Abstract
Background
Despite pharmacologic advances, medication non-adherence continues to challenge primary care providers in blood pressure (BP) management.
Methods
Medical, nursing and pharmacy students (n = 11) were recruited and trained as health coaches for uninsured, hypertensive patients (n = 25) of a free clinic in an uncontrolled open trial. Pre-post analysis was conducted on BP, medication adherence, frequency of home BP monitoring, and healthy behavior (e.g., diet, exercise). Patient satisfaction and feasibility of a student coach model was qualitatively evaluated.
Results
In the 12 patients who completed the intervention, an increase in medication adherence as measured by the Brief Medication Questionnaire was observed (P < 0.01), with a 11 mmHg reduction in systolic BP (P = 0.03). Qualitative data showed patient satisfaction with the intervention and other healthy behavior change.
Conclusions
This feasibility study shows use of student health coaches to combat medication non-adherence in uninsured, hypertensive adults is promising.
Keywords: health coach, hypertension, medication adherence
Hypertension and medication non-adherence
Hypertension (defined as systolic blood pressure (BP) >140 mmHg or diastolic BP >90 mmHg) is a major risk factor for cardiovascular disease, which includes coronary heart disease, congestive heart failure, and ischemic or hemorrhagic stroke.1 According to the National Health and Nutrition Examination Survey (NHANES), 28.7% (age-adjusted prevalence) of U.S. adults, or ≈58.4 million individuals, are affected.2 Treatment of high BP with antihypertensive medications can greatly reduce the risk of cardiovascular disease with a reduction of stroke risk by 31–45% and a reduction of myocardial infarction risk by 8–23%.3
Despite the availability of treatment, BP control remains a problem for those who do not adhere to prescribed antihypertensive drugs. Over half of patients do not adhere to their prescribed medications, resulting in over $100 billion spent on avoidable hospitalizations.4 Poor medication adherence and its sequelae are well-recognized clinical challenges for providers, with many calling for addressing medication adherence as a priority in health care reform.5,6 There are many reasons for medication non-adherence in hypertensive patients. They include the financial cost of medication, the long duration of drug therapy, the lack of symptoms in hypertension, complicated drug regimens, not understanding hypertensive management, lack of motivation and conflicting individual health beliefs.7,8 Many of these reasons are barriers to treatment adherence in chronic diseases in general, especially for uninsured, minority patients.9 These vulnerable patients may require services in addition to their usual brief primary care visits to assist with chronic disease management.
Health coaching
Health coaching promotes healthy behavior change through a structured partnership between an invested patient and a supportive coach. Within a primary care team, health coaches have five important roles: 1) offering self-management support, 2) bridging gaps between clinician and patient, 3) assisting patients in navigating the health care system, 4) providing emotional support and 5) serving as figures of continuity.10 Most importantly, coaches impart patients with knowledge, skill and confidence, so that patients can actively participate in their own health care.10 These services are invaluable for those who struggle with medication adherence in a chronic disease like hypertension.
Although literature reveals that health coaching can be varied (e.g., type of coach, route of coaching, chronic condition studied), its impact on patients generally appears to be positive. In a multicenter, randomized controlled trial study, patients with coronary heart disease who received telephone coaching from dietitians or nurses achieved greater reductions in total cholesterol and many other coronary risk factors, compared to those who received usual care.11 A diabetes lifestyle intervention delivered by trained community residents showed significant decreases in hemoglobin A1C levels in African-American and Latino diabetic patients, compared to A1C levels in the control group.12
Literature reveals various research studies with nurses, medical assistants and community health workers as health coaches, but there are very few reports on using students as health coaches.13,14,15 Health professional students are good candidates for health coaching for several reasons. First, students who self-select into healthcare fields generally have a strong interest in patient interaction. Second, health professional students arrive with a modest amount of training in counseling. Third, these students often have direct service or clinical experience requirements for graduation. Finally, frequent, close patient interaction affords a clinical opportunity for students to learn about primary care medicine.
The concept of using health professional students as health coaches is not entirely novel. Wagner and colleagues proposed using first-year medical students as health coaches, as a part of a patient-doctor course at the Medical College of Georgia.14 From working with assigned diabetic patients, students learned the difficulty of effecting healthy behavior change and became more self-aware about provider-patient communication. These students learned important concepts related to clinical care early during their medical training.
