Abstract
Study Objectives:
To translate, back-translate and cross-language validate (English/Spanish) the Sleep Heart Health Study Sleep Habits Questionnaire for use with Spanish-speakers in clinical and research settings.
Methods:
Following rigorous translation and back-translation, this cross-sectional cross-language validation study recruited bilingual participants from academic, clinic, and community-based settings (N = 50; 52% women; mean age 38.8 ± 12 years; 90% of Mexican heritage). Participants completed English and Spanish versions of the Sleep Habits Questionnaire, the Epworth Sleepiness Scale, and the Acculturation Rating Scale for Mexican Americans II one week apart in randomized order. Psychometric properties were assessed, including internal consistency, convergent validity, scale equivalence, language version intercorrelations, and exploratory factor analysis using PASW (Version18) software. Grade level readability of the sleep measure was evaluated.
Results:
All sleep categories (duration, snoring, apnea, insomnia symptoms, other sleep symptoms, sleep disruptors, restless legs syndrome) showed Cronbach α, Spearman-Brown coefficients and intercorrelations ≥ 0.700, suggesting robust internal consistency, correlation, and agreement between language versions. The Epworth correlated significantly with snoring, apnea, sleep symptoms, restless legs, and sleep disruptors) on both versions, supporting convergent validity. Items loaded on 4 factors accounted for 68% and 67% of the variance on the English and Spanish versions, respectively.
Conclusions:
The Spanish-language Sleep Habits Questionnaire demonstrates conceptual and content equivalency. It has appropriate measurement properties and should be useful for assessing sleep health in community-based clinics and intervention studies among Spanish-speaking Mexican Americans. Both language versions showed readability at the fifth grade level. Further testing is needed with larger samples.
Citation:
Baldwin CM; Choi M; McClain DB; Celaya A; Quan SF. Spanish translation and cross-language validation of a Sleep Habits Questionnaire for use in clinical and research settings. J Clin Sleep Med 2012;8(2):137-146.
Keywords: Spanish translation/validation, sleep health disparities, psychometrics, Hispanic Mexican Americans, sleep habits and culture care
Sleep research over the past two decades has shown associations between sleep disorders and chronic disease,1–7 poorer health-related quality of life,8,9 increased health and work-related costs, and travel and work-related accidents.10,11 Prevalence rates for insomnia, the most commonly reported sleep complaint, range from 20% to 40% of the population, depending on the defined severity and frequency,12 and is suggested to have a bidirectional relationship with several chronic conditions including depression and cardiovascular disease.13,14 Prevalence rates for obstructive sleep apnea syndrome range from 2% to 4%,7 and rates for restless legs syndrome range from 5% to 15% in the general population.15 Snoring (48%), feeling unrested (26.5%), and insufficient sleep (26%) are leading sleep problems identified in a population-based study.5 These and other sleep disruptions can contribute to excessive daytime sleepiness,16 making sleep disorders significant contributors to disability, morbidity, and mortality.1,5,7,11,17,18
Despite the growing clinical and public health concerns regarding sleep disorders, few studies have examined associations between sleep and race/ethnicity in the United States. A majority of extant racial/ethnic studies compared African Americans with and without sleep disorders, or comparing African and Caucasian Americans on sleep disordered breathing, snoring, sleep architecture, insomnia symptoms, sleep quality, daytime sleepiness, comorbid conditions, and health-related quality of life.8,19–23 Recent reviews reported the need for studies of sleep among Hispanics.24,25 This research need is time-critical because Hispanic Americans (e.g., Cuban, Mexican, Puerto Rican) are the second largest and fastest growing minority group and currently constitute 15% of the population; Mexican Americans represent the largest subgroup, comprising 66.7% of the Hispanic American population.26 Many factors combine to make sleep disorders research a high priority among Hispanics in the United States. Hispanics experience the following: higher rates of unemployment and less earned income when employed; greater likelihood of living in poverty; less likelihood of graduating from high school; greater food insecurity; are under- or uninsured; reduced leisure-time physical activity; acculturation pressures, immigration bias, limited access to care, diverse cultural constructions of health and illness; and higher rates of chronic conditions, including obesity, type 2 diabetes, and hypertension.27,28 These factors are associated with disordered or disrupted sleep in other cultural and racial/ethnic groups; thus studying sleep in Hispanics should enrich the overall understanding of their social, emotional, and physical well-being.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Limited knowledge of sleep and health of Hispanics of Mexican descent, the largest Hispanic group in the United States, is partly due to the need for precisely translated and validated sleep measures to assess Spanish-speaking Mexican Americans in clinical and research settings.
Study Impact: This first-of-its-kind study to rigorously translate and cross-language validate the Sleep Heart Health Study Sleep Habits Questionnaire demonstrated conceptual and content equivalency and acceptable psychometric characteristics with items loading on 4 factors that accounted for 68% and 67% of the variance on the English and Spanish versions respectively. This Spanish-language version of the Sleep Habits Questionnaire may be applied in clinical and research settings as a first step toward addressing sleep health disparities of Spanish-speaking Mexican Americans.
A major issue in the adequate and appropriate assessment of sleep disorders of Hispanics is that of language.29 Spanish is the second most common language in the United States and is the primary language spoken at home by more than 34 million people aged 5 or older.26 Disparities in quality and access to care have reportedly been narrowing for all groups except Hispanics due, in part, to language barriers.30 The aim of this paper is to report the psychometrics of a rigorously translated, back-translated, and cross-language validated version of the Sleep Heart Health Study Sleep Habits Questionnaire.31 The development of the Spanish version was guided by Brislin's Translation Model to ensure that the instrument was linguistically and conceptually equivalent and suitable for use in clinical and research settings with Spanish-speaking Mexican Americans.32–34
METHODS
Participants
Translation and Back-Translation
Translators and back translators (N = 6) provided written informed consent (English and Spanish) prior to participating in the study and completed demographic information, including age, sex, race/ethnicity, years of education, current occupation and a questionnaire listing prior translation experience. Each translator was compensated $250 for their time.
Cross-Language Validation
Bilingual men and women volunteers (N = 50) were recruited by flyers posted in community, college and university settings, libraries, places of worship, community centers, and primary care clinics in neighborhoods with a high census of Mexican American/Hispanic residents. Participants completed demographic and health history data in English. English and Spanish versions of the Sleep Habits Questionnaire, the Epworth and an acculturation rating scale were completed 7 to 10 days apart in counterbalanced (randomized) order.35 Participants were provided written informed consent (English and Spanish) prior to participation and were compensated $30 for their time. All facets of this study were reviewed and approved by the university institutional review board.
Instruments
Demographics
Demographic information included age, sex, race/ethnicity, educational level, marital status, smoking status, alcohol, caffeine, prescription and other drug use, health history, and self-reported height and weight to calculate body mass index (BMI).
