollment, or death during an index year. We linked these data with the Medicare Provider Analysis and Review (MEDPAR) files to obtain information on patient demographics, coexisting illnesses, and hospitalization for MI. The MedPAR files contain information on all hospitalizations for FFS Medicare beneficiaries, including demographic information, zip codes of beneficiaries’ primary residence, discharge diagnoses, and procedure codes. We excluded patients that could not be merged with the Medicare denominator file (n = 52,475). Reasons for inability to merge included incorrect MEDPAR beneficiary identification code or gender code. The remaining 292,773,151 beneficiaries were included in the analysis.
Our interest was in measuring the incidence rates of the first hospitalized myocardial infarction each year. We therefore included the first hospitalization for each patient each year with a primary discharge diagnosis of MI based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 410.xx, except 410.x2, similar to previous approaches. 6 Hospitalizations for MI in which patients were discharged alive within 1 day of admission not against medical advice and not transferred to a different facility were excluded, as these are unlikely to have represented true MIs. 14 Hospital transfers occurring within 1 calendar day were linked to form a single episode of care. We excluded patients who were not continuously enrolled in the 12 months period of FFS prior to the index MI hospitalization.
Patient characteristics
We used the Hierarchical Condition Categories (HCC) to assemble variables reflecting patient coexisting conditions. 15 These HCC variables were generated using secondary diagnosis and procedure codes from the index hospitalization, and primary and secondary diagnosis codes from hospitalizations in the 12 months prior to the index MI, including hospitalizations in 1999 for patients hospitalized for MI in the year 2000.
Cardiac catheterization, revascularization, and short-term mortality
To compare trends in the utilization of diagnostic and therapeutic procedures across geographic regions, we identified all cases of in-hospital cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass graft surgery (CABG) up to 30 days after MI using relevant ICD-9-CM and procedure codes (Supplemental Table 1). Similar to previous studies, we selected 30 days following the index event based on the assumption that this would be a sufficient time period to capture the vast majority of associated procedures. 5, 16 We also examined all-cause mortality occurring during the hospitalization and at 30 days after admission, obtained from MEDPAR data and Medicare denominator file, respectively.
Statistical analyses
The principal geographical units of interest were U.S. Census Bureau divisions, due to observed differences in the prevalence cardiovascular risk factors observed between divisions, and states, due to differences in policies influencing cardiovascular public health occurring at the state level. 11, 17 The U.S. Census Bureau has designated grouping of states into the nine census divisions since 1910 for the presentation of data. 18 We assigned all patients to states based on the zip code of their primary residence. We then assigned states to U.S. Census Bureau divisions, denoted here as regions. (Supplemental Table 2) For each year of the study, we calculated crude incidence rates of the first hospitalized MI per 100,000 person-years for each state and region. In addition, we calculated crude rates of cardiac catheterization, PCI, and CABG within 30 days after admission. (Supplemental Figure 1)
Assessing trends
To estimate and compare rates of change in the incidence of MI across regions we developed two-stage hierarchical Poisson regression models. In the first stage, we estimated a model with state-specific random intercepts and state-specific random year effects adjusted for age, sex and race. Year was modeled as a continuous variable after visual inspection of crude incidence rates revealed linear trends. In the second stage, we permitted the state-specific baseline incidences (random intercepts) and state-specific annual rates of change (random slopes) to vary by U.S. Census Division through the inclusion of dummy variables (indicators) for each division.
We used similar methods to compare trends in rates of 30-day cardiac catheterization, PCI, and CABG across regions, adjusted for age, sex and race, and 30-day all cause mortality across regions, adjusted for age, sex, race and comorbidities as ascertained by HCCs. Detailed descriptions of all hierarchical models can be found in the Supplemental Materials.
Testing for geographic disparities
To assess whether geographic differences in incidence, treatment and outcomes of MI widened or narrowed over the study period, we first fitted two separate hierarchical models to obtain between-state variances in the years 2000 and 2008, separately. Specifically, for the year 2000 and then again for the year 2008, we fitted hierarchical models with state-specific random intercepts, adjusted similarly as above but without the variable “year”. We then estimated the percentage change in the between-state variance comparing years 2000 versus 2008. This was performed for adjusted incidence rates of MI, adjusted rates of cardiac catheterization, PCI, CABG, and adjusted 30-day mortality risk over the study period. These values were calculated by subtracting the residual between-state variance estimated in 2000 from that estimated in 2008, and dividing this difference by the residual variance in 2000, e.g. Relative Percent Change = 100 × (τ22008 − τ22000)/τ22000. We tested whether this percentage change was significant using the F-test.
