Abstract
Few interventions have succeeded in reducing psychosocial risk among pregnant women. The objective of this study was to determine whether an integrated group prenatal care intervention already shown to improve perinatal and sexual risk outcomes can also improve psychosocial outcomes compared to standard individual care. This randomised controlled trial included pregnant women ages 14–25 from two public hospitals (N = 1047) who were randomly assigned to standard individual care, group prenatal care or integrated group prenatal care intervention (CenteringPregnancy Plus, CP+). Timing and content of visits followed obstetrical guidelines, from 18-week gestation through birth. Each 2-h group prenatal care session included physical assessment, education/skills building and support via facilitated discussion. Using intention-to-treat models, there were no significant differences in psychosocial function; yet, women in the top tertile of psychosocial stress at study entry did benefit from integrated group care. High-stress women randomly assigned to CP+ reported significantly increased self-esteem, decreased stress and social conflict in the third trimester of pregnancy; social conflict and depression were significantly lower 1-year postpartum (all p-values <0.02). CP+ improved psychosocial outcomes for high-stress women. This ‘bundled’ intervention has promise for improving psychosocial outcomes, especially for young pregnant women who are traditionally more vulnerable and underserved.
Keywords: pregnancy, randomised controlled trial, intervention, psychosocial, adolescents, group
Introduction
Adolescents and young women may be particularly vulnerable to the psychosocial challenges of pregnancy because of developmental immaturity, low self-esteem and limited resources (Ickovics et al., 2006; Paik, 1987; Streetman, 1987; Ventura, Peters, Martin, & Maurer, 1997). Interventions aimed at decreasing psychosocial risk among adolescents and young women have been limited and have yielded mixed results. Interventions that have documented favourable outcomes with regard to psychosocial function among at-risk young women have generally been intensive and long-term, often utilising public health nurses to intervene during and after pregnancy (Barnet, Liu, DeVoe, Alperovitz-Bichell, & Duggan, 2007; Kitzman et al., 1997; Koniak-Griffin, Anderson, Verzemnieks, & Brecht, 2000; Koniak-Griffin, Lesser, Uman, & Nyamathi, 2003; Koniak-Griffin et al., 2002; Nguyen, Carson, Parris, & Place, 2003; Olds, Henderson, Tatelbaum, & Chamberlin, 1986, 1988; Olds et al., 1998; Vieten & Astin, 2008). For example, in the Nurse Family Partnership Program, those randomised to receive ongoing support provided by nurse home visitors reported greater perceived social support, increased use of formal community services, less drug use among mothers and lower rates of hospitalisations and emergency department visits among infants, compared to those who received standard of care (Olds et al., 1986, 1998). These intensive interventions can result in favourable outcomes, but may have limited practical utility because of high cost and time required to effectively implement them. Unfortunately, short-term psychosocial interventions at the time of delivery generally have not been effective in improving psychosocial function among young mothers. For example, in a study examining a brief psychosocial support intervention provided at the time of delivery, no significant differences in mothers' psychological state were documented (Langer, Campero, Garcia, & Reynoso, 1998; Langer et al., 1996).
The dearth of effective psychosocial interventions developed for pregnant women might be the result of a lower priority being given to psychosocial health compared to physical health outcomes among young women (e.g. perinatal and birth outcomes), particularly in settings with limited or scarce resources. Organisations and funding agencies might be wary to implement stand-alone programmes aimed to improve support, esteem and depression at the expense of programmes aimed to reduce teen pregnancy, pre-term birth or HIV. Therefore, the development of integrated prevention programmes that target multiple outcomes including psychosocial health may be more desirable, cost-effective and feasible to implement.
Bundling of psychosocial health promotion with existing systems and structures can increase the accessibility and effectiveness of these programmes by providing opportunities to reach high-risk persons who may not have the motivation or time to attend stand-alone sessions (Ickovics, 2008). Bundling psychosocial health promotion with prenatal care makes conceptual sense because there are a set number of regular visits providing opportunity for multiple intervention components throughout the course of pregnancy. Furthermore, health promotion messages targeting multiple behaviours (e.g. nutrition, safe sex, breastfeeding) and outcomes (e.g. HIV and STI risk reduction, better birth outcomes, decreased depression) can be delivered in a single context in a cost-effective and sustainable way.
The objective of this study was to examine the psychosocial impact of an innovative intervention (CenteringPregnancy Plus, CP+) designed to reduce negative birth outcomes, decrease sexual risk and improve psychosocial outcomes within a model of group prenatal care. This bundled intervention has already been shown to reduce pre-term birth, improve prenatal care satisfaction, reduce pregnancy-related distress, increase breastfeeding, increase condom use, reduce rapid repeat pregnancies and decrease unprotected sex occasions (Ickovics et al., 2007; Kershaw, Magriples, Westdahl, Rising, & Ickovics, 2009). Specifically, we tested the hypothesis that this integrated intervention will result in increased self-esteem and social support as well as decreased stress, social conflict and depression. Moreover, we examined the effects of the intervention for various subgroups based on younger age, race/ethnicity and initial levels of stress, given that such groups are at greater risk for poor pregnancy-related psychosocial health outcomes (Brown, Chireau, Jallah, & Howard, 2007; Dole et al., 2004; Dominguez, Dunkel-Schetter, Mancuso, Rini, & Hobel, 2005; DuPlessis, Bell, & Richards, 1997; Gold, Dalton, Schwenk, & Hayward, 2007; Lu & Halfon, 2003; Morello-Frosch & Shenassa, 2006; Rosen, Seng, Tolman, & Mallinger, 2007). We hypothesise that the intervention will have an even greater effect for those at highest risk of adverse outcomes: younger age, African Americans and those highest in stress.