The Sleep Habits Questionnaire
The Sleep Habits Questionnaire was developed to survey Sleep Heart Health Study (SHHS) participants; a description of the study has been previously published.31 The Sleep Habits Questionnaire includes validated questions and response scales selected from the instruments of the Wisconsin Sleep Cohort Study36 and the Cleveland Family Study.37 The Cleveland study has demonstrated the validity and internal consistency of these questions among Caucasian and African American adults.38 The Sleep Habits Questionnaire includes instructions to complete it without discussing the questions with anyone, including a spouse. The questionnaire addresses several categories of sleep disorders examined in this study: (1) sleep duration (2 items); (2) snoring (3 items); (3) breathing pauses/apnea (4 items); (4) insomnia symptoms (3 items); (5) sleep symptoms, including insufficient sleep, daytime sleepiness, nightmares, leg jerks, leg cramps, and need for sleep aids (12 items); (6) sleep quality, including perception of depth and duration of sleep (3 items); and (7) restless legs syndrome (10 items). There is an additional category that assesses potential sleep disruptors, including sinusitis, room noise, temperature, pain, and frequent toileting (9 items).
The questionnaire can be used in its entirety for a comprehensive overview of subjective reports of sleep disorders, or in categories (e.g., snoring, insomnia symptoms, restless legs syndrome) for focused assessment in clinical and research settings. Snoring is ascertained by the question “Have you ever snored (now or at any time in the past)?” with possible responses “yes,” “no,” or “don't know.” Participants answering “yes” were asked, “How often do you snore now?” with possible responses including “rarely-less than one night a week,” “sometimes-1 or 2 nights a week,” “frequently-3 to 5 nights a week,” “always or almost always-6 or 7 nights a week,” or “don't know.” Breathing pauses during sleep are ascertained by the question, “Are there times when you stop breathing during sleep?” with possible responses “yes,” “no,” or “don't know,” or if a physician ever told them they have sleep apnea. Participants are also asked how often there is someone nearby while they are sleeping, with possible responses of “never,” “sometimes,” and “always.” The questionnaire includes “Sleep Symptoms” containing 2 somnolence statements, “Feel excessively (overly) sleepy during the day,” and “Feel unrested during the day, no matter how many hours of sleep you had,” as well as “Not getting enough sleep,” the insomnia statements, “Trouble falling asleep,” “Wake up during the night and have difficulty resuming sleep,” and “Wake up too early in the morning and be unable to resume sleep,” and “Bad dreams or nightmares,” rated on a 5-point scale from “Never” to “Almost Always.” These symptom questions have been widely used (e.g., the World Health Organization).39 Questions used to identify RLS were drawn from SHHS-29 and reflect NIH diagnostic criteria for the syndrome including description, frequency, time of day, active/at rest status, and degree of discomfort.40
Epworth Sleepiness Scale
The Epworth Sleepiness Scale is a validated self-completion tool that asks subjects to rate the likelihood of falling asleep in several common situations and was included with the sleep habits items.41 Sleepiness using the Epworth is assessed by the question, “What is the chance that you would doze off or fall asleep in each of the following situations?” followed by a list of 8 situations including “riding as a passenger in a car,” “watching TV,” and others. For each situation, possible responses include 4 ordinal categories ranging from “no chance” to “high chance.” The Epworth is a unitary scale, with a Cronbach α of 0.88 and test-retest reliability over 5 months of r = 0.82 in previous studies.41 The Epworth was used in tandem with the Sleep Habits Questionnaire to examine convergent validity. The Epworth measure, translated for this study in the same manner as the Sleep Habits Questionnaire, also demonstrated high reliability for the English (0.780) and Spanish (0.771) versions. The Spearman-Brown and intraclass coefficient for the English/Spanish translated Epworth demonstrated robust correlations as well (0.928 and 0.907, respectively).
Acculturation
Language serves as a general indicator of level of acculturation.28–30 The 30-item Acculturation Rating Scale for Mexican Americans II (ARSMA-II; English and Spanish versions) identifies language familiarity, usage, preference, ethnic identity, generation, reading, writing, cultural exposure, and ethnic interaction. It has an internal reliability of 0.88 and test-retest reliability of 0.72.42 Persons who score high in the “Traditional” category are more likely to identify with the Mexican culture, whereas persons with high scores in the “Assimilated” category identify more with the United States culture. High scores in the “Bicultural” category suggest the person identifies with both the Mexican and United States cultures.
Procedures
This English to Spanish translation of the Sleep Habits Questionnaire was guided by the adaptation of Brislin's Translation Model to address cultural and functional equivalence, to make the translation and validation process more efficient and to ensure the integrity of the process.32,33 Cultural equivalence implies similarity of meaning and construct relevance across cultures.34
The translation and validation model is displayed in Figure 1. In Step 1, 3 independent translations were made simultaneously in a blinded fashion from source (English) to target (Spanish) language by 3 bilingual health providers of Mexican heritage with Spanish as their first language. During Step 2, each target language version of the questionnaire was back-translated in a blinded fashion to the source language by 3 new volunteer bilingual health providers of Mexican heritage with Spanish as their first language. In Step 3, a team member whose first language was Spanish completed a content analysis of the translations and back-translations to aid in assuring credibility, trustworthiness, and transferability of translation. Where differences in meanings were identified in the back-translations, the principal investigator and bilingual team members met with the translators and back-translators involved in Steps 1 and 2 to review differences and adapt the target language version (Spanish) in order to achieve the most accurate culturally equivalent meanings. In Step 4, two additional native Spanish speakers independently back-translated the version of the questionnaire revised in Step 3. Because bilingual speakers and certified translators may introduce bias due to using and understanding languages differently than the population to be tested, the back-translators in Step 4 were lay people from local clinics who were more representative of the population under study. Blinded data were reviewed by lay bilingual experts to determine the need for linguistic adjustments based on early comments in this step. Step 5 consisted of a second meeting of the bilingual experts, who reviewed and compared the back-translations of the expert and lay translators. At this point, the team agreed on culturally equivalent meanings in both the English and Spanish language versions of the Sleep Habits Questionnaire. Step 6 assisted in assuring that both linguistic and cultural equivalence of translation was achieved (cross-language validation).43,44 During this step, bilingual participants completed English and Spanish language version packets 7 to 10 days apart in counterbalanced (randomized) order. These data were examined for psychometric properties of the rigorously translated instrument.
Figure 1.