In addition to comparing changes in between-state variation in 2000 and 2008, we also estimated the correlation between state-specific intercepts and slopes as an assessment of whether disparities had increased or decreased over time. For all the end-points, the state-specific intercepts and slopes were obtained from fitting the hierarchical models. The estimated correlations would serve as an assessment of whether those states with the highest rates of MI incidence or mortality in the year 2000 were also the states that experienced the most rapid subsequent decline. The contribution of data points to the correlation was weighted according to the statistical precision of the state-specific estimated slopes.
Analyses were conducted using SAS version 9.2, 64-bit (SAS Institute Inc, Cary, North Carolina), and HLM Version 6 (Scientific Software International, Lincolnwood, Illinois). All reported P values are two-sided at alpha 0.05. The Institutional Review Board of the investigators’ institution reviewed the study, and the requirement for informed consent was waived based on the nature of the study.
Results
From 292,773,151 annual unique beneficiaries, we identified 2,263,614 patients hospitalized with MI between 2000 and 2008. Patient characteristics differed substantially across geographic regions, particularly with regard to race and prior cardiovascular history (Table 1): for example, non-White patients accounted for only 4.3% of patients in the New England and West North Central regions compared to 16.4% of patients in the Pacific region. Patients in the Mountain Division had the lowest rates of congestive heart failure, prior MI, stroke, cerebrovascular disease, and peripheral vascular disease among regions.
Table 1.
Clinical Characteristics of Medicare Fee-for-Service Patients Hospitalized for Myocardial Infarction by U.S. Census Division, 2000–2008.
| Characteristics | EN Central |
ES Central |
Mid Atlantic |
Mountain | New England |
Pacific | South Atlantic |
WN Central |
WS Central |
Overall |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 429994 | 169298 | 347923 | 96596 | 131576 | 195586 | 474129 | 179723 | 238789 | 2263614 |
| Age, mean (SD) | 79.5 (7.6) | 78.6 (7.6) | 80.5 (7.7) | 78.7 (7.5) | 80.4 (7.6) | 79.8 (7.8) | 79.2 (7.6) | 79.5 (7.7) | 78.8 (7.6) | 79.5 (7.7) |
| Female, % | 51.8 | 51.5 | 53.4 | 45.0 | 52.5 | 48.8 | 50.7 | 49.2 | 50.3 | 50.9 |
| White, % | 91.3 | 88.8 | 90.5 | 92.4 | 95.7 | 82.6 | 86.1 | 95.7 | 84.8 | 89.1 |
| Black, % | 6.9 | 10.2 | 6.0 | 1.4 | 2.0 | 3.8 | 10.8 | 2.5 | 8.8 | 6.9 |
| Other, % | 1.8 | 1.0 | 3.6 | 6.2 | 2.3 | 13.6 | 3.1 | 1.8 | 6.4 | 4.0 |
| Anterior MI, % | 11.8 | 12.3 | 11.5 | 15.9 | 11.8 | (13.9 | 11.8 | 13.2 | 12.9 | 12.4 |
| Inferolateral MI, % |
