Abstract
Experimental and clinical studies suggest that gliclazide may protect pancreatic β-cells from apoptosis induced by an oxidative stress. However, the precise mechanism(s) of this action are not fully understood and requires further clarification. Therefore, using human normal and cancer cells we examined whether the anti-apoptotic effects of this sulfonylurea is due to its free radical scavenger properties. Hydrogen peroxide (H2O2) as a model trigger of oxidative stress was used to induce cell death. Our experiments were performed on human normal cell line (human umbilical vein endothelial cell line, HUVEC-c) and human cancer cell lines (human mammary gland cell line, Hs578T; human pancreatic duct epithelioid carcinoma cell line, PANC-1). To assess the effect of gliclazide the cells were pre-treated with the drug. The 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide assay was employed to measure the impact of gliclazide on cell viability. Generation of reactive oxygen species, mitochondrial membrane potential (∆Ψm), and intracellular Ca2+ concentration [Ca2+] were monitored. Furthermore, the morphological changes associated with apoptosis were determined using double staining with Hoechst 33258-propidium iodide (PI). Gliclazide protects the tested cells from H2O2-induced cell death most likely throughout the inhibition of ROS production. Moreover, the drug restored loss of ΔΨm and diminished intracellular [Ca2+] evoked by H2O2. Double staining with Hoechst 33258-PI revealed that pre-treatment with gliclazide diminished the number of apoptotic cells. Our findings indicate that gliclazide may protect both normal and cancer human cells against apoptosis induced by H2O2. It appears that the anti-apoptotic effect of the drug is most likely associated with reduction of oxidative stress.
Keywords: Apoptosis, Gliclazide, Reactive oxygen species, Mitochondrial membrane potential, Calcium
Introduction
Prospective clinical studies and autopsy studies show significant reduction of β-cell function and mass, respectively, in people with type 2 diabetes mellitus (T2DM) [1]. Several factors including hyperglycemia, hyperinsulinemia, hyperlipidemia, low-grade inflammation, and deposition of islet amyloid polypeptide in human pancreas have been proposed to account for this defect in T2DM [2–4]. Chronic hyperglycemia leads to an increased generation of reactive oxygen species (ROS), oxidative stress, and endoplasmic reticulum stress in a variety of cells. In comparison with many other cell types, the β-cells may be at exceptionally high risk of oxidative damage and an increased sensitivity for apoptosis [5, 6].
Apart from a fundamental role of mitochondrial electron transport chain in ROS overproduction, additional sources of ROS may increase oxidative stress in diabetes including glucose autoxidation, protein kinase C activation, methylglyoxal formation and glycation, hexosamine metabolism, and sorbitol formation [2, 4, 7, 8]. Recently published data indicate, that excessive concentration of ROS in diabetes is responsible for the activation of several intracellular signalling pathways, that may affect cell function and structure, increasing the risk of apoptosis [5, 6].
Gliclazide—a second-generation sulphonylurea—is commonly used for the treatment of T2DM. The drug act by stimulating insulin release from the pancreatic β-cells to lower blood glucose. The insulin secretion is triggered by binding of gliclazide to a specific K+ sulfonylurea receptor subtype of ATP-sensitive potassium channels at the level of β-cells plasma membrane (sulfonylurea receptor 1, SUR1), which leads to its closure and subsequent opening of the calcium channels and activation of an effector system of insulin release [9]. The binding of gliclazide to SUR1 is rapidly reversible in contrast to other sulphonylureas (e.g. glibenclamide), that exhibit prolonged binding to SUR1. Besides its hypoglycemic effect, gliclazide has been found to possess extra - pancreatic and antioxidant properties. It appears, that antioxidant activities are independent of any influence on glycemic control [10, 11].
It is of concern, that the long-term use of sulphonylureas, especially glibenclamide, may cause β-cells dysfunction and apoptosis [1]. However, the mechanism(s) of this serious, unwanted effect is unclear and several explanations have been proposed. One of them is an oxidative stress that in people with T2DM is not only related to chronic hyperglycemia but, it is also suggested that insulin secretagogues may directly increase ROS generation and cause an oxidative stress related in β-cell apoptosis [12]. As a consequence of ROS overproduction and its damaging action, b-cell mass and secretory function in T2DM patients treated with sulfonylurea may progressively decline. Insufficient level of insulin in the circulation is responsible for uncontroled hyperglycemia and hyperlipidemia, which in turn cause β-cell damage and induce apoptosis [13, 14]. According to Rustenberg et al. this situation may create a vicious circle, with the improvement of metabolic control being achieved at the expense of an accelerated loss of beta cell mass [8] .
Interestingly enough, it has recently been found that gliclazide prevented mice, rat and human pancreatic β-cells and human endothelial cells from apoptosis [15–19]. It is suggested that this action of the drug is most likely associated with its free radical scavenging properties [20]. However, anti-apoptotic action of gliclazide in other types of cells, especially cancer cells, has not been explored sufficiently. Therefore, the aim of our study was to check whether gliclazide has also ability to prevent human normal (HUVEC-c) and two cancer cell lines (PANC-1 and Hs578T) from apoptosis induced by an oxidative stress. The HUVEC-c cell line as a one of type of human normal endothelial cells has not been explored for this purpose. We believe that PANC-1 and Hs578T cell lines are good candidates for our study as examples of the most common T2DM associated cancers.
Materials and methods
Chemicals
Hydrogen peroxide (H2O2) and gliclazide were obtained from Sigma Chemicals (St. Louis, USA). Kaighn’s modification of Ham’s F-12 medium (F-12K), Dulbecco’s modified Eagle’s medium (DMEM) and fetal bovine serum was supplied by American Type Culture Collection (ATCC) (Rockville, MD, USA). Trypsin–EDTA, penicillin/streptomycin, 2′,7′-dichlorodihydrofluorescein diacetate (DCFH2-DA) and 5,5′,6,6′-tetrachloro-1,1′,3,3′- tetraethylbenzimidazolcarbocyanine iodide (JC-1) were purchased from Sigma. Fluo-4 NW Calcium Assay Kits were obtained from Molecular Probes (Eugene, USA). All other chemicals and solvents were of high analytical grade and were obtained from Sigma or POCH S.A. (Gliwice, Poland).
Cell culture and treatment
The normal cell line (human umbilical vein endothelial cell line—HUVEC-c), and cancer cell lines (pancreatic duct epithelioid carcinoma cell line—PANC-1 and mammary gland cell line—Hs578T) were purchased from ATCC. PANC-1 cell strain is derived from an epithelioid carcinoma of pancreatic duct of 56 year old Caucasian male. Chromosome studies indicate a modal number of 63 with 3 distinct marker chromosomes and a small ring chromosome. This is a hypertriploid cell line. The Hs 578T cell strain is derived from the breast carcinoma of 74 year old Caucasian female. Cytogenetic analysis revealed that Hs578T cell line is a hypotriploid with a modal chromosome number of 59. This cell line does not express estrogen receptor. All cell lines were grown as a monolayer in standard conditions: 37°C, 100% humidity, the atmosphere being 5% CO2 and 95% air with appropriate growth medium: (1) HUVEC-c cell line—F-12K medium supplemented with 0.1 mg/ml heparin and 0.05 mg/ml endothelial cell growth supplement, (2) PANC-1 cell line—DMEM, and (3) Hs578T cell line—DMEM supplemented with 0.01 mg/ml bovine insulin. Complete growth media were supplemented with 10% fetal bovine serum, penicillin (10 U/ml) and streptomycin (50 μg/ml). In all experiments cells in logarithmic phase of growth were used. The cells were monitored periodically for mycoplasma contamination. Cultured cells were removed by trypsinization, resuspended in fresh medium, centrifuged for 5 min at 200×g and plated into 96-well plates at the density of 105 cells/ml (104 cells/well) for 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT), ROS, mitochondrial membrane potential assays or on petri dishes for morphological examination and at the density of 3 × 104 cells for calcium assay according to the manufacture’s protocol. After 24 h (time necessary to ensure, that the cells were in the exponential growth phase) different concentrations of H2O2 were added to the appropriate microplate wells or Petri dishes and the cells were incubated in a CO2 incubator for different period of time (2–72 h) depending on the assessment method.
In some experiments cells were pre-incubated with the 3 mM N-acetylcysteine (NAC) or different concentrations of gliclazide (5–50 μM) for 1 h, then H2O2 at the appropriate subtoxic concentration (50, 100, 200 μM) was added and incubation was continued for the required period of time under the same conditions. After pre-treatment with NAC or gliclazide the media were replaced with fresh ones without NAC or gliclazide. Control cells were treated with a corresponding volume of medium (instead of H2O2 or antioxidants) according to the same schedule. NAC was used as a control agent for gliclazide.