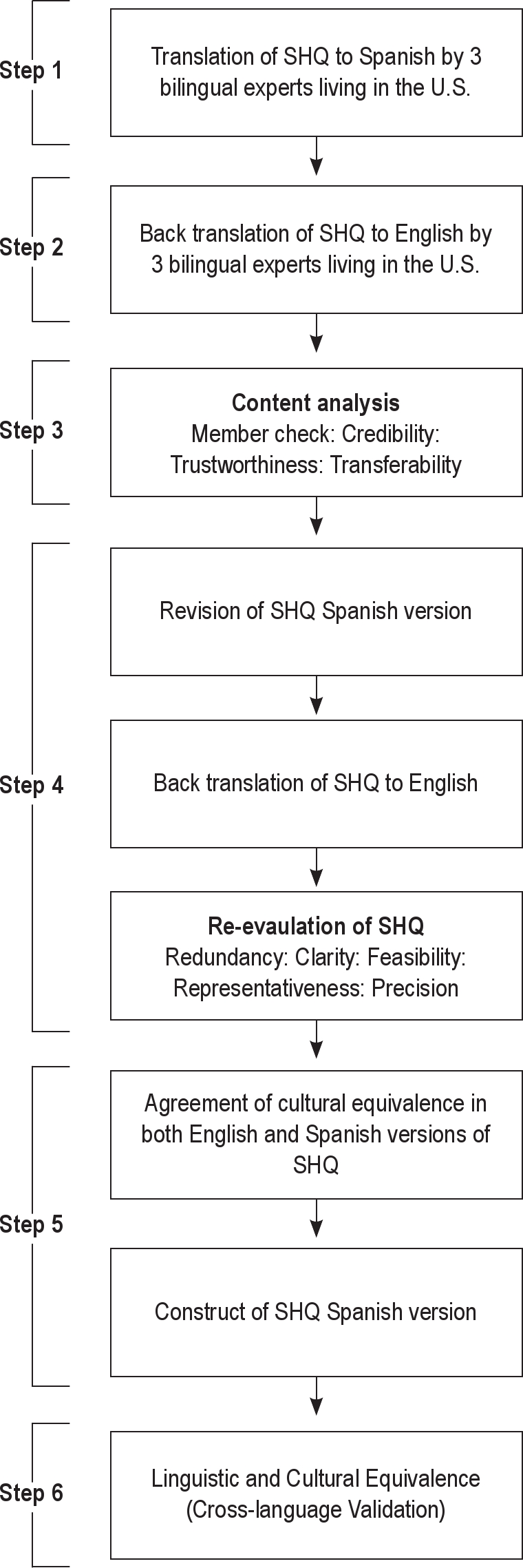
Flow chart for translation and validation of the spanish-translated SHHS SHQ
Readability Scoring
The Spanish translated instrument was assessed for grade level readability using the Huerta Reading Ease Score.45 Readability scores may range from 0 (most difficult) to 100 (least difficult) to read. Scores from 90 to 100 indicate very easy reading at an estimated 5th grade level; scores from 80 to 90 suggest easy reading at an estimated 6th grade level; while scores from 0 to 30 indicate very difficult reading at an estimated graduate college level.
Statistical Analyses
Differences in demographic and health history variables for the cross-language validation participants included analysis of variance for continuous variables and χ2 for nominal variables. Internal consistency reliability and conceptual equivalence were evaluated using Cronbach α, Spearman-Brown, and intraclass coefficients. We used a standardized item α to measure the Spearman-Brown coefficients. Intraclass coefficients are used for test-retest reliability to determine the stability between English and Spanish versions when sample size is small.46 Spearman-Brown and intraclass coefficients will approach 1.0 when there is no variance within items. Spearman-Brown and intraclass coefficients of 0.80 to 0.89 are considered adequate, while coefficients ≥ 0.90 suggest good reliability.46,47 A one-way random effects model was used for intraclass correlations, which conceptualizes each observed subject as a component of subject factor; therefore, the intraclass correlation is interpreted as the proportion of subject variance associated with differences among the scores of the subject. Inter-correlations among sleep variables were conducted using correlation coefficients to determine convergent validity with the Epworth Sleepiness Scale. The criterion level for coefficient α was set at ≥ 0.70 to retain an item in an adequate scale. Exploratory factor analysis utilized principal component analysis without rotation to reduce the number of items to validate item consistency between the 2 language versions. For exploratory purposes, analysis included communalities ≥ 0.400 to determine central factors.48,49 All data analyses were performed using PASW (Version 18).
RESULTS
Translator and Back-translator Participant Characteristics
All 6 translators were of Mexican American heritage with Spanish as their first language. Two men and one woman translated the Sleep Habits Questionnaire from English to Spanish; then 2 other women and one other man reverse-translated the questionnaire from Spanish back to English. Translators and back-translators were 19 to 55 years of age. Their current occupations included physician, nurse, clinic staff members who work with Spanish-speaking patients, and 2 certified hospital translators (one translator and one back-translator). The bilingual experts and lay translators who reviewed the final translated version were no-cost volunteers of Mexican descent with Spanish as their first language.
Cross-Language Validation Participant Characteristics
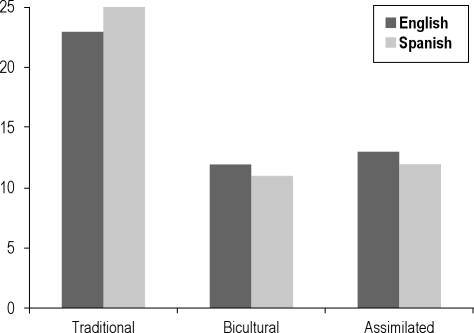
Characteristics of the cross-language validation participants are displayed in Table 1. Ethnic distribution for the bilingual participants (N = 50; 52% women; mean age 38.8 ± 12 years) showed 90% to be of Mexican origin, 4% Central or South American, and 6% non-Hispanic white. The mean education level was 14.9 ± 3.4 years. The range of 6 to 22 years for education suggests a broad sampling for educational achievement. The largest subgroups of participants (n = 23 on the English and n = 25 on the Spanish versions) scored in the “Traditional” category on the ARSMA II,42 suggesting strong identification with Mexican culture. The remainder of the participants (n = 12 and n = 11 on the English and Spanish versions, respectively) scored in the “Bicultural” category, indicating strong identification with the cultures of both Mexico and the United States, and “Assimilated” (n = 13 and n = 12 on the English and Spanish versions, respectively), indicating strong identification with United States culture. Given the higher levels of education seen in this predominantly Mexican American sample, education (as a proxy for socioeconomic status) and acculturation were stratified by sleep disorder categories (duration, snoring, apnea, insomnia symptoms, other sleep symptoms, restless legs, and sleep disruptors). Neither education nor acculturation differed significantly for any sleep category for either language version. Figure 2 portrays the number of participants in each acculturation category for English and Spanish. The acculturation differences between versions were not significant. Participants were also assessed for English and Spanish language fluency, including speaking, reading, writing, and comprehension (Table 2). The ratings ranged from 1 (poor) to 5 (excellent). All participants scored ≥ 4. In addition, a majority of participants reported having lived (n = 34) or studied (n = 26) in a Latin American country, predominantly Mexico.