Methods
Overview of study design
Young women (ages 14–25, N = 1047) entering prenatal care at two publicly funded clinics were randomly assigned to one of three groups (described in more detail below): (1) standard individual care (IC), (2) CenteringPregnancy (CP) group care or (3) the integrated CP+ group care that includes specific skills-building in the areas of HIV/STD prevention including assertiveness and negotiation skills (Ickovics et al., 2007; Kershaw et al., 2009). The focus of the analyses was to assess whether the integrated group prenatal care intervention (CP+) that has already been demonstrated to be effective in reducing negative birth outcomes and sexual risk, also demonstrates improvements in psychosocial outcomes. Therefore, the primary comparison of interest was a planned contrast between CP+ and standard IC, though comparisons with CP were also conducted in planned analyses.
Recruitment
Participants were recruited from two large university-affiliated public hospital prenatal clinics in New Haven, CT, and Atlanta, GA. There were no differences in any major study variables between the two cities; therefore, they were combined for all analyses (Ickovics et al., 2007). Between September 2001 and December 2004, women attending their first or second prenatal care visit were referred by a provider or approached directly by research staff. Inclusion criteria were: <24 weeks gestation; age ≤25; no medical problems requiring individualised care as ‘high-risk pregnancy’ (e.g. diabetes, HIV); English or Spanish-speaking (CP and CP+ group care were offered in both languages; there were no differences by language). Potential participants were screened; if eligible, research staff explained the study in detail and obtained informed consent. Baseline interviews occurred at an average gestational age of 18 weeks (SD = 3.3).
Randomisation
Participants were randomised using a blocked randomised controlled design, stratified based on site and expected month of delivery with the stated allocation goal of 40% IC, 30% CP group care and 30% CP+. A computer-generated randomisation sequence, password-protected to recruitment staff and participants, was used to randomise participants.
Intervention
CP+ provides group prenatal care in groups of 8–12 women led by a trained prenatal care provider (e.g. midwife, obstetrician). The model provides complete care including three primary components of prenatal care: physical assessment (e.g. measurement of fundal height, baby heart rate monitoring), education/skills building and support. All prenatal care occurs within the group setting except for the initial assessment. The structured curriculum consists of 10 structured sessions (120 min each) during pregnancy. Participants engage in self-care activities of weight and blood pressure assessment and participate in group discussions to address issues related to prenatal care, childbirth preparation, postpartum care, HIV prevention and mental health and psychosocial functioning (e.g. depression, stress reduction). Three sessions (sessions 4, 5 and 7) were devoted to more intensive HIV prevention skills that included activities also designed to improve psychosocial functioning. Components included skill-building in assessing behavioural risks, goal setting and communication and negotiation skills. A strength of group prenatal care is the enhanced quantity of time (20 h), permitting enhanced quality of care – by providing training and a structured curriculum so that healthcare providers have the ability to add important content as well as build on the importance of group social processes to enhance outcomes in a cost-neutral way (Ickovics et al., 2007; Kershaw et al., 2009).
The HIV prevention components of CP+ are adapted from previous efficacious interventions, and are based on social cognitive theory and ecological models (Bronfenbrenner, 1989; Malow, Kershaw, Sipsma, Rosenberg, & Dévieux, 2007; Meade & Ickovics, 2005; Sikkema et al., 2000; See the Appendix in the online repository for illustrations of the intervention content).
We targeted key components of social cognitive theory that could impact psychosocial functioning, modelling these across all levels of the ecological model including individual (e.g. efficacy, perceived risk), dyad (e.g. interpersonal communication) and community (e.g. social norms).
The CP group had the same contact time, promotion of prenatal health behaviours and opportunities for social support. Therefore, it served as an attention-matched control with the only difference being the HIV content and focus on skills-building for sexual risk reduction and its concomitant approach to psychosocial function. Those in the IC group met on the same schedule and the same number of times with their healthcare providers as CP+ and CP; however, the contact time was consistent with traditional prenatal care (i.e. 10–15 min per session).
Further description of the intervention content can be found at www.centeringhealthcare.org; www.pregnancyresearch.org/cpplus and measures and materials are available from the first author.
Data collection
Trained study staff facilitated data collection on laptop computers and reviewed medical records. Structured interviews via audio-CASI (computer-assisted self-interview) were conducted upon study entry, prior to 24-week gestation; for those randomised to group care, this was conducted prior to Session 1 (average gestational age = 18.1 weeks, SD = 3.4). Follow-up interviews were conducted during the third trimester of pregnancy (average gestational age = 35.0 weeks, SD = 3.1); as well as 6 and 12 months postpartum. Audio-CASI, previously validated among pregnant women (C'de Baca, Lapham, Skipper, & Watkins, 1997), allows respondents to simultaneously listen with headphones and see questions on a computer laptop, facilitating completion for participants with lower reading skills. All procedures were approved by the Yale and Emory University Human Investigation Committees. Participants were paid $20 for each interview.
Measures
Stress
The 10-item Perceived Stress Scale (PSS) assessed the degree to which respondents perceived situations in their lives to be unpredictable, uncontrollable and overloaded during the past month, (e.g. ‘How often have you felt: upset by something that happened unexpectedly’) (Cohen, Kamarck, & Mermelstein, 1983; Cohen &Williamson, 1998). Responses ranged from 0 (‘never’) to 4 (‘very often’). Validity and reliability of this measure have been previously documented (Cohen &Williamson, 1998; Cohen et al., 1983). In this study, Chronbach's alpha across all participants/treatment conditions was 0.81.
