Abstract
Obesity has progressed in a few decades from a public health footnote in developed countries to a top-priority international issue. Because obesity implies increased morbidity and mortality from chronic, debilitating disorders, it is a major burden on individuals and health systems in both developing and developed countries. Obesity is a complex disorder unequally affecting all age groups and socioeconomic classes. Of special concern is increasing childhood obesity. This review presents the extent of the obesity epidemic and its impact worldwide by way of introduction to a discussion of colon and rectal surgery in the obese patient.
Keywords: Epidemiology, obesity, overweight
OBESITY PREVALENCE WORLDWIDE
Globally, increased weight and obesity are rising in both the developing and developed world. Over the past 20 years, the rate of obesity has tripled in developing countries as they become more urbanized and adopt a Western lifestyle of higher caloric intake combined with a more sedentary lifestyle. Obesity has become recognized as one of the major health problems threatening the world today, along with malnourishment, underweight, and infectious disease. The International Obesity Task Force and the World Health Organization (WHO) report over 1.1 billion adults worldwide are overweight, 312 million of whom are obese. In addition, over 155 million children are overweight or obese worldwide; 42 million of these children are under the age of 5. The areas of the world at greatest risk due to dramatic increases in prevalence rates are the Middle East, Pacific Islands, Southeast Asia, and China.1
The co-existence of obesity and undernutrition in developing countries is not uncommon. The lower-class population in low-income countries tends to be underweight and malnourished. On the other hand, the lower-class population in middle-income countries has a high risk of obesity. Paradoxically, many poor families in these middle-income countries have obese parents with malnourished children. Some studies explain this phenomenon with the “thrifty gene” hypothesis, which states that intrauterine growth retardation and the resulting low birth weight confers a predisposition to obesity later in life.2 Obesity is highly prevalent in the middle-income countries of Eastern Europe, Latin America, and Asia, where obesity is the fifth most common cause of disease-burden, ranking just below underweight.3
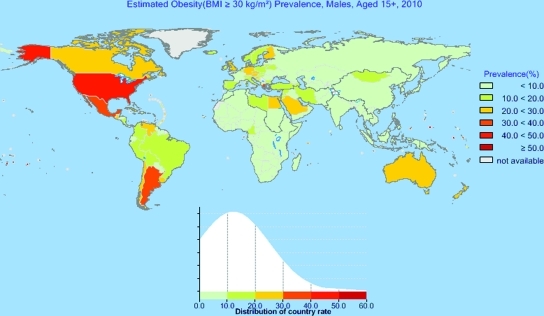
The 2010 WHO Global Infobase shows 90 countries (46.8%) with an average body mass index (BMI) in men greater than 25, and four tiny Western Pacific nations have an average BMI greater than 30 (Tonga, Federated States of Micronesia, Nauru, and Cook Islands). The BMI in the United States is teetering toward the obese mark, with an average of 29.3. The percent prevalence of obesity shown in Fig. 1 depicts the rapid escalation of the obesity epidemic in South America, Eastern Europe, and the Middle East.3
Figure 1.
2010 estimated obesity prevalence in males, ages 15–100 (used by permission, WHO Global Infobase 2010).3
Childhood Obesity
Childhood obesity is a global problem, but the prevalence is higher in developed countries, particularly the United States. Worldwide, the childhood obesity prevalence in 2010 is 6.7%; in the United States, 20% of children are affected.5 Childhood obesity in the United States has more than tripled in the past 30 years. Interestingly, in both developed and developing countries, the prevalence of overweight girls is greater than overweight boys, particularly among adolescents: 70% of obese adolescents become obese adults. This has led many observers to view childhood obesity as the root of the obesity problem, and also its most potentially tractable element.
