Abstract
Study Objectives:
REM sleep behavior disorder (RBD) is a parasomnia in which normal muscle atonia of REM sleep is lost. The aim of this study was to confirm if diagnostic delay exists in RBD and identify any contributing factors.
Methods:
A database was compiled of 49 patients with RBD seen at a tertiary referral center from 2005 to 2011 by retrospective review of referral letters and polysomnographic (PSG) reports. Patients with comorbid narcolepsy were excluded. A questionnaire was sent to investigate diagnostic delay, management, and comorbidities.
Results:
Mean diagnostic delay was 8.7 ± 11 (median 4.5, IQR 1.75–11.75) years in 30 questionnaire responders. Common reasons for diagnostic delay included belief that symptoms were not serious enough to consult a doctor (59%), mild or infrequent occurrence of sleep behavior (56%), belief that symptoms may resolve (47%), and lack of knowledge of treatment options (47%). The bed partner was an important influence, with the decision to seek medical attention being made jointly by the patient and partner in 47%.
Conclusions:
This study has demonstrated the existence of significant diagnostic delay in RBD, mainly due to lack of understanding of the disorder and its treatment by patients and members of the medical profession.
Citation:
White C; Hill EA; Morrison I; Riha RL. Diagnostic delay in REM sleep behavior disorder (RBD). J Clin Sleep Med 2012;8(2):133-136.
Keywords: REM sleep behavior disorder, parasomnias, sleep-related violence, delayed diagnosis, polysomnography, parkinsonian disorders, clonazepam, melatonin
REM sleep behavior disorder (RBD) is a parasomnia characterized by loss of normal muscle atonia in REM sleep.1 Patients may act out dreams, causing injury to themselves or their bed partner, resulting in relationship problems and decreased quality of life. Dream enactment in RBD occasionally has lethal results.2
There are two main diagnostic categories of RBD. Secondary or symptomatic RBD occurs in association with comorbid neurological disease such as narcolepsy or neurodegenerative disease, most commonly Parkinson disease (PD), Lewy body dementia, and multiple system atrophy3,4; or medication, including β-blockers and antidepressants.5–7 Idiopathic RBD occurs in the absence of any associated neurological condition or medication.
RBD appears to be underdiagnosed,3,8,9 with prevalence estimated at 0.5% of the UK population.9,10 RBD occurs predominantly in men, the majority of patients presenting between 52 and 61 years of age.5
RBD was first described in humans in 1986,11 and research in the area has accelerated in recent years, with advances in neuroimaging, and better recognition and understanding of the condition.3,4 However, an important clinical aspect of this disorder which has been neglected is diagnostic delay—a problem encountered in other sleep disorders, especially narcolepsy.12,13
This study aimed to document the degree of diagnostic delay in RBD patients presenting to a tertiary referral center in the UK. The presence of comorbid sleep disorders and presence of a bed partner were hypothesized to reduce diagnostic delay.
BRIEF SUMMARY
Current Knowledge/Study Rationale: REM sleep behavior disorder (RBD) is a potentially lethal parasomnia in which normal muscle atonia during rapid eye movement (REM) sleep is lost. Although diagnostic delay is documented in other sleep disorders, such as narcolepsy, diagnostic delay in RBD has not, thus far, been investigated.
Study Impact: This is the first study to focus specifically on diagnostic delay in RBD. The study demonstrates the existence of significant diagnostic delay, highlighting the need for greater awareness of the disorder and its treatment options amongst patients and medical professionals.
