Abstract
B cells are important for the regulation of autoimmune responses. In experimental autoimmune encephalomyelitis (EAE), B cells are required for spontaneous recovery in acute models. Production of IL-10 by regulatory B cells has been shown to modulate the severity EAE and other autoimmune diseases. Previously, we suggested that B cells regulated the number of CD4+Foxp3+ T regulatory cells (Treg) in the CNS during EAE. Since Treg suppress autoimmune responses, we asked whether B cells control autoimmunity by maintenance of Treg numbers. B cell deficiency achieved either genetically (μMT) or by depletion with anti-CD20 resulted in a significant reduction in the number of peripheral, but not thymic Treg. Adoptive transfer of WT B cells into μMT mice restored both Treg numbers and recovery from EAE. When we investigated the mechanism whereby B cells induce the proliferation of Treg and EAE recovery, we found that glucocorticoid-induced TNF ligand (GITRL), but not IL-10, expression by B cells was required. Of clinical significance is the finding that anti-CD20 depletion of B cells accelerated spontaneous EAE and colitis. Our results demonstrate that B cells play a major role in immune tolerance required for the prevention of autoimmunity by maintenance of Treg via their expression of GITRL.
Introduction
B cells functionally contribute to both innate and adaptive immune responses by contributing to antigen presentation and through antibody production. The first evidence for the existence of regulatory B cells in autoimmunity was obtained using the mouse model of multiple sclerosis (MS), experimental autoimmune encephalomyelitis (EAE). We showed that following EAE induction by immunization with the myelin basic protein (MBP) peptide Ac1-11, B10.PL mice deficient in peripheral B cells (μMT) failed to undergo spontaneous recovery and exhibited chronic disease (1, 2). These studies were replicated in C57BL/6 μMT mice immunized with a myelin oligodendrocyte glycoprotein peptide containing residues 35–55 (MOG35–55) (3). This same study showed that B cell production of IL-10 was required for their regulatory function (3). A role for B cell-derived IL-10 in suppressing autoimmunity has also been reported in models of arthritis and lupus (4). Regulatory B cells have also been reported in humans (4). Recently, the role of B cells in autoimmune diseases has been further studied by their depletion using anti-CD20, which targets B cells from the pre-B cell to memory stages. Plasma cells, which do not express CD20, are not eliminated. In EAE, anti-CD20 depletion of B cells prior to induction of EAE with MOG35–55 recapitulated chronic disease observed in μMT mice (5). However, in humans, treatment of MS with anti-CD20 (Rituximab) resulted in a significant reduction in the number of gandolinium-enhancing lesions, providing evidence that B cells play a pathogenic role in MS (6, 7). Evidence that Rituximab also depletes regulatory B cells are reports that its treatment for autoimmunity has lead to severe exacerbation of colitis and the spontaneous onset of colitis and psoriasis soon after the start of treatment (2, 8–10). Treatment of non-Hodgkin’s lymphoma with Rituximab, has also been associated with the onset of autoimmunity (11).
Although the mechanism whereby B cell depletion results in spontaneous autoimmunity is not known, a link with CD4+FoxP3+ T regulatory cells (Treg) is possible. Both humans and mice with mutations in FoxP3 spontaneously develop autoimmune disorders at a young age, which is now known to be due a deficiency in Treg (12). In addition, the adoptive transfer of Treg has been shown to significantly reduce the severity of EAE (13). Also in EAE, we showed that μMT mice had a reduction in the percentage of Treg in the CNS (14). A subsequent study further demonstrated a critical role for Treg in inhibiting late-phase EAE disease (15). Although the later study did not investigate B cell:Treg interactions, both μMT and anti-CD20-depleted mice have been shown to have reduced percentages of peripheral FoxP3+ Treg (16, 17). However, the absolute number of Treg was not determined. Other studies have provided strong evidence that B cells regulate Treg numbers by the induction of FoxP3 expression (iTreg) using both in vitro and in vivo models by several mechanisms including B cell production of IL-10 and TGF-β (18–20). However, it is not known if B cells can also regulate the number of natural Treg (nTreg), which develop within the thymus (21).
The homeostasis of Treg in the periphery has been shown to be dependent upon the presence of dendritic cells (22). TCR ligation fails to induce Treg expansion in a similar manner as observed in conventional naïve T cells (12). However, a role for glucocorticoid-induced TNF receptor family-related protein (GITR) in Treg expansion has been described (23). GITRL expressing cells include dendritic cells, macrophages and B cells (24). Although it is not known whether GITRL-expressing cells play a role in nTreg homeostasis in WT mice, transgenic mice bearing a B cell-specific GITRL transgene had significantly increased numbers of peripheral FoxP3+ Treg (23), suggesting that B cells could play a role in nTreg homeostasis.
Here, we asked whether B cells regulate autoimmunity via interactions with Treg. To address this question, we asked whether mice genetically susceptible to spontaneous autoimmunity would succumb to disease following B cell depletion with anti-CD20. We found that B cell depletion resulted in the rapid onset of both EAE and colitis, which was accompanied by a significant reduction in the number of peripheral Treg. From these data we further hypothesized that B cells control autoimmunity through the maintenance of Treg numbers. In support of this hypothesis, we found that μMT mice had a significant reduction in the absolute number of Treg that was recapitulated by anti-CD20 B cell depletion in WT mice. Consistent with a reduction in Treg numbers, anti-CD20-depleted mice exhibited chronic EAE, similar to μMT mice. We found that B cell expression of GITRL, but not IL-10, induced Treg proliferation allowing the homeostatic maintenance of peripheral Treg numbers. Furthermore, we showed that restoration of Treg numbers in μMT mice with WT or IL-10−/− B cells resulted in spontaneous recovery, whereas mice that received GITRL-blocked B cells exhibited chronic EAE similar to μMT mice. Our results demonstrate that B cells via expression of GITRL play an essential role in nTreg homeostasis by maintaining their numbers above a threshold required for the prevention of autoimmunity.
Materials and Methods
Mice
B10.PL (H-2u) WT mice, B6.129P2-Il10tm1Cgn/J (IL-10−/−) and B6.SJL-Ptprca Pep3b/BoyJ (CD45.1+) mice on the C57BL/6 (H-2b) background were purchased from The Jackson Laboratory (Bar Harbor, ME). B6.Cg-FoxP3tm2Tch/J mice (FoxP3EGFP) were generated as described (25). B cell deficient B10.PL mice (μMT), MBP-TCR transgenic mice and generation of mixed bone marrow (BM) chimera mice were previously described (1, 14). FoxP3EGFP and knockout mice were backcrossed to B10.PL for three generations and then intercrossed and were housed and bred within the animal facility of the Medical college of Wisconsin (MCW). All animal protocols were approved by the MCW Institutional Animal Care and Use Committee.
B cell depletion in vivo
B cell depleting anti-mouse-CD20 mAb (18B12IgG2a) and its corresponding isotype control (2B8 msIgG2a) were provided by Biogen Idec. 250 μg of antibody was i.v. injected into mice, once, or twice, 14 days apart. B cell depletion kinetics were as previously reported (26).
Peptide and antibodies
MBP Ac1–11 peptide (Ac-ASQKRPSQRSK) was generated by the Protein Core laboratory of the Blood Research Institute, BloodCenter of Wisconsin. The 2.4G2 and Y19 hybridomas were obtained from American Tissue Culture Collection. Mouse specific CD4-Apc-eFluor 780, CD25-Alexa Fluor 700, TCR-β-FITC, CD11b-PE, IL-17-Alexa Fluor 647 were purchased from eBioscience (San Diego, CA). Mouse specific B220-PE-Texas Red, IFN-γ-PE, Vβ8.1,8.2- FITC and anti-human Ki-67-FITC and anti-BrdU-APC were purchased from BD Biosciences (San Diego, CA). Anti-mouse CD25-PE-Cy7 and anti-mouse GITRL-PE were purchased from Biolegend (San Diego, CA). Anti-mouse GITRL (YGL 386) was provided by Biolegend (San Diego, CA). F(ab′)2 fragment of goat anti-mouse IgM was obtained from Jackson ImmunoResearch Laboratories (West Grove, PA).
EAE induction
EAE was induced by the i.v. adoptive transfer of 1 × 106 MBP-specific encephalitogenic T cells activated in vitro with MBP Ac1–11 peptide into sublethally irradiated (360–380 rad) mice as described (14). Clinical symptoms of EAE were scored daily as follows: 0, no disease; 1, limp tail; 1.5, hind limb ataxia; 2, hind limb paresis; 2.5, partial hind limb paralysis; 3, total hind limb paralysis; 4, hind and fore limb paralysis; and 5, death.
