Abstract
Study Objectives:
Sleep apnea has been implicated as an independent risk factor for atherosclerotic coronary artery disease (CAD). An association between the severity of sleep apnea and total cholesterol levels has previously been reported. However, the association with small dense low density lipoprotein (LDL) cholesterol concentration (subclass B), one of the strongest predictors of atherosclerosis, is unknown. We examined the relationship between sleep apnea and LDL subclass B, considering body size.
Methods:
This is a cross-sectional observational cohort of participants enrolled in a cardiovascular health study. Sleep apnea was assessed with a validated portable monitor. Lipid panels included total cholesterol, triglycerides, high density lipoprotein cholesterol, LDL cholesterol, and LDL subclasses A, B, and A/B. Sleep apnea was analyzed categorically using the apnea hypopnea index (AHI).
Results:
A total of 519 participants were evaluated. Mean age was 58.7 ± 7.4 years; BMI was 29.6 ± 5.7; 65% were female; 59% were Caucasian, and 37% were African American. Among participants with abnormal waist circumference by ATP III criteria, moderate to severe sleep apnea (AHI ≥ 25) was not independently associated with LDL subclass B. In contrast, among participants with normal waist circumference, moderate to severe sleep apnea was associated with 4.5-fold odds of having LDL subclass B.
Conclusions:
Sleep apnea is independently associated with an atherogenic phenotype (LDL subclass B) in non-obese individuals. The association between sleep apnea and LDL subclass B in those with normal waist circumference may account, in part, for the increased risk of atherosclerosis and subsequent vascular events.
Citation:
Luyster FS; Kip KE; Drumheller OJ; Rice TB; Edmundowicz D; Matthews K; Reis SE; Strollo PJ. Sleep apnea is related to the atherogenic phenotype, lipoprotein subclass B. J Clin Sleep Med 2012;8(2):155-161.
Keywords: Sleep apnea, atherosclerosis, lipoproteins, phenotype
Sleep apnea has been implicated as an independent risk factor for atherosclerotic coronary artery disease (CAD), stroke, and myocardial infarction.1–3 An association between the severity of sleep apnea and traditional lipid levels has previously been reported.4,5 Small, dense low-density lipoprotein cholesterol concentration (LDL subclass B), is an emerging strong risk factor for atherosclerosis.6 The relationship between LDL subclass B and sleep apnea has not previously been examined.
We hypothesized that sleep apnea would be associated with an atherogenic lipoprotein phenotype, i.e., LDL subclass B, in a community cohort. Our secondary hypothesis was that the effects would be stronger among those who had a normal waist circumference relative to those with an increased waist circumference. We anticipated that the effect of sleep apnea would be masked or minimized among those with increased waist circumference due to the known effects of obesity on lipid profiles.7 Data were stratified by waist circumference as opposed to body mass index (BMI) because of the better correlation of waist circumference to visceral obesity than BMI.8,9
BRIEF SUMMARY
Current Knowledge/Study Rationale: Sleep apnea is known to be associated with atherosclerotic risk. In order to better understand this risk in a community cohort, we examined the relationship of sleep apnea to a known risk factor for atherosclerosis – low density lipoprotein cholesterol (LDL) subclass B.
Study Impact: The atherogenic phenotype LDL subclass B may be an important modifiable therapeutic target in sleep apnea patients. Further research is needed to assess the impact of sleep apnea treatment on LDL subclass B and subsequent atherosclerosis.
METHODS
Study Population
Participants were recruited from a community-based participatory research program, Heart Strategies Concentrating On Risk Evaluation (Heart SCORE) designed to examine the differential effects of race and gender on cardiovascular risk in 2,000 participants, with approximately equal representation of blacks and whites.
Eligibility criteria included age 45 to 75 years, residence in the greater Pittsburgh metropolitan area, ability to undergo baseline and annual follow-up visits, and absence of known comorbidity expected to limit life expectancy to < 5 years. The present analysis is based on 519 participants enrolled in Heart SCORE who participated in a substudy protocol to assess sleep apnea using a portable monitor. Participants in this substudy were not substantially different from participants in the larger study with regards to cardiac and metabolic risk (see Table S1 in the supplement). The design of the study was cross-sectional and observational. The institutional review board at the University of Pittsburgh Medical Center approved the study protocol, and all study participants provided written informed consent.
Data Collection
Detailed demographic and medical histories were collected at the baseline visit. Race and ethnicity were self-reported. A medical history included inquiries about a history of previously diagnosed hypertension, hyperlipidemia, and diabetes mellitus, as well as current medications. Lifestyle characteristics including smoking history, as defined by current or former (> 6 months ago) cigarette use, and use of alcohol were measured by self-developed questionnaires. Physical activity was assessed by the Lipid Research Clinics Questionnaire.10 Physical examination included measurement of vital signs and anthropometric measures of body fat distribution, including waist circumference and waist-to-hip ratio.11 Height and weight were measured to calculate BMI.
Hypertension was defined as either a systolic blood pressure ≥ 140 mm Hg or use of antihypertensive medications. Diabetes mellitus was defined as fasting glucose > 126 mg/dL or a history of previously diagnosed diabetes treated with diet, oral agents, and/or insulin. The metabolic syndrome and individual component abnormalities were defined according to criteria established by the National Cholesterol Education Program.12 This included abnormal waist circumference, defined as ≥ 88 cm for females and ≥ 102 cm for males.