METHODS
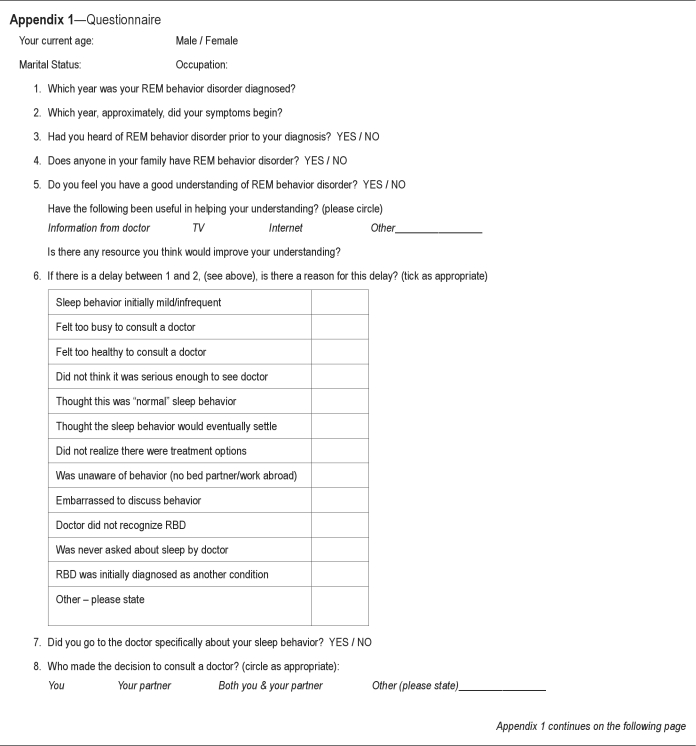
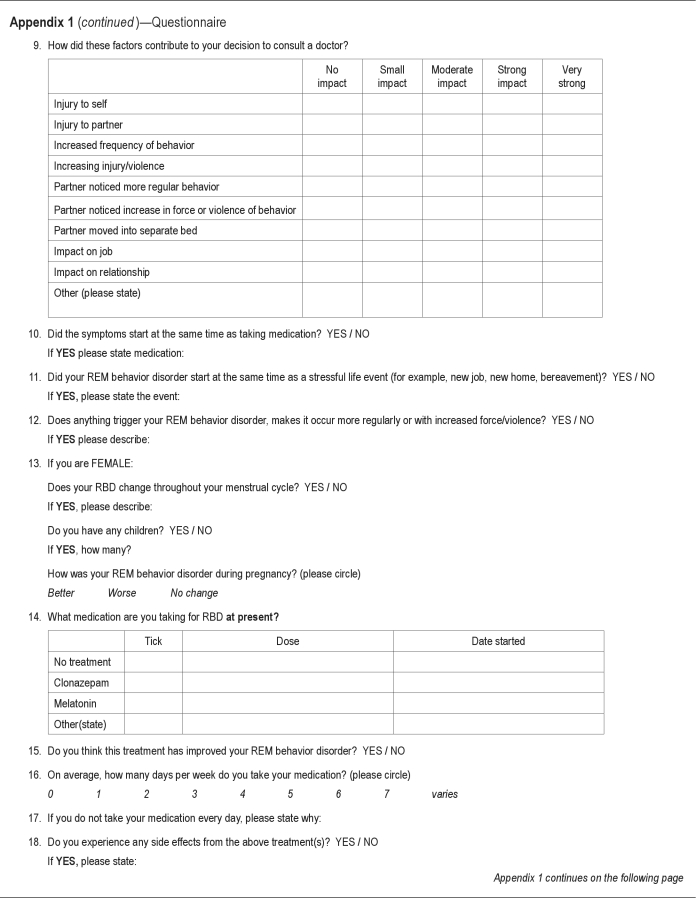
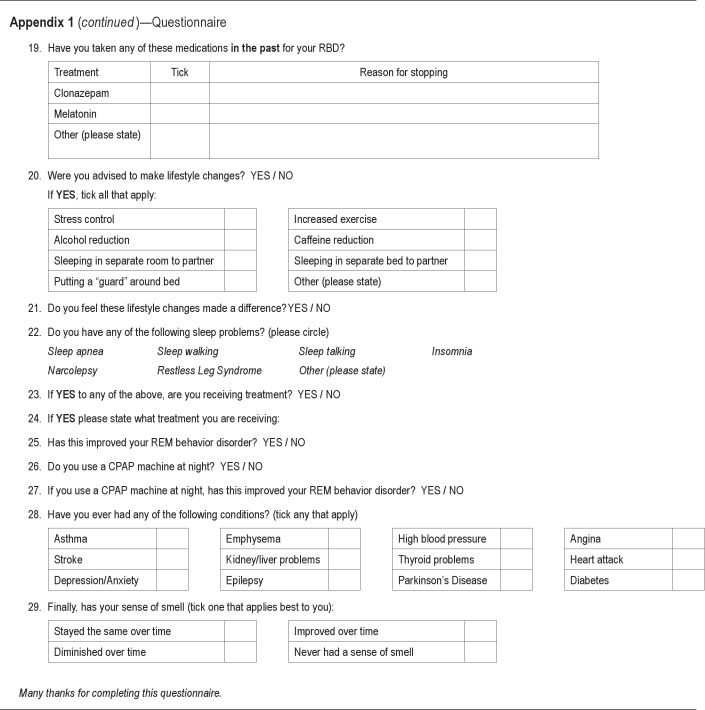
A questionnaire (Appendix 1) was developed to explore aspects of diagnosis and management of RBD: symptom duration before diagnosis; factors delaying diagnosis; features of RBD contributing to seeking medical help; identification of potential triggers (stress, menstruation, medication); management of RBD—pharmacological and behavioral; medication adherence and side effects; control of RBD; and comorbidities including other sleep disorders. All questionnaires were anonymized and mailed to patients with a covering letter. Ethical approval is not required by NHS Lothian for case series or audit.