Table 1.
Characteristics of the cross-language validation studied sample (N = 50)
| Sex, n (%) | |
| Male | 24 (48) |
| Female | 26 (52) |
| Age, years | |
| Mean ± SD | 38.8 ± 12.0 |
| Range | 20 – 62 |
| Education, years | |
| Mean ± SD | 14.9 ± 3.4 |
| Range | 6 – 22 |
| Marital Status, n (%) | |
| Married/Partnered | 34 (68) |
| Single/Divorced | 16 (32) |
| Race/Ethnicity, n (%) | |
| Hispanic (Mexican origin) | 45 (90) |
| Hispanic (Other Latin America) | 2 (4) |
| Non-Hispanic White (NHW) | 3 (6) |
Figure 2.
Acculturation between English (n = 48) and Spanish (n = 48) versions (number of participants in each category)
Table 2.
Language fluency for bilingual participants (N = 50) in the cross-language validation study
| Language Fluency | Scale (Mean ± SD) 1 = Poor to 5 = Excellent |
|---|---|
| English | |
| Speak | 4.52 ± 0.84 |
| Read | 4.48 ± 0.89 |
| Write | 4.34 ± 0.94 |
| Comprehend | 4.68 ± 0.68 |
| Spanish | |
| Speak | 4.62 ± 0.70 |
| Read | 4.40 ± 0.93 |
| Write | 4.00 ± 1.18 |
| Comprehend | 4.78 ± 0.51 |
| Years lived in a Spanish-speaking country (n = 34) | 13.9 ± 10.6 |
| Years studied in a Spanish-speaking country (n = 26) | 9.2 ± 8.0 |
Measurement Psychometrics
Internal consistency and correlation results for the Sleep Habits Questionnaire are displayed in Table 3. All sleep variables except sleep quality showed robust Cronbach α ≥ 0.700.46,47 The 3-item sleep quality category examines short versus long, light versus deep, and non-restful versus tranquil sleep on a 5-point Likert-type scale and showed a Cronbach α of 0.583 and 0.685 for the English and Spanish versions, respectively, suggesting moderate reliability. All categories of sleep variables for both language versions were highly correlated, with Spearman-Brown and intraclass correlations > 0.800, suggesting strong and comparable translation of the English to Spanish measures.46,47
Table 3.
Reliability of English and Spanish sleep scales
| Variables | Number of Items | English Cronbach α | Spearman-Brown Coefficient ξ | Intra-Class Coefficient φ | Spanish Cronbach α |
|---|---|---|---|---|---|
| Sleep Duration | 2 | 0.734 | 0.924 | 0.879 | 0.731 |
| Snoring | 3 | 0.849 | 0.934 | 0.916 | 0.896 |
| Apnea | 4 | 0.796 | 0.994 | 0.898 | 0.741 |
| Insomnia Symptoms | 3 | 0.730 | 0.926 | 0.880 | 0.777 |
| Sleep Symptoms | 12 | 0.824 | 0.915 | 0.911 | 0.838 |
| Sleep Quality | 3 | 0.583 | 0.901 | 0.813 | 0.685 |
| Sleep Disruptors | 9 | 0.778 | 0.874 | 0.858 | 0.707 |
| Restless Legs Syndrome | 10 | 0.900 | 0.931 | 0.943 | 0.890 |
Spearman-Brown Coefficient;
Intraclass Coefficient between English and Spanish versions.
Proportion of Participants Comprising English and Spanish Sleep Disorder Categories
Table 4 displays the proportion of cross-language validation participants with and without sleep disorders by categories. Proportions were consistent between English and Spanish language versions, respectively, for short (18% vs. 20%) and long (14% each) sleep duration on weekdays, short (4% vs. 2%) and long (40% vs. 44%) sleep duration on weekends, snoring (56% vs. 54%), sleep apnea (8% each), insomnia symptoms (24% each), sleep symptoms (22% vs. 26%), sleep quality (28% vs. 32%), and restless legs (10% vs. 12%).
Table 4.
Proportion of participants (N = 50) with and without sleep complaints on English and Spanish versions
| Sleep Categories# | English |
Spanish |
||
|---|---|---|---|---|
| Yes n (%) | No n (%) | Yes n (%) | No n (%) | |
| Sleep Duration | ||||
| Weekdays | ||||
| < 7 hours/night | 9 (18) | 10 (20) | ||
| ∼ 8 hours/night | 34 (68) | 33 (66) | ||
| ≥ 9 hours/night | 7 (14) | 7 (14) | ||
| Weekends | ||||
| < 7 hours/night | 2 (4) | 1 (2) | ||
| ~ 8 hours/night | 28 (56) | 27 (54) | ||
| ≥ 9 hours/night | 20 (40) | 22 (44) | ||
| Snoring | 28 (56) | 22 (44) | 27 (54) | 23 (46) |
| Sleep Apnea | 4 (8) | 46 (92) | 4 (8) | 46 (92) |
| Insomnia Symptoms | 12 (24) | 38 (76) | 12 (24) | 38 (76) |
| Sleep Symptoms | 11 (22) | 39 (78) | 13 (26) | 37 (74) |
| Sleep Quality+ | 13 (26) | 37 (74) | 15 (30) | 35 (70) |
| Sleep Disruptors^ | 14 (28) | 36 (72) | 16 (32 ) | 34 (68) |
| Restless Legs Syndrome | 5 (10) | 45 (90) | 6 (12) | 44 (88) |
| Daytime Somnolence (Epworth > 10) | 11 (22) | 39 (88) | 12 (24) | 38 (86) |
Numbers of items for each category are listed in Table 3. Yes = Presence of sleep disorder.
Poor to below average sleep quality.
Monthly to weekly disrupted sleep.
The means and standard deviations for the Epworth were 7.3 ± 4.8 (range 0-19) for the English version and 7.2 ± 4.5 (range 0-18) for the Spanish version. Proportions of participants with an Epworth score > 10 designating excessive daytime somnolence were 10% and 12% for the English and Spanish versions, respectively.