Adoptive transfer of B cells
Splenic B cells from 8–10 week old mice were purified by complement depletion of T cells using anti-Thy 1 and rabbit complement (Pel-Freez biological, Rogers, AR) (27) followed by removal of adherent cells by incubating in serum-coated petridishes at 37 °C for 30 min. B cell purities were ~ 95% as determined by flow cytometry. GITRL was blocked by incubating cells with anti-mouse GITRL (10 μg/ml) at 4 °C for 60 min. Following washing in PBS, 15–25 × 106 cells were i.v. injected into each recipient mouse. EAE was induced three days later or splenic CD4+FoxP3+ cells were enumerated on day ten. To determine proliferation of CD4+FoxP3+ cells, BrdU (0.8 mg/ml) (Sigma, St. Louis, MO) was added to the drinking water for seven days.
B cell-mediated maintenance and proliferation of Tregs in vivo
Splenic EGFP+ Tregs were sorted from WT FoxP3EGFP mice and labeled with 3 μM Cell Proliferation Dye eFluor® 670 (eBioscience, San Diego, CA). 0.2 × 106 Tregs with or without 20 × 106 purified B cells were i.v. transferred into μMT recipient mice. Seven days later, absolute numbers and proliferation of splenic CD4+EGFP+ cells was determined.
Cell isolation, flow cytometry and cell sorting
Mice were perfused with PBS and the brain and spinal cord were dissected and homogenized. Mononuclear cells were isolated using 40/70% discontinuous Percoll gradients (Sigma-Aldrich, St. Louis, MO). Single cell suspensions from lymph nodes and spleen were obtained, counted and 0.2–1 × 106 cells were incubated with anti-CD16/CD32 (clone 2.4G2) (Fc block) for 15 min followed by cell surface staining. Intracellular FoxP3 staining was performed using an anti-mouse/rat FoxP3-PE staining kit from eBioscience (San Diego, CA), as per manufacturer instructions. Cells were acquired on a LSRII flow cytometer (BD Biosciences, San Diego, CA) and data were analyzed using FlowJo software (Tree Star, Inc., Ashland, OR). Fluorochrome labeled and/or EGFP expressing cells were sorted using a FACSAriacell-sorter (BD Biosciences, San Diego, CA).
Detection of intracellular cytokines
Isolated cells were stimulated in vitro with PMA (50 ng/ml) and ionomycin (600 ng/ml) (both from Sigma-Aldrich, St. Louis, MO) for 4 hr in the presence of monensin (BD Biosciences, San Diego, CA). Cells were surface stained, fixed and permeabilized and stained for intracellular cytokines using the FoxP3 staining buffer set from eBioscience (San Diego, CA).
Histolological analysis
Small and large intestine were fixed, paraffin embedded and 5 μm sections were stained with hematoxylin and eosin.
T cell suppression assay
Splenic CD4+CD25− cells from WT (CD45.1) mice were sorted and labeled with 3 μM carboxyfluorescein diacetate, succinimidyl ester (CFSE) (Molecular Probes, Invitrogen). EGFP+ Tregs (CD45.2) were sorted from WT FoxP3EGFP and μMT FoxP3EGFP mice. CD4+CD25− cells (1 × 105) were cultured alone or with Tregs from WT or μMT mice in different ratios for 96 hr. Anti-CD3 (2 μg/ml) and irradiated (3000 rad) T cell depleted syngeneic splenocytes (1 × 105) were added into each well. Percentages of proliferating CD4+CD45.1+ cells were determined by CFSE dye dilution by flow cytometry.
In vitro co-culture of B cells and Treg
Purified splenic B cells were activated in vitro with 5 μg/ml anti-IgM for 48 hr. CD4+EGFP+ Treg from FoxP3EGFP mice were sorted and labeled with 3 μM Cell Proliferation Dye eFluor® 670 (eBioscience, San Diego, CA). Treg (0.5 × 105) alone or Treg mixed with naïve or anti-IgM activated B cells (1 × 105) were cultured in the presence of soluble anti-CD3 (2 μg/ml) and irradiated (3000 rad) APC (1–2 × 105) for 96 hr. Post culture, the cells were stained with CD4 and percentages of EGFP+ cells gated on CD4+ cells were determined by flow cytometry.
Statistical analysis
Data were analyzed using GraphPad prism software and were presented as mean ± SEM. Statistical significance was determined using the nonparametric Mann-Whitney test or unpaired t-test. p-values <0.05 were considered significant. The cumulative disease score was calculated by adding the daily EAE scores from day 7 to the end of the experiment on day 25 (Fig. 3B) or day 30 (Fig. 7C) post-EAE induction.
Figure 3. Reduced Treg due to B cell depletion with anti-CD20 leads to unresolved EAE.
A–F) B10.PL mice in groups of 3–4 were i.v. administered anti-CD20 (18B12IgG2a) or its isotype control (2B8msIgG2a), twice, 14 days apart (A, black arrows). EAE was induced three days after the first antibody treatment by adoptive transfer of 1 × 106 encephalitogenic T cells. Clinical signs of EAE were evaluated daily (A). The cumulative disease score (B) and disease score on day 25 of EAE (C) are shown. (D–F) At the peak of EAE disease, the absolute number of CNS CD4+Vβ8.2+ T cells (D) and splenic (E) and CNS (F) CD4+FoxP3+ Treg was determined by flow cytometry. Pooled data from 2–3 independent experiments with 6–10 mice in each group are shown. G) B10.PL mice in groups of 3–4 were i.v. administered anti-CD20 (18B12IgG2a) or its isotype control (2B8msIgG2a), twice, 14 days apart. Five days after the second antibody treatment, the absolute number of CD4+FoxP3+ Treg in the spleen was determined by flow cytometry. H) The absolute number of CD4+FoxP3+ Treg in the spleen and inguinal lymph node of WT and μMT mice was determined by flow cytometry. Pooled data from 2–3 independent experiments are shown (G, H). N = 6–10 mice (G) or 3–5 mice (H) in each group. I) The average (± SEM) mean fluorescence intensity (MFI) of CD25 on splenic Treg (CD4+FoxP3+) from WT and μMT mice is shown. J) The suppressive capacity of WT and μMT Treg was measured in an in vitro assay using CD4+CD25− responder (Tresp) cells from CD45.1 mice (labeled with CFSE) and EGFP+ Treg sorted from the spleens of WT FoxP3EGFP and μMT FoxP3EGFP mice (CD45.2). Proliferation of responder cells stimulated with anti-CD3 in the presence or absence of Treg was determined by CFSE dye dilution by flow cytometry. Percent suppression at different Tresp:Treg ratios is shown. Pooled data from 2–3 independent experiments (I) or an average of two independent experiments (J) are shown. *p<0.05, **p<0.01.
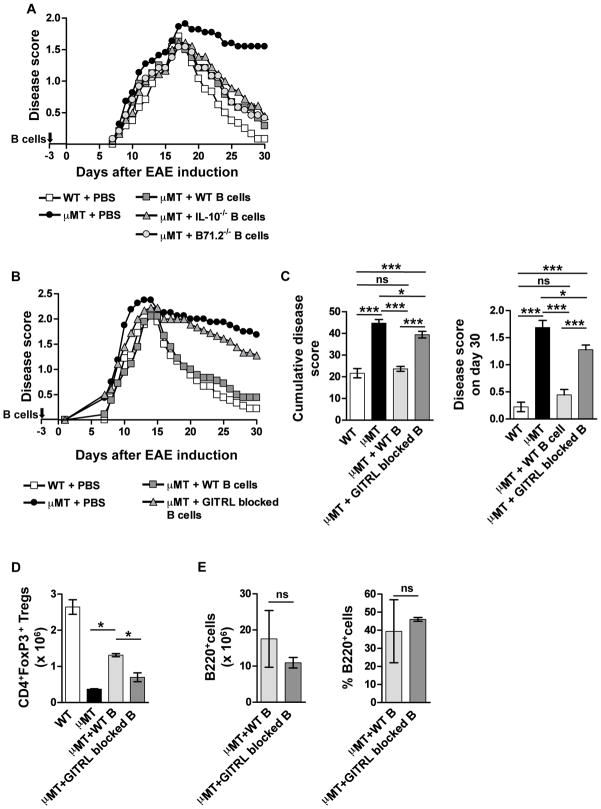
Figure 7. B cell expression of GITRL, but not IL-10 or B7, is required for the resolution of EAE.