16.0 | 16.5 | 14.1 | 21.6 | 14.7 | 17.8 | 15.3 | 17.8 | 16.4 | 16.1 |
| History of CHF, % | 16.5 | 17.1 | 17.6 | 10.6 | 15.8 | 13.9 | 15.9 | 13.6 | 16.2 | 15.8 |
| History of MI, % | 4.8 | 4.5 | 5.4 | 3.2 | 5.5 | 4.2 | 4.7 | 4.2 | 4.5 | 4.7 |
| Unstable angina, % |
4.4 | 4.7 | 4.8 | 3.4 | 4.6 | 3.9 | 4.9 | 3.9 | 4.6 | 4.5 |
| Chronic atherosclerosis, % |
69.2 | 69.3 | 65.5 | 70.1 | 65.4 | 65.5 | 67.0 | 70.3 | 69.1 | 67.8 |
| Hypertension, % | 59.8 | 60.5 | 60.3 | 56.5 | 59.6 | 56.8 | 59.4 | 58.9 | 60.4 | 59.4 |
| Stroke, % | 2.0 | 2.3 | 2.0 | 1.4 | 1.7 | 1.9 | 2.1 | 1.7 | 2.1 | 2.0 |
| Cerebrovascular disease, % |
5.2 | 5.9 | 5.1 | 3.7 | 4.5 | 4.5 | 5.3 | 4.7 | 5.7 | 5.1 |
| Renal failure, % | 7.1 | 6.5 | 7.0 | 4.4 | 7.1 | 6.0 | 7.0 | 5.1 | 5.8 | 6.5 |
| COPD, % | 24.3 | 26.6 | 23.1 | 21.3 | 22.6 | 21.9 | 25.6 | 21.3 | 23.8 | 23.8 |
| Pneumonia, % | 14.6 | 15.0 | 14.8 | 11.6 | 15.0 | 13.9 | 14.0 | 13.2 | 14.7 | 14.3 |
| Protein calorie malnutrition, % |
3.1 | 3.3 | 2.5 | 2.3 | 1.9 | 2.8 | 3.0 | 2.3 | 3.4 | 2.9 |
| Dementia, % | 10.3 | 11.7 | 11.8 | 7.7 | 10.3 | 10.7 | 10.9 | 8.5 | 10.6 | 10.6 |
| Functional disability, % |
2.8 | 2.6 | 2.9 | 1.8 | 2.3 | 2.8 | 2.6 | 2.2 | 2.9 | 2.6 |
| Peripheral vascular disease, % |
7.1 | 7.2 | 7.0 | 4.7 | 6.6 | 5.5 | 7.2 | 5.8 | 6.9 | 6.7 |
| Metastatic cancer, % |
6.7 | 6.0 | 7.4 | 5.6 | 7.2 | 6.3 | 6.5 | 6.2 | 5.9 | 6.5 |
| Trauma in past year, % |
5.9 | 5.5 | 6.1 | 6.2 | 6.5 | 6.8 | 5.9 | 5.8 | 5.8 | 6.0 |
| Major psychiatric disorder, % |
2.1 | 2.3 | 2.1 | 1.4 | 2.2 | 1.9 | 2.1 | 2.0 | 2.2 | 2.1 |
| Chronic liver disease, % |
0.5 | 0.5 | 0.6 | 0.6 | 0.6 | 0.8 | 0.6 | 0.4 | 0.7 | 0.6 |
| Depression, % | 5.4 | 5.3 | 5.9 | 4.7 | 6.2 | 4.4 | 5.3 | 5.7 | 4.9 | 5.3 |
| Diabetes, % | 31.1 | 31.5 | 32.3 | 25.5 | 30.7 | 29.1 | 31.2 | 28.4 | 31.4 | 30.7 |
Abbreviations: MI, myocardial infarction; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease
Trends in incidence of hospitalized MI and impact on geographic disparities
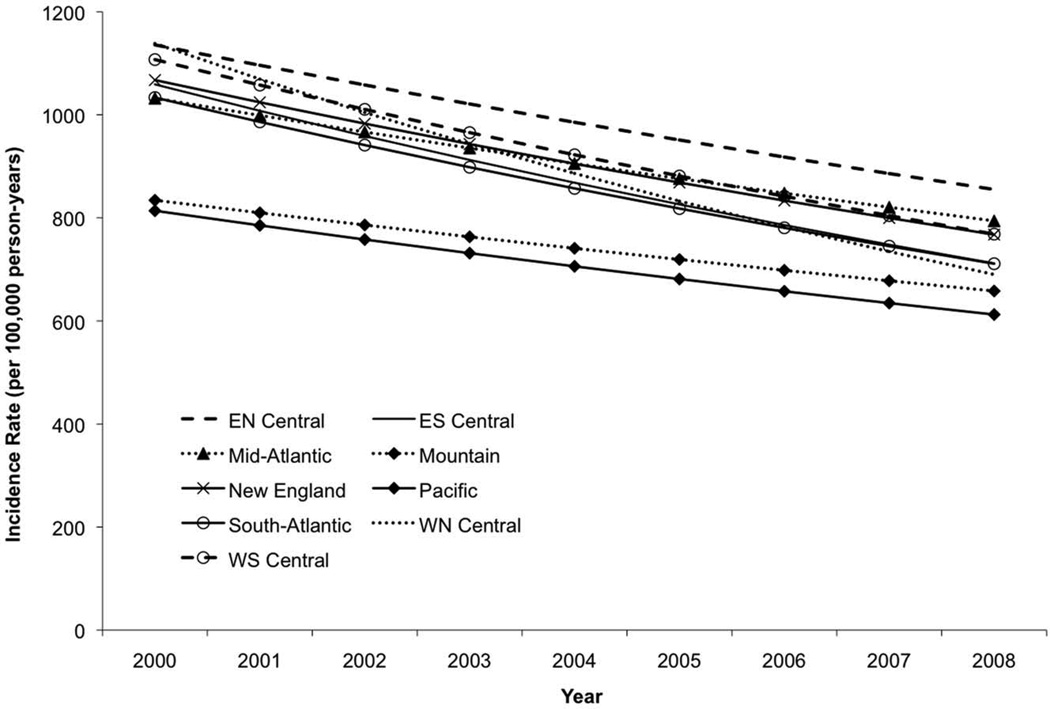
In 2000, there was wide geographic variation in the age-sex-race adjusted incidence of MI, with the lowest rates occurring in the Mountain and Pacific regions. (Figure 1) Thereafter, the adjusted incidence of MI declined in each of the nine regions each year. Rates of decline in MI incidence varied across regions, ranging from 2.9% to 6.1% (national average relative decline of 4.3% per year). (Table 2) As a result of these trends, geographic disparities in MI incidence, as assessed by the between-state variance in incidence rates, increased by a relative 37.6% between 2000 and 2008 (P = 0.03). There was no significant correlation found between age-sex-race adjusted incidence of MI at baseline and subsequent rate of decline (r = 0.046, p = 0.75).