All patients with suspected RBD at a tertiary referral sleep center from 2005 to March 2011 were reviewed (n = 66). Patients were excluded if they had a diagnosis of RBD with narcolepsy (the etiology of RBD in this group may be multifactorial and differ from RBD without narcolepsy14,15) or if they did not fulfil ICSD-2 criteria for diagnosis of RBD.16 The medical case notes and polysomnographic sleep study (PSG) data of the remaining 49 patients were reviewed. Diagnosis was based on history (from both patient and partner where possible) and standard video PSG, in accordance with ICSD-2 criteria.
Statistical analysis was undertaken using SPSS17 (Chicago, Illinois). Student's t-test, χ2 test, and Fisher exact test were used to assess parametric data, and Mann Whitney U test for non-normally distributed variables. All tests were 2-sided. Statistical significance was taken at p < 0.05. Results were reported as mean ± standard deviation (SD) or as a median with interquartile range (IQR 25–75). As not all patients answered every question, n is reported as the number of patients responding to each particular question.
RESULTS
Of 49 RBD patients included in the study, 44 (90%) were male and 5 (10%) female. The mean age at first referral was 55 ± 14 years for males and 36 ± 10 females (p = 0.006). Forty-one patients (36 male: 5 female) were diagnosed with idiopathic RBD, 6 (all male) with RBD secondary to neurological disease, and 2 (both male) secondary to medication (citalopram and bisoprolol; p = 0.6).
The response rate to the questionnaire was 65% (n = 32). Non-responders were significantly younger than responders (responders male 61 ± 9, female 38 ± 11 v. non-responders (male 44 ± 16, female 34 ± 13, p < 0.0001), but did not differ significantly in terms of sex distribution or RBD type (data not shown).
Polysomnographic Data
PSG data were available for all 49 patients. Twenty-seven patients (55%) had evidence of dream enactment on video, with no significant sex (p = 0.16) or age (p = 0.41) differences. All patients were positive for REM sleep without atonia (RSWA).
Fifty-three percent of patients had an apnea-hypopnea index (AHI) > 15 per hour, indicative of moderate-to-severe sleep disordered breathing. This differed significantly by age (p = 0.005); those with AHI < 15 were younger than those with a higher AHI (47 ± 15 years v. 59 ± 13 years). There was no significant difference by sex (p = 0.17) or RBD type (p = 0.6).