20 × 106 splenic B cells from WT (A–E), IL-10−/− (A), B71.2−/− (A) mice or GITRL-blocked WT B cells (B–E) were i.v. transferred into groups of μMT mice. Three days post-transfer, EAE was induced and the mice were scored daily for clinical signs of disease (A, B). C) The cumulative disease score (mean ± SEM, left panel) and the final disease score on day 30 post-EAE induction (mean ± SEM, right panel) are shown. D, E) The absolute number (mean ± SEM) of splenic CD4+FoxP3+ Treg (D) and the absolute number (mean ± SEM) and percentage of B220+ cells in the spleen (E) on day 30 post-EAE induction were determined by flow cytometry. Pooled data from 2–3 independent experiments with 6–10 mice per group (A–C) or data from one experiment with 3 mice per group (D, E) is shown. *p<0.05, ***p<0.001.
Results
Anti-CD20 depletion of B cells results in accelerated onset of spontaneous autoimmunity
The depletion of B cells with anti-CD20 (Rituximab) is being increasingly used for the treatment of autoimmunity. Because a small subset of patients treated with anti-CD20 spontaneously developed autoimmunity (2, 8–10), we asked whether B cell depletion put a mouse susceptible to spontaneous autoimmunity at increased risk to develop disease. TCR transgenic mice specific for MBP (MBP-TCR) have been shown to develop spontaneous EAE, especially when housed under non-SPF conditions (28–30). In our colony with strict SPF conditions, spontaneous EAE is very rare and does not occur under 12 weeks of age. The treatment of six week old MBP-TCR transgenic mice with anti-CD20 treatment exhibited signs of EAE as early as seven days later that continued to progress (Fig. 1A). Consistent with EAE induction, encephalitogenic T cells were present in the CNS (Fig. 1B), displayed an activated CD25+ phenotype (Fig. 1C) and produced IL-17 and IFN-γ (Fig. 1D). Since the onset of spontaneous autoimmunity is consistent with a deficiency in Treg, we next determined that anti-CD20 treatment resulted in a reduction in the percentage of CD4+ cells co-expressing FoxP3 (Fig. 1E) and in the absolute number of splenic Treg numbers (Fig. 1F).
Figure 1. B cell depletion leads to spontaneous EAE in mice susceptible to autoimmunity.
Groups of 3–4 MBP-TCR transgenic at six weeks of age were administered anti-CD20 (18B12IgG2a) or its isotype control (2B8msIgG2a) on day 0. Clinical signs of EAE were scored daily (A). On day 17–21 post-antibody injection the absolute number of CNS encephalitogenic T cells (CD4+Vβ8.2+) (B) and those expressing CD25 (C) and IL-17 (x-axis) and IFN-γ (y-axis) (D) was determined by flow cytometry. The percentage of cells producing each cytokine is indicated. A representative dot plot showing the percentage of CD4-gated cells expressing FoxP3 is shown (E). The absolute number of splenic Treg was also determined at the same timepoint (F). Pooled or representative data from 2–4 independent experiments with 3–9 mice in each group is shown. *p<0.05, ***p<0.001.
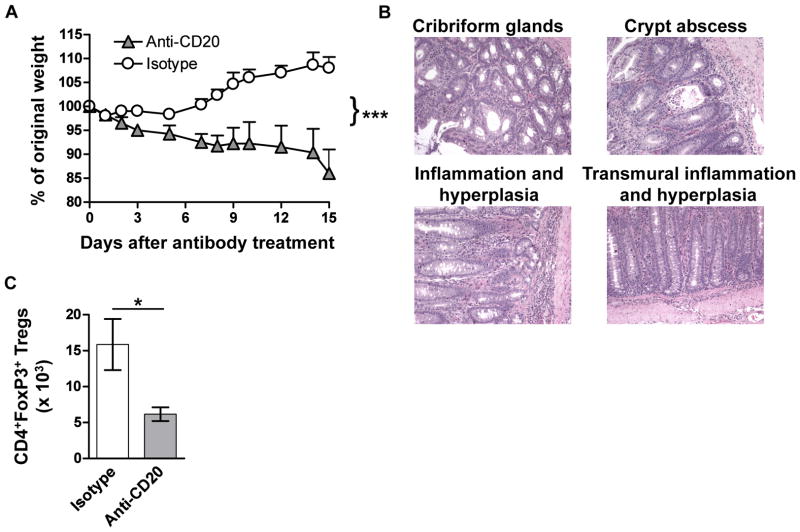
To further demonstrate that B cells play a fundamental role in maintaining autoimmune tolerance, we asked whether B cell depletion would accelerate the onset of colitis in IL-10−/− mice (31). We found that a single injection of anti-CD20 resulted in severe colitis by day 15, as evidenced by significant weight loss (Fig. 2A) and histopathology of the colon (Fig. 2B). Anti-CD20, but not isotype control-treated mice, also developed rectal prolapse by day 15 (data not shown) and had significantly reduced numbers of Treg in the Peyer’s Patch (Fig. 2C). These data demonstrate that B cells play a gate-keeping role in the prevention of autoimmunity by controlling the number of Treg.
Figure 2. B cell depletion leads to accelerated colitis in IL-10−/− mice.
Groups of 3–4 IL-10−/− mice at six weeks of age were administered anti-CD20 (18B12IgG2a) or its isotype control (2B8msIgG2a) on day 0. Mice were weighed daily and the percentage of the starting weight is shown (A). Representative histopathology of the colon from anti-CD20 treated IL-10−/− mice (200x) is shown (B). The absolute number of CD4+FoxP3+ Treg in the Peyer’s patches was determined by flow cytometry (C). Pooled or representative data from 2–4 independent experiments with 3–9 mice in each group is shown. *p<0.05, ***p<0.001.
B cell depletion with anti-CD20 results in chronic EAE and reduced numbers of Treg
If B cell regulation of Treg numbers is a critical factor in the regulation of EAE, then anti-CD20 B cell-depleted mice should exhibit chronic EAE. For these studies, we induced EAE by adoptive transfer instead of active immunization to avoid stimulation of immune cell subsets, including B cells, with TLR ligands present in CFA. As shown in Fig. 3A, when EAE was induced in anti-CD20 treated mice, disease onset and peak severity were similar to the isotype control group, and like μMT mice, were unable to resolve EAE (1, 3, 14). In addition, the anti-CD20 group had a significant increase in both the cumulative (Fig. 3B) and final EAE disease score (Fig. 3C), which was accompanied by a significant increase in the absolute number of encephalitogenic T cells within the CNS (Fig. 3D) and a significant reduction in the number of Treg in the spleen (Fig. 3E), but not the CNS (Fig. 3F). Since the ongoing EAE could have influenced the number of Treg, we next demonstrated that B cell depletion with anti-CD20 resulted in a subsequent significant reduction in the number of Treg in the spleen (Fig. 3G), but not the thymus (data not shown). The absolute number of splenic CD4+ and CD8+ T cells was not reduced in the anti-CD20 treated group (data not shown). To further demonstrate that B cells regulate Treg numbers, we analyzed μMT mice and found that Treg numbers were reduced in the spleen and lymph node (Fig. 3H), but not the thymus (data not shown) compared to WT mice. We obtained identical results with C57BL/6 μMT mice purchased from The Jackson Laboratory (data not shown).
During our analysis, we found that splenic Treg from μMT mice exhibited a lower CD25 MFI (Fig. 3I). Since CD25 expression has been linked to Treg suppressive capacity (32), we compared the ability of WT and μMT Treg to suppress the proliferation of CD3 activated naïve T cells and found no difference (Fig. 3J). These data indicate that B cells are important for Treg homeostasis and that loss of Treg numbers, and not function, is likely a contributing factor in B cell regulation of autoimmunity.