Figure 1.
Temporal trends in age-sex adjusted incidence of hospitalized myocardial infarction by U.S. Census Division within the Medicare fee-for-service population, 2000–2008. Abbreviations: EN, East North; ES, East South; WN, West North; WS, West South.
Table 2.
Temporal Trends in Adjusted Myocardial Infarction Incidence and Rates of Cardiac Catheterization, PCI, CABG and Mortality at 30 Days, 2000 – 2008
| Region | Odds Ratio for Outcome Within 30-days of Admission Each Year Compared to Prior Year |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MI incidence† | Cardiac catheterization‡ | PCI‡ | CABG‡ | Mortality§ | ||||||
| Annual reduction |
95% CI | Odds ratio |
95% CI | Odds ratio |
95% CI | Odds ratio |
95% CI | Odds ratio |
95% CI | |
| Nation | 4.3 | 3.6, 4.9 | 1.04 | 1.04, 1.05 | 1.08 | 1.08, 1.09 | 0.96 | 0.96, 0.97 | 0.97 | 0.96, 0.97 |
| EN Central | 3.5 | 2.7, 4.3 | 1.05 | 1.04, 1.06 | 1.08 | 1.07, 1.09 | 0.97 | 0.96, 0.98 | 0.96 | 0.95, 0.96 |
| ES Central | 4.9 | 3.9, 5.8 | 1.05 | 1.03, 1.06 | 1.08 | 1.07, 1.09 | 0.96 | 0.95, 0.97 | 0.96 | 0.95, 0.96 |
| Mid Atlantic | 3.2 | 1.8, 4.6 | 1.04 | 1.03, 1.06 | 1.09 | 1.08, 1.10 | 0.96 | 0.96, 0.97 | 0.97 | 0.96, 0.97 |
| Mountain | 2.9 | 0.4, 5.3 | 1.05 | 1.03, 1.06 | 1.08 | 1.07, 1.10 | 0.97 | 0.96, 0.98 | 0.98 | 0.97, 0.99 |
| New England |
4.0 | 2.2, 5.9 | 1.05 | 1.03, 1.07 | 1.10 | 1.07, 1.12 | 0.95 | 0.94, 0.97 | 0.97 | 0.96, 0.98 |
| Pacific | 3.5 | 1.0, 5.9 | 1.04 | 1.03, 1.05 | 1.08 | 1.06, 1.11 | 0.97 | 0.95, 0.98 | 0.96 | 0.96, 0.97 |
| South Atlantic |
4.6 | 3.8, 5.3 | 1.05 | 1.03, 1.07 | 1.08 | 1.06, 1.10 | 0.96 | 0.96, 0.97 | 0.96 | 0.96, 0.97 |
| WN Central | 6.1 | 3.3, 8.8 | 1.03 | 1.02, 1.05 | 1.09 | 1.07, 1.10 | 0.97 | 0.96, 0.98 | 0.97 | 0.96, 0.97 |
| WS Central | 4.5 | 3.6, 5.3 | 1.05 | 1.03, 1.07 | 1.08 | 1.07, 1.09 | 0.97 | 0.97, 0.98 | 0.97 | 0.96, 0.98 |
Abbreviations: MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery; CI, confidence interval; EN, East North; ES, East South; WN, West North; WS, West South.