Lipid Testing
Lipid panels included measurement of total cholesterol, triglycerides, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol (calculated). Laboratory assessment of lipoprotein levels and particle sizes was performed on venous blood drawn in the fasting state. Lipid levels and lipoprotein particle sub-fractions were quantified by a commercial laboratory using a vertical auto profile technique (VAP, Atherotech, Birmingham, AL).13,14 These samples were also labeled as patterns A, A/B, and B according to LDL max time value, which increases as the density of LDL peak increases.14 LDL max times of LDL patterns are as follows: LDL pattern B, ≥ 115 seconds; LDL pattern A, ≥ 118 seconds; and LDL pattern A/B, between 115 and 118 seconds.
Evaluation of Sleep Apnea
Sleep apnea was assessed with a previously validated portable monitor that measures airflow and snoring via a nasal pressure signal (ApneaLink, ResMed Corp).15,16 An apnea was defined as a decrease in airflow of ≥ 80% from baseline for ≥ 10 seconds. A hypopnea was defined as a decrease in airflow between > 30% and < 80% from baseline for ≥ 10 seconds. Sleep apnea was analyzed categorically using the apnea-hypopnea index (AHI): 0-4, 5-9, 10-14, 15-24, and ≥ 25 events/hour.
Statistical Analysis
The Wilcoxon Rank Sum test was used to compare the distribution of AHI scores between participants with normal versus abnormal waist circumference. Using AHI scores categorized into 5 groups (0-4, 5-9, 10-14, 15-24, ≥ 25), baseline demographic and clinical characteristics were compared by linear tests of trend. This included contrast statements within general linear models for continuous variables and the Mantel-Haenszel ?2 test for trend. To evaluate the independent relationship between AHI scores (continuous) and lipids, multiple linear regression analysis was used to estimate partial correlation coefficients. To estimate the independent relationship between AHI scores (categorized) and presence versus absence of LDL subclass B, logistic regression analysis was used. In both multivariable analyses, covariates selected for adjustment included those associated with AHI scores and/or considered to be biologically relevant. The statistical interaction between waist circumference (normal versus abnormal) and AHI score (categorized) was tested (p = 0.07). Since the interaction was not significant, analyses were stratified by normal versus abnormal waist circumference (normal waist circumference < 88 cm for females and < 102 cm for males). Stratified analyses using BMI < 30 versus ≥ 30 resulted in similar estimates to normal versus abnormal waist circumference, and are not presented herein. All analyses were performed using the SAS System, version 9.0 (SAS Institute, Cary, NC).
RESULTS
Baseline Characteristics
The mean age of the study population was 58.7 ± 7.4 years, and BMI was 29.6 ± 5.7 (Table 1). The participants were primarily females (65%), with more Caucasians (59%) than African Americans (37%) in the population. Factors associated with higher AHI scores included older age, male gender, higher body mass (kg/m2) and systolic blood pressure (mm Hg), lower HDL cholesterol (mg/dL), and presence of the metabolic syndrome or diabetes. Despite 26% of the population having AHI scores indicative of moderate to severe sleep apnea, only 6% of the participants reported being diagnosed with any sleep disorder.
Table 1.
Baseline characteristics of study cohort by AHI score*
| Baseline Characteristic | All Participants | AHI Score |
p-trend | ||||
|---|---|---|---|---|---|---|---|
| 0 to 4 | 5 to 9 | 10 to 14 | 15 to 24 | 25 or more | |||
| (n = 519) | (n = 166) | (n = 138) | (n = 78) | (n = 75) | (n = 62) | ||
| Age (years) | 58.7 ± 7.4 | 56.8 ± 7.3 | 58.3 ± 7.3 | 59.0 ± 7.3 | 59.7 ± 6.9 | 62.9 ± 6.6 | < 0.0001 |
| Race | 0.92 | ||||||