B cells regulate Treg numbers in an IL-10 and B7-independent manner
The finding that μMT mice and anti-CD20 B cell depleted mice exhibit largely identical EAE disease curves demonstrates that chronic disease in μMT mice is likely not due to alterations in the development or function of the peripheral immune system. This question is of importance because μMT mice have been reported to have T cell deficiencies (33, 34). Thus we asked whether B cell reconstitution in μMT mice would restore Treg numbers. As shown in Fig. 4A, the adoptive transfer of naïve WT splenic B cells resulted in a significant increase in the number of Treg cells as compared to μMT mice within the short timeframe of ten days. To confirm that the transferred B cells are retained for at least ten days, we first determined that the splenocyte population in WT mice contained 56% B220+ B cells and 19% CD4 T cells (Fig. 4B). As expected, mature B cells were not detected in μMT mice thus the percentage of CD4 T cells was subsequently increased to 35% (Fig. 4B). After B cell transfer into μMT mice, B cells composed 12% of splenocytes slightly reducing the percentage of CD4+ T cells to 30% (Fig. 4B). Because B cell production of IL-10 has been implicated in their regulatory function in EAE (3, 5), we asked whether this cytokine was also required for B cell-mediated Treg homeostasis. Interestingly, the adoptive transfer of IL-10-deficient B cells also lead to a significant increase in Treg similar to transfer of WT B cells (Fig. 4A). Since the B7 molecules have been implicated in Treg development and because we have previously shown their importance on B cells in the promotion of recovery from EAE (14), we next asked whether CD80 and CD86 were critical mediators of B cell-mediated Treg homeostasis. The adoptive transfer of CD80/CD86 double deficient (B71.2−/−) B cells resulted in a significant increase in the number of Treg as compared to μMT mice (Fig. 4C). Although the Treg increase was lower that that observed with WT B cells, the difference between the two groups was not statistically significant (Fig. 4C). When CD80 and CD86 single deficient B cells were transferred, the partial reduction in Treg numbers was due to a loss of CD86 (Fig. 4C). Because MHC class II has also been implicated at least in part in Treg homeostasis (35), we transferred B cells rendered deficient in MHC class II via disruption of the C2ta gene (36) into μMT mice and found that they functioned similar to their WT counterparts in driving an increase in Treg numbers (Fig. 4D).
Figure 4. B cell-mediated Treg homeostatis is not dependent upon B cell production of IL-10 or expression of B7 or MHC class II.
20 × 106 splenic B cells from WT (A–D), IL-10−/− (A), CD80/CD86 double deficient (B71.2−/−) (C), CD80−/− (C), CD86−/− (C) or C2ta−/− (D) mice were i.v. transferred into groups of μMT mice. Ten days post-transfer the absolute number (mean ± SEM) of splenic CD4+FoxP3+ Treg (A,C, D) and the percentage of B220+ and CD4+ (B) was determined by flow cytometry. A,C) Pooled data from 2–3 independent experiments with 6–10 mice per group is shown. B) Data are one representative experiment. D) Pooled data from two independent experiments with 3–6 mice per group is shown. *p<0.05, **p<0.01, ***p<0.001.
B cells contribute to Treg homeostasis by inducing their proliferation
We next determined whether B cells maintained Treg homeostasis by inducing their proliferation. First using an in vitro approach, we co-cultured B cells with Treg isolated from FoxP3EGFP reporter mice (25) in the presence of anti-CD3 and measured cell proliferation using a fluorescent dye dilution assay. In the absence of B cells, Treg underwent minimal proliferation (~12%) (Fig. 5A). However, in the presence of resting B cells, ~28% of Treg underwent proliferation (Fig. 5A). B cells deficient in IL-10 or CD80/CD86 induced the proliferation of Treg similarly to WT (data not shown). To determine if B cells drive Treg proliferation in vivo, we adoptively transferred B cells into μMT mice and found that the percentage of proliferating Ki-67+ Treg was increased by 1.5-fold as compared to μMT mice that received PBS (Fig. 5B). To further confirm that B cells promote Treg expansion in vivo, we performed a continuous BrdU labeling study and again found that the percentage of Treg that had proliferated and accumulated over seven days was increased by 1.5-fold in the presence of B cells (Fig. 5C). These data indicate that B cells either directly or indirectly contribute to the homeostasis of Treg by inducing their proliferation.
Figure 5. B cells induce Treg proliferation in vitro and in vivo.
A) Splenic Treg (CD4+EGFP+) were sorted and labeled with cell proliferation dye and cultured with soluble anti-CD3 and irradiated splenic APC in the presence or absence of WT splenic B cells. Four days post-culture, proliferation of EGFP+ cells gated on CD4+ T cells was determined by flow cytometry. B, C) 20 × 106 splenic B cells from WT mice were i.v. transferred into groups of μMT mice. BrdU was added to the drinking water three days later and continued for seven days. Ten days post-transfer, the percentages of Ki-67+ (B) and BrdU+ (C) splenic CD4+FoxP3+ Treg was determined by flow cytometry. Representative contour plots of CD4-gated cells that had incorporated BrdU in μMT mice in the absence and presence of adoptively transferred B cells are shown (C, left panels). Pooled data from 2–4 independent experiments (A) or pooled data from 2 independent experiments with 6 mice per group is shown (B,C). *p<0.05, **p<0.01.
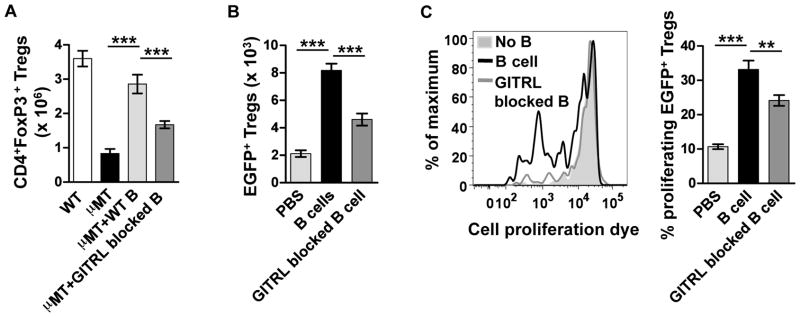
B cells regulate Treg homeostasis via GITRL
Since GITR has been implicated in the Treg proliferation and B cells have been reported to express GITRL (23, 24), we asked whether this receptor:ligand pair was responsible for Treg expansion. First, we confirmed previous reports that resting splenic B cells express a low level of GITRL ligand (Supplementary Fig. 1) (37). When GITRL antibody-blocked B cells were transferred into μMT mice the absolute number of splenic Treg was significantly reduced as compared to WT B cells (Fig. 6A). To further confirm a role for GITRL in B cell induced Treg expansion, we co-transferred EGFP+ Treg with B cells with or without blocked GITRL into μMT mice and measured Treg recovery and proliferation. As compared to Treg transfer alone, the number of recovered Treg was increased 4-fold in the presence of B cells (Fig. 6B) with an increase in the number of proliferating Treg from 10 to 35%, respectively (Fig. 6C). Antibody blocking of GITRL on B cells prior to co-transfer with EGFP+ Treg resulted in a significant reduction in the number of recovered (Fig. 6B) and proliferating (Fig. 6C) Treg. These data indicate that a primary mechanism whereby B cells regulate Treg homeostasis is via their expression of GITRL.
Figure 6. GITRL expressed by B cells promotes the maintenance and proliferation of Treg.
A) 20 × 106 splenic WT or GITRL-blocked WT B cells were i.v. transferred into groups of μMT mice. Ten days post-transfer, the absolute number (mean ± SEM) of splenic CD4+FoxP3+ Treg was determined by flow cytometry. C, D) Splenic Treg (CD4+EGFP+) were sorted and labeled with a cell proliferation dye and were were i.v. transferred into μMT mice with or without purified B cells. Seven days later, the absolute number (mean ± SEM) (B) and proliferation (C) of the labeled EGFP+ Treg in the spleen of the μMT mice was determined by flow cytometry. Representative data (C, left panel) and pooled data from 2–4 independent experiments (C, D) or pooled data from 2–3 independent experiments (A) with 6–10 mice per group is shown. *p<0.05, **p<0.01, ***p<0.001.
B cells require GITRL, but not IL-10, to promote recovery from EAE
Using an active immunization model, it was previously reported that B cell production of IL-10 was required for the recovery from EAE (3). Because the CFA used for those studies contained TLR ligands with the potent ability to induce IL-10 production by B cells, we asked whether in the absence of such external stimuli B cell production of IL-10 was required for recovery from EAE. As was have previously reported, EAE induced by adoptive transfer results in chromic disease in B10.PLμMT as compared to WT mice that undergo spontaneous remission and complete recovery (Fig. 7A, B) (14). The adoptive transfer of WT B cells once three days prior to EAE induction was sufficient to induce EAE recovery (Fig. 7A). Interestingly, neither B cell production of IL-10 nor expression of B7 was required for their ability to drive EAE recovery (Fig. 7A). In contrast, when GITRL-blocked B cells were adoptively transferred the μMT mice exhibited chronic EAE (Fig. 7B). The cumulative disease score of μMT mice that received GITRL-blocked B cells (39.4 ± 1.5) was significantly more severe than both WT (21.7± 2.2) and μMT mice that received WT B cells (23.7 ± 1.2) (Fig. 7C). An identical statistical result was obtained for the final disease score on day 30 (Fig. 7C). As expected, μMT mice exhibited a chronic cumulative disease course (44.8 ± 4.7) (Fig. 7C). On day 30, when we determined the absolute number of Treg in the spleen, we found that mice that received GITRL-blocked B cells had 46% fewer Treg as compared to those that received WT B cells (Fig. 7D). Because of the direct correlation between the number of B cells and Treg, we confirmed that GITRL-blocked B cells were not deleted following transfer. As shown in Fig. 7E, at day 30 after EAE induction, the absolute number and percentage of GITRL-blocked B220+ cells was similar to mice receiving WT B cells (Fig. 7E). These cumulative data demonstrate that B cells play and essential role in immune tolerance to autoimmunity my maintaining a critical number of Treg cells by promoting their expansion through GITRL.