Results are from two stage hierarchical models, as follows:
annual reduction in age-sex-race adjusted AMI incidence;
age-sex-race adjusted odds ratio (OR) of cardiac catheterization, percutaneous coronary intervention, and coronary artery bypass graft surgery compared to prior year; and
comorbidity-adjusted OR of 30-day mortality compared to prior year. Results are reported nationally and separately by U.S. Census Division.
Trends in rates of cardiac catheterization, PCI and CABG and impact on geographic disparities
There was wide variation in the age-sex-race adjusted rates of cardiac catheterization and PCI within 30 days of admission for MI between regions during the entire study period. (Figure 2) Across regions, rates of cardiac catheterization ranged from 43.5% to 60.7%; rates of PCI ranged from 25.3% to 40.3%; and rates of CABG ranged from 9.8% to 12.9%. Rates of procedures were consistently highest in the Mountain division, and lowest in New England and the Mid Atlantic divisions.
Figure 2.
Temporal trends in observed rates of cardiac catheterization and coronary within 30 days after hospitalized myocardial infarction by U.S. Census Division, within the Medicare fee-for-service population, 2000 – 2008. Abbreviations: PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery; EN, East North; ES, East South; WN, West North; WS, West South.
In each region, rates of cardiac catheterization and PCI increased during the initial years of the study, while rates of CABG decreased throughout the time period. These trends persisted after adjustment for age, sex and race. (Table 2)
Geographic variation in rates of PCI after MI tended to increase over the study period (relative increase in between-state variance 31.4% between 2000 and 2008, P = 0.06), while geographic variation in adjusted rates of cardiac catheterization and coronary artery bypass surgery remained stable (relative increase in between-state variance between 2000 and 2008: − 1.0% for cardiac catheterization, P = 0.95; −5.1% for coronary artery bypass graft surgery, P = 0.71). Baseline rates of catheterization, PCI and CABG were not correlated with subsequent rates of increase or decrease in procedure rates among states (r = −0.12, p = 0.42 for catheterization; r = −0.17, p = 0.23 for PCI; r = 0.12, p = 0.41 for CABG).
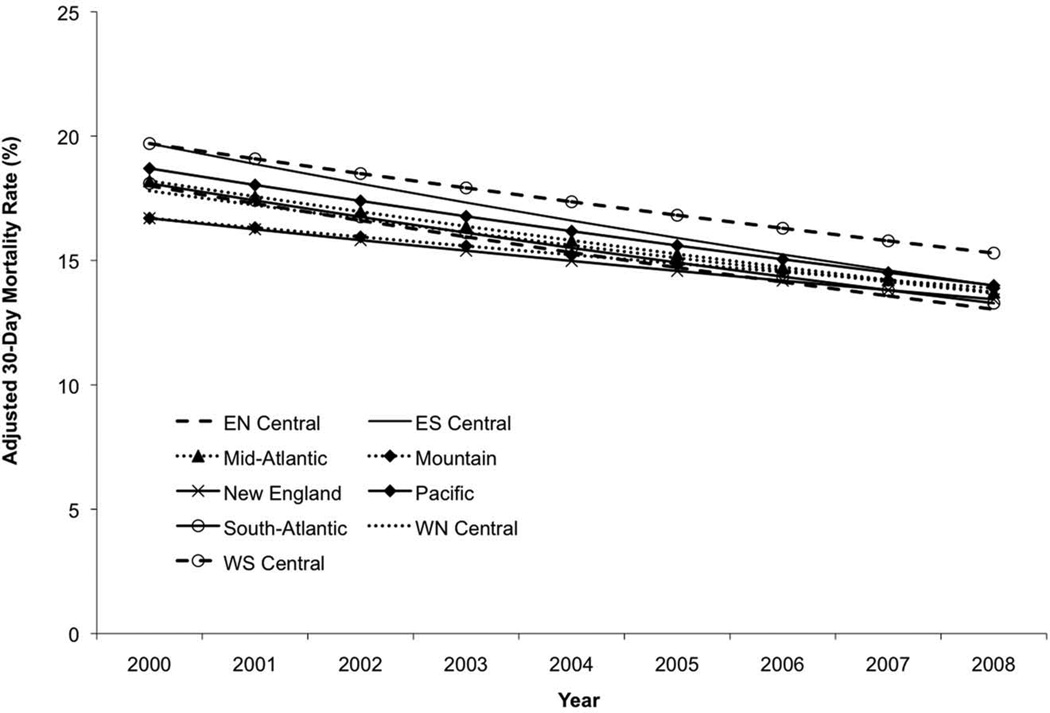
Trends in mortality and impact on geographic disparities
Declines in risk-adjusted 30-day all-cause mortality were seen in each of the nine regions over time (the annual change in the risk adjusted odds ratio for death ranged from 0.96 to 0.98 across regions). (Figure 3) As a result of these trends, percentage change in the between-state variance comparing years 2000 versus 2008 was −31.8%, although the result did not meet statistical significance (P = 0.08). In addition, there was a strong negative correlation between adjusted 30-day mortality at baseline and subsequent rate of decline (r = −0.54, p < 0.001), implying that states with the highest mortality rates in 2000 experienced the most rapid declines in mortality in the subsequent years.