Health coaching involves skills that are interdisciplinary; as such, coaching opportunities should not be limited to medical students. A small study involving teaching students health coaching during a medical nutrition therapy course demonstrated promising results for both patients and students.15 When dietetic students coached families enrolled in a community-based nutrition course, student knowledge of coaching increased and families reported being very satisfied. Since use of allied health professionals is known to effectively improve medication adherence in hypertensive patients,16 different types of health professional students should also provide coaching for hypertensive patients.
As a result, Approach to Antihypertensive Adherence (AAA) was created as a pilot bilingual intervention to increase medication adherence in uninsured, hypertensive adults at a free clinic. It employed a teamwork approach to hypertension management, recruiting student health care providers (i.e., medical, nursing and pharmacy students) as health coaches for hypertensive patients. AAA aimed to utilize an abundant, free resource of the clinic (i.e., student volunteers) to combat medication non-adherence, a prevalent and powerful barrier in hypertension management.
Specific aims of this study were the following: (1) to collect pilot data on health coaching and medication adherence in hypertensive patients, (2) to demonstrate the feasibility and acceptability of this intervention for patients and coaches, and (3) to provide the first example of the incorporation of student health coaches into a primary care team for hypertensive patients, as implemented in a low resource, multicultural clinical setting.
Methods
Patient recruitment
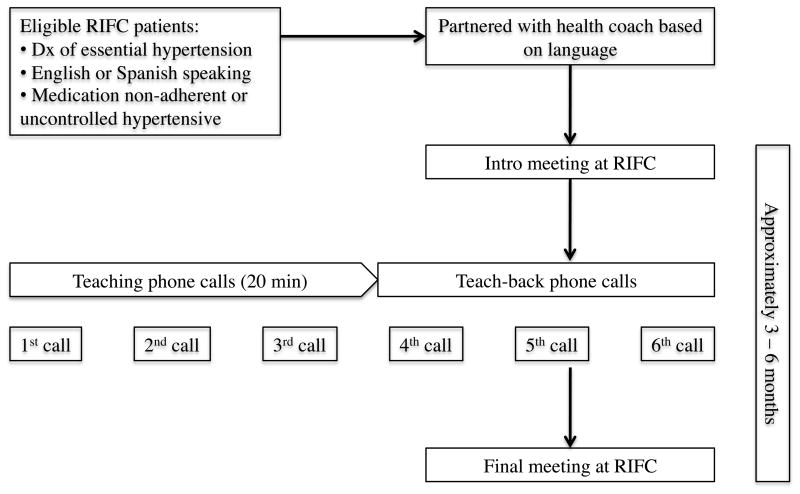
The study was conducted with patients from the Rhode Island Free Clinic (RIFC), a licensed ambulatory care facility in Providence, RI that exclusively serves uninsured state residents. Eligible patients were uninsured English- or Spanish-speaking adults (ages 19–64 years) with a diagnosis of essential hypertension (defined as BP >140/90 without known secondary cause). Patients were either identified as medication non-adherent by a RIFC health provider or as having uncontrolled hypertension. Uncontrolled hypertension was defined as having more than one recently documented high blood pressure (BP > 140/90).
Patient recruitment occurred through chart review (i.e., ICD-9 diagnosis of hypertension and repeat BPs >140/90) and direct referral by RIFC health providers (i.e., clinical suspicion of “medication non-adherence”) from June to August 2010. 30 eligible patients were approached in-person during a clinic visit about the study by one of the study investigators, with two refusing participation and with three who could not be scheduled (uptake rate = 93%). Participants provided informed consent in order to participate. Overall, 25 patients entered the study, with 12 (48%) completing the entire intervention (i.e., 2 visits, 6 phone calls). 88% of patients completed half (i.e., 1 visit, 3 phone calls) and 76% of patients almost completed (i.e., 1 visit, 6 phone calls). 13 (52%) of patients did not complete the intervention. Each patient received a pillbox upon entering the study; they received no other compensation for their participation.