Self-esteem
This 10-item scale assessed self-reported self-esteem (Rosenberg, 1965). Sample items include ‘In general, I am satisfied with myself’ and ‘I am able to do things as well as most people.’ All responses were on a four-point Likert-type scale (Ickovics et al., 2006; Paik, 1987; Streetman, 1987; Ventura et al., 1997), ranging from ‘strongly disagree’ to ‘strongly agree’. Validity and reliability of this measure have been previously documented (Hagsborg, 1996; Silbert, Mokri, & Schievink, 1995; Visintini et al., 1995). In this study, Chronbach's alpha was 0.85.
Social support
The seven items of the social support subscale of the Social Relationship Scale (O'Brien, Wortman, Kessler, & Joseph, 1993) assessed perceived availability of emotional and material support (e.g. talk about an interpersonal problem, borrow money in a medical emergency or for advice in making a decision). Possible responses were on a five-point Likert-type scale (Barnet et al., 2007; Ickovics et al., 2006; Paik, 1987; Streetman, 1987; Ventura et al., 1997), ranging from ‘definitely not’ to ‘definitely yes’. In this study, Cronbach's alpha was 0.87.
Social conflict
The seven items of the social conflict subscale of the Social Relationship Scale (O'Brien et al., 1993) assessed the perceived degree of social conflict in an individual's everyday social network. The first six items asked participants to rate perceived degree of conflict in interpersonal relationships in the past month (e.g. people getting on your nerves, feeling tense from arguing or disagreeing). Possible responses were on a five-point Likert-type scale (Barnet et al., 2007; Ickovics et al., 2006; Paik, 1987; Streetman, 1987; Ventura et al., 1997), ranging from ‘definitely not’ to ‘definitely yes’. The seventh item asked the participant to indicate how often she had been involved in a social interaction or exchange that was unpleasant or distressing in the past month (ranging from everyday to not at all). In this study, Chronbach's alpha was 0.83.
Depression
The affect-only component of the CES-D is a 15-item self-report scale to assess current depressive symptoms in the general population (Radloff, 1977). Items focus on the affective component of depressed mood (e.g. feelings of failure, guilt, hopelessness). Respondents indicate how often they experienced each of the symptoms in the past week on a four-point scale, ranging from less than 1 day to 5–7 days. In this study, Chronbach's alpha was 0.85.
Demographic and behavioural characteristics
Participants also reported basic social and demographic characteristics (e.g. age, race, ethnicity, education). Questions regarding both health-promoting behaviours (nutrition, physical activity) and health-damaging behaviours (e.g. tobacco, alcohol, illicit drugs) were also asked, and were used as control variables in this study.
Data analysis
Initial analyses were all based on intention-to-treat models with randomised study condition as the primary independent variable: IC, CP and CP+. Chi-squared and analyses of variance were conducted to assess any differences between groups on demographic, medical history and major study variables at baseline (e.g. whether randomisation produced initially equivalent groups).
To assess the effectiveness of the intervention, a series of random effects regression analyses were conducted. These models (also called hierarchical linear regression, mixed regression or multilevel models) offer a powerful tool for evaluating the effectiveness of interventions assessed longitudinally (Raudenbush & Bryk, 2002; Singer & Willett, 2003). Random effects regression analysis offers several advantages over traditional ANOVA models including allowing use of all available data from all participants rather than excluding or imputing missing data and incorporating serial correlations over time leading to less bias than traditional repeated measures ANOVA models.
The experimental group was the primary fixed-effect independent variable. The main effect of interest was the intervention condition × time interaction. Furthermore, because we were interested in assessing both short- and long-term effects of the intervention, we modelled a series of planned comparisons that looked at significant changes from study entry at each time point for CP+ compared to each of the other two groups (IC, CP).
Finally, we assessed the possibility that the intervention was more effective for certain population subgroups. Therefore, we tested for three possible moderators: age (14–19 years, n = 513 vs. 20–25 years, n = 534), race (African American, n = 838 vs. Latina/White, n = 209), and stress (top tertile, n = 388 vs. middle/lower tertiles, n = 659) to represent highest risk groups. Separate tests for the moderator were assessed on each outcome by entering the Intervention condition × Moderator × Time interaction in the random effects regression for each planned contrast. Significant interactions were followed with simple effects to assess the nature of the interaction.
Results
Description of study participants
Of the 1538 eligible adolescents and young women, 1047 enrolled in the study: 68% participation rate (CONSORT Figure available in prior publication (18)). Those who agreed to participate in the study were more likely to be African American, older and at a later gestational age at initial screening than those who refused to participate (all p < 0.01). Recruitment was nearly equivalent between the two study sites: Atlanta, GA, (n = 544, 52%) and New Haven, CT, (n = 503, 48%). There were no differences by study arm in rates of attrition, which was uniformly high; 92% of women interviewed at study entry completed at least one follow-up interview.
Eighty per cent of participants were African American, 13% were Latina, 6% White, and 1% were mixed or other race/ethnicity. Average age was 20.4 years (SD = 2.6), with 49% aged 14–19 and 51% aged 20–25. With regard to education: 38% had completed high school (or graduate equivalent degree), 36% were still in high school and 26% had dropped out. Only 32% were currently employed; the remainder received public assistance (22%) or economic support from the baby's father (25%) or family members (16%). All patients had public (e.g. Medicaid) or hospital assistance for complete prenatal care coverage. Forty-eight per cent were nulliparous.