Figure 3.
Temporal trends in adjusted 30-day all-cause mortality after hospitalized myocardial infarction by U.S. Census Division, within the Medicare fee-for-service population, 2000–2008. Abbreviations: EN, East North; ES, East South; WN, West North; WS, West South.
Discussion
In a study including nearly 300 million Medicare fee-for-service beneficiary-years, we have found significant declines in the incidence of MI and associated 30-day mortality in all U.S. Census Divisions. However, there were significant differences in the incidence of MI between geographic regions throughout the study period. In addition, we found strong evidence of a wide and persistent variation in rates of cardiac catheterization and revascularization after MI across regions. Despite these trends, geographical disparities in 30-day mortality after MI have narrowed. To our knowledge, this is the largest study to date that examines geographic differences of trends in acute MI in the U.S. elderly, and the first that examines geographic differences in MI incidence, procedures and 30-day mortality.
Widespread improvements in the treatment of cardiovascular risk factors have occurred in the U.S. over the previous decade. 2–4, 19, 20 Several recent studies have suggested that these improvements may have coincided with declines in the incidence of MI. 5–7 In a study of Medicare beneficiaries between 2002 and 2007, MI incidence fell by 23.4% overall, with black men and women having slower rates of decline compared to their white counterparts. 6 The incidence of MI fell by 24% within the Kaiser Permanente Northern California population between 1999 and 2008, with particularly steep declines in ST-elevation MI. 5 Similar findings have been observed within Olmsted County, Minnesota, where the incidence rate of MI declined by 20% between 1987 and 2006. 7 However, whether these declines have occurred similarly across different U.S. geographic regions had not previously been assessed.
Geographic differences in cardiovascular disease burden in the U.S. are well recognized. In a report among Medicare beneficiaries between 2000 and 2006, the Centers for Disease Control and Prevention found significant geographic disparities in hospitalizations for heart disease, including MI, with the highest rates occurring in Louisiana, Kentucky, Pennsylvania, and West Virginia. 11 In addition, the growth of certain cardiovascular risk factors, including obesity and diabetes, has disproportionately afflicted certain geographic regions, particularly Southern and Southeastern U.S. states. 21, 22 Public smoking bans have been implemented at various times over the previous decade in some but not all cities and states, and the prevalence of smoking continues to vary widely between regions, with Western states showing the lowest rates. 17, 23, 24 In light of these significant and potentially widening geographic differences in the prevalence of cardiovascular risk factors, the possibility existed that MI incidence had not declined similarly across regions. Our findings reassuringly indicate that improvements in the prevention and treatment of MI have indeed occurred across all U.S. Census Divisions despite differences in risk factor burden.
However, while widespread declines in MI incidence and mortality are encouraging, our data also indicate that regional disparities in cardiovascular disease and treatment continue. For example, the Pacific and Mountain divisions had incidence rates of MI that were 20–30% lower than other regions throughout the study period, and regional disparities in MI incidence, as assessed by between-state variation in rates, actually increased by 37% over the study period. Variation in the rates of coronary procedures was substantial at the start of the study period and did not change for cardiac catheterization or CABG, while increasing by one-third for PCI between 2000 and 2008. While procedure appropriateness or feasibility could not be assessed in this study, prior studies have suggested that regional variation in invasive cardiac procedures is more likely attributable to differences in physician practice patterns and systems of reimbursement rather than differences in disease severity or clinical indication. 25–29
Between-state differences in adjusted mortality declined during the study period despite the persistent differences in procedure rates. In addition, states starting with the highest adjusted mortality rates in 2000 also experienced the steepest decline. Both of these findings support the notion that geographical disparities in short-term mortality after myocardial infarction have improved. These consistent reductions in MI-related mortality between regions, contrasted with the heterogeneity in MI incidence, may be reflective of the more pervasive and equitable dissemination of best practices for the management of acute coronary syndromes across U.S. hospitals that has not been matched by equal dissemination of public health and primary prevention efforts. These observations imply that future efforts to reduce disparities in cardiovascular disease burden may be most impactful if they focus on preventing cardiovascular disease occurrence in the outpatient setting as opposed to those aimed at improving hospital care.
