Abstract
Background & Aims
Although childhood and adult abuse are more prevalent among patients with irritable bowel syndrome (IBS) than healthy individuals (controls), other types of early adverse life events (EALs) have not been well characterized. We investigated whether different types of EALs, before an age of 18 years, are more prevalent among patients with IBS, and the effects of gender and non-gastrointestinal symptoms on the relationship between EALs and IBS.
Methods
EALs were evaluated in 294 IBS patients (79% women) and 435 controls (77% women) using the early trauma inventory self report form, which delineates sub-categories of general trauma and physical, emotional, and sexual abuse. Validated questionnaires assessed gastrointestinal, psychological, and somatic symptoms.
Results
Compared to controls, IBS patients reported a higher prevalence of general trauma (78.5% vs 62.3%), physical punishment (60.6% vs 49.2%), emotional abuse (54.9% vs 27.0%), and sexual events (31.2% vs 17.9%) (all P’s <.001). These significant differences were mainly observed in women. Of the EAL domains, emotional abuse was the strongest predictor of IBS (P<.001). Eight of the 27 EAL items were significant (P<.001) and increased the odds of having IBS by 108%–305%. Although EAL and psychological variables were related, EALs had an independent association with IBS (P=.04).
Conclusion
Various types of EALs are associated with development of IBS—particularly among women. Psychological distress and somatic symptoms might contribute to this relationship. When appropriate, EALs and non-gastrointestinal symptoms should be assessed in IBS patients.
Keywords: ETI-SF, psychology, somatization, nervous system
INTRODUCTION
Early adverse life events (EALs) refer to traumatic experiences during childhood encompassing physical, sexual, or emotional abuse, as well as discordant relationships with primary caretaker, or the loss of a parent.1–5 Children with a history of EALs have an increased risk of developing a range of chronic medical disorders later in life.6–10
EALs also appear to be associated with an increased vulnerability toward developing functional gastrointestinal disorders (FGIDs), including irritable bowel syndrome (IBS).1, 11,12, 13 The most common EAL assessed in IBS is childhood or adulthood abuse. In a population-based survey by Talley et al.,14 the prevalence of childhood abuse was significantly higher in individuals with vs. without IBS (15.4% vs. 9.5%).14 Similarly, Drossman and colleagues15 found that patients with FGIDs experienced more severe forms of abuse in childhood and/or adulthood, including rape and life-threatening physical abuse, compared to patients with organic gastrointestinal (GI) diseases.15 EALs other than abuse have not been studied extensively in IBS patients. In 1979, Hislop16 reported that 31% of IBS patients had experienced parental death, divorce or separation and 61% reported unsatisfactory relationships with or between their parents before the age of 15, but there was no comparison to a control group.
EALs have been associated with negative outcomes in patients with GI conditions. Among patients with upper GI and chest conditions, childhood adversity maintained an independent effect on poorer health-related quality of life (HRQOL) in patients with non-cardiac chest pain and functional dyspepsia, two types of FGIDs.17 An abuse history has been associated with greater pain, disability, psychological distress and functioning in GI patients independent of diagnosis.18 In addition, sexual abuse correlated with more severe IBS symptoms, non-GI symptoms and abdominal surgery.19
Although associations between an abuse history and IBS have been reported before, in the current study we aimed to simultaneously assess the association of a range of EALs, not limited to abuse, with IBS and the impact of sex differences and psychological factors on these associations. Specifically, we aimed to address the following questions: 1) Is a history of EALs before the age of 18 associated with IBS? 2) What are the types of EALs most commonly associated with IBS? 3) Is there a sex-related difference in the association of EALs and IBS? 4) What is the impact of psychological symptoms on the relationship between EALs and IBS?
METHODS
Study subjects
Male and female IBS patients who were ≥18 years of age were recruited from newspaper or internet community advertisements and from GI clinics and fulfilled Rome III diagnostic criteria.20 Healthy control subjects (HCs) were recruited by advertisement without a history of IBS or other chronic GI or pain conditions, and were not taking psychotropic medication or participating in psychotherapy. Subjects were compensated $50 for completion of a medical history and physical examination and questionnaires.