| White | 58.8% | 57.2% | 58.7% | 59.0% | 61.3% | 59.7% | |
| Black | 37.4% | 39.2% | 38.4% | 38.5% | 33.3% | 33.9% | |
| Other | 3.8% | 3.6% | 2.9% | 2.6% | 5.3% | 6.4% | |
| Female gender | 64.7% | 75.9% | 68.8% | 71.8% | 48.0% | 37.1% | < 0.0001 |
| Smoking status | 0.96 | ||||||
| Current smoker | 7.9% | 8.4% | 8.7% | 5.1% | 8.0% | 8.1% | |
| Former smoker | 40.3% | 33.7% | 49.3% | 43.6% | 33.3% | 41.9% | |
| Never smoker | 51.8% | 57.8% | 42.0% | 51.3% | 58.7% | 50.0% | |
| Body mass index (kg/m2) | 29.6 ± 5.7 | 28.2 ± 5.7 | 29.6 ± 5.1 | 30.9 ± 5.3 | 30.6 ± 6.8 | 30.6 ± 5.1 | 0.002 |
| Systolic blood pressure (mm Hg) | 136 ± 19 | 132 ± 20 | 136 ± 19 | 137 ± 18 | 139 ± 19 | 140 ± 19 | 0.004 |
| Diastolic blood pressure (mm Hg) | 81 ± 11 | 79 ± 10 | 81 ± 10 | 83 ± 10 | 84 ± 11 | 82 ± 12 | 0.03 |
| Resting pulse (per minute) | 62 ± 10 | 61 ± 10 | 62 ± 9 | 64 ± 9 | 63 ± 12 | 61 ± 9 | 0.74 |
| Pulse pressure (mm Hg) | 55 ± 14 | 53 ± 15 | 55 ± 14 | 55 ± 15 | 55 ± 14 | 58 ± 13 | 0.03 |
| History of hyperlipidemia | 46.7% | 42.9% | 44.9% | 53.9% | 48.0% | 50.0% | 0.20 |
| Total cholesterol (mg/dL) | 215 ± 42 | 220 ± 42 | 214 ± 39 | 219 ± 44 | 207 ± 37 | 208 ± 49 | 0.03 |
| LDL cholesterol (mg/dL) | 143 ± 35 | 146 ± 35 | 141 ± 33 | 148 ± 41 | 139 ± 31 | 141 ± 40 | 0.32 |
| HDL cholesterol (mg/dL) | 58 ± 15 | 62 ± 17 | 60 ± 14 | 57 ± 15 | 54 ± 13 | 53 ± 14 | < 0.0001 |
| Triglycerides (mg/dL) | 122 ± 80 | 118 ± 82 | 112 ± 67 | 136 ± 111 | 129 ± 61 | 131 ± 71 | 0.01** |
| Glucose (mg/dL) | 97 ± 22 | 96 ± 19 | 97 ± 24 | 102 ± 28 | 94 ± 15 | 99 ± 17 | 0.47** |
| ATP3 criteria (% abnormal) | |||||||
| Waist circumference | 50.5% | 41.1% | 52.2% | 68.8% | 54.9% | 43.6% | 0.14 |
| Triglycerides | 26.6% | 25.2% | 19.6% | 29.5% | 34.7% | 32.3% | 0.05 |
| HDL cholesterol | 18.4% | 18.4% | 11.6% | 25.6% | 20.0% | 22.6% | 0.19 |
| Blood pressure | 64.1% | 52.4% | 60.9% | 73.1% | 73.0% | 80.6% | < 0.0001 |
| Glucose | 14.7% | 15.1% | 10.9% | 18.2% | 16.2% | 16.4% | 0.51 |
| Metabolic Status (ATP3) | |||||||
| Normal | 70.9% | 76.3% | 77.9% | 61.8% | 64.3% | 60.7% | |
| Metabolic syndrome | 19.6% | 17.3% | 14.7% | 22.4% | 27.1% | 24.6% | |
| History of diabetes | 9.4% | 6.4% | 7.4% | 15.8% | 8.6% | 14.7% | |
| History diagnosed sleep disorder | 6.4% | 4.8% | 6.5% | 2.6% | 9.3% | 11.3% | 0.08 |
| Medications in past 48 hours | |||||||
| Aspirin | 34.2% | 34.3% | 26.8% | 34.6% | 40.0% | 42.6% | 0.10 |
| Lipid lowering agent | 23.6% | 17.5% | 23.2% | 26.9% | 24.0% | 36.1% | 0.006 |
| Anti-anxiety agent | 4.1% | 4.2% | 4.4% | 3.8% | 5.3% | 1.6% | 0.63 |
| Anti-depressant | 9.1% | 9.0% | 8.7% | 11.5% | 9.3% | 6.6% | 0.80 |
| Sleep medication | 2.9% | 3.6% | 0.7% | 6.4% | 2.7% | 1.6% | 0.83 |
Continuous variables presented as mean + SD; categorical variables presented as percentages.
p-value based on log-transformed values. Missing cases exist for some variables.
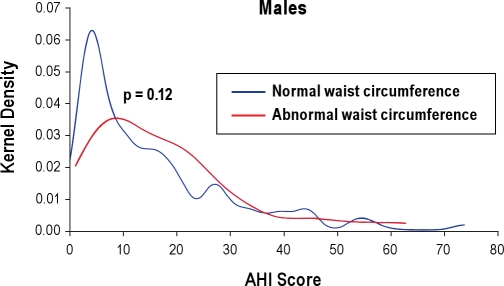
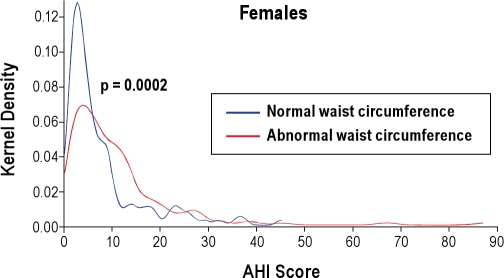
Distribution of AHI Scores
The mean AHI score was 11.4 ± 11.7, and 26% had moderate to severe sleep apnea as defined by an AHI ≥ 15. Based on Adult Treatment Panel III (ATP 3) criteria for waist circumference, there was only a nominal trend, indicating that participants with abdominal obesity had higher AHI scores than with normal waist circumference (11.6 ± 11.4 versus 11.3 ± 12.1, p = 0.07). This trend was similar in males and females (Figures 1 and 2).
Figure 1.
Distribution of apnea-hypopnea index (AHI) scores stratified by waist circumference (ATP3 criteria) for males
For males, abnormal waist circumference: > 102 cm. For females, abnormal waist circumference: > 88 cm.
Figure 2.
Distribution of apnea hypopnea index (AHI) scores stratified by waist circumference (ATP3 criteria) for females
For females, abnormal waist circumference: > 88 cm.