Cytotoxicity assays
The cytotoxicity of H2O2 in human tumor and normal cell lines was measured by a standard microplate MTT colorimetric method [21]. For this purpose 104 cells in 0.1 ml culture medium were seeded to each well. After 24 h, 0.05 ml H2O2 in different concentrations (50–600 μM) was added to appropriate wells, and cells were incubated for 24, 48 or 72 h. After incubation, 50 μl MTT at the final concentration of 6 × 10−3 M in PBS was added to each well and the microplates were incubated in a CO2 incubator for 3 h. After aspiration of the culture medium, the obtained formazan crystals were dissolved in 100 μl dimethyl sulfoxide (DMSO), the plates were mechanically agitated for 1 min, and absorbance at 570 nm was measured with a microplate reader (Awareness Technology Inc., USA). Cytotoxicity of the H2O2 was expressed as IC50 value, which is the concentration of compound that reduces cell viability by 50% relative to the control (untreated cells).
In the experiments with antioxidant, the cells were preincubated with NAC (3 mM) or gliclazide (5–50 μM) and then treated with 50, 100 or 200 μM of H2O2 for 24, 48 or 72 h. The relative number of viable cells was determined by comparing the absorbance of the treated cells with the corresponding absorbance of untreated (control) cells taken as 100%.
Determination of ROS level
Intracellular ROS production was determined directly in cell monolayers in black 96-well flat-bottom microtiter plates using a Fluoroskan Ascent FL microplate reader (Labsystems, Sweden). Cells in complete medium were incubated with 50–200 μM of H2O2 for 2, 4 or 24 h in the presence or absence of the antioxidants (3 mM NAC, gliclazide: 5–50 μM). To measure the production of ROS, cells were treated with 5 μM DCFH2-DA at 37°C for 30 min and the fluorescence of DCF was measured at 530 nm after excitation at 485 nm (DCFH2-DA after deacetylation to DCFH2 is oxidized intracellularly to its fluorescent derivative DCF). Assays were performed in modified Hank’s buffered salt solution (HBSS) (140 mM NaCl, 5 mM KCl, 0.8 mM MgCl2, 1.8 mM CaCl2, 1 mM Na2HPO4, 10 mM HEPES and 1% glucose, pH 7.0).
Mitochondrial membrane potential (ΔΨm)
Cells were seeded in 0.1 ml culture medium into black 96-well titration microplates. After 24 h, 0.05 ml H2O2 (50–200 μM) or an uncoupling mitochondrial agent chlorophenylhydrazone (CCCP) in various concentrations (0.01–10 μM) was added to appropriate wells. The cells were incubated with H2O2 and CCCP for 2, 4 or 24 h. At the end of H2O2 or CCCP treatment, the medium was removed and the cells were incubated with 5 μM JC-1 in HBSS for 30 min, at 37°C, in the dark. Then the fluorescence of both JC-1 monomers and dimers was measured on a Fluoroskan Ascent FL microplate reader (Labsystems, Sweden) using filter pairs of 530 nm/590 nm (dimers) and 485 nm/538 nm (monomers). JC-1 is a fluorescent carbocyanine dye, which accumulates in the mitochondrial membrane in two forms (monomers or dimers), depending on mitochondrial membrane potential. JC-1 monomers show maximum fluorescence excitation and emission at 485 and 538 nm wavelengths, respectively. Negative potential of the inner mitochondrial membrane facilitates the formation of dye aggregates, which results in the shift of JC-1 monomer fluorescence towards red light (from λex = 530 nm to λem = 590 nm) [22]. Thus, the measurement of the JC-1 dimer to monomer fluorescence ratio is a convenient and reliable method for estimation of changes in mitochondrial membrane potential. Prior to fluorescence measurements and taking pictures, the cells were washed twice with HBSS to remove the dye, which could be adsorbed into the microplate well plastic and disturb the measurements. The results in the figures are shown as a ratio of dimer to monomer fluorescence in relation to the control fluorescence ratio, assumed to be 100%. As a positive control for the dissipation of ΔΨm, cells were incubated with an uncoupling mitochondrial agent CCCP.
The cells presented in the pictures in Fig. 5 were pre-incubated with 25 μM gliclazide or 3 mM NAC for 1 h, then H2O2 (200 μM) was added and incubation was continued for the next 4 h. JC-1 fluorescence was photographed immediately after drug treatment.
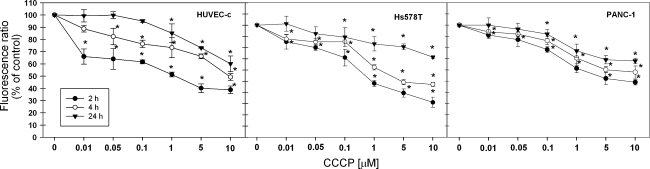
Fig. 5.
Changes in mitochondrial membrane potential (ΔΨm) of HUVEC-c, Hs578T and PANC-1 cells incubated with CCCP for 2, 4 or 24 h. ΔΨm was estimated with a fluorescence dye JC-1 directly in monolayers of cells seeded into black 96-well titration microplates. Fluorescence ratio of JC-1 dimers/JC-1 monomers of control was assumed as 100%. Results are presented as mean ± SD of 3–4 independent experiments. *P < 0.05 in comparison to respective control cells taken as 100%
Monitoring of apoptosis and necrosis
The appearance of apoptotic and necrotic cells was monitored by double staining with Hoechst 33258 and propidium iodide using a fluorescence microscopy (Olympus IX70, Japan; magnification 400×). After 24, 48 or 72 h treatment of cells with 200 μM of H2O2, the cells were removed from the culture dishes by trypsinization, centrifuged and suspended in PBS at the concentration 106 cells/ml. 1 μl Hoechst 33258 (0.13 mM) and 1 μl PI (0.23 mM) were added to 100 μl of cell suspension. After 10 min of incubation at room temperature in the dark, the cells were dropped onto microscopic slides and examined. When antioxidants were included the cells were firstly incubated with 3 mM NAC or 25 μM gliclazide for 1 h, and then with a H2O2 for additional 24, 48 or 72 h. The cells were classified on the basis of their morphological and staining characteristics as: live (mate blue fluorescence), early apoptotic cells (intensive bright blue fluorescence), late apoptotic cells (blue-violet fluorescence) and necrotic (red fluorescence) [23]. Representative areas of cells stained at 48 h of were chosen for documentation.
Intracellular calcium measurement
Control and H2O2 treated cells were seeded into a 96-well plate (3 × 104 cells in 0.2 ml culture medium per well). After 24 h the cells were treated with H2O2 (50–200 μM) for 4, 24, 48 or 72 h. In experiments with antioxidants, cells were preincubated with 3 mM NAC or 5–50 μM gliclazide for 1 h, then H2O2 was added and incubation was continued for another 4, 24, 48 or 72 h. At the end of incubations the medium was removed in order to eliminate sources of baseline fluorescence (the cells were washed twice with PBS). Subsequently cells were incubated with dye loading solution (Fluo-4 NW dye, probenecid, assay buffer—1× HBSS, 20 mM HEPES), which were processed according to the Fluo-4 NW Calcium Assay Kit protocol supplied by the manufacturer (Molecular Probes) and incubated for 30 min in the dark at 37°C, and then for another 30 min at the room temperature. The measurement was done on Fluoroskan Ascent FL microplate reader (Labsystems, Sweden) using 494 nm excitation and 516 nm emission wavelengths.
Statistical analysis
Data are expressed as a mean ± SD. Analysis of ANOVA variance with a Tukey post hoc test was used for multiple comparisons. All statistics were calculated using the STATISTICA program (StatSoft, Tulsa, OK, USA). A P value of <0.05 was considered significant.