Convergent Validity Within and Between Language Versions
English Version Intercorrelations
Correlations for both language versions are displayed in Table 5. Correlations for the English language version are shown below the diagonal. For the English version, weekday sleep duration (average in h) was significantly negatively correlated with insomnia symptoms (r = −0.426, p < 0.01), sleep symptoms (r = −0.538, p < 0.01), sleep disruptors (r = −0.466, p < 0.01), and restless legs (r = −0.327, p < 0.05), and significantly positively correlated with sleep quality (r = 0.354, p < 0.05). Weekend sleep duration (in h) was negatively correlated with sleep symptoms (r = −304) and sleep disruptors (r = −328, each p < 0.05) and restless legs (r = −0.462, p < 0.01). Snoring was significantly positively correlated with apnea (r = 0.412, p < 0.01), sleep symptoms (r = 0.291, p < 0.05), and sleep disruptors (r = 0.306, p < 0.05). Apnea was negatively correlated sleep quality (r = −0.317, p < 0.05). Insomnia symptoms were positively correlated with other sleep symptoms (r = 0.805, p < 0.01), sleep disruptors (r = 0.675, p < 0.01), and restless legs (r = 0.403, p < 0.01), and negatively correlated with sleep quality (r = −0.401, p < 0.01). Sleep symptoms (e.g., insufficient sleep) were positively correlated with sleep disruptors (r = 0.824, p < 0.01) and restless legs (r = 0.540, p < 0.01) and negatively correlated with sleep quality (r = −405, p < 0.01). Sleep quality was negatively correlated with sleep disruptors (r = −0.347, p < 0.01). Sleep disruptors were positively correlated with restless legs (r = 0.586, p < 0.05) and negatively correlated with sleep quality (r = −347, p < 0.05).
Table 5.
Intercorrelations among sleep variables and comparisons with Epworth for convergent validity
| Sleep Duration (Weekdays) | Sleep Duration (Weekends) | Snoring | Apnea | Insomnia Symptoms | Sleep Symptoms | Sleep Quality | Sleep Disruptors | Restless Legs | Epworth | |
|---|---|---|---|---|---|---|---|---|---|---|
| Sleep Duration (Weekdays) | 1 | 0.581** | 0.012 | −0.226 | −0.399** | −0.426** | 0.415** | −0.334** | −0.233 | −0.161 |
| Sleep Duration (Weekends) | 0.593** | 1 | 0.068 | −0.180 | −0.295* | −0.301* | 0.295 | −0.269 | −0.411** | −0.068 |
| Snoring | −0.070 | −0.086 | 1 | 0.259 | 0.120 | 0.247 | −0.139 | 0.312* | 0.141 | 0.309* |
| Apnea | −0.087 | −0.208 | 0.412** | 1 | −0.030 | 0.189 | −0.319* | 0.243 | 0.204 | 0.356* |
| Insomnia Symptoms | −0.426** | −0.238 | 0.236 | 0.182 | 1 | 0.748** | −0.426** | 0.640** | 0.396** | 0.192 |
| Sleep Symptoms | −0.538** | −0.304* | 0.291* | 0.237 | 0.805** | 1 | −0.456** | 0.820** | 0.609** | 0.510** |
| Sleep Quality | 0.354* | 0.247 | −0.057 | −0.317* | −0.401** | −0.405** | 1 | −0.385* | −0.157 | −0.034 |
| Sleep Disruptors | −0.466** | −0.328* | 0.306* | 0.277 | 0.675** | 0.824** | −0.347** | 1 | 0.622** | 0.344* |
| Restless Legs | −0.327* | −0.462** | 0.199 | 0.265 | −0.403** | 0.540** | −0.100 | 0.586** | 1 | 0.303* |
| Epworth | −0.334* | −0.221 | 0.325* | 0.340* | 0.290* | 0.477** | 0.057 | 0.505** | 0.330* | 1 |
Bolded are significant between the Epworth and items from the Sleep Habits Questionnaire for construct validity.
Correlation is significant at the p < 0.05 level (2-tailed).
Correlation is significant at the p < 0.01 level (2-tailed). Correlations for English are below the diagonal and correlations for Spanish are above the diagonal.
Spanish Version Intercorrelations
Correlations for the Spanish language version are shown above the diagonal in Table 5. Weekday sleep duration (in h) was negatively correlated with insomnia symptoms (r = −0.399, p < 0.01), sleep symptoms (r = −0.426, p < 0.01), and sleep disruptors (r = −0.334, p < 0.05), and positively correlated with sleep quality (r = 0.415, p < 0.01). Weekend sleep duration was negatively correlated with insomnia symptoms (r = −0.295, p < 0.05), sleep symptoms (r = −0.301, p < 0.05), and restless legs (r = −0.411, p < 0.01), and positively correlated with sleep quality (r = 0.295, p < 0.01). Snoring was positively correlated with sleep disruptors (r = 0.312, p < 0.05). As with the English version, apnea was negatively correlated with sleep quality (r = −0.319, p < 0.05). Insomnia symptoms were positively correlated with other sleep symptoms (r = 0.748, p < 0.01), sleep disruptors (r = 0.640, p < 0.01), restless legs (r = 0.396, p < 0.01), and negatively correlated with sleep quality (r = −0.426, p < 0.01). Consonant with the English version, sleep symptoms were positively correlated with sleep disruptors (r = 0.820, p < 0.01) and restless legs (r = 0.609, p < 0.01) and negatively correlated with sleep quality (r = −456, p < 0.01); sleep disruptors were positively correlated with restless legs (r = 0.622, p < 0.01) and negatively correlated with sleep quality (r = −385, p < 0.01).
Approximately 87% (39 of 45) of the correlations between the English and Spanish versions were consistent in direction and magnitude of the relationships. Differences noted showed snoring to be negatively (English) and positively (Spanish) associated with weekend sleep duration; however, neither finding was significant. Snoring was significantly positively associated with apnea and sleep symptoms in English, while the Spanish version showed trends toward significance for apnea (r = 0.259, p = 0.07) and sleep symptoms (r = 0.247, p = 0.08).
Convergent Validity between Language Versions
The Epworth scale provided convergent validity for 5 of 8 of the sleep categories (63%) for both language versions. For the English and Spanish versions, respectively, the Epworth was significantly positively correlated with snoring (r = 0.325 and r = 0.309, each p < 0.05), apnea (r = 0.340 and r = 0.354, each p < 0.05), sleep symptoms (r = 0.477 and r = 0.510, each p < 0.01), sleep disruptors (r = 0.505, p < 0.01 and r = 0.344, p < 0.05), and restless legs (r = 0.330 and r = 0.303, each p < 0.05). The Epworth was also noted to be significantly negatively correlated with weekday sleep duration (r = −0.334, p < 0.05) and positively associated with insomnia symptoms (r = 0.290, p < 0.05) on the English, but not the Spanish versions; however the directions of the correlations for both versions were the same.