Diagnostic Delay
Overall, the mean delay in diagnosing RBD was 8.7 ± 11 years (median 4.5, IQR 1.75–11.75; n = 30). There was a significant gender difference with women having a longer diagnostic delay than men (22 ± 11 years v. 7 ± 10 years, respectively; p = 0.03). There was no significant difference in diagnostic delay between the different types of RBD (p = 0.56): idiopathic RBD 9.4 ± 11.4 years, neurological RBD 8.7 ± 9.9 years, RBD secondary to medication 0.5 ± 0.7 years. Of the 32 people who responded, the most common reason for not seeking medical help was a belief that the symptoms were not serious enough to consult a doctor (59%; n = 19). Other common reasons were mild or infrequent occurrence of the sleep behavior (56%; n = 18), belief that the symptoms would eventually settle (47%; n = 15) and failure to realize that there might be treatment options for the condition (47%; n = 15). Thirty-one percent of patients (n = 10) were never asked about sleep by their doctor. There were no significant gender differences. There was no significant difference in reasons for diagnostic delay with RBD type or age, although those older than 50 years were more likely to experience delay due to their doctor not recognizing RBD, with a trend towards significance (p = 0.07). AHI and symptoms of possible obstructive sleep apnea did not play a role in bringing attention to RBD (p = 0.72): AHI < 15 8 ± 10 years (n = 12), AHI > 15 9 ± 12 years (n = 18).
Seventy-two percent (n = 23) of patients consulted a doctor specifically regarding their sleep behavior, with no significant age or gender differences observed. The decision to consult a doctor was most commonly a joint decision by both partners (47%, n = 15). All females making the decision to consult a doctor did so themselves (p = 0.023, n = 3); however, the low number of responders in this group should be noted.
Factors influencing the decision by patients to seek medical assessment of their nocturnal behavior are shown in Table 1. The most important factors cited by patients as having a strong or very strong impact on their decision to seek medical review were: (i) the partner noticing more regular abnormal sleep behaviors (88%, n = 23); (ii) the partner noticing an increase in the violence or force of the behavior (79%, n = 19); (iii) increased frequency of behavior (76%, n = 19); (iv) injury to the partner (55%, n = 12); and (v) increasing injury/violence (54%; n = 12). No significant age differences were evident (data not shown). However, men were significantly more likely to consult on the basis of factors i and iii above (both p = 0.002).
Table 1.
Factors influencing patients’ decision to consult a doctor regarding abnormal sleep behavior
| Males (n = 29) |
Females (n = 3) |
p | |||||
|---|---|---|---|---|---|---|---|
| No or small impact | Moderate impact | Strong or very strong impact | No or small impact | Moderate impact | Strong or very strong impact | ||
| Injury to self | 13 | 6 | 1 | 2 | 0 | 0 | 0.60 |
| Injury to partner | 2 | 7 | 11 | 1 | 0 | 1 | 0.24 |
| Increased frequency of behavior | 0 | 5 | 18 | 1 | 0 | 1 | 0.002 |
| Increasing injury/violence | 5 | 4 | 11 | 1 | 0 | 1 | 0.66 |
| Partner noticed more regular behavior | 0 | 2 | 22 | 1 | 0 | 1 | 0.002 |
| Partner noticed increase in force or violence of behavior | 2 | 2 | 18 | 1 | 0 | 1 | 0.24 |
| Partner moved into separate bed | 9 | 2 | 6 | 1 | 0 | 0 | 0.66 |
| Impact on job | 11 | 0 | 5 | 0 | 0 | 1 | 0.35 |
| Impact on relationship | 8 | 6 | 7 | 0 | 0 | 2 | 0.18 |
The impact of RBD on the individual's career was important in 53% of patients, with 9 of 17 patients rating this as having at least a small impact on their decision to seek treatment.
Comorbidities
Twenty-five of 31 responders (81%) reported that they had one or more comorbid sleep disorders. Thirteen patients (41%) had comorbid sleep apnea (defined as an AHI > 15), 8 of whom (62%) were using continuous positive airway pressure (CPAP) treatment. Six users (75%) found CPAP improved their RBD symptoms. No significant differences in mean diagnostic delay were found between those with or without comorbid sleep disorders (data not shown).
Treatment
Current treatment information was provided by 28 responders. Thirty-six percent were not on medication; 50% were taking clonazepam only, at doses in the range 0.5–2 mg per night; 4% were taking melatonin only, 2–6 mg per night; 7% were on combined clonazepam and melatonin therapy. One patient stated he was taking mirtazapine as his only treatment for RBD. In terms of medication use, there were no significant differences with age, gender or RBD type (data not shown).