Baseline comparisons by study condition
Despite randomisation, group differences can emerge. Therefore, we examined differences between participants by study condition at study entry. There were no differences between the three intervention groups on age, education, relationship status, alcohol or drug use, stress, depression, social support or conflict (all p > 0.05). However, there were baseline differences on three variables: race, health behaviour and self-esteem. By chance, individuals randomised to CP+ were more likely to be African American: 87% CP+ vs. 79% CP vs. 74% IC (χ2 = 19.97, p = 0.003). CP+ and CP groups reported slightly fewer positive health behaviours (e.g. nutrition, exercise) at study entry (M = 34.3 vs. M = 33.3 vs. 33.0; F = 3.13, p = 0.04). Finally, those randomised to CP+had lower self-esteem than CP and IC groups (M = 5.0 vs. 5.3 vs. 5.2, F = 3.65, p = 0.03). Therefore, race as well as baseline levels of positive health behaviours and self-esteem were controlled in all subsequent analyses.
Psychosocial changes over time by intervention condition
Based on intention-to-treat analyses, there was only one difference in change of any psychosocial outcomes over time between study conditions (Table 1). There were no differences in change of psychosocial outcomes over time between CP+ and the IC group. There were no main effects, but there was one significant Time × Intervention Condition Interaction between CP+ and CP: individuals in CP+ had significantly less reduction in stress from study entry to 1-year postpartum compared to those randomised to CP (t = 2.03, p = 0.04). Note, however, while not statistically significant, the CP+ group reported the lowest levels of baseline stress (18.6 for CP+, 19.9 for CP and 19.4 for IC), stress declined for all study participants, and that by 12 months postpartum, stress was relatively equivalent for all groups (14.6–14.9).
Table 1.
Means of psychological outcomes over time across intervention conditions.
| Baseline | Time 2 | Time 3 | Time 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Second trimester pregnancy | Third trimester pregnancy | 6 months postpartum | 12 months postpartum | |||||||||
|
|
|
|
|
|||||||||
| IC | CP | CP+ | IC | CP | CP+ | IC | CP | CP+ | IC | CP | CP+ | |
| M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | |
| Self-esteem | 32.8 (0.61) | 32.2 (0.62) | 33.0 (0.63) | 33.4 (0.38) | 33.3 (0.38) | 34.3 (0.38) | 34.2 (0.40) | 34.0 (0.41) | 34.8 (0.40) | 34.9 (0.79) | 34.4 (0.80) | 34.7 (0.70) |
| Depression | 13.1 (0.99) | 14.2 (1.0) | 13.2 (1.0) | 12.3 (0.64) | 12.8 (0.64) | 11.5 (0.63) | 9.8 (0.64) | 10.3 (0.67) | 9.2 (0.65) | 9.3 (1.3) | 9.4 (1.3) | 9.4 (1.3) |
| Social support | 28.9 (0.72) | 28.5 (0.74) | 28.7 (0.74) | 29.6 (0.44) | 29.6 (0.44) | 29.9 (0.43) | 29.6 (0.48) | 29.6 (0.48) | 29.9 (0.48) | 29.6 (0.95) | 29.6 (0.95) | 29.8 (0.94) |
| Social conflict | 21.3(0.86) | 22.0 (0.88) | 21.2 (0.88) | 20.1 (0.55) | 21.0 (0.54) | 19.9 (0.54) | 19.0 (0.57) | 18.9 (0.59) | 18.2 (0.55) | 18.6 (1.1) | 18.6 (1.1) | 18.1 (1.1) |
| Stress* | 19.4 (0.84) | 19.9 (0.86) | 18.6 (0.87) | 17.5 (0.54) | 18.5 (0.53) | 16.6 (0.53) | 15.9 (0.56) | 16.2 (0.58) | 14.8 (0.56) | 14.6 (1.1) | 14.8 (1.1) | 14.9 (1.1) |
Notes: IC, individual care; CP, CenteringPregnancy; CP+, CenteringPregnancy Plus; M, mean; SE, standard error; CP+ compared to CP group between time 1 and time 4; t-test = 2.03.
p = 0.04.
Psychosocial changes over time by intervention condition for high-risk subgroups
Results showed no significant interactions for age or race (i.e. no differences in intervention effectiveness for those aged 14–19 vs. 20–25 or for African Americans vs. Latina/White). However, several significant interactions based on psychosocial stress at study entry were found. Participants in the top tertile of stress early in pregnancy (n = 388) who were randomly assigned to CP+ had significantly better psychosocial outcomes compared to those randomised to IC. Specifically, there were significant Stress × Intervention × Time interactions for self-esteem, stress, social conflict and depression. There was no effect for social support.