This study has a number of limitations. First, the use of more sensitive cardiac biomarkers may have influenced the observed incidence rates of MI. However, as the increased use of these biomarkers in later years would be expected to artificially increase the incidence of MI; in this study, we found that MI incidence has declined in all regions. Therefore it is unlikely that our results are attributable to changes in biomarker sensitivity.
While the vast majority of Medicare beneficiaries are enrolled in the fee-for-service plan, since 2005, a growing percentage has participated in Medicare Advantage managed care plans. 30 It is difficult to determine whether differential enrollment across regions over time in Medicare managed care plans may have contributed to the observed trends. We were only able to capture hospitalized events, including MIs and subsequent procedures. Out-of-hospital MIs not surviving to admission and outpatient catheterization and PCI procedures were not included, and differential trends by region could confound our analysis.
In this study, we relied on administrative claims data for the identification of MI and coexisting illnesses. We were not able to include outpatient information, such as medication use, smoking status, and lipid levels, which might help explain the observed differences in absolute incidence rates of MI at any point in time between regions as well as the observed declines in incidence of MI in all regions. However, at present, the Medicare database is one of the only populations in which population denominators are adequately characterized across all geographic regions in the U.S. to allow a comprehensive regional comparison of MI incidence, treatment and outcomes.
Changes in coding practices for coexisting conditions over time could affect the calculated risk-adjusted mortality rates. However, it has been shown that the association of these comorbid conditions and short-term mortality has not changed over time, arguing against the influence of “drift” in diagnostic coding practices. 15 In addition, as the primary intent of this study was to compare trends across geographic regions, only those temporal changes in coding practices that occurred differentially between geographic regions would be expected to influence the findings.
In summary, the incidence of hospitalized MI and associated 30-day mortality decreased significantly in all U.S. Census Divisions between 2000 and 2008. While wide regional differences in both the incidence of MI and in the use of PCI have continued, disparities in short-term mortality have improved.
What is Known.
-
-
Geographical disparities in cardiovascular disease burden and outcomes in the US are well described historically.
-
-
Several studies have shown recent substantial declines in myocardial infarction incidence and mortality in selected populations.
-
-
Whether these trends have occurred similarly across geographical regions, or whether disproportionate improvements have led to increasing disparities is unknown.
What this Article Adds.
-
-
We demonstrate that significant declines in incidence of myocardial infarction and 30-day mortality have occurred across all US Census Divisions.
-
-
Despite these declines, wide geographical disparities in myocardial infarction incidence and associated rates of percutaneous coronary intervention have persisted, and perhaps widened.
-
-
On the other hand, geographical disparities in 30-day mortality rates after myocardial infarction have declined.
-
-
Efforts to reduce cardiovascular disparities may be best served at disseminating best practices at the primary prevention rather than hospital level.