Coach recruitment
Students, who were M.D., Pharm.D., or R.N. candidates, were offered the opportunity to volunteer as health coaches. Volunteers received two hours of interactive training from a multidisciplinary team of physicians, nurses and psychologists in the following: logistics (e.g., documentation, HIPAA), patient education (e.g., hypertension), patient-centered counseling (e.g., motivation interviewing, idiographic goal-setting), and medical care in Spanish when appropriate (e.g., cultural considerations, hypertension terminology).
Investigators sent one recruitment email message to a faculty contact at local pharmacy and nursing schools and directly to local first year medical students, which generated interested replies from 18 students. A total of 11 coaches (5 medical, 2 pharmacy, 4 nursing students) agreed to participate. Five of the coaches were bilingual in English and Spanish languages. Each coach was assigned an average of two patients, ranging from one to five. One coach dropped out mid-study for personal reasons. Health coaches received no monetary compensation for their services.
Intervention
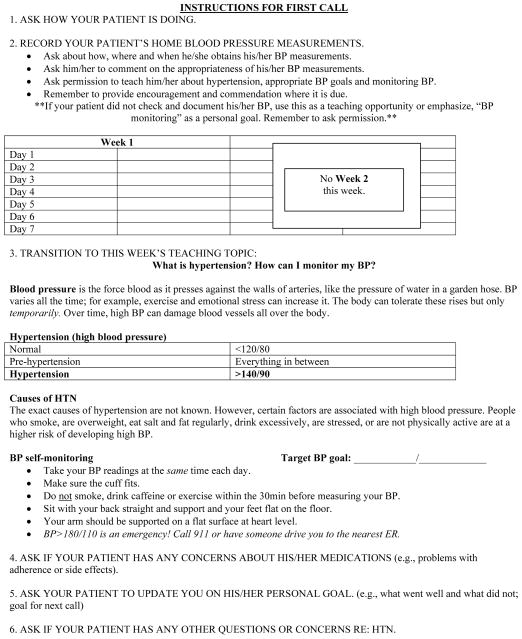
Patients were partnered with health coaches by investigators, based on language of preference and scheduling. With minimal training, student volunteers worked alongside RIFC providers, leaving detailed documentation in medical records on every patient encounter. During an introductory meeting, coaches reviewed current medications, discussed perceived barriers to adherence, explained proper medication use, gave instructions for home BP monitoring (or BP monitoring at local pharmacies) and encouraged at least one patient-selected lifestyle goal (e.g., exercise).
Next, patients received a series of six 20-minute telephone calls approximately every other week from their coaches. Using standardized protocols developed by investigators, coaches made calls to document patient BP measurements, concerns about medications, and progress on their lifestyle goal and to provide patients with appropriate support. The intervention lasted approximately three to six months, depending on patients’ accessibility by telephone. Coaches met their patients for a final time to review progress and conclude the intervention.
Evaluation design
Because AAA was a pilot study with a small sample, an uncontrolled open trial design was employed. Socio-demographic and health information was collected from medical charts of patients. Medication adherence and disease condition were assessed with two self-reports of adherence and with blood pressure. BP was an average of two systolic and diastolic measurements. Behavior change was additionally assessed with documentation of home BP monitoring and lifestyle goal progress during patient-coach encounters.
As a screening tool for the study and to characterize each patient’s baseline medication adherence level, the 8-item Morisky Scale was administered to patients by coaches during the introductory meeting.17 Because the scale was not designed to track adherence levels over time, no post-test Morisky score was recorded. This scale has been validated for use in low income, minority hypertensive patients, based on its ability to detect medication non-adherence as measured by BP (93% sensitivity, 53% specificity).
As a tool to monitor change in adherence level, the Brief Medication Questionnaire (BMQ) was administered to patients by coaches during both introductory and concluding meetings.18 The BMQ is a sensitive test of medication adherence, with its validity assessed using the Medication Events Monitoring System (MEMS), the “gold standard” of adherence measurement (Regimen and belief screens are 80–100% sensitivity for repeat non-adherence).18,19,20 The BMQ Adherence Risk Scale is a composite score of four screens, that can detect adherence barriers.
In qualitative evaluation of the intervention, two investigators unaffiliated with the intervention design conducted structured participant interviews and administered surveys after the intervention. Patients were interviewed in their language of choice with ten multiple-choice questions and four open-ended questions. Coaches were given structured interviews and electronic pre-interview questionnaires on each of their patients, including nine multiple-choice questions and five open-ended questions. Coaches were also asked to rate how successful their patients were in achieving their lifestyle goal.