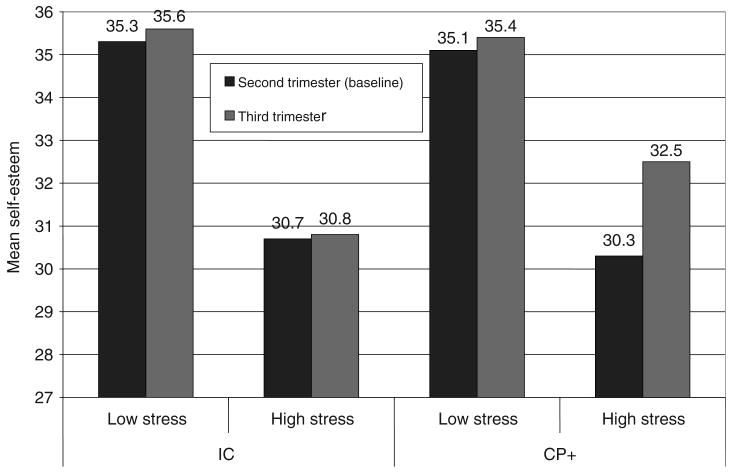
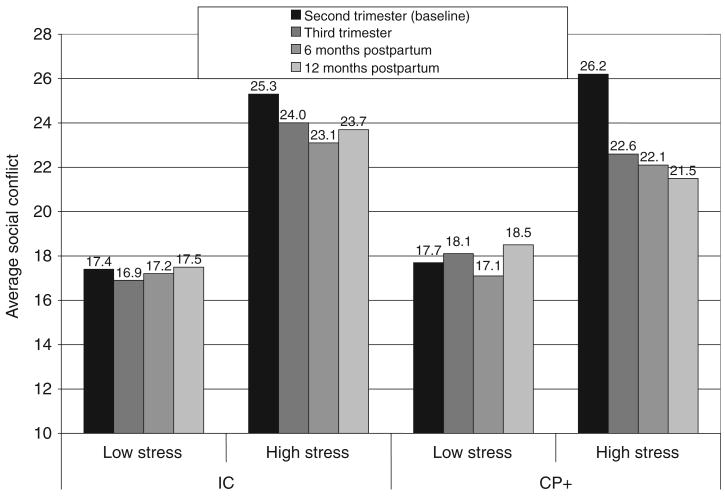
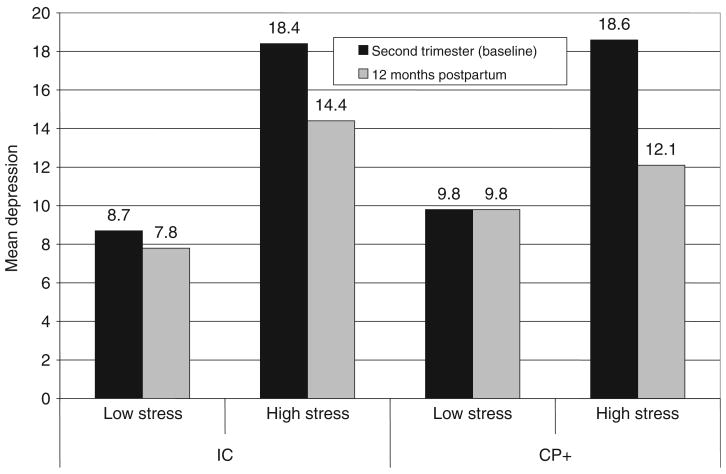
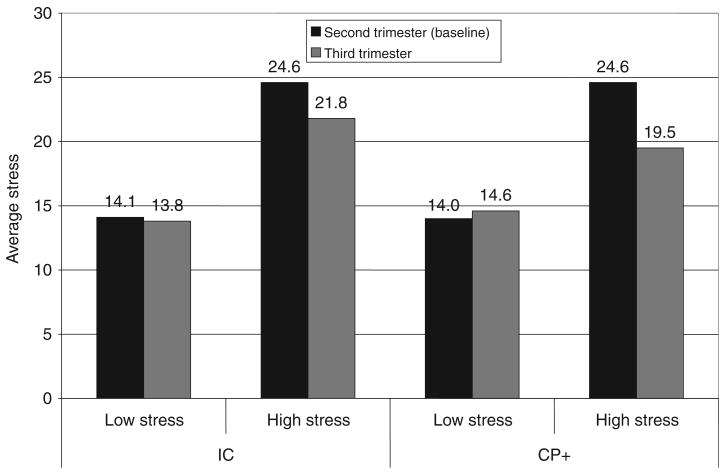
High stress young women assigned to CP+ vs. IC had significant increases in self-esteem (t = −2.64, p = 0.009), and significant decreases in stress (t = 2.84, p = 0.005) and social conflict (t = 2.68, p = 0.008) in the third trimester of pregnancy (Figures 1–3), though with the exception of social conflict, these did not persist into the postpartum period. There were marked differences for social conflict (t = 2.89, p = 0.004; Figure 3) and depression postpartum (t = 2.32, p = 0.02; Figure 4): among those in the top tertile of stress, those randomly assigned to CP+ showed significantly greater decline in social conflict and depression from study entry to 1-year postpartum, compared to those randomly assigned to standard IC. In addition, CP+ had significantly greater reduction in perceived social conflict from baseline to time 2 compared to CP (t = 2.62, p = 0.009), though again no differences in the postpartum period. Post hoc analyses indicated that participants in the top tertile of stress did not differ from those with lower stress by race, age, education, employment status or parity (all p-values > 0.05, chi-squared tests).
Figure 1.
Changes in self-esteem from second (time 1) to third (time 2) trimester of pregnancy for IC and CP+ groups.
Figure 3.
Changes in social conflict from second trimester (time 1) to 12 months postpartum (time 4) for IC and CP+ groups.
Figure 4.
Changes in depression from time 1 to time 4 for IC and CP+ groups.