Results
Cytotoxicity studies
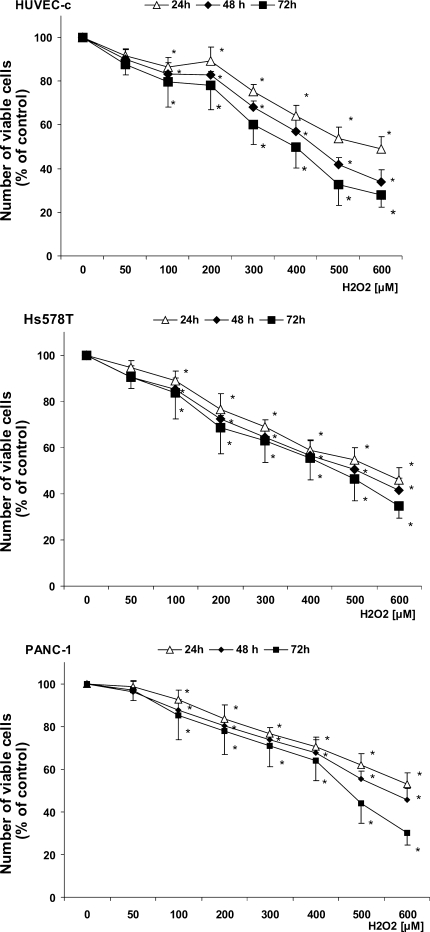
The cytotoxic activity of hydrogen peroxide was determined by the MTT test after 24,48 and 72 h (Table 1). The highest cytotoxicity of H2O2 was observed after 72 h of incubation. The IC50 values of H2O2 after 72 h of treatment were 343 μM, 433 μM and 482 μM for normal cell line (HUVEC-c), breast (Hs578T) and pancreatic cancer cell line (PANC-1), respectively (Table 1) (P ≤ 0.005). Thus, the Hs578T cells and PANC-1 cells were about 1.3 and 1.4 fold more resistant to the H2O2 than the normal cells (HUVEC-c). To discriminate the differences between early and the late effects of H2O2 action, the investigated cell lines were exposed to increasing hydrogen peroxide concentrations for 24, 48 and 72 h. The results revealed the marked differences between 24 and 72 h of incubation. As shown in Fig. 1, 24 h of incubation with toxic (600 μM) concentration of H2O2 reduced a viability of tested cells to about 50% in relation to 72 h exposure (30% of control) (P ≤ 0.05). A comparison of cell viability after 24 and 72 h treatment with H2O2 revealed that the duration of treatment is an important factor for H2O2 cytotoxic effects. Experimental data indicate that nontoxic concentration of H2O2 (50–200 μM) should be used to explore the effect of gliclazide on early apoptotic changes [15, 19]. Table 2 presents, that pre-treatment of all type of cells with NAC (3 mM) or gliclazide (5–50 μM) followed by H2O2 (50 μM) treatment improved cell viability by about 100%. Gliclazide used in the entire range of concentrations increased viability after exposure to hydrogen peroxide (200 μM) to 90% regardless of the type of cell line.
Table 1.
Cytotoxicity of H2O2 in HUVEC-c, Hs578T and PANC-1 cell lines
| IC50 [μM] values determined by the MTT test | |||
|---|---|---|---|
| Cell line | 24 h | 48 h | 72 h |
| HUVEC-c | 885.11 ± 0.011* | 467.73 ± 0.016* | 343.55 ± 0.012* |
| Hs578T | 641.21 ± 0.009* | 523.60 ± 0.019* | 433.51 ± 0.013* |
| PANC-1 | 1086.42 ± 0.014* | 770. 90 ± 0. 022* | 481.95 ± 0.021* |
The values are the mean ± SD of 3–4 independent experiments
*P < 0.005
Fig. 1.
Number of viable HUVEC-c, Hs578T and PANC-1 cells, The cells were treated with H2O2 (50–600 μM) for 24, 48 and 72 h, At the end of treatment period MTT was added and cells were incubated for an additional 3 h. Formazan crystals were dissolved in DMSO and absorbance at 570 nm was measured with a microplate reader. Data are the mean ± SD of 3–4 independent experiments. *P < 0.05 significant differences between drugs treated and untreated, control cells (taken as 100%)
Table 2.
Number of viable HUVEC-c, Hs578T and PANC-1 cells
| Treatment time (h) | Agent | Cell line (% of viable cells) | ||
|---|---|---|---|---|
| HUVEC-c | H578T | PANC-1 | ||
| 24 | H2O2 [50μM] | 91.48 ± 2.953 | 94.65 ± 5.96 | 98.43 ± 4.52 |
| NAC [3 mM] | 99.78 ± 4.67 | 100.01 ± 5.65 | 98.58 ± 5.45 | |
| 5 | 99.71 ± 5.30 | 102.57 ± 1.10 | 99.50 ± 3.00 | |
| 25 gliclazide [μM] | 99.53 ± 8.76 | 99.32 ± 5.31 | 100.34 ± 2.35 | |
| 50 | 99.54 ± 5.35 | 101.43 ± 4.12 | 99.03 ± 4.20 | |
| H2O2 [100 μM] | 86.50 ± 4.245 | 88.87 ± 3.12 | 92.54 ± 7.04 | |
| NAC [3 mM] | 102.36 ± 5.36 | 99.87 ± 5.26 | 102.65 ± 5.87 | |
| 5 | 97.36 ± 4.18 | 97.53 ± 4.90 | 95.62 ± 4.72 | |
| 25 gliclazide [μM] | 97.23 ± 2.04 | 98.67 ± 7.71 | 94.99 ± 5.99 | |
| 50 | 95.16 ± 5.52 | 98.92 ± 5.00 | 93.78 ± 5.39 | |
| H2O2 [200 μM] | 89.08 ± 6.59 | 76.54 ± 8.09* | 83.65 ± 2.45 | |
| NAC [3 mM] | 102.54 ± 4.65 | 97.36 ± 4.56# | 97.45 ± 5.12 | |
| 5 | 94.87 ± 3.63 | 95.43 ± 5.24# | 94.89 ± 5.78 | |
| 25 gliclazide [μM] | 93.39 ± 4.07 | 96.56 ± 2.87# | 93.77 ± 2.61 | |
| 50 | 95.01 ± 4.36 | 95.62 ± 9.31# | 90.78 ± 4 88 | |
| 48 | H2O2 [50 μM] | 90.10 ± 4.87 | 90.43 ± 4.56 | 96.32 ± 5.56 |
| NAC [3 mM] | 101.27 ± 2.93 | 100.33 ± 3.87 | 100.11 ± 4.57 | |
| 5 | 99.27 ± 4.32 | 99.87 ± 3.43 | 100.11 ± 4.32 | |
| 25 gliclazide [μM] | 97.21 ± 6.87 | 98.43 ± 4.56 | 99.21 ± 5.37 | |
| 50 | 98.12 ± 2.33 | 101.01 ± 6.71 | 101.33 ± 6.71 | |
| H2O2 [100 μM] | 83.45 ± 4.89* | 85.32 ± 7.43 | 87.43 ± 4.87 | |
| NAC [3 mM] | 98.25 ± 6.32# | 97.19 ± 4.52 | 96.12 ± 3.33 | |
| 5 | 97.12 ± 1.67# | 102.34 ± 4.56 | 95.27 ± 4.34 | |
| 25 gliclazide [μM] | 98.11 ± 2.43# | 99.99 ± 4.39# | 96.28 ± 3.28 | |
| 50 | 96.23 ± 3.78# | 97.43 ± 2.67# | 94.33 ± 6.72 | |
| H2O2 [200 μM] | 82.89 ± 1.65 | 72.15 ± 2.45* | 80.32 ± 7.45* | |
| NAC [3 mM] | 97.34 ± 3.12# | 98.11 ± 4.18# | 97.11 ± 3.12# | |
| 5 | 93.11 ± 4.57# | 94.43 ± 9.17# | 90.32 ± 2.32# | |
| 25 gliclazide [μM] | 90.12 ± 6.87# | 96.12 ± 6.32# | 90.12 ± 4.371# | |
| 50 | 89.43 ± 4.36# | 94.77 ± 4.87# | 90.18 ± 7.17# | |
| 72 | H2O2 [50 μM] | 87.87 ± 5.01 | 90.42 ± 4.59 | 97.11 ± 1.44 |
| NAC [3 mM] | 98.78 ± 6.89# | 97.89 ± 4.95 | 99.89 ± 3.89 | |
| 5 | 98.34 ± 4.29# | 102.57 ± 0.53# | 99.50 ± 0.79 | |
| 25 gliclazide [μM] | 101.23 ± 2.15# | 99.32 ± 3.63 | 100.34 ± 2.26 | |
| 50 | 99.95 ± 5.14# | 1010.41 ± 1.70 | 99.03 ± 4.92 | |
| H2O2 [100 μM] | 79.64 ± 6.24* | 83.77 ± 6.24 | 85.21 ± 3.89* | |
| NAC [3 mM] | 99.98 ± 9.08# | 100.89 ± 5.89# | 99.98 ± 7.58# | |
| 5 | 88.26 ± 9.48# | 87.55 ± 7.19# | 85.15 ± 3.77# | |
| 25 gliclazide [μM] | 86.38 ± 6.66# | 86.59 ± 7.73 | 84.50 ± 2.73# | |
| 50 | 88.43 ± 5.10# | 87.67 ± 5.52 | 84.93 ± 2.43 | |
| H2O2 [200 μM] | 78.181 ± 1.20* | 68.53 ± 6.77* | 77.87 ± 8.08* | |
| NAC [3 mM] | 98.67 ± 6.98# | 102.67 ± 8.43# | 99.78 ± 4.76# | |
| 5 | 94.32 ± 4.52# | 93.32 ± 5.55# | 90.62 ± 0.79# | |
| 25 gliclazide [μM] | 90.43 ± 6.25# | 95.43 ± 3.79# | 90.99 ± 2.26# | |
| 50 | 88.32 ± 3.54# | 90.32 ± 6.15* | 89.13 ± 4.92# | |
The cells were preincubated with 5–50 μM gliclazide for 1 h at 37°C. Then the cells were treated with 50, 100 or 200 μM H2O2 for 24, 48 or, 72 h. At the end of treatment period MTT was added and cells were then incubated for an additional 3 h. Formazan crystals were dissolved in DMSO and absorbance at 570 nm was measured with a microplate reader. Data are the mean ± SD of 3–4 independent experiments. *P < 0.05 in comparison to respective control cells taken as 100%. # P < 0.05 indicates significant differences between H2O2-treated cells and samples preincubated with NAC or gliclazide
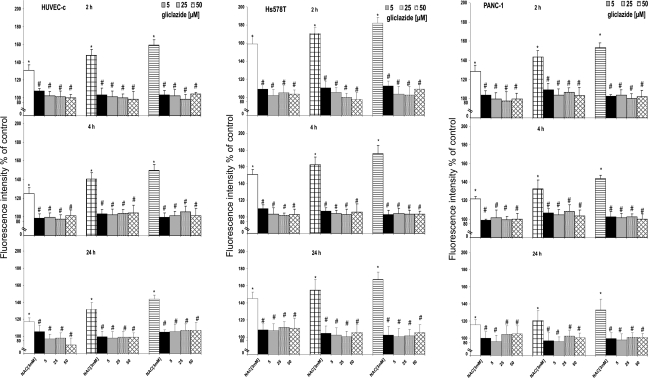
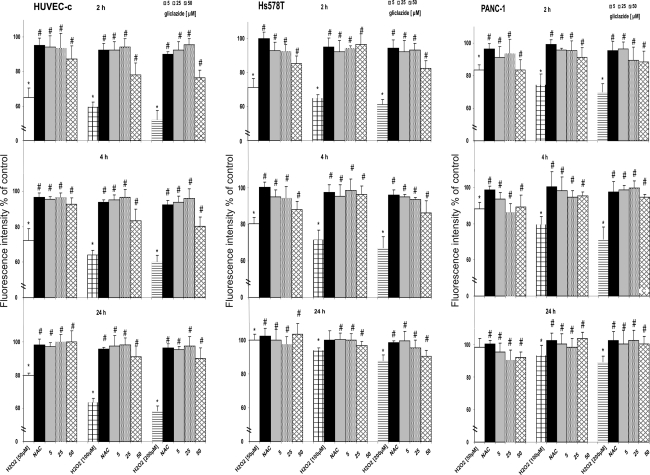
ROS detection