Supplementary Material
Acknowledgments
Sources of Funding
The project described was supported by Award Number R01ES012054 from the National Institute of Environmental Health Sciences and Award Numbers EPA RD83479801 and EPA RD83489401 from the Environmental Protection Agency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
None.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics-2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31:81–86. doi: 10.2337/dc07-1572. [DOI] [PubMed] [Google Scholar]
- 3.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 4.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: US trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009;150:505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 5.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 6.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 7.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar A, Fonarow GC, Eagle KA, Hirsch AT, Califf RM, Alberts MJ, Boden WE, Steg PG, Shao M, Bhatt DL, Cannon CP. Regional and practice variation in adherence to guideline recommendations for secondary and primary prevention among outpatients with atherothrombosis or risk factors in the United States: a report from the REACH Registry. Crit Pathw Cardiol. 2009;8:104–111. doi: 10.1097/HPC.0b013e3181b8395d. [DOI] [PubMed] [Google Scholar]
- 9.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. Jama. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown JR, O'Connor GT. Coronary heart disease and prevention in the United States. N Engl J Med. 2010;362:2150–2153. doi: 10.1056/NEJMp1003880. [DOI] [PubMed] [Google Scholar]
- 11.Greer SA NI, Capser ML. Atlas of Heart Disease Hospitalizations Among Medicare Beneficiaries. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. 2010 [Google Scholar]
- 12.Ko DT, Wang Y, Alter DA, Curtis JP, Rathore SS, Stukel TA, Masoudi FA, Ross JS, Foody JM, Krumholz HM. Regional variation in cardiac catheterization appropriateness and baseline risk after acute myocardial infarction. J Am Coll Cardiol. 2008;51:716–723. doi: 10.1016/j.jacc.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 13.Krumholz HM, Chen J, Rathore SS, Wang Y, Radford MJ. Regional variation in the treatment and outcomes of myocardial infarction: investigating New England's advantage. Am Heart J. 2003;146:242–249. doi: 10.1016/S0002-8703(03)00237-0. [DOI] [PubMed] [Google Scholar]
- 14.Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995–2006. JAMA. 2009;302:767–773. doi: 10.1001/jama.2009.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krumholz HM, Wang Y, Mattera JA, Han LF, Ingber MJ, Roman S, Normand SL. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 16.Popescu I, Vaughan-Sarrazin MS, Rosenthal GE. Certificate of need regulations and use of coronary revascularization after acute myocardial infarction. Jama. 2006;295:2141–2147. doi: 10.1001/jama.295.18.2141. [DOI] [PubMed] [Google Scholar]
- 17.Juster HR, Loomis BR, Hinman TM, Farrelly MC, Hyland A, Bauer UE, Birkhead GS. Declines in hospital admissions for acute myocardial infarction in New York state after implementation of a comprehensive smoking ban. Am J Public Health. 2007;97:2035–2039. doi: 10.2105/AJPH.2006.099994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau USC. Census 2000 Geographic Definitions. [Accessed August 30, 2011]; Available at: http://www.census.gov/geo/www/geo_defn.html#CensusRegion.
- 19.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 20.Steinberg BA, Bhatt DL, Mehta S, Poole-Wilson PA, O'Hagan P, Montalescot G, Ballantyne CM, Cannon CP. Nine-year trends in achievement of risk factor goals in the US and European outpatients with cardiovascular disease. Am Heart J. 2008;156:719–727. doi: 10.1016/j.ahj.2008.05.020. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 22.Voeks JH, McClure LA, Go RC, Prineas RJ, Cushman M, Kissela BM, Roseman JM. Regional differences in diabetes as a possible contributor to the geographic disparity in stroke mortality: the REasons for Geographic And Racial Differences in Stroke Study. Stroke. 2008;39:1675–1680. doi: 10.1161/STROKEAHA.107.507053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herman PM, Walsh ME. Hospital Admissions for Acute Myocardial Infarction, Angina, Stroke, and Asthma After Implementation of Arizona's Comprehensive Statewide Smoking Ban. Am J Public Health. 2011;101:491–496. doi: 10.2105/AJPH.2009.179572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vital signs: current cigarette smoking among adults aged =18 years --- United States 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1135–1140. [PubMed] [Google Scholar]
- 25.Petersen LA, Normand SL, Leape LL, McNeil BJ. Regionalization and the underuse of angiography in the Veterans Affairs Health Care System as compared with a fee-for-service system. N Engl J Med. 2003;348:2209–2217. doi: 10.1056/NEJMsa021725. [DOI] [PubMed] [Google Scholar]
- 26.Lucas FL, Siewers AE, Malenka DJ, Wennberg DE. Diagnostic-therapeutic cascade revisited: coronary angiography, coronary artery bypass graft surgery, and percutaneous coronary intervention in the modern era. Circulation. 2008;118:2797–2802. doi: 10.1161/CIRCULATIONAHA.108.789446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lucas FL, Sirovich BE, Gallagher PM, Siewers AE, Wennberg DE. Variation in cardiologists' propensity to test and treat: is it associated with regional variation in utilization? Circ Cardiovasc Qual Outcomes. 2010;3:253–260. doi: 10.1161/CIRCOUTCOMES.108.840009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Ann Intern Med. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- 29.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medicare beneficiaries. Managed care versus fee for service. N Engl J Med. 2000;343:1460–1466. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 30.Medicare Advantage Fact Sheet: September 2010. Report from the Henry J Kaiser Family Foundation. [Accessed September 20, 2010];2010 Availabe at www.kff.org/medicare.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.