Discussion
In this study, we investigated the mechanism whereby B cells regulate autoimmunity. We found that in the absence of B cells the absolute number of Treg was reduced rendering mice vulnerable to the rapid onset of spontaneous autoimmunity and the inability to resolve EAE. Furthermore, we discovered that B cell expression of GITRL controlled the number of Treg by inducing their proliferation. Thus we conclude that B cells play an essential role in controlling the onset and severity of autoimmunity by controlling Treg homeostasis and maintaining their numbers at a critical threshold required for optimal inhibition and downregulation of autoimmune responses.
The clinical relevance of our study is that the loss of B cells and the subsequent reduction in Treg resulted in the rapid onset of spontaneous EAE and colitis (Fig. 1, 2). These data are highly significant since one side effect of Rituximab (anti-CD20) treatment of autoimmunity has been the spontaneous onset of a different autoimmune disease often with a putative T cell-mediated etiology with colitis and psoriasis being the most prominent (2, 8–10). Rituximab was developed as a treatment for non-Hodgkin’s lymphoma and incidences of autoimmunity in these patients are very rare (11). One prominent reason for the increased incidence of autoimmunity following Rituximab treatment of autoimmune disorders in a subset of patients is likely due to their genetic susceptibility to multiple autoimmune disorders (38). It is unlikely that non-Hodgin’s lymphoma patients would have increased risk for the development of autoimmunity since cancer and autoimmunity are at opposites ends of the immune spectrum with cancer being associated with an underactive and autoimmunity with an overactive immune response. Similar to our studies in mice, the onset or exacerbation of autoimmunity following Rituximab treatment in several cases occurred within days (9, 10), which is consistent with a rapid decline in Treg numbers (Fig. 3).
Although Rituximab results in dramatic reduction in the number of peripheral blood B cells, little is known about its affects on Treg numbers. In this regard, in immune thrombocytopenia patients it was recently reported that the ratio of circulating CD4+CD25hiFoxP3+ to CD4+ blood cells was not altered one month following the first infusion of Rituximab, while B cells were essentially eliminated (39). Following splenectomy therapy, a similar analysis was conducted using the spleen of normal controls and patients with and without Rituximab therapy (39). The percentage of splenic B cells was similar between normal controls and untreated immune thrombocytopenia patients (39). As with peripheral blood, patients treated with Rituximab had a significant reduction in the percentage of B cells (39). When the ratio of Treg:CD4+ cells was examined, untreated immune thrombocytopenia patients had a significant reduction in the ratio as compared to normal controls, consistent with their autoimmune status (39). Of interest was the finding that Rituximab treated patients exhibited a further reduction the Treg:CD4+ ratio, although the reduction did not reach significance (39). When the Th1:Treg ratio was examined in CD4+ splenocytes, patients treated with Rituximab had a significant increase in the ratio compared to both controls and nontreated patients (39). To our knowledge this is the only human study that examined splenic Treg following Rituximab therapy. The cumulative data demonstrate that the findings in immune thrombocytopenia patients are consistent with our studies in the mouse. Of particular interest, is that we also did not detect a difference in CD4+FoxP3+ Treg in the blood following anti-CD20 treatment (data not shown), indicating that changes in Treg cells in the circulation cannot be used as a therapeutic marker of whether or not a particular patient would be susceptible to the onset of spontaneous autoimmunity.
Although blocking of GITRL on B cells led to a significant reduction in the number of Treg, the affect was not complete (Fig. 6). One reason is likely due to an incomplete block in B cell:Treg interactions because of antibody shedding and/or turnover of GITRL. We also cannot exclude the possibility that blocking of GITRL on B cells alters Treg function. Another possibility is that other cell surface molecules are involved. Due to the importance of B7 in Treg development and homeostasis (33, 40), we examined whether CD80 and/or CD86 were also required. The transfer of CD86-deficient B cells into μMT mice resulted in partial recovery of the Treg as compared to WT B cells (Fig. 4). CD80-deficient B cells were equivalent to WT. This difference is likely due to resting B cell expression of CD86, but not CD80 (data not shown). Although CTLA-4 has been implicated in Treg function (41–43), using a blocking antibody, we found no evidence that it plays a role in B cell-induced Treg homeostasis (data not shown). Because the homeostatic expansion of CD4+CD25+ T cells was shown to require MHC class II (44), we determined whether its expression by B cells promoted Treg expansion. Using both in vitro and in vivo approaches, we found no evidence for its role in Treg expansion induced by B cells (Fig. 4D and data not shown). Several experimental differences could account for this result including the use of CD4+CD25+ T cells in the original study (44). Since Fox3 expression could not be measured at the time, it is possible that CD4+CD25+ cells that were FoxP3− expanded in the lymphopenic host (Rag-1−/−). In our studies, we used FoxP3+ cells and an animal that was only partially lymphopenic (μMT). A later study using conditional ablation demonstrated an indirect role for MHC class II in Treg maintenance (35). Finally, we showed that B cell production of IL-10 was not required for the maintenance of Treg (Fig. 4). Additional supporting evidence is that IL-10−/− mice do not have altered numbers of Treg (Ray, Basu and Dittel, unpublished observations).
Although in our study, we determined that MHC class II expression was not required for their interactions with Treg, a role for self-antigen-specific B cells in either promoting or inhibiting EAE has been reported using genetically modified mice. An elegant study by Wekerle and colleagues demonstrated that T cells bearing a TCR specific for myelin oligodendrocyte glycoprotein (MOG) were able to recruit endogenous MOG-specific B cells, which expanded and produced pathogenic immunoglobulins contributing to the onset of spontaneous EAE (45). Using transgenic mice in which B cells expressed MOG-MHC class II complexes these antigen-specific B cells were shown to contribute to the negative selection of MOG-TCR transgenic T cells (46). In a second study using the same mice, the antigen-specific B cells were shown to contribute to peripheral tolerance of MOG-specific CD4 T cells (47). No affect on Treg was noted in either study, which supports our data that MHC class II is not required for B cell-mediated Treg homeostasis. Although antigen-specific B cells can induce tolerance in genetically modified mice, whether a similar mechanism exists in humans is not known. Evidence that immune tolerance to myelin self-antigens is at least incomplete in humans is the finding that healthy donors harbor T cells with specificity for a variety of myelin antigens, including MOG (48). In addition, Rituximab studies in which treated MS patients had significant reductions in the formation of new lesions supports a role for B cells in antigen presentation (2, 6, 7). Rituximab does not deplete plasma cells nor does it reduce serum Ig levels, further supporting a role for antigen presentation (2). Thus antigen presentation by B cells likely has dual functions contributing to both tolerance and disease onset/progression.
When we determined whether adoptively transferred B cells could function therapeutically in EAE, we found that WT B cells were able to drive the resolution of EAE in μMT mice (Fig. 7). B cells deficient in IL-10 or B7 also promoted EAE recovery. This result was surprising since both have been implicated in regulatory B cell functions in EAE (3, 14). In contrast, μMT mice that received GITRL-blocked B cells were unable to resolve EAE and had significantly fewer Treg cells 33 days after B cell transfer as compared to WT B cells. The finding that equal numbers of B cells were present in the anti-GITRL and WT groups, suggests that the antibody blocking had a long-term affect (Fig. 7).