The generation of ROS was measured using the DCFH2-DA dye. It is well documented that long-term incubation with H2O2 (up to 72 h) may result in additional generation of ROS due to its reaction with transient metals present in medium (via Fenton reaction) and release of cytochrome c which catalyzes DCFH2-DA oxidation [24]. Thus, in order to determine ROS generation exclusively for H2O2 we decided to measure the level of ROS at 2, 4 and 24 h. Changes in ROS level after H2O2 treatment are shown in Fig. 2. In all three cell lines, a gradual increase of DCF fluorescence with the increasing concentrations of H2O2 was observed at 2, 4 and 24 h after the treatment. The kinetics of ROS formation, in relation to time of incubation was dependent on the H2O2 concentration and the type of cell line. At 24 h of incubation with H2O2 (200 μM), the level of ROS in Hs578T and HUVEC-c cells increased 143 and 167%, respectively (P ≤ 0.05). Generation of ROS did not correlate with the sensitivity of cells to hydrogen peroxide. The level of ROS in PANC-1 cells was similar to HUVEC-c cells and did not exceed 139% (P ≤ 0.05). To confirm whether ROS are the mediator for H2O2 induced apoptosis, the cells were treated with antioxidants. The amounts of ROS were markedly reduced by NAC and gliclazide. Our results showed that H2O2 increased the level of ROS in time-dependent manner both in normal and cancer cells, and pretreatment with NAC or gliclazide efficiently protected these cells against ROS generation. These results confirm an antioxidant property of gliclazide.
Fig. 2.
Induction of ROS by H2O2 in HUVEC-c, Hs578T and PANC-1 cells in the presence and absence of NAC or gliclazide. The cells (104), seeded into 96-well microplates 24 h before the experiment were treated with different H2O2 concentrations for 2, 4 or 24 h. Oxidation of 5 μM DCFH2-DA fluorescence probe was used for monitoring the produced ROS after drug treatment. In experiments with NAC or gliclazide, cells were preincubated with 3 mM NAC or 5–50 μM gliclazide for 1 h, then H2O2 was added and incubation was continued for another 2, 4 or 24 h, The results represent mean ± SD of four independent experiments, *P < 0.05 in comparison to respective control cells taken as 100%. # P < 0.05 indicates significant differences between H2O2-treated cells and samples preincubated with NAC or gliclazide
Mitochondrial membrane potential (ΔΨm)
In this study, normal HUVEC-c and cancer cells: Hs578T and PANC-1 were stained with a fluorogenic probe JC-1 to detect changes of their mitochondrial membrane potential after the treatment with H2O2. JC-1 has the unique property of forming red fluorescent aggregates locally and spontaneously under high mitochondrial potential, whereas the monomeric form, prevalent in cells with low ΔΨm, fluorescens in green. Thus, the changes of the ratio of red/green fluorescence reflect the variation of ΔΨm. ROS are responsible for dissipation of mitochondrial potential thus, it is reasonable to measure mitochondrial membrane potential at the same time points as determination of the level of ROS. Images of staining with a fluorogenic probe JC-1 tested cell lines at 4 h after treatment with 200 μM of H2O2 in the presence or absence of antioxidants are presented in Fig. 3.
Fig. 3.
Fluorescent microscopy images of a HUVEC-c, b Hs578T and c PANC-1 cell lines at 4 h after 200 μM of H2O2 treatment without or in the presence of NAC or gliclazide. In the experiments with the antioxidants the cells were preincubated with 25 μM gliclazide or 3 mM NAC for 1 h, then H2O2 was added and incubation was continued for the next 4 h, mitochondria depolarization is indicated by a decrease in the red to green fluorescence intensity ratio, green fluorescence of JC-1 monomers is present in the cells areas with high mitochondrial membrane potential, while yellow-orange fluorescence of JC- dimers is prevalent in the cell areas with low mitochondrial membrane potential. The JC-1 stained cells were visualized under an inverted fluorescence microscope (Olympus IX70, Japan), 400× magnification. (Color figure online)
Figure 4 shows the accumulation of JC-1 within the active mitochondria of the investigated cells after exposure to H2O2. Treatment of cells with increasing concentrations of H2O2 (50–200 μM) caused the collapse of ΔΨm, as detected by the reduction of JC-1 dimer to monomer fluorescence ratio. Changes in ΔΨm were dependent on both H2O2 concentration and the length of incubation. The highest changes were observed at 2 h of H2O2 treatment. A 200 μM concentration of H2O2 induced a drop in mitochondrial membrane potential in HUVEC-c, Hs578T and PANC-1 cells by 51%, 61 and 69% respectively (Fig. 4) (P ≤ 0.05). The prolonged incubation (4–24 h) with the H2O2 led to an increase of mitochondrial membrane potential. The enhancement of ΔΨm to a level of control was observed at 24 h in all cell lines. NAC and gliclazide pre-treatment effectively inhibited H2O2 -induced loss of ΔΨm in all cell lines. Our results suggest that antioxidant action of gliclazide in therapeutic concentrations (5–25 μM) was comparable to NAC. Interestingly, it was observed that higher concentrations of gliclazide evoked greater increase in mitochondrial membrane potential level in cancer cells than in normal human endothelial cells.
Fig. 4.
Changes in mitochondrial membrane potential (ΔΨm) of HUVEC-c, Hs578T and PANC-1 cells seeded into black 96-well titration microplates in the presence and absence of antioxidant-NAC or gliclazide, The cells were treated with different H2O2 concentrations for 2, 4 or 24 h. In experiments with antioxidant or gliclazide, cells were preincubated with 3 mM NAC or 5–50 μM gliclazide for 1 h, then H2O2 was added and incubation was continued for another 2, 4 or 24 h. ΔΨm was estimated with a fluorescence dye JC-1 at the end of incubation directly in the cell monolayers. Fluorescence ratio of JC-1 dimers/JC-1 monomers of control was assumed as 100%, The results represent mean ± SD of four independent experiments. *P < 0.05 in comparison to respective control cells taken as 100%. # P < 0.05 indicates significant differences between H2O2-treated cells and samples preincubated with NAC or gliclazide
As a positive control, prior to JC-1 labeling, cells were preincubated with CCCP, a protonophoric uncoupler of oxidative phosphorylation, for the same period of time as that used for H2O2 treatment. The results are presented in Fig. 5. After 2 h incubation, 10 μM CCCP caused loss of mitochondrial membrane potential in HUVEC-c, Hs578T, and PANC-1 cells up to 38, 31, and 49% respectively (P ≤ 0.05). We observed increase in ΔΨm at 4 h of incubation with 10 μM CCCP: 49% for HUVEC-c, 47% for Hs578T, and 58% for PANC-1 (P ≤ 0.05). In the longest time of incubation (24 h) with the 10 μM CCCP a gradual increase in ΔΨm was reported [60% for HUVEC-c, 71% for Hs578T, and 68% for PANC-1 (P ≤ 0.05)].