Within-subject analyses of interval data were conducted with STATA 11.0 using paired t-tests. Between-subject analyses of interval data were conducted using independent sample t-tests. Within-subject analyses of dichotomous data (i.e., medication adherence) were conducted with McNemar’s tests. The study protocol was approved by the human research ethics committee at Brown University.
Results
Baseline (pre-test) results
A total of 25 hypertensive patients enrolled in AAA. Socio-demographic and health data revealed that most patients were Latino, received high school education or less, and were low-income. Notably, four of the 25 patients had co-morbid psychiatric diagnoses assessed by medical chart review and self-report of medical history (three depression, one depression and anxiety disorder).
At baseline (n = 25), 76% of patients had uncontrolled BP (mean = 141/89, SD = 17.7, 13.8). Enrolled patients took between 1.5 to 12 total pills (mean = 4.9, SD = 2.4) daily, with a range of one to five antihypertensive pills (mean = 2.2, SD = 1.2). They were prescribed the following antihypertensive medications: lisinopril (n = 10), hydrochlorothiazide (n = 10), metoprolol (n = 7), amlodipine (n = 5), atenolol (n = 4), hydrochlorothiazide/lisinopril (n = 4), quinapril (n = 2), valsartan (n = 1).
8-item Morisky scale scores ranged from 4 to 8 (mean = 6.6, SD = 1.3), indicating mean medium adherence (low adherence < 6). As expected, patients with controlled BPs had a higher mean Morisky score (mean = 7.5, SD = 0.55), compared to patients with uncontrolled BPs (mean = 6.3, SD = 1.34; t (24.01) = 3.11, P < 0.01).
Post-test results
Post-test data was collected on 12 patients, who completed the entire intervention. These patients did not differ from those who dropped out (n = 13) on any variable listed in Table 1.
Table 1.
Socio-demographic and Health Characteristics of Patients.
| Total (n=25) | Complete (n=12) | Drop out (n=13) | ||
|---|---|---|---|---|
| Systolic BP | 141 +/− 17.7 mmHg | 147 +/− 18.7 mmHg | 135 +/− 15.6 mmHg | |
| Diastolic BP | 89 +/− 13.8 mmHg | 92 +/− 17.4 mmHg | 86 +/− 9.0 mmHg | |
| Age | 54 +/− 6.7 years | 56 +/− 2.9 years | 53 +/− 8.8 yrs | |
| Gender | Male | 15 (60%) | 9 (75%) | 6 (46%) |
| Female | 10 (40%) | 3 (25%) | 7 (54%) | |
| Ethnicity | Black | 6 (24%) | 3 (25%) | 3 (23%) |
| Latino | 13 (52%) | 6 (50%) | 7 (54%) | |
| White | 6 (24%) | 3 (25%) | 3 (23%) | |
| Income | $0–9999 | 12 (48%) | 6 (50%) | 6 (46%) |
| $10–19999 | 10 (40%) | 5 (42%) | 5 (38%) | |
| >$20000 | 2 (8%) | 1 (8%) | 1 (8%) | |
| No response | 1 (4%) | 0 (0%) | 1 (8%) | |
| Marital status | Single | 9 (36%) | 3 (25%) | 6 (46%) |
| Married | 10 (40%) | 5 (42%) | 5 (38%) | |
| Divorced | 4 (16%) | 2 (17%) | 2 (15%) | |
| No response | 2 (8%) | 2 (17%) | 0 (0%) | |
| Education level | 8th grade or less | 3 (12%) | 0 (0%) | 3 (23%) |
| Some/graduate of high school | 13 (52%) | 8 (67%) | 5 (38%) | |
| Some/graduate of college | 5 (20%) | 3 (25%) | 2 (15%) | |
| Graduate school | 4 (16%) | 1 (8%) | 3 (23%) | |
| Body mass index | Overweight | 10 (40%) | 5 (42%) | 5 (38%) |
| Obese | 15 (60%) | 7 (58%) | 8 (62%) | |
| Tobacco use | Yes | 4 (16%) | 1 (8%) | 3 (23%) |
| No | 21 (84%) | 11 (92%) | 10 (77%) | |
| Excessive alcohol use* | Yes | 2 (8%) | 2 (17%) | 0 (0%) |
| No | 23 (92%) | 10 (83%) | 13 (100%) | |
| Language preference | Spanish | 11 (44%) | 6 (50%) | 5 (38%) |
| English | 14 (56%) | 6 (50%) | 8 (62%) |
Excessive alcohol use = >2 drinks per day for females or >3 drinks per day for males
Pre- and post-intervention adherence risk scale scores are presented in Table 2. Significant improvements were observed in medication adherence. Pre-post analysis of individual BMQ subscales (e.g., regimen, belief, recall and access screen) revealed that 92% of completed patients had a positive regimen screen at baseline. Following the intervention, only 25% screened positive on the regimen screen (McNemar P < 0.01), also indicating improved medication adherence. When considered individually, none of the three adherence barrier screens demonstrated a statistically significant trend in either direction (McNemar Ps = 0.375, 0.625, 1.000).