Sleep Apnea and Traditional Lipid Levels
In multivariable analysis adjusting for age, gender, race, smoking status, blood pressure, BMI, and statin use, lipid levels were not independently associated with AHI scores: total cholesterol (r = ?0.01, p = 0.96), LDL cholesterol (r = 0.00, p = 0.99), HDL cholesterol (r = ?0.02, p = 0.69), and triglycerides (log transformed) (r = 0.04, p = 0.40). Similar results were observed in analyses stratified by normal versus abnormal waist circumference (data not shown).
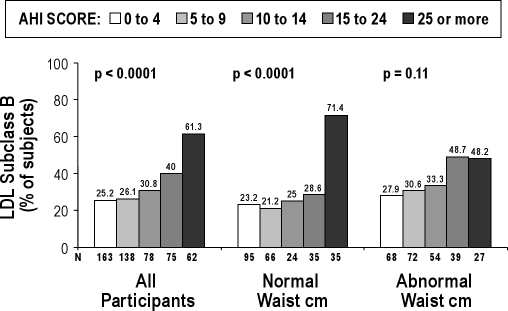
Sleep Apnea and LDL Subclass B
The percentage of participants with LDL subclass B varied significantly in relation to AHI score (Figure 3). Specifically, 61% of participants with AHI ≥ 25 had LDL subclass B, compared to only 25% of those with AHI ≥ 4 (p < 0.0001) in unadjusted analyses. However, the relationship between AHI score and LDL subclass B differed substantially by waist circumference. Among participants with abnormal elevated waist circumference, there was a nonsignificant trend of higher AHI scores being associated with LDL subclass B. In contrast, among participants with normal waist circumference, a threshold value of AHI ≥ 25 greatly increased the probability of having LDL subclass B (71% of all participants). In both the normal and abnormal waist circumference groups, a greater proportion of participants with AHI ≥ 25 had LDL subclass B as compared to LDL subclasses A and A/B (normal: 71% vs. 23% vs. 6%; abnormal: 48% vs. 30% vs. 22%, respectively). Analyses conducted separately for men and women showed a similar relationship between sleep apnea and LDL subclass B (data not shown), although women tended to have less severe sleep apnea overall than men in the Heart SCORE cohort.
Figure 3.
Percentage of subjects with LDL subclass B (atherogenic phenotype) by apnea hypopnea index (AHI) score overall and stratified by waist circumference
Consistent results were observed in multivariable analysis adjusted for age, gender, race, BMI, smoking status, statin use, and abnormal blood pressure per ATP3 criteria (systolic blood pressure ≥ 130 mm Hg, diastolic blood pressure ≥ 85 mm Hg, or use of antihypertensive drug therapy). Specifically, among 256 participants with abnormal waist circumference, AHI was not independently associated with LDL subclass B (Table 2). In contrast, among 255 participants with normal waist circumference, AHI ≥ 25 (compared to a score of 0 to 4) was associated with a 4.5-fold odds of having LDL subclass B (adjusted odds ratio = 4.53, 95% confidence interval: 1.67-12.24, p = 0.003). The formal test of interaction between abnormal waist circumference (dichotomous) × AHI ≥ 25 in relation to prevalence of LDL subclass B was statistically significant (p = 0.02), and was a more sensitive indicator of interaction than continuous measures of waist circumference, waist-to-hip ratio, and BMI (p = 0.10, 0.83, 0.07, respectively). In aggregate, these data indicate that AHI ≥ 25 is independently associated with a substantially elevated risk of having proatherogenic LDL subclass B, but only among participants with normal waist circumference.
Table 2.
Logistic regression analysis of adjusted odds ratios (OR) of LDL Subclass B in relation to apnea hypopnea index (AHI) score stratified by waist circumference
| AHI Score (compared to 0 to 4) | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Normal waist cm (n = 255) | 5 to 9 | 0.68 | (0.30 – 1.57) | 0.37 |
| 10 to 14 | 0.74 | (0.23 – 2.35) | 0.61 | |
| 15 to 24 | 1.06 | (0.40 – 2.82) | 0.90 | |
| 25 or more | 4.53 | (1.67 – 12.24) | 0.003 | |
| AHI Score (compared to 0 to 4) | OR | 95% CI | p-value | |
| Abnormal waist cm (n = 256) | 5 to 9 | 1.03 | (0.46 – 2.30) | 0.93 |
| 10 to 14 | 1.12 | (0.48 – 2.61) | 0.79 | |
| 15 to 24 | 1.48 | (0.58 – 3.77) | 0.41 | |
| 25 or more | 1.45 | (0.49 – 4.28) | 0.50 | |
Models were adjusted for age, gender, race, body mass index, smoking status, statin use, and abnormal blood pressure per ATP3 criteria (systolic blood pressure ≥ 130 mm Hg, diastolic blood pressure ≥ 85 mm Hg, or use of antihypertensive drug therapy).
DISCUSSION
We have shown that sleep apnea is independently associated with an atherogenic phenotype (LDL subclass B) in a diverse community cohort. The interaction between sleep apnea and LDL subclass B may account, in part, for the increased risk of atherosclerosis and subsequent vascular events that are associated with sleep apnea. However, this association appears to exist principally among those with a normal waist circumference. We chose to present these data stratified by waist circumference as opposed to BMI because of the better correlation of waist circumference to visceral obesity than BMI.8,9 There was a nominal trend indicating that participants with abnormal waist circumference had higher AHI scores than those with normal waist circumference. Our community-based sample had primarily mild sleep apnea; however, if the sample were enriched with more severe sleep apnea, more striking differences in AHI scores may have been found. In participants with normal waist circumference, the odds of having LDL subclass B were more than 4-fold higher among those with moderate to severe sleep apnea (AHI ≥ 25).