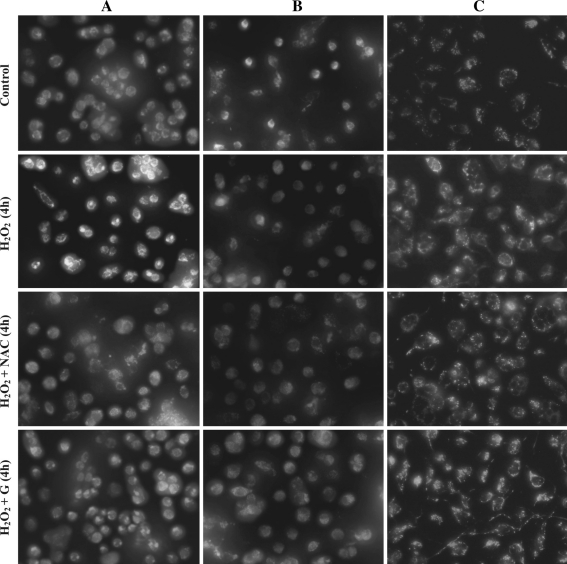
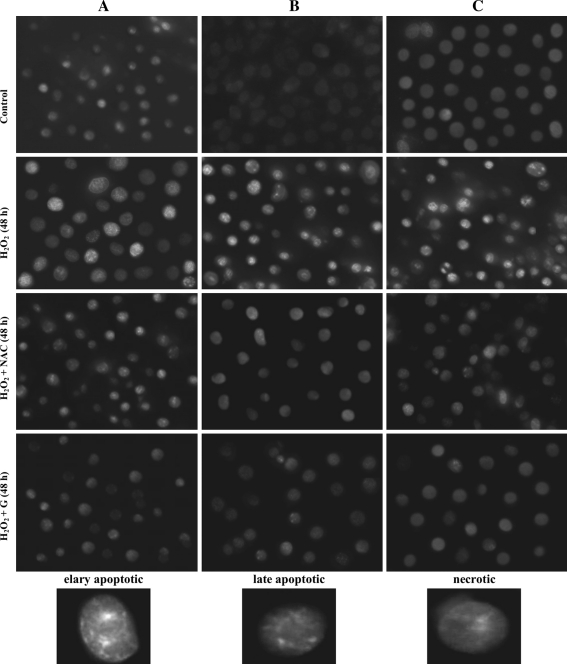
Morphological changes in H2O2 treated cell lines
The ability of H2O2 to induce apoptosis or necrosis was evaluated by treating the cells of each cell line with a concentration of 200 μM for 24, 48 or 72 h. Analysis was performed immediately after H2O2 treatment. To assess the effect of H2O2 at the single cell level directly, we used fluorescence microscopy for examination of cells stained simultaneously with the membrane permeating and intercalating dye bisbenzimide Hoechst 33258 and propidium iodide. Changes in cell morphology, typical either of apoptosis or necrosis are presented in Fig. 6. Alterations in the structure, size and shape of the cell nucleus were detected 24, 48 and 72 h after the treatment with H2O2. The maximal increase in the amount of apoptotic cells was noted at 48 h of H2O2 treatment. After the prolonged incubation time (72 h) we observed chromatin condensation, cell shrinkage and nuclear fragmentation as well as a formation of apoptotic bodies. We reported that H2O2 could induce both apoptosis and necrosis in the investigated cancer and normal cell lines. The number of apoptotic and necrotic cells were dependent on the time of incubation with H2O2 and the type of cell line. The considerable higher increase in the amount of necrotic cells was noted at 72 h after treatment of all tested cell lines with H2O2 (data not shown). The largest apoptotic changes were observed in HUVEC-c cell line. Pre-treatment of tested cells with the antioxidants, NAC or gliclazide partially reduced both apoptotic and necrotic cell population. It seems that gliclazide exhibit a similar protection compared to NAC in relation to normal as well as cancer cells treated with H2O2.
Fig. 6.
Morphological changes of a HUVEC-c, b Hs578T and c PANC-1 cell lines at 48 h after 200 μM of H2O2 treatment without or in the presence of antioxidants. The cells were stained with the PI and the DNA specific dye Hoechst 33258. In the experiments with the antioxidants the cells were preincubated with 25 μM gliclazide or 3 mM NAC for 1 h, then H2O2 was added and incubation was continued for the next 48 h. The cells were analyzed under an inverted fluorescence microscope (Olympus IX70, Japan) under magnification 400×. (Color figure online)
Intracellular calcium ion concentration
To examine whether the intracellular calcium changes were involved in apoptosis induced by H2O2, we studied the level of calcium using the fluorescence probe Fluo- 4-NW. Our results indicate that calcium level also depends on H2O2 concentration, the time of incubation and the type of cells. Table 3 shows that in the tested cells H2O2 induced a significant increase in the intracellular free calcium no sooner than at 48 h of incubation. At this time point, the level of intracellular calcium in the HUVEC-c, Hs578T and PANC-1 cells, treated with 200 μM H2O2 increased by about 60, 36 and 20%, respectively (P ≤ 0.005). After 72 h incubation of the cells with H2O2 the level of calcium decreased in normal and cancer cells. The largest decrease in calcium content was noted in HUVEC-c cell line (about 37%) (P ≤ 0.005) and the lowest in PANC-1 cells (about 14%) (P ≤ 0.005) compared to the values at 48 h after the treatment. Free radical scavengers, NAC and gliclazide, significantly reduced H2O2-induced changes in calcium level at 48 h of incubation in all types of cells. At 72 h, NAC and gliclazide markedly diminished H2O2-induced (100, 200 μM) changes in calcium level in normal cells (P ≤ 0.05). Only in Hs578T cells changes in calcium level induced by 200 μM H2O2 after 72 h of incubation were markedly diminished by gliclazide.
Table 3.
Effect of H2O2 on intracellular level of Ca2+ in HUVEC-c, Hs578T and PANC-1 cells
| Treatment time (h) | Agent | Cell line (% of viable cells) | ||
|---|---|---|---|---|
| HUVEC-c | HS578T | PANC-1 | ||
| 4 | H2O2 [50 μM] | 102.22 ± 2.39 | 106.16 ± 12.36 | 102.36 ± 13.69 |
| NAC [3 mM] | 94.26 ± 1.80 | 98.30 ± 4.58 | 98.36 ± 5.68 | |
| 5 | 99.06 ± 0.01 | 95.61 ± 13.3# | 97.12 ± 3.69 | |
| 25 gliclazide [μM] | 92.12 ± 0.01 | 100.98 ± 1.25 | 94.26 ± 6.36 | |
| 50 | 104.18 ± 2.70 | 97.37 ± 1.69 | 93.45 ± 4.52 | |
| H2O2 [100 μM] | 102.07 ± 3.58 | 99.22 ± 2.58 | 101.36 ± 3.35 | |
| NAC [3 mM] | 91.20 ± 1.36 | 92.93 ± 4.69 | 102.36 ± 1.23 | |
| 5 | 107.72 ± 5.12 | 87.19 ± 1.2S | 96.36 ± 3.69 | |
| 25 gliclazide [μM] | 103.19 ± 0.04 | 94.78 ± 4.58 | 99.26 ± 3.36 | |
| 50 | 104.65 ± 5.54 | 91.91 ± 3.69 | 93.65 ± 1.58 | |
| H2O2 [200 μM] | 98.44 ± 4.12 | 98.00 ± 2.58 | 103.24 ± 1.58 | |
| NAC [3 mM] | 103.27 ± 3.25 | 96.54 ± 5.59 | 102.53 ± 3.69 | |
| 5 | 105.93 ± 2.00 | 90.89 ± 3.69 | 100.36 ± 2.58 | |
| 25 gliclazide [μM] | 100.67 ± 4.04 | 87.00 ± 4.69 | 96.36 ± 2.98 | |
| 50 | 100.93 ± 1.04 | 93.11 ± 6.54 | 97.89 ± 5.45 | |
| 24 | H2O2 [50 μM] | 94.79 ± 1.25 | 85.11 ± 2.45 | 92.36 ± 1.23 |
| NAC [3 mM] | 98.35 ± 2.36 | 90.13 ± 1.22 | 98.12 ± 2.36 | |
| 5 | 92.12 ± 0.01 | 103.02 ± 372 | 101.32 ± 4.39 | |
| 25 gliclazide [μM] | 100.98 ± 2.6 | 103.70 ± 2.48 | 100.31 ± 1.58 | |
| 50 | 100.59 ± 3.42 | 98.26 ± 1.54 | 100.01 ± 6.67 | |
| H2O2 [100 μM] | 95.24 ± 2.36 | 90.85 ± 2.43 | 102.53 ± 1.36 | |
| NAC [3 mM] | 104.78 ± 1.25 | 93.98 ± 1.42 | 103.21 ± 2.25 | |
| 5 | 96.59 ± 0.03 | 109.41 ± 0.82 | 99.87 ± 6.65 | |
| 25 gliclazide [μM] | 106.77 ± 6.56 | 106.11 ± 1.37 | 101.3 ± 6.64 | |
| 50 | 104.04 ± 7.37 | 92.60 ± 1.3 | 103.65 ± 2.64 | |
| H2O2 [200 μM] | 98.21 ± 2.36 | 91.73 ± 1.33 | 101.23 ± 1.36 | |
| NAC [3 mM] | 106.77 ± 1.36 | 94.54 ± 2.34 | 99.87 ± 554 | |
| 5 | 96.78 ± 5.23 | 100.32 ± 1.51 | 102.36 ± 6.36 | |
| 25 gliclazide [μM] | 102.52 ± 7.43 | 102.10 ± 0.77 | 100.32 ± 1.36 | |
| 50 | 106.30 ± 4.21 | 112.51 ± 1.48 | 100.02 ± 5.23 | |
| 48 | H2O2 [50 μM] | 122.65 ± 2.36* | 110.23 ± 1.36 | 108.23 ± 2.36 |
| NAC [3 mM] | 107.91 ± 2.54# | 96.26 ± 2.58# | 102.32 ± 5.54 | |