Construct Validity: Exploratory Factor Analysis
Exploratory factor analysis was conducted using principal components analysis without rotation that resulted in 4 factors. The factor loadings for items in the questionnaire are displayed in Table 6. Items 4 and 5 from each language version loaded on Factor 1 (Sleep Duration); Items 13, 14, 15 (Snoring) and 17, 18, 19 (Breathing Pauses/Apnea) loaded on Factor 2 (Snoring and Apnea); Items 21 a-e and h-j loaded on Factor 3 (Sleep Symptoms); Items 24 a-b, 25, 26, 27, 28, 29, 30, 30a, and 32 loaded on Factor 4 (Restless Legs). The bedtime, time to sleep, time arising in the morning, napping, reasons for napping, sleep quality, insufficient sleep, use of sleep aids, nightmares/bad dreams, sleep disruptors, age at onset of restless legs, and physician diagnosed restless legs did not centrally load on any of the factors. Based on these factor loadings, the structure of the Spanish version of the Sleep Habits Questionnaire is similar to the structure of the English version which supports construct validity across language. Categories included in Factors 2, 3, and 4 also correlated strongly with the Epworth Sleepiness Scale, which provided convergent validity. The Epworth was significantly negatively correlated with sleep duration on the English version, but not the Spanish version, or for weekend sleep duration on both language versions.
Table 6.
Exploratory factor analysis of the Sleep Habits Questionnaire in English and Spanish
| Factor Structure Item number and description | English | Spanish |
|---|---|---|
| Factor 1: Sleep Duration | ||
| #4 Hours of sleep during the week | −0.498 | −0.417 |
| #5 Hours of sleep on weekends | −0.535 | −0.493 |
| Factor 2: Snoring and Apnea | ||
| #13 Snoring frequency | 0.765 | 0.714 |
| #14 Snoring loudness | 0.776 | 0.662 |
| #15 Snoring over time | 0.640 | 0.432 |
| #17 Witnessed apnea | 0.711 | 0.586 |
| #18 Self-reported apnea | 0.802 | 0.613 |
| #19 Apnea frequency | 0.778 | 0.658 |
| Factor 3: Sleep Symptoms | ||
| #21a Difficulty falling asleep | 0.418 | 0.452 |
| #21b Difficulty staying asleep | 0.567 | 0.597 |
| #21c Awakening early with inability to resume sleep | 0.431 | 0.573 |
| #21d Un-refreshing (non-restorative) sleep | 0.503 | 0.559 |
| #21e Excessive daytime sleepiness | 0.400 | 0.606 |
| #21h Nasal stuffiness/obstruction at night | 0.467 | 0.588 |
| #21i Leg jerks | 0.754 | 0.775 |
| #21j Leg cramps | 0.577 | 0.598 |
| Factor 4: Restless Legs Syndrome (RLS) | ||
| #24a Urge to move legs | 0.841 | 0.836 |
| #24b Unpleasant/uncomfortable feelings in legs | 0.887 | 0.851 |
| #25 Frequency of symptoms | 0.857 | 0.823 |
| #26 Degree of discomfort from symptoms | 0.878 | 0.917 |
| #27 Activity when symptoms occur | 0.722 | 0.696 |
| #28 Symptoms worsen when reclining | 0.764 | 0.733 |
| #29 Symptoms improve when walking | 0.861 | 0.827 |
| #30 Time of day symptoms occur | 0.892 | 0.798 |
| #30a If day and night, worse at night | 0.406 | 0.524 |
| #32 Family history of symptoms | 0.640 | 0.637 |
Readability Scores for the Spanish-translated Sleep Habits Questionnaire
The Spanish-translated instrument was assessed in sections of sleep categories. Readability scores for the instrument were 89.1 (6th to near 5th grade reading level) for the snoring category, 91.7 for the sleep quality category, 95.7 for the for sleep duration category, 99.1 for the apnea category, and 99.7 each for the restless legs syndrome category and the Epworth Sleepiness Scale (all 5th grade reading level).45 Readability scores could not be calculated for the sleep items that address insomnia symptoms, sleep symptoms (e.g., unrefreshing sleep, leg jerks), or sleep disruptors (e.g., nighttime toileting, noise in the surroundings). These categories, arranged with Likert-type scales for frequency of symptoms, do not provide enough words or sentences with punctuation marks to allow for readability calculations.
DISCUSSION
Overall, the Spanish-translated version of the Sleep Habits Questionnaire demonstrated acceptable psychometric characteristics. Both language versions showed high levels of content validity and conceptual equivalency. The rigorous translation process and review of the Spanish version by experts found the items and content to be conceptually similar to the English version. The Spearman-Brown and intraclass correlation coefficients, which measure the homogeneity of the scales, indicated strong correlation and agreement between language versions. The Epworth provided convergent validity for a majority of sleep categories on both language versions, and exploratory factor analyses provided construct validity across language. Thus, the Sleep Habits Questionnaire is suitable for use with clinic patients and in community-based studies that examine various categories of self-identified sleep disorders.
All Sleep Habits Questionnaire categories except for sleep quality demonstrated strong internal consistency reliability for both language versions, ranging from 0.734 (English) and 0.731 (Spanish) for the 2-item sleep duration variable to 0.900 (English) and 0.890 (Spanish) for the 10 restless legs items. The 3-item sleep quality category that assessed perception of length, depth, and satisfaction with sleep showed only moderate internal consistency for the English (0.583) and Spanish (0.685) versions. The quality of sleep items are determined by using a 5-point scale with short/long, light/deep, and poor/good anchors. This scaling feature may not provide enough definition or information for persons whose first language is not English to respond adequately to these items. Future studies will need to examine these items with additional bilingual and Spanish-only speakers to determine if the psychometrics for the sleep quality items remain consistent or fluctuate with other groups. Nevertheless, the coefficients between language versions are robust, suggesting good correlation and agreement. Furthermore, the readability scores45 suggest that each of the sleep categories, as well as the Epworth, are suitable to a fifth- to sixth-grade reading level. Translation issues and years of schooling have been posited as barriers to adequate health assessment of Spanish-speaking Hispanics in the United States.27–29
Proportions of participants with the presence of sleep disorders by categories showed consistency in reporting between language versions. Percentages of participants who report sleep disorders provide a foundation for prevalence rates among Spanish-speaking Mexican Americans. A majority of these rates are consistent with population studies undertaken in the United States, including the rates for insomnia symptoms, weekday short sleep duration, and, in particular, the high rates for snoring among the Hispanics in this study with Hispanics in other studies.4,5,8,16,24,25 Age, education, and acculturation category were not significantly associated with any of the sleep categories. Future studies will need to determine if these and other socioeconomic status variables, including naturalization or U.S.-born status,50 may play roles in the type and severity of sleep disorder category among Mexican American Hispanics.