Lifestyle
Thirty-eight percent of responders stated that lifestyle changes had been recommended to them (n = 12). Changes to sleeping arrangements were recommended to 14 of the 31 patients: sleeping in separate beds (19%), sleeping in a separate room (19%) and putting a guard around the bed (6%). Along with sleeping in separate beds or rooms, caffeine reduction (19%) was the most common lifestyle change. Other recommended changes included alcohol reduction and increased exercise (both 16%). Of the 12 patients who made lifestyle changes, 5 (42%) stated that lifestyle changes made a difference to their symptoms, and 6 (50%) stated they made no difference (1 patient did not answer). Lifestyle changes showed no significant association with sex, age, or RBD type (data not shown).
DISCUSSION
This is the first study to specifically focus on diagnostic delay of an under-diagnosed and potentially lethal parasomnia. Our patient group is comparable to previously published series,4,17 with male predominance (90%) and mean age at first referral of 55 ± 14 years.
Although 72% of patients consulted specifically about their sleep behavior, the mean delay of 8.7 ± 11 years (median 4.5, IQR 1.75–11.75) shows that patients tolerated symptoms for some time before diagnosis. Additionally, 56% of patients classified their sleep behavior as initially mild/infrequent. The course of RBD often fluctuates,18 and these patients may delay seeking medical attention due to these periods of normal or only mildly disrupted sleep.
In this study, many patients initially dismissed their behavior as neither serious nor medically important. However, a large proportion consulted specifically about their sleep (72%, n = 23), showing the cumulative effect of chronic sleep disorders causing major disruption to patients' lives. Common factors for delaying diagnosis included the belief that the symptoms were not serious enough to consult a doctor (59%) and failure to realize that treatment options were available (47%). Heightening public awareness of sleep disorders could reduce diagnostic delay and improve quality of life with many RBD, patients, but this is a challenging agenda.19
The impact of RBD on the bed partner appeared to be the major driver for patients to seek medical advice. Four patients (13%) were unaware of their sleep behavior, thus delaying diagnosis. If the impact of RBD on the bed partner is more significant than the impact on the patient independently, underdiagnosis of patients who are single or have mild sleep behaviors may occur.
The absence of daytime symptoms may also delay presentation. In narcolepsy, patients with cataplexy have a shorter diagnostic delay than those without.13 If RBD patients do not have dramatic nocturnal symptoms such as violent dream enactment or injurious behavior, the condition may be tolerable. Dream enactment behavior is found in the normal, healthy population but is usually less violent and frequent than RBD.20 If this behavior is considered “subclinical RBD,”21 this may explain why increased frequency and severity of RBD symptoms were a strong or very strong prompt for presentation to a doctor in the majority of patients.
Diagnostic delay can be attributed to obstacles in health service provision.22 Lack of access to PSG can hinder diagnosis. In this study, failure to recognize the presence of RBD in primary care contributed to diagnostic delay in 31% of patients (n = 10). Thorough history-taking with direct questioning about RBD symptoms is required.9,23 To this end, an RBD screening questionnaire has been developed, and its routine use in clinical practice (particularly in at-risk populations such as PD) could aid prompt diagnosis.24 This may have particular bearing upon delayed recognition of neurodegenerative disease. Postuma et al.25 found a mean RBD diagnostic delay of 7.2 years, with 26 of 93 patients developing either PD or dementia at 11.5 ± 6.6 years from onset of symptoms.
No significant difference was found in mean diagnostic delay between those with or without comorbid sleep disorders, which suggests that the impact of RBD on the individual and their partner may be an independent factor in a patient's diagnostic delay, not influenced by the presence of comorbidities.
Clonazepam, a sedating benzodiazepine which reduces phasic EMG activity,26 is considered first-line therapy in RBD, although the evidence for its use is not strong and it should only be used in selected groups.27,28 Clonazepam contributed to improvement in 77% (n = 10) of patients. This is lower than the quoted figure from some studies, but supports others.4,14,17 Only one responder was taking melatonin, the other major treatment option, and he reported that it improved his symptoms. Melatonin can be used either alone or in conjunction with clonazepam, but again there have been few studies examining its use in detail.27,29,30 Two of our patients were taking a combination of melatonin and clonazepam, and both stated this had improved their symptoms.