Questionnaires
Bowel Symptom Questionnaire
The questionnaire included Rome III questions for IBS21 and a 0-20 numeric rating scale of overall IBS symptom severity over the past week (none to most intense imaginable).22
EAL Questionnaire
Presence of EALs (before age 18) was assessed by the Early Trauma Inventory Self Report Form (ETI-SF),4 It assesses EALs in the following domains (number of items): general trauma (11), physical (5), emotional (5), and sexual abuse (6). Each of the 27 items was scored as “Yes”=1 or “No”=0 (total score range 0-27). The ETI-SF has been validated in post-traumatic stress disorder (PTSD), where the best predictor of PTSD symptoms was the total score.4 General trauma include various stressful and traumatic events. Physical punishment is defined as physical contact, constraint or confinement with intent to hurt or injure. Emotional abuse included events defined by verbal communication with intent to humiliate or degrade. Sexual abuse is unwanted sexual contact for the gratification of the perpetrator or for the purposes of dominating or degrading the victim.4 The prevalence of EAL in each of the four domains was considered positive if any one of the items within each domain was endorsed.
Other Psychometric Instruments
The Hospital Anxiety and Depression (HAD) scale23 measured current anxiety and depression symptoms. Trait anxiety was measured using the State-Trait Anxiety Inventory (STAI).24 Somatic symptom severity was measured using the Personal Health Questionnaire (PHQ-15),25 modified by removal of three GI symptom items (score 0–24). The Visceral Sensitivity Index (VSI)26 assessed GI-specific anxiety.
The study was approved by the UCLA Institutional Review Board, and all subjects signed a written informed consent prior to start of study.
Statistical Analysis
Logistic regression analyses controlling for age, race, education, and gender were conducted to determine the associations between individual ETI-SF items and IBS. Psychological variables were highly correlated with ETI-SF items and thus we first modeled them separately with demographic variables. In order to determine if ETI-SF items had an independent association with IBS not accounted for by psychological variables, we compared pseudo R2 from these separate models to a full model containing demographics, psychological variables and ETI-SF items.
We also modeled males and females separately relating ETI-SF items and EAL while controlling for demographics. Associations with IBS were tested by Fisher’s exact tests for categorical variables and Mann Whitney U tests for continuous variables. Because we assessed 27 items within the ETI-SF questionnaire, the adjusted significance level was p<0.0018 for all comparisons using the Bonferroni correction.
RESULTS
Subject characteristics (Table 1)
Table 1.
Clinical characteristics
| Variable (±SEM) | IBS patients (n=294) | Controls (n=435) | P value |
|---|---|---|---|
| Age (years) | 36.17±0.72 | 29.45±0.50 | <0.001 |
| Sex (% female) | 79 | 76.7 | 0.468 |
| Racial/Ethnic category (%) | <0.001 | ||
| Hispanic | 13.61 | 18.39 | |
| Asian | 8.84 | 26.21 | |
| Black or African American | 11.22 | 11.26 | |
| White | 55.44 | 35.40 | |
| Decline to Answer/Other/Multiracial | 10.88 | 8.74 | |
| Education (%) | <0.001 | ||
| At least some high school but no college | 7.61 | 5.37 | |
| Some college | 28.02 | 43.22 | |
| College graduate | 38.41 | 32.71 | |
| Any postgraduate work | 25.95 | 18.69 | |
| Bowel Habit Type | |||
| IBS-C | 29.3 | NA | |
| IBS-D | 29.9 | NA | |
| IBS-M | 27.2 | NA | |
| IBS-U | 13.6 | NA | |
| GI symptom severity score (0-20) | 10.64±0.25 | NA | NA |
| HAD Anxiety score (0-20) | 7.42±0.25 | 3.86±0.14 | <0.001 |
| HAD Depression score (0-20) | 3.90±0.20 | 1.52±0.10 | <0.001 |
| STAI Trait anxiety (need range) | 54.45±0.80 | 45.02±0.47 | <0.001 |
| VSI score (0-90) | 35.50±0.94 | 3.47±0.41 | <0.001 |
| PHQ-12 score (0-24) | 10.68±0.30 | 2.43±0.11 | <0.001 |
Abbreviations: IBS, irritable bowel syndrome; IBS-C, IBS with constipation; IBS-D, IBS with diarrhea; IBS-M, IBS with mixed pattern; IBS-U, IBS unsubtyped; GI, gastrointestinal; HAD, Hospital Anxiety and Depression Scale; STAI, State-Trait Anxiety Inventory; VSI, Visceral Sensitivity Index; PHQ, Personal Health Questionnaire; SEM, standard error of mean; NA=not applicable.