OBESITY PREVALENCE IN THE UNITED STATES
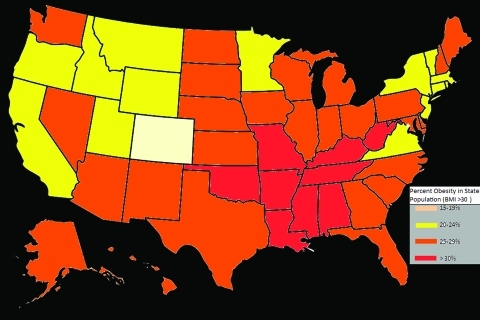
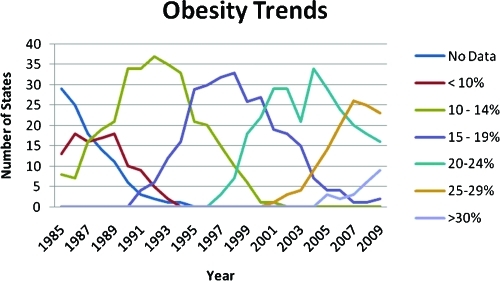
As a major developed country with the highest average BMI, the United States faces a great obesity challenge. The U.S. obesity rate has been consistently increasing since 1985, when the Center for Disease Control (CDC) began collecting data. In 1998, the National Institute of Health (NIH) found that 97 million people in the United States—55% of the population—were obese or overweight. According to the CDC, in 1990, no states had a prevalence of obesity greater than or equal to 15%. By 1999, no state had prevalence less than 10%, 18 states had a prevalence of obesity between 20 to 24%, and no state had prevalence greater than or equal to 25%. In 2009, only Colorado and the District of Columbia had a prevalence of obesity less than 20%; twenty-seven states had prevalence greater than or equal to 25%; nine states (Alabama, Arkansas, Kentucky, Louisiana, Mississippi, Missouri, Oklahoma, Tennessee, and West Virginia) had a prevalence of obesity greater than or equal to 30%.6 The increased prevalence of obesity is shown in Fig. 2, and the seemingly inexorable movement of state populations toward obesity is shown in Fig. 3. As seen in Fig. 2, although obesity is a nationwide issue, the problem is greatest in the less-affluent states of the South due to racial and socioeconomic demographic differences.4
Figure 2.
Percent obesity in state populations in the United States (2009 data).4
Figure 3.
Obesity trends among US adults.6
ETIOLOGY
The worldwide obesity epidemic reflects the substantial changes in behavioral patterns as more people adopt Western lifestyles. Although genetics determines an individual's susceptibility to weight gain, the primary mechanism of obesity is simply a chronic caloric imbalance: high caloric intake combined with a sedentary lifestyle. Human genetics has not changed significantly in the past two decades, but obesity has risen dramatically in developing countries. A reasonable explanation for this phenomenon is a change in environmental factors.
Although differences in individuals' metabolic efficiency are a subject of current obesity research, genetic differences are clearly insufficient in explaining the causes of obesity. Resting energy expenditure has only a limited capacity to adjust to changes in food intake. Even when comparing fasting with overfeeding, energy expenditure is only altered by 5 to 10%.7 Thus, differences in the metabolic rate among individuals cannot solely account for the rise in obesity.
Rising incomes, increasing urban populations, diets high in fats and simple sugars, and a shift toward less physically demanding jobs are some of the societal changes resulting in increased obesity. Less physical activity is promoted by automated transport, labor-saving technology in the home and workplace, television, and computer games. These changes in the social environment promote excessive food intake and decreased physical activity, leading to obesity.7
Increased caloric intake in the United States is evidenced by larger portion sizes and high-fat diets. Studies in humans have shown that a high-fat diet (>35% of calories from fat) leads to increased energy intake, efficiency of body fat gain, and obesity.7 The average percent body fat is proportional to the fat intake. Although the majority of individuals become obese with increased fat intake, a few do not gain weight on low-fat diets, compared with controls. Dietary restraint (consciously refraining from food consumption) is protective.
Despite these studies, self-report studies have shown that dietary fat intake has decreased from 37% to 34% over the past decade despite continual increase in obesity.7 This has led to arguments over the true impact of high-fat diets on weight, with some arguing that low-fat diets do not lead to decreases in obesity. Most studies agree that reducing fat in the diet will not decrease obesity but will prevent a further increase in body fat.