Discussion
In this randomised controlled trial of young urban women, we documented no differences in psychosocial outcomes across all three study conditions based on intent-to-treat analyses. However, for a group of potentially vulnerable women with high reported stress early in pregnancy, CP+ resulted in several benefits throughout the pregnancy: increased self-esteem as well as decreased stress and social conflict. Moreover, there were significant declines in social conflict and depression 1-year postpartum. Therefore, these results show that this integrated prevention programme that has already been shown to improve prenatal, postnatal and reproductive health for young women (Ickovics et al., 2007; Kershaw et al., 2009), also improves psychosocial functioning for a core group of high-risk women. This suggests that it may be feasible to incorporate components that improve psychosocial functioning within existing programmes and services (e.g. group prenatal care) designed to change other important health outcomes.
Psychosocial factors among pregnant women are important, given their impact on perinatal outcomes. Specifically, previous study findings highlight the important of stress during pregnancy on health outcomes such as pre-term labour and infant birthweight (Dole et al., 2004; Dominguez et al., 2005; Dunkel-Schetter, Gurung, Lobel, & Wadhwa, 2001; Feldman, Dunkel-Schetter, Sandman, & Pathik, 2000; Messer, Dole, Kaufman, & Savitz, 2005; Sable & Wilkinson, 2000; Wadhwa, Culhane, Rauh, & Barve, 2001). Adolescents who experience high stress during and after pregnancy are at increased risk for difficult maternal adjustment and high postpartum emotional distress (Holub et al., 2007). Interventions are needed during pregnancy tailored to those most vulnerable to stress to reduce negative pregnancy-related health outcomes. We documented reduction in stress as well as a positive impact on other psychosocial factors during and after pregnancy.
The dynamics of CP+ group prenatal care includes several components by which positive psychosocial outcomes are realised. Individuals learn stress reduction techniques and engage in discussions about depression and affect regulation which may help them manage stressors and depression that can occur during and after pregnancy. In addition, women engage in self-care activities, goal setting exercises and communication and negotiation skills-building which could serve to increase feelings of self-esteem. Most notably, the strongest finding for CP+ women was the reduction in social conflict. This effect is probably attributed to the heavy emphasis in CP+ on developing effective communication and negotiation skills. Women are taught proper use of assertiveness and negotiation techniques and role-play several scenarios using these techniques to convince their partners to engage in safe sex practices. These techniques might easily transfer to handling conflict situations in other aspects of their lives.
CP+ may be particularly advantageous in resource-poor settings with women at risk for greater stress during pregnancy (e.g. medically or socially high risk due to indigent or immigration status, low education and skills). Group interventions are more multi-faceted than many other clinical and psychosocial interventions that seek to augment care with more visits or more information using didactic approaches, which may be one reason for these relatively favourable outcomes (Amaro, Raj, Reed, & Cranston, 2002; DiClemente et al., 2004). Other intervention approaches must also be considered. For instance, a recent systematic review by Pate concluded that breastfeeding promotion programmes delivered via the Internet were an appealing alternative to time-consuming and expensive provider-based breastfeeding education and support (Pate, 2009).
This study is limited in several ways. First, overall effects of the intervention were not found using intention to treat analysis, though important subgroup differences were identified. Nonetheless, the use of multiple comparisons and its consequent risk of Type-I error is notable. In terms of the potency of the intervention, it may be necessary to strengthen the psychosocial components of CP+ in order to improve psychosocial functioning for everyone and not just those with high initial levels of stress. Second, the sample represents a relatively restricted group of young, ethnic minority women of low socioeconomic status who attend urban hospital clinics for prenatal care. This is a group at highest risk of adverse perinatal and psychosocial outcomes, and therefore may be most in need of substantive clinical intervention to reduce risk. We believe that this model may be useful in other urban clinics and resource-poor settings in the US and abroad, where women have more limited access to comprehensive prenatal care services and information. Replication with diverse patient populations and within diverse clinical settings is essential to ensure reliability, generalisability and clinical effectiveness.
Future directions
Future research is needed to better identify those at highest risk of stress and to further investigate the mechanisms by which CP+ may have its effects as well as to demonstrate the actual impact on pregnancy-related health outcomes. Group prenatal care provides substantially more contact with providers, and we describe how medical and ancillary support services are well-integrated to respond to the complex needs of pregnant women (18–19). Further examination on how increased self-esteem as well as reduced stress, social conflict and depression, as found in this study, could translate into a positive impact on biological outcomes of pregnancy (e.g. low birthweight, pre-term birth) is needed. Once identified, factors most influential in determining positive psychosocial and clinical health outcomes should be incorporated into group prenatal care programmes and such programmes should be targeted and tailored to young women most vulnerable to high stress during pregnancy.
Figure 2.
Changes in stress from second (time 1) to third (time 2) trimester of pregnancy for IC and CP+ groups.
Acknowledgments
This research was funded by NIMH R01 MH/HD61175. The trial is registered on ClinicalTrials.gov: NCT00271960. This publication was also made possible by CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Ickovics was the Principal Investigator who designed the study and prepared the manuscript. Kershaw was the Project Director. Reed and Kershaw conducted all data analyses. Reed, Kershaw and Ickovics were responsible for interpretation of the data. Westdahl was responsible for study implementation in Atlanta. Ickovics and Magriples were responsible for study implementation in New Haven. Kershaw, Reed and Magriples contributed substantively to the writing and editing of this manuscript. Rising developed the CenteringPregnancy group prenatal care model and conducted all provider training. All authors contributed to manuscript review and editorial suggestion.
Footnotes
Declaration of interest: Claire M. Westdahl conducts occasional training facilitation workshops for the Centering Healthcare Institute. No commercial entity has agreed to direct any benefits to any organisation with which she is affiliated. Sharon Schindler Rising is the Executive Director of the non-profit entity, Centering Healthcare Institute that promotes the CenteringPregnancy model of care nationally and internationally. There are no other known conflicts of interest.