| 5 | 100.27 ± 4.58# | 101.13 ± 3.65 | 99.36 ± 6.32 | |
| 25 gliclazide [μM] | 100.41 ± 4.96# | 104.81 ± 3.05 | 98.36 ± 6.14 | |
| 50 | 102.68 ± 5.63# | 104.81 ± 5.28 | 95.3 ± 1.25 | |
| H2O2 [100 μM] | 139.67 ± 6.54* | 125.48 ± 3.69* | 113.25 ± 5.87* | |
| NAC [3 mM] | 106.3S ± 7.41# | 97.24 ± 5.40# | 98.36 ± 7.87# | |
| 5 | 100.98 ± 2.65# | 98.45 ± 6.36# | 97.54 ± 5.69# | |
| 25 gliclazide [μM] | 100 86 ± 6.32# | 99.12 ± 3.36# | 94.15 ± 4.12# | |
| 50 | 95.37 ± 4.12# | 92.41 ± 1.25# | 93.65 ± 6.48# | |
| H2O2 [200 μM] | 159.57 ± 1.23* | 135.56 ± 1.25* | 120.36 ± 12.54* | |
| NAC [3 mM] | 101.15 ± 6.54# | 100.10 ± 2.23# | 102.53 ± 4.38# | |
| 5 | 112.52 ± 6.32# | 91.00 ± 12.57# | 102.36 ± 8.58# | |
| 25 gliclazide [μM] | 103.95 ± 4.52# | 94.64 ± 6.32# | 98.26 ± 6.36# | |
| 50 | 111.49 ± 4.23# | 92.88 ± 6.54# | 98.64 ± 554# | |
| 72 | H2O2 [50 μM] | 108.68 ± 2.36 | 104.36 ± 1.23 | 103.36 ± 3.65 |
| NAC [3 mM] | 95.39 ± 1.54 | 102.92 ± 3.36 | 102.53 ± 4.21 | |
| 5 | 10553 ± 6.36 | 92.31 ± 3.65 | 98.65 ± 5.36 | |
| 25 gliclazide [μM] | 103.15 ± 4.23 | 97.15 ± 1.25 | 96.32 ± 4.65 | |
| 50 | 102.26 ± 6.36 | 104.29 ± 3.164 | 92.36 ± 6.32 | |
| H2O2 [100 μM] | 113.32 ± 1.54* | 97.91 ± 3.65 | 105.36 ± 8.12 | |
| NAC [3 mM] | 100.32 ± 16.36# | 102.56 ± 5.14 | 98.26 ± 6.54 | |
| 5 | 98.261 ± 4.58# | 104.94 ± 4.87 | 96.54 ± 7.26 | |
| 25 gliclazide [μM] | 97.50 ± 6.32# | 100.42 ± 5.87 | 93.25 ± 5.21 | |
| 50 | 95.65 ± 1.25# | 101.73 ± 4.56 | 91.25 ± 1.36 | |
| H2O2 [200 μM] | 123.53 ± 1.36* | 111.23 ± 2.36* | 106.32 ± 2.54 | |
| NAC [3 mM] | 105.32 ± 2.64# | 110.87 ± 3.65 | 102.51 ± 4.65 | |
| 5 | 102.26 ± 4.65# | 97.73 ± 4.58# | 99.36 ± 6.58 | |
| 25 gliclazide [μM] | 105.50 ± 3.60# | 86.39 ± 9.65# | 95.36 ± 2.65 | |
| 50 | 101.67 ± 5.45# | 95.43 ± 4.58# | 97.12 ± 6.32 | |
The cells were treated with different H2O2 concentrations for 4, 24, 48 or 72 h. In experiments with antioxidant or gliclazide, cells were preincubated with 3 mM NAC or 5–50 μM gliclazide for 1 h, then H2O2 was added and incubation was continued for another 4, 24, 48 or 72 h. The results represent mean ± SD of four independent experiments. *P < 0.05 in comparison to respective control cells taken as 100%, # P < 0.05 indicates significant differences between H2O2-treated cells and samples preincubated with NAC or gliclazide
In summary, H2O2 caused a significant increase in intracellular calcium levels after 48 h. Moreover, at the same time the greatest apoptotic changes were observed (Fig. 6). The ROS generation was observed already at 2 h of H2O2 incubation. Our results indicate that ROS evoked increased level of calcium. Pre-incubation with antioxidants: NAC and gliclazide effectively decreased H2O2 -induced ROS enhancement and diminished an increase of cytoplasmic free calcium in all cell lines.
Discussion
It is well known that T2DM generally progresses over time and majority of diabetics previously well-metabolically controlled with sulfonylureas may require insulin replacement therapy. It has been suggested that exhaustion or desensitization of pancreatic β-cells by prolonged exposure to sulphonylureas and possibly acceleration of oxidative stress and apoptosis are major causes of secondary failure to these oral hypoglycemic medications. The association of glibenclamide with increased β-cell apoptosis in human islets has been demonstrated in vitro by Meadler et al. [25]. Clinical studies indicate that early insulin treatment in newly diagnosed T2DM patients preserved β-cell secretory function more effectively than glibenclamide [26]. Interestingly, a retrospective analysis performed by Satoh et al. found that patients treated with gliclazide required exogenous insulin support less frequently, than those treated with glibenclamide. These observations suggest that gliclazide but not glibenclamide may protect β-cells and thereby delay development of a secondary failure [27]. It is worth mentioning that gliclazide may protect against oxidative stress-related diabetic complications since a significantly lower mortality for cardiovascular diseases and malignancies was suggested in patients treated with gliclazide compared to other hypoglycaemic drugs, especially sulphonylureas [28–30].
There are several mechanisms that may be responsible for β -cell mass loss and dysfunction associated with sulfonylureas use in diabetics. ROS overproduction and disequilibrium of Ca2+ homeostasis induced by sulfonylureas seem to be involved in these processes. It was demonstrated that glibenclamide, glimepiride and nateglinide stimulate ROS production in the pancreatic β-cell line MIN6 within the therapeutic concentration range in plasma of treated patients [12, 31]. Sawada et al. have found that these compounds-related ROS production was mediated by a PKC-dependent activation of NAD(P)H oxidase [12]. The secreatgogues raise the intracellular Ca2+ concentration by opening of voltage-operated Ca2+ channels and increasing Ca2+ influx [32]. Since Ca2+ plays an important role in cell survival regulation, the significant increase in the intracellular Ca2+ concentration induced by glibenclamide or tolbutamide may initiate Ca2+ dependent β-cell apoptosis [33, 34].
In our experiments, we used H2O2 which by generation of ROS increases an oxidative stress insult that may cause cells death [35]. Number of evidence indicates that H2O2/ROS activate K+ATP channels and hyperpolarize the plasma membrane potential. It has been reported that an oxidative stress potentates the amount of ROS by stimulating mitochondrial ROS production. ROS are also able to trigger the opening of the mitochondrial permeability transition pore to an extent, that collapses the mitochondrial membrane potential and leads to ATP depletion [15, 36, 37]. Moreover, a reduction in the mitochondrial membrane potential (ΔΨm) results in the release of mitochondrial Ca2+ and a rise in cytosolic [Ca2+] and may also contribute to cell death [38, 39].