GENETICS
Neel's widely cited “thrifty gene” hypothesis posits that during human evolution, food was sporadically available and famine a constant risk. In that setting, genes that allowed for energy conservation (and thus predisposed to obesity) were advantageous for survival and thus evolutionarily selected for.2 Examples of thrifty genes would include polymorphisms in the leptin system and other heritable elements that allow for accumulation of adipose tissue. Today, when most people have access to an abundance of food, thrifty genes have become a liability.
Energy homeostasis is controlled by neurons in the hypothalamus that regulate appetite and metabolism. Endocrine signals such as glucose, insulin, free fatty acids, and leptin send messages about the body's energy state to the hypothalamus, thus controlling the firing of these neurons. Leptin is a hormone produced by adipose tissue that signals a decrease in appetite when fat stores are high, thus regulating intake according to body fat stores.8 With weight loss, circulating leptin decreases, leading to increased appetite and decreased energy expenditure. Conversely, with weight gain, the increased leptin causes decreased appetite and increased energy expenditure. Variation among individuals may explain why some people seem protected against becoming overweight despite living in the same environment and consuming the same food as the obese.9 The leptin system also helps explain why it is more difficult to lose weight than to gain it.
Numerous studies have confirmed the contribution of genetics in the obesity epidemic. Ten percent of morbidly obese children come from consanguineous families, suggesting that other forms of genetic links are present.2 The heritability of obesity is similar to the heritability of height. There are clear genetic elements in obesity. Genetic polymorphisms, causing decreased or nonfunctional levels of leptin or malfunctioning mutations in the leptin receptor, result in an abnormally high appetite and obesity beginning in childhood. Daily injections of leptin result in appetite normalization followed by weight loss back to normal levels. Some obese individuals have been found to be leptin-resistant.10 When such individuals are given leptin therapy, there is no resultant decrease in body fat.
As a complex multifactorial disorder, obesity is very difficult to treat. Significant weight loss leads to intense hunger, mediated by the decrease in circulating leptin after the loss of adpiocytes.10 The greater the weight loss, the greater the hunger, until for most dieters hunger trumps the desire to lose weight. Only one out of six adults in the United States who has ever been overweight or obese has accomplished long-term weight loss of at least 10%.11 Many studies demonstrate that obese adults can lose ∼0.5 kg per week by decreasing their daily intake by 500 to 1000 kcals below the caloric intake required to maintain their weight. Although modest weight loss is achievable by dieting,9 the most effective method of long-term weight loss is lifestyle change.
MEASUREMENT OF OBESITY
Obesity is commonly measured by the body mass index (BMI). BMI is an estimate of body fat based on height and weight that applies to adult men and women (BMI = weight in kg/height2 in m2). BMI makes an assumption about the distribution of adipose tissue and lean muscle mass of an individual using only weight and height. BMI calculation thus overestimates adiposity of an individual with a large proportion of lean muscle mass and underestimates the adiposity in an individual with low lean muscle mass. Similarly, with aging, body fat naturally increases and muscle mass decreases without a corresponding change in BMI such that BMI is underestimated in older individuals. The last major limitation of BMI is ethnicity due to differences in heights, muscle mass, and adipose distribution. For example, Asian-Pacific populations have an increased risk of obesity-related complications at a BMI of 23, whereas Caucasians have an increased risk at a BMI of 25.12
BMI cannot accurately measure adiposity in children. In pubertal adolescents, weight can double, while the height only increases by 20%. Childhood weight is measured differently from adult obesity. The CDC defines overweight in children as above the 95th percentile of BMI for a specified age group and “at risk for overweight” between the 85th and 95th percentile for age.5
Although all adipose tissue increases the risk of obesity-related diseases, not all fat equally contributes to disease states. Visceral obesity is associated with a higher risk of cardiovascular disease, hypertension, insulin resistance (metabolic syndrome), and diabetes mellitus type II. Some argue that anthropometric measurements are better estimates of adiposity because central obesity more directly assesses health risk. Computed tomography (CT) is considered to give the most accurate measurement of body fat, particularly intraabdominal fat deposition. However, CT scans are costly, time consuming, and involve exposure to unnecessary ionizing radiation. A simpler and cheaper way to measure intraabdominal fat is through waist circumference. Waist circumference or a simple waist-to-height ratio may give a more accurate assessment of health risks (from metabolic syndrome, for example) for athletes such as body builders, who are heavy but have a high percentage of muscle and a low percentage of central body fat (Table 1).13
Table 1.