Despite finding that sleep apnea was associated with an atherogenic LDL subclass, we did not find an association between total cholesterol, HDL, or triglycerides and the severity of sleep apnea. This was true for all participants and when stratifying the analysis by waist circumference or BMI. These null findings are compatible with previous reports.17–19 One possible explanation for the lack of association between AHI and HDL or triglyceride levels is that our diverse community-based population was enriched with African American participants (37%), who as a group are known to have high HDL and low triglycerides at the same weight as compared to Caucasians.20 An alternate explanation is that the effect of sleep apnea is primarily on LDL subclass B, which would not be reflected in measurements of traditional lipid levels. Lipid-lowering agents such as niacin and fibric acid derivatives can shift lipoprotein particle size through their effects on triglycerides.21,22 Since triglycerides and HDL cholesterol were not significantly associated with AHI scores in both the normal and abnormal waist circumference groups, it is unlikely that differences in lipid-lowering medications between the groups accounted for our findings.
Dyslipidemia has been attributed to insulin resistance.23 A biochemical stress response possibly mediated by intermittent hypoxia, up-regulation of sympathetic activity, and oxidative stress triggers insulin resistance, which results in increased free fatty acids that form LDL.24–26 In the setting of insulin resistance and with the counter regulation by cortisol, LDL clearance is delayed, favoring the production of LDL subclass B. LDL subclass B, as opposed to LDL subclasses A and A/B, is inefficiently cleared from the circulation, resulting in an increased opportunity for oxidation and subsequent development of the atherogenic plaque. Clinically, insulin resistance is associated with increased LDL subclass B levels.27
It is biologically plausible that sleep apnea and consequent intermittent hypoxemia adversely affect LDL metabolism via one or more pathways. Li et al. have demonstrated in a mouse model that intermittent hypoxia will induce hyperlipidemia via sterol regulatory element binding protein (SREBP) 1, a master regulator of lipogenesis.28 Intermittent hypoxia has been shown to increase lipid loading in human macrophages.29 In addition, a recent report by Drager et al. has shown in a mouse model that chronic intermittent hypoxia inactivates lipoprotein lipase.30 Lipoprotein lipase deficiency is known to favor production of small dense LDL subclass B.31 Finally, in sleep apnea, there may be an additional effect of upregulation of cortisol independent of obesity, further promoting the production of LDL subclass B.32–34
The ability to detect an independent signal attributable to sleep apnea alone would be more likely in the non-obese sleep apnea population because the known effects of obesity on lipid profiles that may mask or diminish the effect of sleep apnea on LDL subclass B.7 Similar to the observation by Harsch and colleagues relative to sleep apnea and insulin resistance, we found that the relationship of LDL subclass B was strong and only evident in non-obese participants (Figure 3 and Table 2).35
The prevalence of moderate sleep apnea (AHI ≥ 15) was somewhat surprising at 26% in a cohort of participants who self-reported a 6% prevalence of a coexisting sleep disorder.36 This slightly higher rate than previously reported can probably be explained by the methodology used to identify sleep apnea.37,38 In our study, we used nasal pressure without oximetry as opposed to a nasal pressure with oximetry to identify apnea and hypopnea. Determining the presence of sleep apnea by assessment of nasal pressure alone may be considered a limitation of the current study. A direct measure of intermittent hypoxemia was not assessed with this device. Also, with nasal pressure alone, obstructive apneas could not be discriminated from central apneas. However, the portable monitor (ApneaLink, ResMed Corp) that we used has been previously validated with acceptable performance to identify obstructive sleep apnea.15,16,39 This finding has been corroborated by Ayappa et al., who compared nasal pressure alone to full polysomnography in and out of the laboratory.40
We controlled for weight in our analyses, including stratification by normal versus abnormal waist circumference. Thus, weight alone did not explain the relationship with AHI and LDL subclass B, although the direct contribution of visceral adiposity as an important covariate21 could not be formally assessed in our analysis. Insulin resistance was not measured. However, we controlled statistically for multiple components of the metabolic syndrome in our analysis, thereby suggesting that the metabolic syndrome or impaired glucose control did not account for the elevated LDL subclass B relationship to the severity of sleep apnea. In addition, there were slight differences in smoking history, racial distribution, and physical activity levels between the sub-study population and the Heart SCORE cohort. However, since this was a convenience sample, differences in demographic and clinical variables would be expected.
In summary, we have shown in a large community sample that sleep apnea is common, underdiagnosed (6.4% self-reported the diagnosis of any sleep disorder), and associated with the atherogenic phenotype LDL subclass B. The relationship is principally evident and strong in non-obese compared to obese participants and appears to have a threshold effect, i.e., at AHI > 25. These results indicate that sleep apnea may be an important target for treatment in patients with moderate to severe sleep apnea because of the increased risk of atherosclerotic vascular disease that has been identified in patients with this severity of sleep apnea.1,3 Further research is required to better define the relationship of sleep apnea, atherogenic LDL subclass B and atherosclerosis, and whether treatment of sleep apnea can favorably modify the atherogenic phenotype.