Given that IL-10 production by B cells has been implicated in their regulatory potential in a number of autoimmune disorders, including as studied here in EAE and colitis (3, 5, 49), our finding that B cell maintenance of Treg is IL-10-independent is particularly interesting. One major difference between our study and others in EAE is that our adoptive transfer model does not require the use of CFA, which can contain TLR2, TLR4 and TRL9 ligands. Because we generate our T cell lines from MBP-TCR transgenic mice, we also avoid the use of CFA in their generation by using an in vitro approach (50). TLR2, TLR4 and TLR9 ligands have been shown to induce IL-10 production by B cells ((51) and Ray and Dittel, unpublished observations). In regards to TLR ligands, the TLR-signaling adaptor protein MyD88 was found to be essential for induction of EAE when globally knocked out, but not when deficient in B cells (52). However, MyD88 expression by B cells was required for their ability to mediate recovery from EAE (52). In earlier studies using a similar approach, this same group also demonstrated that B cell production of IL-10 was required for their regulatory function (3). This leads to the speculation that TLR signaling in B cells in response to CFA induces IL-10 production and subsequent immune regulation leading to recovery from EAE. However, more recently it was shown that MyD88-deficient mice were also resistant to EAE induction by adoptive transfer, indicating that exogenous TLR ligands are not required for EAE induction (53). Interestingly, the transferred encephalitogenic T cells proliferated and migrated to the CNS in MyD88−/− mice in the absence of lesion progression (53). A role for suppression by IL-10 in MyD88−/− mice was demonstrated by the susceptibility to EAE in MyD88/IL-10 double knockout mice (53). Interestingly, the source of the IL-10 was determined to be from T cells, not B cells. Since in this later study the EAE disease was very severe (score 4) the ability of the mice to recover could not be assessed. Nevertheless, in our adoptive transfer model using a less severe EAE disease (score 2) the mice are able to recover without the need for TLR ligands. These data indicate that engagement of TLR on B cells and their production of IL-10 is not an absolute requirement for their regulation of EAE. Rather, we propose, that TLR ligands in CFA produce a bystander effect by inducing B cell production of IL-10 that then in turn downregulates the immune response allowing recovery from EAE. Indeed, IL-10 production by T cells and its forced expression within the CNS also alleviates EAE clinical signs (53, 54). Since all B cell subpopulations produce IL-10 upon TLR engagement, bystander production of IL-10 by B cells will be common to all autoimmune models that require CFA, such as arthritis, or when TLR ligands are naturally present, such as in colitis.
We previously reported that mice bearing B7-deficient B cells had a delay in the production of IL-10 and presence of Treg cells in the CNS during EAE (14). From these data we hypothesized that B cells regulate Treg via B7, and found in the current study that CD86 only plays a minor role in Treg homeostasis. However, one major difference between our previous and current studies is that when μMT mice were reconstituted with B7-deficient B cells by bone marrow transplantation (BMT), the mice exhibited chronic EAE (14). Since neither study used CFA, the difference is not attributed to B cell activation via TLR ligands. We do not think that the irradiation required for the transplant resulted in dysfunctional immune responses because μMT mice receiving WT BM and WT mice that received B7−/− BM were both able to recover from EAE. In addition, we found that μMT mice transplanted with WT and B7−/− BM had similar numbers of Treg (data not shown), ruling out a Treg deficiency in our previous study. We think that the most likely explanation resides in differences in the balance of B cell subpopulations present in the two systems. BMT will reconstitute all populations of B cells, while in the transfer studies only splenic B cells will be present. B cell transfer into the partially lymphopenic μMT host will drive homeostatic expansion of the transferred cells likely resulting in changes in cell surface expression. We speculate that this process, which does not occur in the transplantation system, upregulates a currently unknown molecule that compensates for the loss of B7. Both the B7 and TNF families contain members that could contribute to B cell:Treg interactions. In addition, we speculate that a unique population of regulatory B cell is present in the spleen that is either preferentially expanded or has a survival advantage allowing for the efficient induction of Treg proliferaton when B cell numbers are limiting.
In our previous study, we reported that percentage of FoxP3+ cells (CD11b−) in the CNS was reduced at the peak of disease in μMT mice as compared to WT (14). Whereas in the current study, we found that the absolute number of Treg in the CNS in WT and μMT mice at the peak of disease was similar (Fig. 3), illustrating that the percentage of Treg fails to accurately reflect absolute cell numbers. Our data suggests that the absolute number of Treg is critical to their ability to suppress autoimmune responses. Indeed, only a 50% reduction in peripheral Treg whether achieved by genetic ablation, B cell depletion or GITRL-blocking was sufficient to prevent EAE recovery. These results suggest that Treg regulation of EAE occurs in the periphery and not in the CNS. Although other studies have shown that μMT mice have reduced percentages of Treg (16, 19), we are to the best of our knowledge the first to show a direct relationship between the presence of B cells and the absolute number of Treg in mice without disease. In mice with disease, EAE induced by active immunization in anti-CD20-treated mice was accompanied by a reduction in the percentage of CD4+FoxP3+ cells in both the periphery and CNS (17). A similar analysis was performed in mice with arthritis that was induced by immunization with methylated BSA emulsified in CFA in BM chimera mice generated by transplanting μMT mice with either WT or IL-10−/− BM (20). The IL-10 chimera mice exhibited more severe disease and five-days post-disease onset the absolute number CD4+FoxP3+ Treg was significantly reduced in the draining lymph node, but not in the synovia (20). These data are consistent with similar studies in EAE and arthritis demonstrating a suppressive role for IL-10 in models requiring CFA (3, 20). Indeed, the induction of IL-10 production by a putative regulatory B cell population characterized as CD1dhighCD5+ required TRL stimulation via LPS (55). A similar IL-10 producing B cell with the capacity to suppress intestinal inflammation has been described (56). Cumulatively, these data clearly indicate that B cells have the capacity to utilize both IL-10-dependent and -independent mechanisms to regulate the onset and severity of autoimmunity.
All of the above studies examining the relationship between B cells and Treg used C57BL/6 mice or as in our studies B10.PL mice, which are genetically similar. The B10.PLμMT mice used in our studies were derived by backcrossing to C57BL/6 μMT mice. Recently a study utilizing B cell deficient Balb/c JHD mice showed that these mice have an increase in the percentage of CD4+CD25+Foxp3+ cells, but no alteration in the absolute number of Treg in the spleen was observed (57). The contrary results could be due to genetic differences that account for the level of B cell contribution to Treg maintenance. It is not known whether GITRL or GITR expression is differentially regulated on immune cell types in different genetic backgrounds that could account for the differences. Thus the question remains as to whether or not a specific splenic B cell subpopulation with high levels of GITRL expression drives Treg expansion. If this population is reduced or absent in Balb/c mice, dendritic alone cells would likely be the primary cell type mediating Treg homeostasis.
In this study, we demonstrate the B cells are important for the maintenance of Treg at a level capable of constraining the onset of autoimmunity in genetically susceptible mouse strains. Evidence for a similar function in humans has emerged in Ritiximab-treated autoimmune patients that succumbed to either exacerbated disease or the onset of a new autoimmune disorder. Our discovery that B cells promote Treg homeostasis by promoting their proliferation without affecting their function via GITR:GITRL interactions, opens a therapeutic window for strategies whereby B cells or GITR-based drugs could be utilized to quickly increase or decrease the number of Treg. We envision the ability to decrease Treg numbers in cancer and during immunotherapies or increase their numbers for the treatment of autoimmunity and other inflammatory diseases. These studies also illustrate that as a lineage B cells are very complex and contain a large arsenal of mechanisms whereby they control the onset and extent of immune responses.
Supplementary Material
Acknowledgments
We thank Robert Dunn and Biogen Idec for providing the anti-CD20 antibody, Biolegend for providing the anti-GITRL antibody, Shelley Morris and Nichole Miller for technical support, and Dr. Jeffrey Woodliff and Hope Campbell for cell sorting assistance.