Measurements of Obesity13
| Categories | BMI | Waist Circumference | Waist-to-Height Ratio | ||||
|---|---|---|---|---|---|---|---|
| Men | Women | Men (5′9″) | Women (5′4″) | ||||
| Underweight | <18.5 | ||||||
| Normal weight (healthy) | 18.5–24.9 | <37.0″ | <31.5″ | <53.6% | <49.2% | ||
| Overweight (increased health risk) | 25.0–29.9 | 37.0–40.2″ | 31.5–34.6″ | 53.6–58.3% | 49.2–54.0% | ||
| Obese (substantially increased health risk) | >30 | >40.2″ | >34.6″ | >58.3% | >54.0% | ||
| Morbidly obese | >40 | ||||||
>BMI, Body mass index.
EFFECTS OF OBESITY
In 2005, the CDC estimated that 365,000 die annually in the United States from obesity.14 Some studies predict that U.S. life expectancy will level off or decline by 2050 due to childhood obesity.15 Obesity's health risks include a long list of debilitating but not life-threatening diseases—respiratory difficulties, osteoarthritis, skin problems, infertility, etc. Increased body fat leads to adverse metabolic effects on blood pressure, insulin resistance, and cholesterol levels. The major obesity-associated conditions stem from these metabolic effects: cardiovascular disease, type 2 diabetes, cancers (particularly colorectal, breast, prostate, endometrial, kidney, and gallbladder), and gallbladder disease.
About 90% of type 2 diabetes is attributable to obesity, and obesity-related metabolic syndrome causes impaired glucose tolerance in 197 million people worldwide. The world prevalence of type 2 diabetes is expected to increase to 366 million by 2033, with the most prominent increase in developing countries.1
HEALTHCARE COSTS AND PROJECTIONS FOR THE FUTURE
The financial costs of obesity are growing. Overweight and obesity has been estimated to account for 16% of the global burden of disease. In the developed world, 2 to 7% of total health care costs are attributable to obesity. In the United States, the direct and indirect costs of obesity were estimated at $123 billion in 2001.1
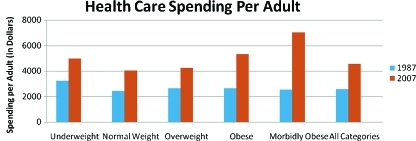
The Congressional Budget Office (CBO) found that healthcare costs have increased among all weight categories from 1987 to 2007, but the increase was disproportional among the obese. Health care spending per adult rose 80% between 1987 and 2007 from $2,560 to $4,550, driven by the increase in medical technology, the aging population, the increase in coverage by insurance companies, and the rising price of health care services. Per capita spending for obese individuals exceeds spending for normal weight individuals by 38% in 2007 (Fig. 4).16 Assuming that the average body weight does not change in the future, the CBO predicts that the average per capita health care cost per adult will rise from $4,550 in 2007 to $7,500 in 2020.
Figure 4.
Health care spending per adult in 1987 and 2007 (CBO data).16
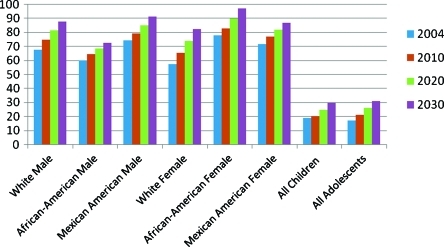
If obesity continues its current rate of increase, by 2030, 86.3% of all American adults will be overweight or obese and 51% of all adults will be obese (Fig. 5). By 2048, all American adults will be overweight or obese. The groups most affected will be African American females (96.9% by 2030) and Mexican American males (91.1% by 2030). The prevalence of overweight children will also double by 2030. Total health care costs attributable to obesity/overweight would double every decade to 861 to 957 billion dollars by 2030, accounting for 16 to 18% of total U.S. health care costs.17
Figure 5.