As we expected, H2O2 induced apoptosis in human normal and cancer cells since the cytotoxic effects of this molecule is well known [40]. The results of our study indicate that gliclazide reduced the number of H2O2 -related necrotic and apoptotic cells. These findings are consistent with the earlier reports showing, that gliclazide attenuated apoptotic β-cell as well as endothelial cells death induced by an oxidative stress. As was suggested by others, we believe that this effect is most likely caused by free radical scavenging properties of gliclazide [15–18]. It is worth underlying that these unique activities of the drug are not shared by other sulphonylureas [20, 41]. Recently, it has been reported that glibenclamide and glimepiride, but not gliclazide, significantly increased ROS production in β-cell [12]. It is suggested that several mechanisms may be responsible for these differences. Firstly, gliclazide possesses free radical scavenging activity. Secondly, the binding of gliclazide to SUR1 receptor is rapidly reversible in contrary to other sulphonylureas [10, 42]. Finally, Gier et al. have found that gliclazide may up-regulate the expression of antioxidant enzymes (superoxide dismutase, glutathione peroxidase, catalase). Their experiments demonstrated that enzyme activity changes in pancreatic β-cells were dependent on [Ca2+] mediated via KATP channels [15]. Interestingly, the results of our study may at least partially support these findings because we showed that gliclazide decreased the intracellular [Ca2+] in tested cell lines exposed to H2O2.
Mitochondria are major intracellular source of reactive oxygen species and play an important role in apoptotic form of cell death [43]. As was mentioned earlier, ROS/H2O2 cause depolarization of mitochondria and local Ca2+ release, what leads to loss of ∆Ψm, opening of mitochondrial permeability transition pore, damage to cell and finally cell death [39, 44]. This effect of H2O2 was confirmed in our experiments. We observed significant loss of ∆Ψm in all kind of cells as early as after 2 h of exposure to H2O2. Furthermore, we have observed an increase in the intracellular free [Ca2+] in H2O2-treated human normal and cancer cell lines at 48 h of incubation. The accumulation of fluorescent dye JC-1 in mitochondria as a consequence of changes in ∆Ψm after treatment with H2O2 was also noted. These findings are in agreement with previous observations [36, 44, 45]. Nakazaki et al. found, that in rat pancreatic β-cells H2O2 led to an increase in intracellular [Ca2+] due to its release from cytosolic stores and increase in Ca2+ influx across the plasma membrane (through L-type Ca2+ channels) [36]. Gonzalez et al. reported that H2O2 caused loss of ∆Ψm and an increase in intracellular [Ca2+] in isolated mouse pancreatic acinar cells [46]. The results of our experiments showed that pre-treatment with gliclazide effectively inhibits H2O2-induced loss of mitochondrial membrane potential and significantly decreases the level of intracellular [Ca2+] in tested cell lines.
Recently, it was reported that the oxidative stress and Ca2+ homeostasis are associated with endoplasmic reticulum stress (ER stress) [47]. Marchetti et al. found that both ER stress and oxidative stress may play a prominent role in β-cell apoptosis evoked by high glucose concentration in islets isolated from diabetic patients [48]. Since we noted, that gliclazide decreased the intracellular [Ca2+] in H2O2-treated cell lines, it cannot be excluded, that the drug may protect from apoptosis not only via decreasing the level of oxidative stress, but also the level of ER stress.
In summary, the results of our work provide an additional evidence that gliclazide may diminish oxidative stress-related cell damage and death. Gliclazide decreases ROS production, elevates ∆Ψm and diminishes intracellular [Ca2+] in human normal and cancer cells exposed to H2O2. However, further studies are needed to explore whether the same effect occurs in T2DM patients treated with this drug.
Acknowledgments
This work was supported by the grant from the Polish Society of Metabolic Disease and by the grants 503-0077-9 and 502-04-007 from Medical University of Lodz.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab. 2008;10(Suppl 4):32–42. doi: 10.1111/j.1463-1326.2008.00969.x. [DOI] [PubMed] [Google Scholar]
- 2.Prentki M, Nolan CJ. Islet beta cell failure in type 2 diabetes. J Clin Invest. 2006;116:1802–1812. doi: 10.1172/JCI29103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donath MY, Böni-Schnetzler M, Ellingsgaard H, Ehses JA. Islet inflammation impairs the pancreatic beta-cell in type 2 diabetes. Physiology (Bethesda) 2009;24:325–331. doi: 10.1152/physiol.00032.2009. [DOI] [PubMed] [Google Scholar]
- 4.Robertson RP, Harmon J, Tran PO, Poitout V. Beta-cell glucose toxicity, lipotoxicity, and chronic oxidative stress in type 2 diabetes. Diabetes. 2004;53(Suppl 1):S119–S124. doi: 10.2337/diabetes.53.2007.S119. [DOI] [PubMed] [Google Scholar]
- 5.Evans JL, Goldfine ID, Maddux BA, Grodsky GM. Oxidative stress and stress-activated signaling pathways: a unifying hypothesis of type 2 diabetes. Endocr Rev. 2002;23:599–622. doi: 10.1210/er.2001-0039. [DOI] [PubMed] [Google Scholar]
- 6.Robertson RP, Harmon J, Tran PO, Tanaka Y, Takahashi H. Glucose toxicity in β-cells: type 2 diabetes, good radicals gone bad, and the glutathione connection. Diabetes. 2003;52:581–587. doi: 10.2337/diabetes.52.3.581. [DOI] [PubMed] [Google Scholar]
- 7.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 8.Rustenbeck I, Baltrusch S, Tiedge M. Do insulinotropic glucose–lewering drugs do more harm than good? The hypersecretion hypothesis revisited. Diabetologia. 2010;53:2105–2111. doi: 10.1007/s00125-010-1839-0. [DOI] [PubMed] [Google Scholar]
- 9.Krentz AJ, Bailey CJ. Oral antidiabetic agents: current role in type 2 diabetes mellitus. Drugs. 2005;65:385–411. doi: 10.2165/00003495-200565030-00005. [DOI] [PubMed] [Google Scholar]
- 10.Jennings PE. Vascular benefits of gliclazide beyond glycemic control. Metabolism. 2000;49:17–20. doi: 10.1053/meta.2000.17825. [DOI] [PubMed] [Google Scholar]
- 11.Fava D, Cassone-Faldetta M, Laurenti O, De Luca O, Ghiselli A, De Mattia G. Gliclazide improves anti-oxidant status and nitric oxide-mediated vasodilation in type 2 diabetes. Diabet Med. 2002;19:752–757. doi: 10.1046/j.1464-5491.2002.00762.x. [DOI] [PubMed] [Google Scholar]
- 12.Sawada F, Inoguchi T, Tsubouchi H, et al. Differential effect of sulfonylureas on production of reactive oxygen species and apoptosis in cultured pancreatic beta-cell line, MIN6. Metabolism. 2008;57:1038–1045. doi: 10.1016/j.metabol.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 13.Lortz S, Gurgul-Convey E, Lenzen S, Tiedge M. Importance of mitochondrial superoxide dismutase expression in insulin-producing cells for the toxicity of reactive oxygen species and proinflammatory cytokines. Diabetologia. 2005;48:1541–1548. doi: 10.1007/s00125-005-1822-3. [DOI] [PubMed] [Google Scholar]
- 14.Eizirik DL, Cardozo AK, Cnop M. The role for endoplasmic reticulum stress in diabetes mellitus. Endocr Rev. 2008;29:42–61. doi: 10.1210/er.2007-0015. [DOI] [PubMed] [Google Scholar]
- 15.Gier B, Krippeit-Drews P, Sheiko T, et al. Suppression of KATP channel activity protects murine pancreatic beta cells against oxidative stress. J Clin Invest. 2009;119:3246–3256. doi: 10.1172/JCI38817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li L, Renier G. The oral anti-diabetic agent, gliclazide, inhibits oxidized LDL-mediated LOX-1 expression, metalloproteinase-9 secretion and apoptosis in human aortic endothelial cells. Atherosclerosis. 2009;204:40–46. doi: 10.1016/j.atherosclerosis.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 17.Corgnali M, Piconi L, Ihnat M, Ceriello A. Evaluation of gliclazide ability to attenuate the hyperglycaemic ‘memory’ induced by high glucose in isolated human endothelial cells. Diabetes Metab Res Rev. 2008;24:301–309. doi: 10.1002/dmrr.804. [DOI] [PubMed] [Google Scholar]