A number of limitations should be considered when interpreting the results of this study, namely small sample size, the use of an unvalidated, self-administered questionnaire, and possible responder bias. In future studies, we would consider the use of a partner questionnaire in tandem with the patient questionnaire to further explore partner aspects of diagnostic delay.
This study has demonstrated the existence of significant diagnostic delay in RBD, mainly due to lack of knowledge of the disorder and its treatment options among both patients and medical professionals. We suggest that increasing knowledge of sleep disorders by targeting medical education and public awareness, particularly with RBD, would improve patients' quality of life and limit potential harm to the patient and their bed partner. Additionally, it has been suggested that RBD is an early marker of neurodegenerative disease, and identifying these patients may allow for improved treatment with neuroprotective agents in the future.1,28,31
DISCLOSURE STATEMENT
This was not an industry supported study. The author has indicated no financial conflicts of interest.
REFERENCES
- 1.Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007;130:2770–88. doi: 10.1093/brain/awm056. [DOI] [PubMed] [Google Scholar]
- 2.Schenck CH, Lee SA, Bornemann MAC, Mahowald MW. Potentially lethal behaviors associated with rapid eye movement sleep behavior disorder: review of the literature and forensic implications. J Forensic Sci. 2009;54:1475–84. doi: 10.1111/j.1556-4029.2009.01163.x. [DOI] [PubMed] [Google Scholar]
- 3.Boeve BF. REM sleep behavior disorder: Updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann N Y Acad Sci. 2010;1184:15–54. doi: 10.1111/j.1749-6632.2009.05115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schenck CH, Mahowald MW. REM sleep behavior disorder: clinical, developmental, and neuroscience perspectives 16 years after its formal identification in Sleep. Sleep. 2002;25:120–38. doi: 10.1093/sleep/25.2.120. [DOI] [PubMed] [Google Scholar]
- 5.Ebrahim IO, Peacock KW. REM sleep behavior disorder--psychiatric presentations: a case series from the United Kingdom. J Clin Sleep Med. 2005;1:43–7. [PubMed] [Google Scholar]
- 6.Morrison I, Frangulyan R, Riha RL. Beta-blockers as a cause of violent rapid eye movement sleep behavior disorder: a poorly recognized but common cause of violent parasomnias. Am J Med. 2011;124:e11. doi: 10.1016/j.amjmed.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 7.Teman PT, Tippmann-Peikert M, Silber MH, Slocumb NL, Auger RR. Idiopathic rapid-eye-movement sleep disorder: associations with antidepressants, psychiatric diagnoses, and other factors, in relation to age of onset. Sleep Med. 2009;10:60–5. doi: 10.1016/j.sleep.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Chiu HF, Wing YK, Lam LC, et al. Sleep-related injury in the elderly--an epidemiological study in Hong Kong. Sleep. 2000;23:513–7. [PubMed] [Google Scholar]
- 9.Frauscher B, Gschliesser V, Brandauer E, et al. REM sleep behavior disorder in 703 sleep-disorder patients: the importance of eliciting a comprehensive sleep history. Sleep Med. 2010;11:167–71. doi: 10.1016/j.sleep.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Ohayon MM, Caulet M, Priest RG. Violent behavior during sleep. J Clin Psychiatry. 1997;58:369–76. quiz 77. [PubMed] [Google Scholar]
- 11.Schenck CH, Bundlie SR, Ettinger MG, Mahowald MW. Chronic behavioral disorders of human REM sleep: a new category of parasomnia. 1986 [classical article] Sleep. 1986;25:293–308. [PubMed] [Google Scholar]