Table 2.
Pre- vs. Post-intervention BP and BMQ Adherence Scale
| Pre-intervention | Post-intervention | ||
|---|---|---|---|
| Mean Systolic BP (SD) | 146.5 (18.68) | 135.5 (18.34) | t(11) =2.02. P=.03 |
| Mean Diastolic BP (SD) | 91.67 (17.44) | 84.71 (6.52) | t(11) =1.33. P=ns |
| Mean BMQ Adherence Risk Scale (SD) | 2.33 (0.78) | 1.25 (0.87) | t(11) =3.03. P=<0.01 |
Pre- and post-intervention BP results are presented in Table 2. Significant improvements were observed in systolic BP. The pre-test mean BP of 147/92 (SD = 18.7, 17.4) was uncontrolled, compared to the post-test mean BP of 136/85 (SD = 18.3, 6.5) that was controlled. Patients with unchanged BMQ regimen screens (i.e., no change in medication adherence) had mean systolic BP increase of 5 mmHg (n = 4, SD = 15.6); however, those with changed BMQ regimen screens (i.e., switching from positive to negative screen, indicating increased medication adherence) had a mean decrease of 19 mmHg (n = 8, SD = 15.8; t(11) = 2.41, P = 0.02).
According to patient self-report, 75% of patients increased frequency of home BP monitoring by ≥ 100% between pre and post-intervention. ≥92% of patients reported making progress towards lifestyle goals, which consisted of the following: increase exercise (n = 6), improve diet (n = 4), weight loss (n = 1), reduction in alcohol use (n = 1). On a scale 1 to 10 (10 = most successful), coaches rated their patients a mean of 6.5 (SD = 2.5) at achieving their lifestyle goal.
Fourteen of the 25 enrolled patients, including all 12 who completed the entire intervention, were reached for a post-intervention interview. Over 90% of patients reported that AAA had a positive influence on three key domains related to health behavior. Those domains were the following: (1) Self-efficacy, feeling able to make changes to improve hypertension, (2) Knowledge, figuring out healthy choices to improve hypertension, (3) Awareness, feeling motivated to pay more attention to hypertension. When asked to describe AAA to a friend, patients offered the following responses: “It gets you on track to get your BP under control,” “I learned a few things to not harm my body,” “I’ve had hypertension for a while and sometimes you don’t know why,” “I am more aware of the danger [of hypertension].”
Coaches reported “never” or “sometimes” getting frustrated (92%), with only 1 out 12 reporting “often” getting frustrated. They were frustrated for the following reasons: difficulty finding a good time to talk with patient (most frequently listed reason), difficulty communicating to patient in a way he/she could understand, difficulty getting patient to listen and cooperate with goal-setting, difficulty getting patient to change after he/she had committed to change.
In addition to the standardized protocols, coaches reported using the following adjunctive techniques to communicate with patients: spoke slowly and simply, asked open-ended questions, asked the patient to summarize, spoke in lay terms, focused on patient-relevant concerns in hypertension (e.g., where to take home BP measurements). Coaches used different methods to teach about hypertension, such as role-playing with patients or drawing images of pipes/hoses to convey BP. Consistent with patient-centered care, one coach remarked that goals needed to be “set up so that it’s the patient’s idea.”