References
- Amaro H, Raj A, Reed E, Cranston K. Implementation and long-term outcomes of two HIV intervention programs for Hispanic women. Health Promotion Practice. 2002;3:245–254. [Google Scholar]
- Barnet B, Liu J, DeVoe M, Alperovitz-Bichell K, Duggan AK. Home visiting for adolescent mothers: Effects on parenting, maternal life course, and primary care linkage. Annals of Family Medicine. 2007;5:224–232. doi: 10.1370/afm.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Ecological systems theory. In: Vasta R, editor. Annals of child development. Greenwich, CT: JAI Press; 1989. pp. 187–249. [Google Scholar]
- Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: An investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. American Journal of Obstetrics and Gynecology. 2007;197:e1–e9. doi: 10.1016/j.ajog.2007.04.036. [DOI] [PubMed] [Google Scholar]
- C'de Baca J, Lapham SC, Skipper BJ, Watkins ML. Use of computer interview data to test associations between risk factors and pregnancy outcomes. Computers and Biomedical Research. 1997;30:232–243. doi: 10.1006/cbmr.1997.1449. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont symposium on applied social psychology. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, III, et al. Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of the American Medical Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- Dole N, Savitz DA, Siega-Riz AM, Hertz-Picciotto I, McMahon MJ, Buekens P. Psychosocial factors and preterm birth among African American and White women in central North Carolina. American Journal of Public Health. 2004;94:1358–1365. doi: 10.2105/ajph.94.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominguez TP, Dunkel-Schetter C, Mancuso R, Rini CM, Hobel C. Stress in African American pregnancies: Testing the roles of various stress concepts in prediction of birth outcomes. Annals of Behavioral Medicine. 2005;29:12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- Dunkel-Schetter C, Gurung RAR, Lobel M, Wadhwa PD. Stress processes in pregnancy and birth: Psychological, biological, and sociocultural influences. In: Baum A, Revenson TA, Singer JE, editors. Handbook of health psychology. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. pp. 495–518. [Google Scholar]
- DuPlessis HM, Bell R, Richards T. Adolescent pregnancy: Understanding the impact of age and race on outcomes. Journal of Adolescent Health. 1997;20:187–197. doi: 10.1016/S1054-139X(96)00174-7. [DOI] [PubMed] [Google Scholar]
- Feldman P, Dunkel-Schetter C, Sandman C, Pathik D. Maternal social support predicts birth weight and fetal growth in human pregnancy. Psychosomatic Medicine. 2000;62:715–725. doi: 10.1097/00006842-200009000-00016. [DOI] [PubMed] [Google Scholar]
- Gold KJ, Dalton VK, Schwenk TL, Hayward RA. What causes pregnancy loss? Preexisting mental illness as an independent risk factor. General Hospital Psychiatry. 2007;29:207–213. doi: 10.1016/j.genhosppsych.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Hagsborg WJ. Scores of middle school-age students on the Rosenberg Self-Esteem Scale. Psychological Report. 1996;78:1071–1074. [Google Scholar]
- Holub CK, Kershaw TS, Ethier KA, Lewis JB, Milan S, Ickovics JR. Prenatal and parenting stress on adolescent maternal adjustment: Identifying a high-risk subgroup. Maternal and Child Health Journal. 2007;11:153–159. doi: 10.1007/s10995-006-0159-y. [DOI] [PubMed] [Google Scholar]
- Ickovics JR. “Bundling” HIV prevention: Integrating services to promote synergistic gain. Preventive Medicine. 2008;46:222–225. doi: 10.1016/j.ypmed.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, Rising SS. Group prenatal care and perinatal outcomes: A randomized controlled trial [erratum in Obstetrics and Gynecology. 2007 Oct., 110, 937] Obstetrics and Gynecology. 2007;110:330–339. doi: 10.1097/01.AOG.0000275284.24298.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics JR, Meade CS, Kershaw TS, Milan S, Lewis JB, Ethier KA. Urban teens: Trauma, posttraumatic growth, and emotional distress among female adolescents. Journal of Consulting and Clinical Psychology. 2006;74:841–850. doi: 10.1037/0022-006X.74.5.841. [DOI] [PubMed] [Google Scholar]
- Kershaw T, Magriples U, Westdahl C, Rising S, Ickovics J. Pregnancy as a window of opportunity for HIV prevention: Effects of an HIV intervention delivered within prenatal care. American Journal of Public Health. 2009;99:2079–2086. doi: 10.2105/AJPH.2008.154476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Henderson CR, Hanks C, Cole R, Tatelbaum R, et al. Barnard K. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: A randomized controlled trial. Journal of the American Medical Association. 1997;278:644–652. [PubMed] [Google Scholar]
- Koniak-Griffin D, Anderson NL, Brecht ML, Verzemnieks I, Lesser J, Kim S. Public health nursing care for adolescent mothers: Impact on infant health and selected maternal outcomes at 1 year postbirth. Journal of Adolescent Health. 2002;30:44–54. doi: 10.1016/s1054-139x(01)00330-5. [DOI] [PubMed] [Google Scholar]
- Koniak-Griffin D, Anderson NL, Verzemnieks I, Brecht ML. A public health nursing early intervention program for adolescent mothers: Outcomes from pregnancy through 6 weeks postpartum. Nursing Research. 2000;49:130–138. doi: 10.1097/00006199-200005000-00003. [DOI] [PubMed] [Google Scholar]
- Koniak-Griffin D, Lesser J, Uman G, Nyamathi A. Teen pregnancy, motherhood, and unprotected sexual activity. Research in Nursing and Health. 2003;26:4–19. doi: 10.1002/nur.10062. [DOI] [PubMed] [Google Scholar]