Estimated percent overweight or obese in the United States.17
The net impact of reductions in obesity rates on national health care expenditures and on federal budget deficits contributing to retirement programs such as Social Security and Medicare, would depend on the increased life expectancy that results from decreased obesity rates. Savings from lower per-capita spending would be partially offset by additional health care spending during those added years of life.16
The U.S. government, the WHO, and other governmental entities have begun a long and so far minimally successful struggle against obesity, with public-education campaigns, regulation of public-school lunch choices, and the like. Knowledge of the obesity epidemic is universal and has become a popular cliché, as in the 2008 movie WALL-E. Given the coincidence of genes, environment, psychology, technology, and culture, all promoting–or at least allowing—overweight and obesity, this will be a difficult trend to reverse. New technology and culture change are needed, as is the power of economics to make incentives that drive culture change. Meanwhile, health care providers may expect to take care of more and more obese patients.
References
- 1.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. Erratum in: N Engl J Med 2007 Mar 1;356(9):973. N Engl J Med. 2007;356(3):213–215. doi: 10.1056/NEJMp068177. [DOI] [PubMed] [Google Scholar]
- 2.Friedman J M. A war on obesity, not the obese. Science. 2003;299(5608):856–858. doi: 10.1126/science.1079856. [DOI] [PubMed] [Google Scholar]
- 3.Global Infobase WHO Available at: Mortalities, May 10, 2010. https://apps.who.int/infobase/ Accessed November 30, 2010. https://apps.who.int/infobase/
- 4.Centers for Disease Control and Prevention (CDC) Vital signs: state-specific obesity prevalence among adults—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(30):951–955. [PubMed] [Google Scholar]
- 5.Dehghan M, Akhtar-Danesh N, Merchant A T. Childhood obesity, prevalence and prevention. Nutr J. 2005;4:24. doi: 10.1186/1475-2891-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Obesity Trends among US Adults between 1985 and 2009. Atlanta: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 7.Hill J O, Peters J C. Environmental contributions to the obesity epidemic. Science. 1998;280(5368):1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz M W, Porte D., Jr Diabetes, obesity, and the brain. Science. 2005;307(5708):375–379. doi: 10.1126/science.1104344. [DOI] [PubMed] [Google Scholar]
- 9.Wisse B E, Kim F, Schwartz M W. Physiology. An integrative view of obesity. Science. 2007;318(5852):928–929. doi: 10.1126/science.1148032. [DOI] [PubMed] [Google Scholar]
- 10.Erez G, Tirosh A, Rudich A, et al. Phenotypic and genetic variation in leptin as determinants of weight regain. Int J Obes (Lond) 2010;35(6):785–792. doi: 10.1038/ijo.2010.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kraschnewski J L, Boan J, Esposito J, et al. Long-term weight loss maintenance in the United States. Int J Obes (Lond) 2010;34(11):1644–1654. doi: 10.1038/ijo.2010.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lara-Esqueda A, Aguilar-Salinas C A, Velazquez-Monroy O, et al. The body mass index is a less-sensitive tool for detecting cases with obesity-associated co-morbidities in short stature subjects. Int J Obes Relat Metab Disord. 2004;28(11):1443–1450. doi: 10.1038/sj.ijo.0802705. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Global Strategy on Diet, Physical Activity and Health. Geneva: World Health Organization; 2004. [Google Scholar]
- 14.Couzin J. Public health. A heavyweight battle over CDC's obesity forecasts. Science. 2005;308(5723):770–771. doi: 10.1126/science.308.5723.770. [DOI] [PubMed] [Google Scholar]
- 15.Mann C C. Public health. Provocative study says obesity may reduce U.S. life expectancy. Science. 2005;307(5716):1716–1717. doi: 10.1126/science.307.5716.1716. [DOI] [PubMed] [Google Scholar]
- 16.Duchovny N, Baker C. How Does Obesity in Adults Affect Spending on Health Care? Washington, DC: Congressional Budget Office; 2010. [Google Scholar]
- 17.Wang Y, Beydoun M A, Liang L, Caballero B, Kumanyika S K. Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 2008;16(10):2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]