Footnotes
This work was supported by NIH grant R01 AI069358 and the BloodCenter Research Foundation
References
- 1.Wolf SD, Dittel BN, Hardardottir F, Janeway CA., Jr Experimental autoimmune encephalomyelitis induction in genetically B cell-deficient mice. J Exp Med. 1996;184:2271–2278. doi: 10.1084/jem.184.6.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ray A, Mann MK, Basu S, Dittel BN. A case for regulatory B cells in controlling the severity of autoimmune-mediated inflammation in experimental autoimmune encephalomyelitis and multiple sclerosis. J Neuroimmunol. 2010;230:1–9. doi: 10.1016/j.jneuroim.2010.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fillatreau S, Sweenie CH, McGeachy MJ, Gray D, Anderton SM. B cells regulate autoimmunity by provision of IL-10. Nat Immunol. 2002;3:944–950. doi: 10.1038/ni833. [DOI] [PubMed] [Google Scholar]
- 4.Mauri C. Regulation of immunity and autoimmunity by B cells. Curr Opin Immunol. 2010;22:761–767. doi: 10.1016/j.coi.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 5.Matsushita T, Yanaba K, Bouaziz JD, Fujimoto M, Tedder TF. Regulatory B cells inhibit EAE initiation in mice while other B cells promote disease progression. J Clin Invest. 2008;118:3420–3430. doi: 10.1172/JCI36030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, Bar-Or A, Panzara M, Sarkar N, Agarwal S, Langer-Gould A, Smith CH. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med. 2008;358:676–688. doi: 10.1056/NEJMoa0706383. [DOI] [PubMed] [Google Scholar]
- 7.Bar-Or A, Calabresi PA, Arnold D, Markowitz C, Shafer S, Kasper LH, Waubant E, Gazda S, Fox RJ, Panzara M, Sarkar N, Agarwal S, Smith CH. Rituximab in relapsing-remitting multiple sclerosis: a 72-week, open-label, phase I trial. Ann Neurol. 2008;63:395–400. doi: 10.1002/ana.21363. [DOI] [PubMed] [Google Scholar]
- 8.Dass S, Vital EM, Emery P. Development of psoriasis after B cell depletion with rituximab. Arthritis Rheum. 2007;56:2715–2718. doi: 10.1002/art.22811. [DOI] [PubMed] [Google Scholar]
- 9.Goetz M, Atreya R, Ghalibafian M, Galle PR, Neurath MF. Exacerbation of ulcerative colitis after rituximab salvage therapy. Inflamm Bowel Dis. 2007;13:1365–1368. doi: 10.1002/ibd.20215. [DOI] [PubMed] [Google Scholar]
- 10.El Fassi D, Nielsen CH, Kjeldsen J, Clemmensen O, Hegedus L. Ulcerative colitis following B lymphocyte depletion with rituximab in a patient with Graves’ disease. Gut. 2008;57:714–715. doi: 10.1136/gut.2007.138305. [DOI] [PubMed] [Google Scholar]
- 11.Mielke F, Schneider-Obermeyer J, Dorner T. Onset of psoriasis with psoriatic arthropathy during rituximab treatment of non-Hodgkin lymphoma. Ann Rheum Dis. 2008;67:1056–1057. doi: 10.1136/ard.2007.080929. [DOI] [PubMed] [Google Scholar]
- 12.Rudensky AY. Regulatory T cells and Foxp3. Immunol Rev. 2011;241:260–268. doi: 10.1111/j.1600-065X.2011.01018.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohm AP, Carpentier PA, Anger HA, Miller SD. Cutting edge: CD4+CD25+ regulatory T cells suppress antigen-specific autoreactive immune responses and central nervous system inflammation during active experimental autoimmune encephalomyelitis. J Immunol. 2002;169:4712–4716. doi: 10.4049/jimmunol.169.9.4712. [DOI] [PubMed] [Google Scholar]
- 14.Mann MK, Maresz K, Shriver LP, Tan Y, Dittel BN. B cell regulation of CD4+CD25+ T regulatory cells and IL-10 via B7 is essential for recovery from experimental autoimmune encephalomyelitis. J Immunol. 2007;178:3447–3456. doi: 10.4049/jimmunol.178.6.3447. [DOI] [PubMed] [Google Scholar]
- 15.Matsushita T, Horikawa M, Iwata Y, Tedder TF. Regulatory B Cells (B10 Cells) and Regulatory T Cells Have Independent Roles in Controlling Experimental Autoimmune Encephalomyelitis Initiation and Late-Phase Immunopathogenesis. J Immunol. 2010;185:2240–2252. doi: 10.4049/jimmunol.1001307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun JB, Flach CF, Czerkinsky C, Holmgren J. B lymphocytes promote expansion of regulatory T cells in oral tolerance: powerful induction by antigen coupled to cholera toxin B subunit. J Immunol. 2008;181:8278–8287. doi: 10.4049/jimmunol.181.12.8278. [DOI] [PubMed] [Google Scholar]
- 17.Weber MS, Prod’homme T, Patarroyo JC, Molnarfi N, Karnezis T, Lehmann-Horn K, Danilenko DM, Eastham-Anderson J, Slavin AJ, Linington C, Bernard CC, Martin F, Zamvil SS. B-cell activation influences T-cell polarization and outcome of anti-CD20 B-cell depletion in central nervous system autoimmunity. Ann Neurol. 2010;68:369–383. doi: 10.1002/ana.22081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhong X, Gao W, Degauque N, Bai C, Lu Y, Kenny J, Oukka M, Strom TB, Rothstein TL. Reciprocal generation of Th1/Th17 and T(reg) cells by B1 and B2 B cells. Eur J Immunol. 2007;37:2400–2404. doi: 10.1002/eji.200737296. [DOI] [PubMed] [Google Scholar]
- 19.Shah S, Qiao L. Resting B cells expand a CD4+CD25+Foxp3+ Treg population via TGF-beta3. Eur J Immunol. 2008;38:2488–2498. doi: 10.1002/eji.200838201. [DOI] [PubMed] [Google Scholar]
- 20.Carter NA, Vasconcellos R, Rosser EC, Tulone C, Munoz-Suano A, Kamanaka M, Ehrenstein MR, Flavell RA, Mauri C. Mice Lacking Endogenous IL-10-Producing Regulatory B Cells Develop Exacerbated Disease and Present with an Increased Frequency of Th1/Th17 but a Decrease in Regulatory T Cells. J Immunol. 2011;186:5569–5579. doi: 10.4049/jimmunol.1100284. [DOI] [PubMed] [Google Scholar]
- 21.Itoh M, Takahashi T, Sakaguchi N, Kuniyasu Y, Shimizu J, Otsuka F, Sakaguchi S. Thymus and autoimmunity: production of CD25+CD4+ naturally anergic and suppressive T cells as a key function of the thymus in maintaining immunologic self-tolerance. J Immunol. 1999;162:5317–5326. [PubMed] [Google Scholar]
- 22.Darrasse-Jeze G, Deroubaix S, Mouquet H, Victora GD, Eisenreich T, Yao KH, Masilamani RF, Dustin ML, Rudensky A, Liu K, Nussenzweig MC. Feedback control of regulatory T cell homeostasis by dendritic cells in vivo. J Exp Med. 2009;206:1853–1862. doi: 10.1084/jem.20090746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Olffen RW, Koning N, van Gisbergen KP, Wensveen FM, Hoek RM, Boon L, Hamann J, van Lier RA, Nolte MA. GITR triggering induces expansion of both effector and regulatory CD4+ T cells in vivo. J Immunol. 2009;182:7490–7500. doi: 10.4049/jimmunol.0802751. [DOI] [PubMed] [Google Scholar]
- 24.Nocentini G, Riccardi C. GITR: a modulator of immune response and inflammation. Adv Exp Med Biol. 2009;647:156–173. doi: 10.1007/978-0-387-89520-8_11. [DOI] [PubMed] [Google Scholar]
- 25.Haribhai D, Lin W, Relland LM, Truong N, Williams CB, Chatila TA. Regulatory T cells dynamically control the primary immune response to foreign antigen. J Immunol. 2007;178:2961–2972. doi: 10.4049/jimmunol.178.5.2961. [DOI] [PubMed] [Google Scholar]
- 26.Hamel K, Doodes P, Cao Y, Wang Y, Martinson J, Dunn R, Kehry MR, Farkas B, Finnegan A. Suppression of proteoglycan-induced arthritis by anti-CD20 B Cell depletion therapy is mediated by reduction in autoantibodies and CD4+ T cell reactivity. J Immunol. 2008;180:4994–5003. doi: 10.4049/jimmunol.180.7.4994. [DOI] [PubMed] [Google Scholar]
- 27.Dittel BN. Depletion of specific cell populations by complement depletion. J Vis Exp. 2010:36. doi: 10.3791/1487. http://www.jove.com/index/details.stp?id=1487. [DOI] [PMC free article] [PubMed]
- 28.Goverman J, Woods A, Larson L, Weiner LP, Hood L, Zaller DM. Transgenic mice that express a myelin basic protein-specific T cell receptor develop spontaneous autoimmunity. Cell. 1993;72:551–560. doi: 10.1016/0092-8674(93)90074-z. [DOI] [PubMed] [Google Scholar]
- 29.Lafaille JJ, Nagashima K, Katsuki M, Tonegawa S. High incidence of spontaneous autoimmune encephalomyelitis in immunodeficient anti-myelin basic protein T cell receptor transgenic mice. Cell. 1994;78:399–408. doi: 10.1016/0092-8674(94)90419-7. [DOI] [PubMed] [Google Scholar]