- 12.Dhondt K, Verhelst H, Pevernagie D, Slap F, Van Coster R. Childhood narcolepsy with partial facial cataplexy: a diagnostic dilemma. Sleep Med. 2009;10:797–8. doi: 10.1016/j.sleep.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 13.Morrish E, King MA, Smith IE, Shneerson JM. Factors associated with a delay in the diagnosis of narcolepsy. Sleep Med. 2004;5:37–41. doi: 10.1016/j.sleep.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Bonakis A, Howard RS, Williams A. Narcolepsy presenting as REM sleep behaviour disorder. Clin Neurol Neurosurg. 2008;110:518–20. doi: 10.1016/j.clineuro.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 15.Nightingale S, Orgill JC, Ebrahim IO, de Lacy SF, Agrawal S, Williams AJ. The association between narcolepsy and REM behavior disorder (RBD) Sleep Med. 2005;6:253–8. doi: 10.1016/j.sleep.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 2nd edition. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 17.Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–9. doi: 10.1093/brain/123.2.331. [DOI] [PubMed] [Google Scholar]
- 18.Gjerstad MD, Boeve B, Wentzel-Larsen T, Aarsland D, Larsen JP. Occurrence and clinical correlates of REM sleep behaviour disorder in patients with Parkinson's disease over time. J Neurol Neurosurg Psychiatry. 2008;79:387–91. doi: 10.1136/jnnp.2007.116830. [DOI] [PubMed] [Google Scholar]
- 19.Seale C, Boden S, Williams S, Lowe P, Steinberg D. Media constructions of sleep and sleep disorders: A study of UK national newspapers. Soc Sci Med. 2007;65:418–30. doi: 10.1016/j.socscimed.2007.03.035. [DOI] [PubMed] [Google Scholar]
- 20.Nielsen T, Svob C, Kuiken D. Dream-enacting behaviors in a normal population. Sleep. 2009;32:1629–36. doi: 10.1093/sleep/32.12.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schenck CH, Mahowald MW. Subclinical REM sleep behavior disorder and its clinical and research implications. Sleep. 2008;31:1627. doi: 10.1093/sleep/31.12.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zozula R, Rosen RC, Jahn EG, Engel SH. Recognition of sleep disorders in a community-based setting following an educational intervention. Sleep Med. 2005;6:55–61. doi: 10.1016/j.sleep.2004.09.004. [Erratum appears in Sleep Med 2007 Mar;8:189 Note: Engel, Samuel H [added]] [DOI] [PubMed] [Google Scholar]
- 23.Bejot Y, Juenet N, Garrouty R, et al. Sexsomnia: an uncommon variety of parasomnia. Clin Neurol Neurosurg. 2010;112:72–5. doi: 10.1016/j.clineuro.2009.08.026. [DOI] [PubMed] [Google Scholar]
- 24.Stiasny-Kolster K, Mayer G, Schafer S, Moller JC, Heinzel-Gutenbrunner M, Oertel WH. The REM sleep behavior disorder screening questionnaire--a new diagnostic instrument. Mov Disord. 2007;22:2386–93. doi: 10.1002/mds.21740. [DOI] [PubMed] [Google Scholar]
- 25.Postuma RB, Gagnon JF, Vendette M, Fantini ML, Massicotte-Marquez J, Montplaisir J. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology. 2009;72:1296–300. doi: 10.1212/01.wnl.0000340980.19702.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med. 2009;5:235–9. [PMC free article] [PubMed] [Google Scholar]
- 27.Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD) J Clin Sleep Med. 2010;6:85–95. [PMC free article] [PubMed] [Google Scholar]
- 28.Daly JJ, Compton SA. Rapid eye movement (REM) sleep behaviour disorder; an easily missed diagnosis, a readily treatable condition. Ulster Med J. 2002;71:62–5. [PMC free article] [PubMed] [Google Scholar]
- 29.Boeve BF, Silber MH, Ferman TJ. Melatonin for treatment of REM sleep behavior disorder in neurologic disorders: results in 14 patients. Sleep Med. 2003;4:281–4. doi: 10.1016/s1389-9457(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 30.Kunz D, Mahlberg R. A two-part, double-blind, placebo-controlled trial of exogenous melatonin in REM sleep behaviour disorder. J Sleep Res. 2010;19:591–6. doi: 10.1111/j.1365-2869.2010.00848.x. [DOI] [PubMed] [Google Scholar]
- 31.Fetveit A, Bjorvatn B. [Sleep disorders in the elderly] Tidsskr Nor Laegeforen. 2009;129:2004–6. doi: 10.4045/tidsskr.08.0403. [DOI] [PubMed] [Google Scholar]