Comment
Despite pharmacologic advances in the treatment of hypertension, medication non-adherence continues to challenge primary care providers in BP management. This is a salient issue among uninsured, multicultural hypertensive patients in low-resource ambulatory clinics. Thus, cost-effective primary care innovation is needed to improve hypertension management.
This feasibility study suggests that incorporating student health coaches into primary care teams for uninsured hypertensive patients may have promise for increasing medication adherence and other healthy behaviors. In our sample AAA’s effect on self-reported medication adherence was statistically significant, in accordance with coaches’ pre-post impressions of patients’ motivation to adhere to medications. There were also documented patient gains in home BP monitoring frequency and in achievement of lifestyle changes (e.g., exercise, healthy diet). Furthermore, there were self-reported gains by patients in self-efficacy, knowledge, and awareness which are key domains related to health behavior.
Improvements in medication adherence or other healthy behavior change may explain the observed statistically significant decline in BP for patients who completed the intervention. Medication adherence has specifically been documented in literature to reduce BP.21 Although our demonstrated decrease in BP was modest, it has been documented that even the most effective of interventions do not lead to large decreases in BP.16
Patients were generally satisfied with health coaching. In addition to reporting satisfaction with timing, method and amount of coaching, patients provided agreeable quotations when asked to describe the intervention to a friend. Many patients requested continued access to health coaching after the intervention’s conclusion, a likely indicator of their satisfaction with the intervention.
In addition to its promising impact on patients, use of students as health coaches and their incorporation into primary care teams appears feasible. Despite minimal training, coaches supplied quotations at the conclusion of the intervention, which suggested that they had a good grasp of patient-centered care for their level of clinical training. Moreover, students reported learning important realities surrounding chronic disease management early in training (e.g., importance of patient-provider communication).
There are several limitations to this study. As this is a feasibility study, an uncontrolled open trial design was used. In addition, the sample size of completers in this study is small. Thus, one should not draw conclusions regarding treatment efficacy from study results. Nevertheless, promising findings were observed in BP reduction, medication adherence, healthy behavior change, and patient satisfaction. These findings speak to the feasibility of a student coach model and suggest that future research is warranted.
Another limitation was our loss to follow-up rate of 52%. In previous studies that examine medication adherence in hypertensive patients, similarly high loss to follow-up rates were observed.22,23 Of the few studies on student health coaches, the rates were even higher, with one reporting a loss to follow-up rate of 67%.13 Furthermore, this study was conducted in a low income, urban, free clinic which raises unique barriers to contacting patients for follow-up assessments (e.g., unstable mailing addresses, phone service outages due to unpaid bills). Thus, our loss to follow-up rate may be expected for this treatment context. Our loss to follow-up rate may have been mitigated if we attempted to contact patients more frequently; however, student coach flexibility was constrained by their limited time as volunteers. In addition, this study did not pay participants to complete assessments.
Since depression is a known barrier to medication adherence,24,25 our lack of depression measurement is a limitation. We did assess whether or not a psychiatric diagnosis was listed in medical records and asked patients to self-report psychiatric diagnosis history. However, this method likely missed some current psychiatric diagnoses and sub-diagnostic threshold symptomatology. Future work should include a measure of depression severity.
Because our sample was predominantly Latino, certain methodological challenges should be addressed. Researchers have found that Latinos, especially those of low socioeconomic status and education level, are more likely to convey agreement than the general population, a type of response bias called acquiescence.26,27 In order to mitigate this bias, some contradictory or negatively worded items were included in the instrument assessing patient satisfaction, which was administered by a researcher of similar cultural background.
Based on our evaluation results, several changes to the intervention may be considered. First, despite an observed increase in adherence level, coaching did not appear to decrease perceived barriers to adherence. Adding specific techniques to problem-solve barriers may be fruitful. Second, as suggested by patients, the intervention could provide for continued contact with a health coach after the intervention period in the event that patients relapse to unhealthy habits. Third, we may decrease our loss to follow-up rate of patients if we provided financial incentive for completion of the intervention. While such incentives would increase internal validity, they would decrease external validity.