DISCLOSURE STATEMENT
This study was partially funded by the ResMed Foundation. Dr. Drumheller has received research funding from ResMed, the ResMed Foundation and Respironics for work completed with the approval of the University of Pittsburgh Office of Research. Dr. Strollo has received research support from ResMed and the ResMed Foundation. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Heart SCORE Investigators and Staff: University of Pittsburgh: Cardiovascular Institute: Steven E. Reis, M.D. (Principal Investigator), Aryan N. Aiyer, M.D., Daniel Edmundowicz, M.D., MPH, Oscar C. Marroquin, M.D., Suresh R. Mulukutla, M.D. Staff: Amy Beto, R.N., B.S.N., Rev. Sherry Brooks, Patti Chioda, Rebecca Chambers, B.S., Mary Catherine Coast, R.N., B.S.N., Andrea Dinga, M.Ed., R.D., L.D.N., Louise Martin, R.N., B.S.N., Lee Ann McDowell, Rosalyn Rapsinski, M.A., Kathleen Sward, Ph.D., Pamela White, R.N., B.S.N. Department of Epidemiology: Lewis Kuller, M.D., Dr.P.H., Janet Bonk R.N., MPH, Jennifer Rush, M.P.H.; Department of Medicine: Oliver J. Drumheller, Ed.D., R.R.T., Patrick J. Strollo, Jr., M.D.; Department of Psychiatry: Karen Matthews, Ph.D., Jane Owens, Ph.D. Center for Minority Health: Stephen Thomas, Ph.D., Mario Browne. Children's Hospital of Pittsburgh: Marin Kiesau, M.D., Deborah Moss, M.D., Evelyn C. Reis, M.D. Pittsburgh Theological Seminary: Rev. Dr. Ronald E. Peters, Ed.D., Rev. Sharon Washington. Urban League of Pittsburgh: Milana Barr, Lee Hipps, Jr., B.A. University of South Florida: College of Nursing: Kevin E. Kip, Ph.D. Carnegie Mellon University: Department of Psychiatry: Michael Scheier, Ph.D. Former Investigators and Staff: Matthew Kabala, B.S., Cheryl R. Rickens, R.N., B.S.N., Mavis Burks. Data and Safety Monitoring Board: Sheryl Kelsey, Ph.D., Sunil Mankad, M.D., Trevor Orchard, M.D.
This project is funded, in part, under a grant with the Pennsylvania Department of Health. (Contract ME-02-384), NIH 1 R01 HL076379-01, NIH 1 R24 HL076852-1, and the ResMed Foundation. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations, or conclusions.
ABBREVIATIONS
- CAD
coronary artery disease
- LDL subclass B
small, dense low-density lipoprotein cholesterol concentration
- Heart SCORE
Heart Strategies Concentrating On Risk Evaluation
- BMI
body mass index
- LDL
low density lipoprotein cholesterol
- AH
apnea hypopnea index
- ATP III
Adult Treatment Panel III
- HDL
high-density lipoprotein cholesterol
Table S1.
Characteristics of the total Heart SCORE sample, participants in sleep apnea sub-study, and the remaining Heart SCORE participants
| Characteristic | Total (N = 2000) | Sleep apnea sub-study (N = 519) | Other Heart SCORE participants (N = 1481) | p-value |
|---|---|---|---|---|
| Age (years), mean ± SD | 59.1±7.5 | 58.7±7.4 | 59.2±7.5 | 0.21 |
| Gender, % | 0.76 | |||
| Male | 34.7 | 35.5 | 34.5 | |
| Female | 65.3 | 64.7 | 65.5 | |
| Race, % | 0.04 | |||
| White | 53.9 | 58.8 | 52.2 | |
| Black | 42.8 | 37.4 | 44.6 | |
| Other | 3.4 | 3.9 | 3.2 | |
| Education, % | < 0.001 | |||
| Less than HS | 2.4 | 1.4 | 2.7 | |
| HS diploma | 16.7 | 12.6 | 18.1 | |
| Some college | 32.7 | 32.4 | 32.9 | |
| Bachelor's degree | 22.3 | 24.4 | 21.5 | |
| Advanced degree | 26.0 | 29.3 | 24.8 | |
| Annual income, % | < 0.001 | |||
| Less than $10,000 | 6.2 | 2.6 | 7.4 | |
| $10K to < $20K | 12.5 | 10.8 | 13.1 | |
| $20K to < $40K | 28.8 | 27.4 | 29.3 | |
| $40K to < $80K | 32.9 | 35.4 | 32.1 | |
| $80K or more | 19.6 | 23.8 | 18.2 | |
| Smoking status, % | 0.02 | |||
| Current smoker | 10.4 | 7.9 | 11.2 | |
| Former smoker | 41.5 | 40.3 | 41.9 | |
| Never smoker | 48.2 | 51.8 | 46.9 | |
| Alcohol – total drinks/week, % | 0.07 | |||
| No drinks | 63.3 | 60.6 | 64.6 | |
| 1 drink | 3.3 | 2.9 | 3.4 | |
| 2-3 drinks | 8.9 | 9.3 | 8.8 | |
| 4-7 drinks | 11.5 | 12.8 | 11.0 | |
| > 7 drinks | 12.7 | 14.3 | 12.2 | |
| Current physical activity level, % | 0.02 | |||
| Sedentary | 9.2 | 7.4 | 9.9 | |
| Mild | 31.6 | 28.2 | 32.8 | |
| Moderate | 52.9 | 58.8 | 50.9 | |
| Strenuous | 6.3 | 5.6 | 6.5 | |
| History of hypertension, % | 0.94 | |||
| No | 57.4 | 57.5 | 57.3 | |
| Yes | 42.6 | 42.5 | 42.7 | |
| History of hyperlipidemia, % | 0.65 | |||
| No | 54.2 | 53.3 | 54.5 | |
| Yes | 45.8 | 46.7 | 45.5 | |
| History of diabetes, % | 0.10 | |||
| No | 89.7 | 91.5 | 89.0 | |
| Yes | 10.4 | 8.5 | 11.0 | |
| Body mass index, mean ± SD | 30.1 ± 6.3 | 29.6 ± 5.7 | 30.2 ± 6.6 | 0.15 |