- 30.Brabb T, Goldrath AW, von Dassow P, Paez A, Liggitt HD, Goverman J. Triggers of autoimmune disease in a murine TCR-transgenic model for multiple sclerosis. J Immunol. 1997;159:497–507. [PubMed] [Google Scholar]
- 31.Kuhn R, Lohler J, Rennick D, Rajewsky K, Muller W. Interleukin-10-deficient mice develop chronic enterocolitis. Cell. 1993;75:263–274. doi: 10.1016/0092-8674(93)80068-p. [DOI] [PubMed] [Google Scholar]
- 32.Furtado GC, Curotto de Lafaille MA, Kutchukhidze N, Lafaille JJ. Interleukin 2 signaling is required for CD4(+) regulatory T cell function. J Exp Med. 2002;196:851–857. doi: 10.1084/jem.20020190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Homann D, Tishon A, Berger DP, Weigle WO, von Herrath MG, Oldstone MB. Evidence for an underlying CD4 helper and CD8 T-cell defect in B-cell-deficient mice: failure to clear persistent virus infection after adoptive immunotherapy with virus-specific memory cells from muMT/muMT mice. J Virol. 1998;72:9208–9216. doi: 10.1128/jvi.72.11.9208-9216.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bergmann CC, Ramakrishna C, Kornacki M, Stohlman SA. Impaired T cell immunity in B cell-deficient mice following viral central nervous system infection. J Immunol. 2001;167:1575–1583. doi: 10.4049/jimmunol.167.3.1575. [DOI] [PubMed] [Google Scholar]
- 35.Shimoda M, Mmanywa F, Joshi SK, Li T, Miyake K, Pihkala J, Abbas JA, Koni PA. Conditional ablation of MHC-II suggests an indirect role for MHC-II in regulatory CD4 T cell maintenance. J Immunol. 2006;176:6503–6511. doi: 10.4049/jimmunol.176.11.6503. [DOI] [PubMed] [Google Scholar]
- 36.Chang CH, Guerder S, Hong SC, van Ewijk W, Flavell RA. Mice lacking the MHC class II transactivator (CIITA) show tissue- specific impairment of MHC class II expression. Immunity. 1996;4:167–178. doi: 10.1016/s1074-7613(00)80681-0. [DOI] [PubMed] [Google Scholar]
- 37.Tone M, Tone Y, Adams E, Yates SF, Frewin MR, Cobbold SP, Waldmann H. Mouse glucocorticoid-induced tumor necrosis factor receptor ligand is costimulatory for T cells. Proc Natl Acad Sci U S A. 2003;100:15059–15064. doi: 10.1073/pnas.2334901100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Criswell LA, Pfeiffer KA, Lum RF, Gonzales B, Novitzke J, Kern M, Moser KL, Begovich AB, Carlton VE, Li W, Lee AT, Ortmann W, Behrens TW, Gregersen PK. Analysis of families in the multiple autoimmune disease genetics consortium (MADGC) collection: the PTPN22 620W allele associates with multiple autoimmune phenotypes. Am J Hum Genet. 2005;76:561–571. doi: 10.1086/429096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Audia S, Samson M, Guy J, Janikashvili N, Fraszczak J, Trad M, Ciudad M, Leguy V, Berthier S, Petrella T, Aho-Glele S, Martin L, Maynadie M, Lorcerie B, Rat P, Cheynel N, Katsanis E, Larmonier N, Bonnotte B. Immunologic effects of rituximab on the human spleen in immune thrombocytopenia. Blood. 2011;118:4394–4400. doi: 10.1182/blood-2011-03-344051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salomon B, Lenschow DJ, Rhee L, Ashourian N, Singh B, Sharpe A, Bluestone JA. B7/CD28 costimulation is essential for the homeostasis of the CD4+CD25+ immunoregulatory T cells that control autoimmune diabetes. Immunity. 2000;12:431–440. doi: 10.1016/s1074-7613(00)80195-8. [DOI] [PubMed] [Google Scholar]
- 41.Wing K, Onishi Y, Prieto-Martin P, Yamaguchi T, Miyara M, Fehervari Z, Nomura T, Sakaguchi S. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 42.Friedline RH, Brown DS, Nguyen H, Kornfeld H, Lee J, Zhang Y, Appleby M, Der SD, Kang J, Chambers CA. CD4+ regulatory T cells require CTLA-4 for the maintenance of systemic tolerance. J Exp Med. 2009;206:421–434. doi: 10.1084/jem.20081811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Read S, Greenwald R, Izcue A, Robinson N, Mandelbrot D, Francisco L, Sharpe AH, Powrie F. Blockade of CTLA-4 on CD4+CD25+ regulatory T cells abrogates their function in vivo. J Immunol. 2006;177:4376–4383. doi: 10.4049/jimmunol.177.7.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gavin MA, Clarke SR, Negrou E, Gallegos A, Rudensky A. Homeostasis and anergy of CD4(+)CD25(+) suppressor T cells in vivo. Nat Immunol. 2002;3:33–41. doi: 10.1038/ni743. [DOI] [PubMed] [Google Scholar]
- 45.Pöllinger B, Krishnamoorthy G, Berer K, Lassmann H, Bösl MR, Dunn R, Domingues HS, Holz A, Kurschus FC, Wekerle H. Spontaneous relapsing-remitting EAE in the SJL/J mouse: MOG-reactive transgenic T cells recruit endogenous MOG-specific B cells. J Exp Med. 2009;206:1303–1316. doi: 10.1084/jem.20090299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frommer F, Waisman A. B cells participate in thymic negative selection of murine auto-reactive CD4+ T cells. PLoS One. 2010;5:e15372. doi: 10.1371/journal.pone.0015372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frommer F, Heinen TJ, Wunderlich FT, Yogev N, Buch T, Roers A, Bettelli E, Muller W, Anderton SM, Waisman A. Tolerance without clonal expansion: self-antigen-expressing B cells program self-reactive T cells for future deletion. J Immunol. 2008;181:5748–5759. doi: 10.4049/jimmunol.181.8.5748. [DOI] [PubMed] [Google Scholar]
- 48.Raddassi K, Kent SC, Yang J, Bourcier K, Bradshaw EM, Seyfert-Margolis V, Nepom GT, Kwok WW, Hafler DA. Increased frequencies of myelin oligodendrocyte glycoprotein/MHC class II-binding CD4 cells in patients with multiple sclerosis. J Immunol. 2011;187:1039–1046. doi: 10.4049/jimmunol.1001543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yanaba K, Yoshizaki A, Asano Y, Kadono T, Tedder TF, Sato S. IL-10-producing regulatory B10 cells inhibit intestinal injury in a mouse model. Am J Pathol. 2011;178:735–743. doi: 10.1016/j.ajpath.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dittel BN, Merchant RM, Janeway CA., Jr Evidence for Fas-dependent and Fas-independent mechanisms in the pathogenesis of experimental autoimmune encephalomyelitis. J Immunol. 1999;162:6392–6400. [PubMed] [Google Scholar]
- 51.Barr TA, Brown S, Ryan G, Zhao J, Gray D. TLR-mediated stimulation of APC: Distinct cytokine responses of B cells and dendritic cells. Eur J Immunol. 2007;37:3040–3053. doi: 10.1002/eji.200636483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lampropoulou V, Hoehlig K, Roch T, Neves P, Calderon Gomez E, Sweenie CH, Hao Y, Freitas AA, Steinhoff U, Anderton SM, Fillatreau S. TLR-activated B cells suppress T cell-mediated autoimmunity. J Immunol. 2008;180:4763–4773. doi: 10.4049/jimmunol.180.7.4763. [DOI] [PubMed] [Google Scholar]
- 53.Cohen SJ, I, Cohen R, Nussbaum G. IL-10 mediates resistance to adoptive transfer experimental autoimmune encephalomyelitis in MyD88(−/−) mice. J Immunol. 2010;184:212–221. doi: 10.4049/jimmunol.0900296. [DOI] [PubMed] [Google Scholar]
- 54.Cua DJ, Groux H, Hinton DR, Stohlman SA, Coffman RL. Transgenic interleukin 10 prevents induction of experimental autoimmune encephalomyelitis. J Exp Med. 1999;189:1005–1010. doi: 10.1084/jem.189.6.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yanaba K, Bouaziz JD, Matsushita T, Tsubata T, Tedder TF. The development and function of regulatory B cells expressing IL-10 (B10 cells) requires antigen receptor diversity and TLR signals. J Immunol. 2009;182:7459–7472. doi: 10.4049/jimmunol.0900270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mizoguchi A, Mizoguchi E, Takedatsu H, Blumberg RS, Bhan AK. Chronic intestinal inflammatory condition generates IL-10-producing regulatory B cell subset characterized by CD1d upregulation. Immunity. 2002;16:219–230. doi: 10.1016/s1074-7613(02)00274-1. [DOI] [PubMed] [Google Scholar]
- 57.Hamel KM, Cao Y, Ashaye S, Wang Y, Dunn R, Kehry MR, Glant TT, Finnegan A. B cell depletion enhances T regulatory cell activity essential in the suppression of arthritis. J Immunol. 2011;187:4900–4906. doi: 10.4049/jimmunol.1101844. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.