Further research is needed to better analyze the impact of health coaching. An updated version of AAA can be compared to treatment as usual for a larger sample of medication non-adherent hypertensive patients. Research in the distant future may measure intervention sustainability and assess various hypertension morbidities (e.g., stroke, myocardial infarction). Moreover, it would be valuable to research the effectiveness of student health coaching, as compared to other health coaching models, and its educational value for health professional students.
In conclusion, this study suggests that student volunteers are an untapped resource that may be feasibly and acceptably incorporated into primary care teams caring for hypertensive patients. Student health coaching may be a cost-effective innovation in combating medication non-adherence in the uninsured. Since the study protocol was designed to be simple and of minimal cost, this intervention can be reasonably replicated in other low-resource, multicultural ambulatory clinics. This study shows promise that student health coaching may provide a dual opportunity to educate and support vulnerable patients while actively engaging trainees in primary care medicine.
Figure 1.
Sample of AAA protocol.
Figure 2.
AAA model.
Table 3.
Patient Satisfaction.
| Not at all % (N) | A little % (N) | Somewhat % (N) | Very much % (N) | |
|---|---|---|---|---|
| Self-efficacy | ||||
| Talking to my counselor made me feel more confident that I can improve my hypertension | --- | --- | 7.1 (1) | 92.9 (13) |
| The counselor made me feel like I am able to make changes to my hypertension | --- | --- | 7.1 (1) | 92.9 (13) |
|
| ||||
| Knowledge | ||||
| I learned important facts about hypertension from my counselor | --- | 7.1 (1) | 21.4 (3) | 71.4 (10) |
| The counselor helped me figure out healthy choices I can make to improve my hypertension | --- | --- | 7.1 (1) | 92.9 (13) |
|
| ||||
| Awareness | ||||
| Talking to my counselor motivated me to pay more attention to my hypertension | 7.1 (1) | --- | --- | 92.9 (13) |
|
| ||||
| Patient Satisfaction | ||||
| I felt that the counselor understood how I feel about having hypertension | --- | 14.3 (2) | 7.1 (1) | 78.5 (11) |
| The counselor ignored the concerns I have about my hypertension medication | 78.5 (11) | 21.4 (3) | ||
| I felt like I was being told what to do about my hypertension | 57.1 (8) | 7.1 (1) | 14.2 (2) | 21.4 (3) |
|
| ||||
| % (N) | ||||
|
| ||||
| I felt the calls were “just right” | 92.8 (13) | |||
| The amount of information I received was “just right” | 100 (14) | |||
| I prefer that the intervention be delivered via phone | 92.8% (13) | |||
Acknowledgments
Funding statement: This research was supported by a research fellowship from the Arnold P. Gold Foundation. The preparation of this manuscript was supported by K23-HL107391 to A. Busch from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
The authors acknowledge all the students who served as coaches for this study. The authors also acknowledge David Margolius and his University of California San Francisco colleagues for assistance in developing health coach training materials.
Footnotes
Conflicting and completing interests: None
References
- 1.Kotchen Theodore A. Hypertensive Vascular Disease. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine, 17e [Internet] McGraw-Hill; c2008. [Accessed February 7 2010]. http://www.accessmedicine.com/content.aspx?aID=2872428.chapter.241. [Google Scholar]
- 2.Brookes L. National health and nutrition examination survey (NHANES) data on hypertension [Internet] [Accessed Feb 7, 2010];Medscape. 2003 http://www.medscape.com/viewarticle/456437. Updated May 7, 2003.