| Waist circumference (cm), mean ± SD | 96.1 ± 15.2 | 95.2 ± 14.1 | 96.3 ± 15.5 | 0.29 |
| Total cholesterol (mg/dL), mean ± SD | 213.0 ± 42.8 | 214.6 ± 41.8 | 212.4 ± 43.1 | 0.51 |
| LDL cholesterol (mg/dL), mean ± SD | 142.2 ± 36.3 | 143.0 ± 35.5 | 141.9 ± 36.6 | 0.56 |
| HDL cholesterol (mg/dL), mean ± SD | 57.5 ± 15.0 | 58.3 ± 15.3 | 57.2 ± 14.8 | 0.22 |
| Triglycerides (mg/dL), mean ± SD | 123.4 ± 75.4 | 122.1 ± 79.6 | 123.9 ± 73.9 | 0.16 |
| Framingham risk strata | 0.16 | |||
| Low risk | 56.9 | 57.9 | 56.6 | |
| Intermediate risk | 24.3 | 26.6 | 23.5 | |
| High risk | 18.8 | 15.4 | 19.9 | |
| Blood pressure abnormal (ATP3), % | 0.68 | |||
| No | 35.2 | 35.9 | 34.9 | |
| Yes | 64.8 | 64.1 | 65.1 |
REFERENCES
- 1.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 2.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 3.Redline S, Yenokyan G, Gottlieb DJ, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Newman AB, Nieto FJ, Guidry U, et al. Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol. 2001;154:50–9. doi: 10.1093/aje/154.1.50. [DOI] [PubMed] [Google Scholar]
- 5.Roche F, Sforza E, Pichot V, et al. Obstructive sleep apnoea/hypopnea influences high-density lipoprotein cholesterol in the elderly. Sleep Med. 2009;10:882–6. doi: 10.1016/j.sleep.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 6.Rizzo M, Berneis K. Low-density lipoprotein size and cardiovascular risk assessment. QJM. 2006;99:1–14. doi: 10.1093/qjmed/hci154. [DOI] [PubMed] [Google Scholar]
- 7.Howard BV, Ruotolo G, Robbins DC. Obesity and dyslipidemia. Endocrinol Metab Clin North Am. 2003;32:855–67. doi: 10.1016/s0889-8529(03)00073-2. [DOI] [PubMed] [Google Scholar]
- 8.Carr DB, Utzschneider KM, Hull RL, et al. Intra-abdominal fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III criteria for the metabolic syndrome. Diabetes. 2004;53:2087–94. doi: 10.2337/diabetes.53.8.2087. [DOI] [PubMed] [Google Scholar]
- 9.Ross R, Rissanen J, Hudson R. Sensitivity associated with the identification of visceral adipose tissue levels using waist circumference in men and women: effects of weight loss. Int J Obes (Lond.) 1996;20:533–8. [PubMed] [Google Scholar]
- 10.Ainsworth BE, Jacobs DR, Jr, Leon AS. Validity and reliability of self-reported physical activity status: the Lipid Research Clinics questionnaire. Med Sci Sports Exerc. 1993;25:92–8. doi: 10.1249/00005768-199301000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Franklin BA, Whaley MH, Howley ET. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2000. ACSM's guidelines for exercise testing and prescription. [Google Scholar]
- 12.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults et al. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 13.Chung BH, Wilkinson T, Geer JC, Segrest JP. Preparative and quantitative isolation of plasma lipoproteins: rapid, single discontinuous density gradient ultracentrifugation in a vertical rotor. J Lipid Res. 1980;21:284–91. [PubMed] [Google Scholar]
- 14.Kulkarni KR. Cholesterol profile measurement by vertical auto profile method. Clin Lab Med. 2006;26:787–802. doi: 10.1016/j.cll.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Teschler T, Weinreich G, Hess S, Wessendorf TE, Teschler H. Validation of microMESAM as screening device for sleep disordered breathing. Pneumologie. 2003;57:734–40. doi: 10.1055/s-2003-812423. [DOI] [PubMed] [Google Scholar]
- 16.Oktay B, Rice TB, Atwood CW, et al. Evaluation of a single channel portable monitor for the diagnosis of obstructive sleep apnea. J Clin Sleep Med. 2011;7:384–390. doi: 10.5664/JCSM.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP. Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J. 2004;25:735–41. doi: 10.1016/j.ehj.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 18.Kono M, Tatsumi K, Saibara T, et al. Obstructive sleep apnea syndrome is associated with some components of metabolic syndrome. Chest. 2007;131:1387–92. doi: 10.1378/chest.06-1807. [DOI] [PubMed] [Google Scholar]
- 19.Tan KC, Chow WS, Lam JC, et al. HDL dysfunction in obstructive sleep apnea. Atherosclerosis. 2006;184:377–82. doi: 10.1016/j.atherosclerosis.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 20.Kuller LH. Ethnic differences in atherosclerosis, cardiovascular disease and lipid metabolism. Curr Opin Lipidol. 2004;15:109–13. doi: 10.1097/00041433-200404000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Bays HE, McGovern ME, Kopin L. Once daily niacin extended release/lovastatin combination tablet has more favorable effects on lipoprotein particle size and subclass distribution than atorvastatin and simvastatin. Prev Cardiol. 2003;6:179–188. doi: 10.1111/j.1520-037x.2003.03142.x. [DOI] [PubMed] [Google Scholar]