Intercorrelations for both language versions show similar and consistent relationships and directions among variables that support what might be expected in clinical and research settings for persons with sleep disturbances, suggesting good criterion validity. For example, persons who snore would be more likely to have apnea and report daytime sleepiness (positive correlations). Persons who experience more sleep disruption due to noisy nighttime environment, pain, or the need for frequent toileting would be more likely to report shorter weekday and weekend sleep durations and poor sleep quality (negative correlations) and greater reports of insomnia symptoms, other sleep symptoms, and daytime somnolence (positive correlations). Likewise, significant correlations between the Epworth with the sleep symptoms, sleep disruptors, restless legs, and, in particular, the snoring and apnea categories on both language versions support the convergent validity of the Spanish-translated measure. Notably, the comprehensiveness of this questionnaire relevant to the number and type of sleep categories have identified variables and their direction for both English and Spanish speakers that can be examined in future clinical and research studies. These covariates include insomnia symptoms, other sleep symptoms (e.g., insufficient or unrefreshing sleep), restless legs, daytime somnolence, and sleep disruptors.
Reasons for the limited number of English and Spanish variables (6 of 45) that did not significantly correlate are not known, but the lack of power due to the small sample size may have contributed to the lack of significance. In addition, there may have been unexpected circumstances that could have affected these few correlations. For example, snoring showed a positive correlation in English and a negative correlation in Spanish with weekend sleep duration. Weekend events or changes in weekend activities might possibly have influenced differences in snoring responses during the 7- to 10-day time frame. Future studies of this sort will need to include a brief question regarding change in lifestyle habits in repeated measures studies.
Items in the Spanish version loaded on the same factors in the English version (Sleep Duration, Snoring and Apnea, Sleep Symptoms, and Restless Legs). The four factors explained 68% of the variance on the English version and 67% of the variance on the Spanish version. Loadings for inclusion in this exploratory factor analysis were set at ≥ 0.400 to determine central factors, while loadings > 0.600 are considered high.48,49 Findings from this analysis suggest strong loadings for the measured variables most associated with each of the four extracted factors. Factor loadings and variance accounted for are consistent between language versions, supporting the construct validity between the English and Spanish versions.
Limitations
Limitations to this study include sample size and bilingual Spanish speakers of predominantly Mexican heritage residing in the Southwest. This sample of 50 bilingual volunteers is sufficient for initial analyses of reliability and validity, but is not adequate to demonstrate the critical relationships between sleep health and other comorbid conditions that should be studied in the Hispanic population. The design of a cross-language validation study is not appropriate for establishing the test-retest reliability of the Spanish version, providing normative data, or assessing cultural equivalence across other Spanish-speaking ethnic groups from Central and South America, Cuba, and Puerto Rico. Education and acculturation, included as a prelude to examining sociocultural factors on the development of this Spanish language version did not have an impact on the sleep categories for either language version. Future studies will need to examine if these and other socioeconomic, immigration, and access to care factors may be linked to type and severity of sleep disorder category among Mexican American Hispanics.50
Acculturation status, age, and recruitment locations (clinics, community-based neighborhood centers and programs, and academic milieus) suggest the participants are representative of the general Mexican American population residing in Maricopa County, Arizona, who are clinic patients or would participate in community-based research studies. Notably, however, the high educational achievement reflected in their mean years of education (14.9) is not representative of academic levels generally seen among Mexican Americans (10th grade).27–29 Nevertheless, their range of education (6 to 22 years) suggests that the translated measure is relevant to a broad span of Spanish-speaking learners with a minimum of sixth grade education. These shortcomings will need to be addressed in future studies to determine the settings and populations in which use of the new instrument is most appropriate. Future studies will also need to determine item equivalence with confirmatory factor analysis.
Summary
This study examined the psychometric properties of the English to Spanish translated, back-translated, and cross-language validated Sleep Habits Questionnaire with bilingual community-dwelling adults predominantly of Mexican American heritage with Spanish as their first language. Results demonstrate that the Sleep Habits Questionnaire is a psychometrically sound measure with robust correlations within and between language versions for a broad range of subjective sleep disorder categories that can be self-administered in community and clinic settings. The Epworth provided convergent validity for the snoring, apnea, sleep symptoms, restless legs, and sleep disruptors categories, while loadings from exploratory factor analysis supported the structure of both English and Spanish versions of the instrument. The English version of the Sleep Habits Questionnaire has been used ubiquitously in clinical and population-based studies. Findings indicate that the Spanish-language version has robust and appropriate measurement properties and may be useful for assessing sleep health in community-based and intervention studies among Spanish speakers residing in the Southwest.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors gratefully acknowledge Mary Z. Mays, Ph.D. and Janice Jirsak, M.S. for data coordination and data integrity. Funding: NIH Grant #1R03HD051678 and, in part, the ASU CONHI Dean's Research Award.
REFERENCES
- 1.Baldwin CM, Bell IR, Guerra S, Quan SF. Obstructive sleep apnea and ischemic heart disease in southwestern U.S. veterans: Implications for clinical practice. Sleep Breath. 2005;9:111–8. doi: 10.1007/s11325-005-0025-y. [DOI] [PubMed] [Google Scholar]
- 2.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–8. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- 3.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: The Sleep Heart Health Study. Sleep. 2006;29:1009–14. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 4.Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ram S, Seirawan H, Kumar SK, Clark GT. Prevalence and impact of sleep disorders and sleep habits in the United States. Sleep Breath. 2009;14:63–70. doi: 10.1007/s11325-009-0281-3. [DOI] [PubMed] [Google Scholar]
- 6.Winkelman JW, Shahar E, Sharief I, Gottlieb DJ. Association of restless legs syndrome and cardiovascular disease in the Sleep Heart Health Study. Neurology. 2008;70:35–42. doi: 10.1212/01.wnl.0000287072.93277.c9. [DOI] [PubMed] [Google Scholar]
- 7.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 8.Baldwin CM, Ervin A, Mays MZ, et al. Sleep disturbances, quality of life and ethnicity: The Sleep Heart Health Study. J Clin Sleep Med. 2010;6:176–83. [PMC free article] [PubMed] [Google Scholar]