- 18.Del Guerra S, Grupillo M, Masini M, et al. Gliclazide protects human islet beta-cells from apoptosis induced by intermittent high glucose. Diabetes Metab Res Rev. 2007;23:234–238. doi: 10.1002/dmrr.680. [DOI] [PubMed] [Google Scholar]
- 19.Kimoto K, Suzuki K, Kizaki T, et al. Gliclazide protects pancreatic beta-cells from damage by hydrogen peroxide. Biochem Biophys Res Commun. 2003;303:112–119. doi: 10.1016/S0006-291X(03)00310-3. [DOI] [PubMed] [Google Scholar]
- 20.Noda Y, Mori A, Cossins E, Packer L. Gliclazide scavenges hydroxyl and superoxide radicals: an electron spin resonance study. Metabolism. 2000;49(2 Suppl 1):14–16. doi: 10.1016/S0026-0495(00)80079-7. [DOI] [PubMed] [Google Scholar]
- 21.Carmichael J, DeGraff WG, Gazdar AF, Minna JD, Mitchell JB. Evaluation of a tetrazolium-based semiautomated colorimetric assay: assessment of radiosensitivity. Cancer Res. 1987;47:943–946. [PubMed] [Google Scholar]
- 22.Nuydens R, Novalbos J, Dispersyn G, Weber C, Borgers M, Geerts H. A rapid method for the evaluation of compounds with mitochondria-protective properties. J Neurosci Meth. 1999;92:153–159. doi: 10.1016/S0165-0270(99)00107-7. [DOI] [PubMed] [Google Scholar]
- 23.Gasiorowski K, Brokos B, Kulma A, Ogorzałek A, Skórkowska K. A comparison of the methods applied to detect apoptosis in genotoxically-damaged lymphocytes cultured in the presence of four antimutagens. Cell Mol Biol Lett. 2001;6:141–159. [PubMed] [Google Scholar]
- 24.Burkitt MJ, Wardman P. Cytochrome C is a potent catalyst of dichlorofluorescin oxidation: implications for the role of reactive oxygen species in apoptosis. Biochem Biophys Res Commun. 2001;282:329–333. doi: 10.1006/bbrc.2001.4578. [DOI] [PubMed] [Google Scholar]
- 25.Maedler K, Carr RD, Bosco D, Zuellig RA, Berney T, Donath MY. Sulfonylurea induced beta-cell apoptosis in cultured human islets. J Clin Endocrinol Metab. 2005;90:501–506. doi: 10.1210/jc.2004-0699. [DOI] [PubMed] [Google Scholar]
- 26.Alvarsson M, Sundkvist G, Lager I, et al. Beneficial effects of insulin versus sulphonylurea on insulin secretion and metabolic control in recently diagnosed type 2 diabetic patients. Diabetes Care. 2003;26:2231–2237. doi: 10.2337/diacare.26.8.2231. [DOI] [PubMed] [Google Scholar]
- 27.Satoh J, Takahashi K, Takizawa Y, et al. Secondary sulfonylurea failure: comparison of period until insulin treatment between diabetic patients treated with gliclazide and glibenclamide. Diabetes Res Clin Pract. 2005;70:291–297. doi: 10.1016/j.diabres.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Monami M, Balzi D, Lamanna C, Barchielli A, Masotti G, Buiatti E, Marchionni N, Manucci E. Are sulphonylureas all the same? A cohort study on cardiovascular and cancer-related mortality. Diabetes Metab Res Rev. 2007;23(2007):479–484. doi: 10.1002/dmrr.736. [DOI] [PubMed] [Google Scholar]
- 29.Monami M, Lamanna C, Balzi D, Marchionni N, Mannucci E. Sulphonylureas and cancer: a case-control study. Acta Diabetol. 2009;46:279–284. doi: 10.1007/s00592-008-0083-2. [DOI] [PubMed] [Google Scholar]
- 30.Horsdal HT, Johnsen SP, Søndergaard F, Jacobsen J, Thomsen RW, Schmitz O, Sørensen HT, Rungby J. Sulfonylureas and prognosis after myocardial infarction in patients with diabetes: a population-based follow-up study. Diabetes Metab Res Rev. 2009;25:515–522. doi: 10.1002/dmrr.971. [DOI] [PubMed] [Google Scholar]
- 31.Tsubouchi H, Inoguchi T, Inuo M, et al. Sulfonylurea as well as elevated glucose levels stimulate reactive oxygen species production in the pancreatic beta-cell line, MIN6-a role of NAD(P)H oxidase in beta-cells. Biochem Biophys Res Commun. 2005;326:60–65. doi: 10.1016/j.bbrc.2004.10.201. [DOI] [PubMed] [Google Scholar]
- 32.Dufer M, Haspel D, Krippeit-Drews P, et al. KATP channel is critical for calcium sequestration into non-ER compartments in mouse pancreatic beta cells. Cell Physiol Biochem. 2007;20:65–74. doi: 10.1159/000104154. [DOI] [PubMed] [Google Scholar]
- 33.Demaurex N, Distelhorst C, Cell biology Apoptosis–the calcium connection. Science. 2003;300:65–67. doi: 10.1126/science.1083628. [DOI] [PubMed] [Google Scholar]
- 34.Iwakura T, Fujimoto S, Kagimoto S, et al. Sustained enhancement of Ca(2+) influx by glibenclamide induces apoptosis in RINm5F cells. Biochem Biophys Res Commun. 2000;271:422–428. doi: 10.1006/bbrc.2000.2616. [DOI] [PubMed] [Google Scholar]
- 35.Cross CE, Halliwell B, Borish ET, et al. Oxygen radicals and human disease. Ann Intern Med. 1987;107:526–545. doi: 10.7326/0003-4819-107-4-526. [DOI] [PubMed] [Google Scholar]
- 36.Nakazaki M, Kakei M, Yaekura K, et al. Diverse effects of hydrogen peroxide on cytosolic Ca2+ homeostasis in rat pancreatic beta-cells. Cell Struct Funct. 2000;25:187–193. doi: 10.1247/csf.25.187. [DOI] [PubMed] [Google Scholar]
- 37.Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial ROS-induced ROS release: an update and review. Biochim Biophys Acta. 2006;1757:509–517. doi: 10.1016/j.bbabio.2006.04.029. [DOI] [PubMed] [Google Scholar]
- 38.Pariente JA, Camello C, Camello PJ, Salido GM. Release of calcium from mitochondrial and nonmitochondrial intracellular stores in mouse pancreatic acinar cells by hydrogen peroxide. J Membr Biol. 2001;179:27–35. doi: 10.1007/s002320010034. [DOI] [PubMed] [Google Scholar]
- 39.Jacobson J, Duchen MR. Mitochondrial oxidative stress and cell death in astrocytes–requirement for stored Ca2+ and sustained opening of the permeability transition pore. J Cell Sci. 2002;115:1175–1188. doi: 10.1242/jcs.115.6.1175. [DOI] [PubMed] [Google Scholar]
- 40.Bae JY, Ahn SJ, Han W, Noh DY. Peroxiredoxin I and II inhibit H2O2-induced cell death in MCF-7 cell lines. J Cell Biochem. 2007;101:1038–1045. doi: 10.1002/jcb.21241. [DOI] [PubMed] [Google Scholar]
- 41.Scott NA, Jennings PE, Brown J, Belch JJ. Gliclazide: a general free radical scavenger. Eur J Pharmacol. 1991;208:175–177. doi: 10.1016/0922-4106(91)90069-T. [DOI] [PubMed] [Google Scholar]
- 42.Gribble FM, Reimann F. Differential selectivity of insulin secretagogues: mechanisms, clinical implications, and drug interactions. J Diabetes Complicat. 2003;17(2 Suppl):11–15. doi: 10.1016/S1056-8727(02)00272-6. [DOI] [PubMed] [Google Scholar]
- 43.Orrenius S. Reactive oxygen species in mitochondria-mediated cell death. Drug Metab Rev. 2007;39:443–455. doi: 10.1080/03602530701468516. [DOI] [PubMed] [Google Scholar]
- 44.Duchen MR. Mitochondria and calcium: from cell signalling to cell death. J Physiol. 2000;1:57–68. doi: 10.1111/j.1469-7793.2000.00057.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Choi SE, Min SH, Shin HC, Kim HE, Jung MW, Kang Y. Involvement of calcium-mediated apoptotic signals in H2O2-induced MIN6N8a cell death. Eur J Pharmacol. 2006;547:1–9. doi: 10.1016/j.ejphar.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 46.González A, Granados MP, Salido GM, Pariente JA. H2O2-induced changes in mitochondrial activity in isolated mouse pancreatic acinar cells. Mol Cell Biochem. 2005;269:165–173. doi: 10.1007/s11010-005-3457-6. [DOI] [PubMed] [Google Scholar]
- 47.Casas S, Novials A, Reimann F, Gomis R, Gribble FM. Calcium elevation in mouse pancreatic beta cells evoked by extracellular human islet amyloid polypeptide involves activation of the mechanosensitive ion channel TRPV4. Diabetologia. 2008;51:2252–2262. doi: 10.1007/s00125-008-1111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marchetti P, Bugliani M, Lupi R, et al. The endoplasmic reticulum in pancreatic beta cells of type 2 diabetes patients. Diabetologia. 2007;50:2486–2494. doi: 10.1007/s00125-007-0816-8. [DOI] [PubMed] [Google Scholar]