- Langer A, Campero L, Garcia C, Reynoso S. Effects of psychosocial support during labour and childbirth on breastfeeding, medical interventions, and mothers' wellbeing in a Mexican public hospital: A randomised clinical trial. British Journal of Obstetrics and Gynaecology. 1998;105:1056–1063. doi: 10.1111/j.1471-0528.1998.tb09936.x. [DOI] [PubMed] [Google Scholar]
- Langer A, Farnot U, Garcia C, Barros F, Victora C, Belizan JM, Villar J. The Latin American trial of psychosocial support during pregnancy: Effects on mother's wellbeing and satisfaction. Latin American Network for Perinatal and Reproductive Research (LANPER) Social Science and Medicine. 1996;42:1589–1597. doi: 10.1016/0277-9536(95)00262-6. 6. [DOI] [PubMed] [Google Scholar]
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: A life-course perspective [see comment] Maternal and Child Health Journal. 2003;7:13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- Malow RM, Kershaw T, Sipsma H, Rosenberg R, Dévieux JG. HIV preventive interventions for adolescents: A look back and ahead. Current HIV/AIDS Reports. 2007;4:173–180. doi: 10.1007/s11904-007-0025-6. [DOI] [PubMed] [Google Scholar]
- Meade CS, Ickovics JR. Systematic review of sexual risk among pregnant and mothering teens in the USA: Pregnancy as an opportunity for integrated prevention of STD and repeat pregnancy. Social Science and Medicine. 2005;60:661–678. doi: 10.1016/j.socscimed.2004.06.015. [DOI] [PubMed] [Google Scholar]
- Messer LC, Dole N, Kaufman JS, Savitz DA. Pregnancy intendedness, maternal psychosocial factors and preterm birth. Maternal and Child Health Journal. 2005;9:403–412. doi: 10.1007/s10995-005-0021-7. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Shenassa ED. The environmental “riskscape” and social inequality: Implications for explaining maternal and child health disparities. Environmental Health Perspectives. 2006;114:1150–1153. doi: 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen JD, Carson ML, Parris KM, Place P. A comparison pilot study of public health field nursing home visitation program interventions for pregnant Hispanic adolescents. Public Health Nursing. 2003;20:412–418. doi: 10.1046/j.1525-1446.2003.20509.x. [DOI] [PubMed] [Google Scholar]
- O'Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Social Science and Medicine. 1993;36:1161–1167. doi: 10.1016/0277-9536(93)90236-w. [DOI] [PubMed] [Google Scholar]
- Olds D, Henderson CR, Jr, Cole R, Eckenrode J, Kitzman H, Luckey D, et al. Powers J. Long-term effects of nurse home visitation on children's criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial [see comment] Journal of the American Medical Association. 1998;280:1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Tatelbaum R, Chamberlin R. Improving the delivery of prenatal care and outcomes of pregnancy: A randomized trial of nurse home visitation. Pediatrics. 1986;77:16–28. [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: A randomized trial of nurse home visitation. American Journal of Public Health. 1988;78:1436–1445. doi: 10.2105/ajph.78.11.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paik SJ. Self concept of pregnant teenagers. Journal of Health and Social Policy. 1987;3:93–111. doi: 10.1300/J045v03n03_07. [DOI] [PubMed] [Google Scholar]
- Pate B. A systematic review of the effectiveness of breastfeeding intervention delivery methods. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2009;38:642–653. doi: 10.1111/j.1552-6909.2009.01068.x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raudenbush S, Bryk AS. Hierarchical linear models. 2nd. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Rosen D, Seng JS, Tolman RM, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. Journal of Interpersonal Violence. 2007;22:1305–1314. doi: 10.1177/0886260507304551. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Sable MR, Wilkinson DS. Impact of perceived stress, major life events and pregnancy attitudes on low birth weight. Family Planning Perspectives. 2000;32:288–294. [PubMed] [Google Scholar]
- Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, et al. Mercer MB. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. American Journal of Public Health. 2000;90:57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silbert PL, Mokri B, Schievink WI. Headache and neck pain in spontaneous internal carotid and vertebral artery dissections. Neurology. 1995;45:1517–1522. doi: 10.1212/wnl.45.8.1517. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Streetman LG. Contrasts in the self-esteem of unwed teenage mothers. Adolescence. 1987;22:459–464. [PubMed] [Google Scholar]
- Ventura SJ, Peters KD, Martin JA, Maurer JD. Births and deaths: United States, 1996. Monthly Vital Statistics Report. 1997;46:1–40. [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Archives of Women's Mental Health. 2008;11:67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]
- Visintini R, Bagnato M, Campanini E, Fontana S, Fossati A, Novella L, Maffei C. An assessment of self-esteem in HIV-positive patients. AIDS Care. 1995;7:S99–S104. doi: 10.1080/09540129550126902. [DOI] [PubMed] [Google Scholar]
- Wadhwa PD, Culhane JF, Rauh V, Barve SS. Stress and preterm birth: Neuroendocrine, immune/inflammatory, and vascular mechanisms. Maternal and Child Health Journal. 2001;5:119–125. doi: 10.1023/a:1011353216619. [DOI] [PubMed] [Google Scholar]