- 9.Winkelman JW, Redline S, Baldwin CM, Resnick HE, Newman AB, Gottlieb DJ. Polysomnographic and health-related quality of life correlates of restless legs syndrome in the Sleep Heart Health Study. Sleep. 2009;32:772–8. doi: 10.1093/sleep/32.6.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, Lerner D. The cost of poor sleep: Workplace productivity loss and associated costs. J Occup Environ Med. 2010;52:91–8. doi: 10.1097/JOM.0b013e3181c78c30. [DOI] [PubMed] [Google Scholar]
- 11.Colten HR, Altevogt BM. Washington, DC: National Academic Press; 2006. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. [PubMed] [Google Scholar]
- 12.Leger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010;14:379–89. doi: 10.1016/j.smrv.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Phillips B, Mannino D. Correlates of sleep complaints in adults: the ARIC Study. J Clin Sleep Med. 2005;2:277–83. [PubMed] [Google Scholar]
- 14.Szklo-Coxe M, Young T, Peppard PE, Finn LA, Benca RM. Prospective associations of insomnia markers and symptoms with depression. Am J Epidemiol. 2010;171:709–20. doi: 10.1093/aje/kwp454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Partinen M, Hublin C. Philadelphia: Elsevier Saunders; 2005. Epidemiology of sleep disorders. [Google Scholar]
- 16.Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: The role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90:4510–5. doi: 10.1210/jc.2005-0035. [DOI] [PubMed] [Google Scholar]
- 17.Quan SF, Wright R, Baldwin CM, et al. Obstructive sleep apnea-hypopnea and neurocognitive functioning in the Sleep Heart Health Study. Sleep Med. 2006;7:498–507. doi: 10.1016/j.sleep.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Durrence HH, Lichstein KL. The sleep of African Americans: a comparative review. Behav Sleep Med. 2006;4:29–44. doi: 10.1207/s15402010bsm0401_3. [DOI] [PubMed] [Google Scholar]
- 20.Fiorentino L, Marler M, Stepnowski C, Johnson S, Ancoli-Israel S. Sleep in older African Americans and Caucasians at risk for sleep-disordered breathing. Behav Sleep Med. 2006;4:164–78. doi: 10.1207/s15402010bsm0403_3. [DOI] [PubMed] [Google Scholar]
- 21.Hale L, Do P. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Redline S, Kirchner L, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2009;164:406–18. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- 23.Scofield H, Roth T, Drake C. Periodic limb movements during sleep: Population prevalence, clinical correlates and racial differences. Sleep. 2008;31:1221–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Baldwin CM, Reynaga-Ornelas L, Caudillo-Cisneros C, Marquez-Gamino S, Quan SF. Overview of sleep disorders among Latinos in the United States. Hisp Health Care Int. 2010;8:180–7. [Google Scholar]
- 25.Loredo JS, Soler X, Bardwell W, Ancoli-Israel S, Dimsdale JE, Palinkas LA. Sleep health in U.S. Hispanic population. Sleep. 2010;33:962–7. doi: 10.1093/sleep/33.7.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Census Bureau. Selected social characteristics in the United States: 2007. [Accessed September 27, 2010]. http://factfinder.census.gov/servlet/ADPTable?_bm=y&geo_id=01000US&-qr_name=ACS_2007_1YR_G00_DP2&-context=adp&-ds_name=ACS_2007_1YR_G00_&-tree_id=306&-_lang=en&-redoLog=false&-format.
- 27.Escarce JJ, Morales LS, Rumbaut RG. The health status and health behaviors of Hispanics. In: Tienda M, Mitchell F, editors. National Research Council: Hispanics and the future of America. Washington, DC: National Academies Press; 2006. pp. 362–409. [Google Scholar]
- 28.Gresenz CR, Rogowski J, Escarce JJ. Community demographics and access to health care among U.S. Hispanics. Health Serv Res. 2009;44:1542–62. doi: 10.1111/j.1475-6773.2009.00997.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among U.S. Hispanics. Am J Pub Health. 2008;98:2021–8. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Research and Quality (AHRQ 2006) AHRQ 2005 National Healthcare Quality and Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; Retrieved September 14, 2010 from http://www.qualitytools.ahrq.gov. [Google Scholar]
- 31.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: Design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 32.Brislin RW. The wording and translation of research instruments. In: WL Lonner WL, Berry JW, editors. Field methods in cross-cultural research. Newbury Park, CA: Sage; 1986. pp. 17–164. [Google Scholar]
- 33.Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An adaptation of Brislin's Translation Model for cross-cultural research. Nurs Res. 2001;50:300–4. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Phillips LR, de Hernandez IL, de Ardon ET. Strategies for achieving cultural equivalence. Res Nurs Health. 1994;17:149–54. doi: 10.1002/nur.4770170210. [DOI] [PubMed] [Google Scholar]
- 35.Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Thousand Oaks, CA: Sage; 1996. Outcome measures for health education and other health care interventions. [Google Scholar]
- 36.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. New Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 37.Redline S, Kump K, Tishler PV, Browner I, Ferrette V. Gender differences in sleep disordered breathing in a community-based sample. Am J Respir Crit Care Med. 1993;149:722–6. doi: 10.1164/ajrccm.149.3.8118642. [DOI] [PubMed] [Google Scholar]
- 38.Kump K, Whalen C, Tishler PV, et al. Assessment of the validity and utility of a sleep-symptom questionnaire. Am J Respir Crit Care Med. 1994;150:735–41. doi: 10.1164/ajrccm.150.3.8087345. [DOI] [PubMed] [Google Scholar]
- 39.Zielinski J, Zgierska A, Polakowska M, et al. Snoring and excessive daytime somnolence among Polish middle-aged adults. Eur Respir J. 1999;14:946–50. doi: 10.1034/j.1399-3003.1999.14d36.x. [DOI] [PubMed] [Google Scholar]
- 40.Allen RP, Picchietti D, Hening WA, Trenkwalder C, Walters AS, Montplaisir J Restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–19. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 41.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 42.Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans II: a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;17:275–304. [Google Scholar]
- 43.Willis G. Overview of methods for developing equivalent measures across multiple cultural groups. In: Cohen SB, Lepkowski JM, editors. Eighth Conference on Health Survey Research Methods. Hyattsville, MD: National Center for Health Statistics; 2004. pp. 91–6. [Google Scholar]
- 44.Harkness JA. Problems in establishing conceptually equivalent health definitions across multiple cultural groups. In: Cohen SB, Lepkowski JM, editors. Eighth Conference on Health Survey Research Methods. Hyattsville, MD: National Center for Health Statistics; 2004. pp. 85–90. [Google Scholar]
- 45.Accessibility Institute, the University of Texas at Austin. TxReadability from the Accessibility Institute a multi-language readability tool. [Accessed July 28, 2008]. http://webapps.lib.utexas.edu/TxReadability/app.
- 46.Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–5. doi: 10.1002/sim.1108. [DOI] [PubMed] [Google Scholar]
- 47.Nunnally JC, Bernstein IM. New York: McGraw-Hill; 1994. Psychometric theory. [Google Scholar]
- 48.Pett M, Lackey NR, Sullivan JJ. Thousand Oaks, CA: Sage; 2003. Making sense of factor analysis: the use of factor analysis for instrument development in health care research. [Google Scholar]
- 49.Raubenheimer JE. An item selection procedure to maximize scale reliability and validity. So African J Indust Psychol. 2004;30:59–64. [Google Scholar]
- 50.Seicean S, Neuhauser D, Strohl K, Redline S. An exploration of differences in sleep characteristics between Mexico-born US immigrants and other Americans to address the Hispanic Paradox. Sleep. 2011;34:1021–31. doi: 10.5665/SLEEP.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]