- 3.Collins OR, Peto R. Antihypertensive drug therapy: effects on stroke and coronary heart disease. In: Swales JD, editor. Textbook of hypertension. Oxford: Blackwell Scientific Publications; 1994. pp. 1156–64. [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Bodenheimer T. A 63-year-old man with multiple cardiovascular risk factors and poor adherence to treatment plans. JAMA. 2007;298(17):2048–2056. doi: 10.1001/jama.298.16.jrr70000. [DOI] [PubMed] [Google Scholar]
- 6.Cutler DM, Everett W. Thinking outside the pillbox — medication adherence as a priority for health care reform. N Engl J Med. 2010;362(17):1552–55. doi: 10.1056/NEJMp1002305. [DOI] [PubMed] [Google Scholar]
- 7.Dowell J, Jones A, Snadden D. Exploring medication use to seek concordance with ‘non-adherent’ patients: a qualitative study. British Journal of General Practice. 2002;52:24–32. [PMC free article] [PubMed] [Google Scholar]
- 8.Ebrahim S. Detection, adherence and control of hypertension for the prevention of stroke: a systematic review. Health Technology Assessment. 1998;2(11) [PubMed] [Google Scholar]
- 9.Kaplan RC, Bhalodkar NC, Brown EJ, Jr, et al. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Prev Med. 2004;39(6):1249–1255. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- 10.Bennett HD, Coleman EA, Parry C, Bodenheimer T, Chen EH. Health coaching for patients with chronic illness. Family Practice Management. 2010;17(5):24–9. [PubMed] [Google Scholar]
- 11.Vale MJ, Jelinek MV, Best JD, et al. Coaching patients on achieving cardiovascular health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163:2775–83. doi: 10.1001/archinte.163.22.2775. [DOI] [PubMed] [Google Scholar]
- 12.Two Feathers J, Kieffer EC, Palmisano G, et al. Racial and ethnic approaches to community health (REACH) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health. 2005;95:1552–1560. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sacco WP, Malone JI, Morrison AD, Friedman A, Wells K. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med. 2009;32:349–359. doi: 10.1007/s10865-009-9209-4. [DOI] [PubMed] [Google Scholar]
- 14.Wagner PJ, Jester DM, Moseley GC. Medical students as health coaches. Academic Medicine. 2002;77(11):1164–5. [PubMed] [Google Scholar]
- 15.Sheehan-Smith L, Brinthaupt TM. Using service-learning to teach health coaching. Academic Exchange Quarterly [Internet] 2010;14(2) [cited 2011 Apr 13] Available from: http://www.rapidintellect.com/AEQweb/cho4529.htm.
- 16.Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database Syst Rev. 2004;(2):CD004804. doi: 10.1002/14651858.CD004804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morisky DE, Ang A, Krousel-Wood M, Ward H. Predictive validity of a medication adherence measure for hypertension control. Journal of Clinical Hypertension. 2008;10(5):348–354. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The brief medication questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Education and Counseling. 1999;37:113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 19.Urquhart J. The electronic medication event monitor - lessons for pharmacotherapy. Clinical Pharmacokinetics. 1997;32:345–356. doi: 10.2165/00003088-199732050-00001. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton GA. Measuring adherence in a hypertension clinical trial. Eur J Cardiovasc Nurs. 2003;2:219–228. doi: 10.1016/S1474-5151(03)00058-6. [DOI] [PubMed] [Google Scholar]
- 21.Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Current Opinion in Cardiology. 2004;19(4):357–362. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- 22.Kerr JAC. Adherence and self-care. Heart and Lung. 1985;14(1):24–31. [PubMed] [Google Scholar]
- 23.Rehder T, McCoy L, Blackwell W, Whitehead W, Robinson A. Improving medication compliance by counseling and special prescription calendar. American Journal of Hospital Pharmacy. 1980;37:379–85. [PubMed] [Google Scholar]
- 24.Krousel-Wood M, Islam T, Muntner P, et al. Association of depression with antihypertensive medication adherence in older adults: cross-sectional and longitudinal findings from CoSMO. Ann Behav Med. 2010 Dec;40(3):248–57. doi: 10.1007/s12160-010-9217-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pompili M, Serafini G, Del Casale A, Rigucci S, Innamorati M, Girardi P, Tatarelli R, Lester D. Improving adherence in mood disorders: the struggle against relapse, recurrence and suicide risk. Expert Rev Neurother. 2009 Jul;9(7):985–1004. doi: 10.1586/ern.09.62. [DOI] [PubMed] [Google Scholar]
- 26.Lange JW. Methodological concerns for non-Hispanic investigators conducting research with Hispanic Americans. Res Nurs Health. 2002;25:411–419. doi: 10.1002/nur.10049. [DOI] [PubMed] [Google Scholar]
- 27.Aday LA, Chiu GY, Andersen R. Methodological issues in health care surveys of the Spanish heritage population. Am J Public Health. 1980;70:367e74. doi: 10.2105/ajph.70.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]