- 22.Yuan J, Tsaic MY, Hunninghake DB. Changes in composition and distribution of LDL subspecies in hypertriglyceridemic and hypercholesterolemic patients during gemfibrozil therapy. Atherosclerosis. 1994;110:1–11. doi: 10.1016/0021-9150(94)90062-0. [DOI] [PubMed] [Google Scholar]
- 23.Punjabi NM, Polotsky VY. Disorders of glucose metabolism in sleep apnea. J Appl Physiol. 2005;99:1998–2007. doi: 10.1152/japplphysiol.00695.2005. [DOI] [PubMed] [Google Scholar]
- 24.Drager LF, Jun J, Polotsky VY. Obstructive sleep apnea and dyslipidemia: implications for atherosclerosis. Curr Opin Endocrinol Diabetes Obes. 2010;17:161–5. doi: 10.1097/MED.0b013e3283373624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jun J, Reinke C, Bedja D, et al. Effect of intermittent hypoxia on atherosclerosis in apolipoprotein E-deficient mice. Atherosclerosis. 2010;209:381–6. doi: 10.1016/j.atherosclerosis.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tkacova R, Rizzo M, Berneis K. Therapy with noninvasive ventilation in patients with obstructive sleep apnoea: effects on atherogenic lipoprotein phenotype. Med Hypotheses. 2009;73:441–4. doi: 10.1016/j.mehy.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 27.Howard BV. Insulin resistance and lipid metabolism. Am J Cardiol. 1999;84:28J–32J. doi: 10.1016/s0002-9149(99)00355-0. [DOI] [PubMed] [Google Scholar]
- 28.Li J, Thorne LN, Punjabi NM, et al. Intermittent hypoxia induces hyperlipidemia in lean mice. Circ Res. 2005;97:698–706. doi: 10.1161/01.RES.0000183879.60089.a9. [DOI] [PubMed] [Google Scholar]
- 29.Lattimore JD, Wilcox I, Nakhla S, Langenfeld M, Jessup W, Celermajer DS. Repetitive hypoxia increases lipid loading in human macrophages-a potentially atherogenic effect. Atherosclerosis. 2005;179:255–9. doi: 10.1016/j.atherosclerosis.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 30.Drager LF, Li J, Shin M, et al. Intermittent hypoxia inhibits clearance of triglyceride-rich lipoproteins and inactivates adipose lipoprotein lipase in a mouse model of sleep apnoea. Eur Heart J. 2011 doi: 10.1093/eurheartj/ehr097. Apr 9 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hokanson JE, Brunzell JD, Jarvik GP, Wijsman EM, Austin MA. Linkage of low-density lipoprotein size to the lipoprotein lipase gene in heterozygous lipoprotein lipase deficiency. Am J Hum Genet. 1999;64:608–18. doi: 10.1086/302234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005;90:3106–14. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 33.Lanfranco F, Gianotti L, Pivetti S, et al. Obese patients with obstructive sleep apnoea syndrome show a peculiar alteration of the corticotroph but not of the thyrotroph and lactotroph function. Clin Endocrinol. 2004;60:41–8. doi: 10.1111/j.1365-2265.2004.01938.x. [DOI] [PubMed] [Google Scholar]
- 34.Parlapiano C, Borgia MC, Minni A, Alessandri N, Basal I, Saponara M. Cortisol circadian rhythm and 24-hour Holter arterial pressure in OSAS patients. Endocr Res. 2005;31:371–4. doi: 10.1080/07435800500456895. [DOI] [PubMed] [Google Scholar]
- 35.Harsch IA, Schahin SP, Radespiel-Troger M, et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004;169:156–62. doi: 10.1164/rccm.200302-206OC. [DOI] [PubMed] [Google Scholar]
- 36.Quan SF, Gillin JC, Littner MR, Shepard JW. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 37.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–39. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 38.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med. 2002;162:893–900. doi: 10.1001/archinte.162.8.893. [DOI] [PubMed] [Google Scholar]
- 39.Erman M, Stewart D, Einhorn D, Gordon N, Casal E. Validation of the ApneaLink for the screening of sleep apnea: a novel and simple single-channel recording device. J Clin Sleep Med. 2007;3:387–92. [PMC free article] [PubMed] [Google Scholar]
- 40.Ayappa I, Norman RG, Suryadevara M, Rapoport DM. Comparison of limited monitoring using a nasal-cannula flow signal to full polysomnography in sleep-disordered breathing. Sleep. 2004;27:1171–9. doi: 10.1093/sleep/27.6.1171. [DOI] [PubMed] [Google Scholar]