Subjects were recruited primarily from community advertisements in the Greater Los Angeles area and included 294 IBS patients and 435 HCs (79% and 77% women, respectively). Ninety-four percent of the IBS patients were recruited from advertisement. There were no significant differences in demographic or clinical symptoms between those recruited by advertisement or from the GI clinic. Forty-two percent of the subjects recruited from advertisement had seen a physician in the past year for their abdominal symptoms and 58% had not. Compared to IBS non-consulters in the past year, IBS consulters had higher GI symptom severity (11.25±0.4 vs. 10.16±0.36, p=0.06), and significantly greater current anxiety symptoms (8.03±0.44 vs. 6.73±0.37, p=0.04), GI symptom anxiety (40.48±1.48 vs. 31.99±1.37, p<0.001), and somatic symptom severity (6.76±0.50 vs. 5.22±0.33, p=0.02). However, there were no differences in EAL scores. Compared to HCs, IBS patients were older, had achieved higher education, and had higher scores for anxiety and depression, trait and symptom-specific anxiety, and somatic symptom severity. Ninety percent of the HCs had no (0) or mild somatic symptoms (score 1–4).
Prevalence of EALs in IBS and controls
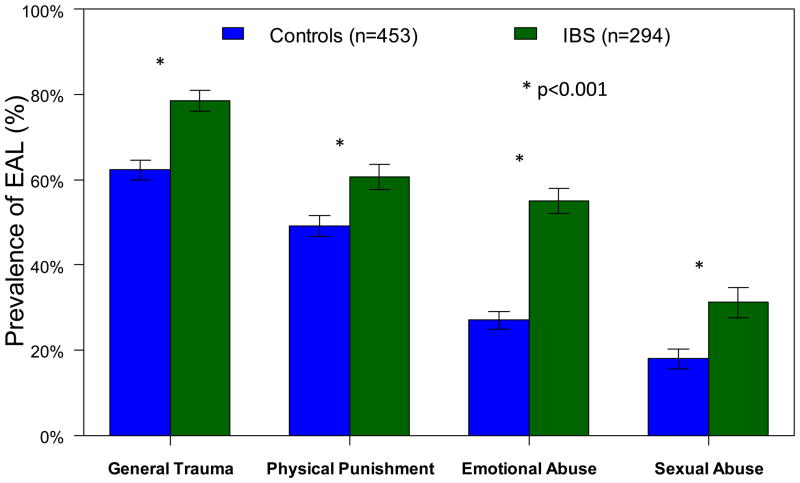
Compared to HCs, IBS patients had significantly higher prevalence of the four EAL domains even after adjusting for demographic variables (Figure 1, Supplementary Table A) (p<0.001). IBS patients also had significantly higher scores for total number of ETI-SF items and for the domains of general trauma, physical punishment, emotional abuse and sexual abuse (all p’s < 0.001, Supplementary Table B). Emotional abuse was the strongest predictor of IBS status (p<0.001). Eight of the 27 ETI-SF items were significantly associated with the odds of having IBS after adjusting for multiple comparisons (Table 2). Sexual abuse and feeling ignored or made to feel not counted conferred the highest odds of having IBS (ORs of up to 4.05).
Figure 1.
The prevalence of the four subcategories of EAL based on the ETI-SF questionnaire in IBS patients and controls are shown. The prevalence of the four subcategories were significantly higher in IBS patients vs. controls (*p<0.001).
Table 2.
Individual items associated with IBS
| Question | Coefficient (SE) | Odds Ratio | Interpretation |
|---|---|---|---|
| Did you ever witness violence towards others, including family members? | 0.73 (0.19) | 2.08 | If yes, the odds of having IBS is 108% higher. |
| Did anyone in your family ever suffer from mental or psychiatric illness or have a “breakdown”? | 0.82 (0.21) | 2.27 | If yes, the odds of having IBS is 127% higher. |
| Were you often put down or ridiculed? | 0.82 (0.18) | 2.26 | If yes, the odds of having IBS is 126% higher. |
| Were you often ignored or made to feel that you didn’t count? | 1.13 (0.21) | 3.08 | If yes, the odds of having IBS is 208% higher. |
| Most of the time were you treated in a cold, uncaring way or made to feel like you were not loved? | 0.97 (0.29) | 2.64 | If yes, the odds of having IBS is 164% higher. |
| Did your parents or caretakers often fail to understand you or your needs? | 0.92 (0.2) | 2.51 | If yes, the odds of having IBS is 151% higher. |
| Were you ever forced or coerced to touch another person in an intimate or private part of their body? | 1.07 (0.31) | 2.92 | If yes, the odds of having IBS is 192% higher. |
| Did anyone ever have genital sex with you against your will? | 1.4 (0.41) | 4.05 | If yes, the odds of having IBS is 305% higher. |
Each odds ratio was statistically significant (p<0.001) and was adjusted for age, gender, education, and race using logistic regression.
Impact of gender
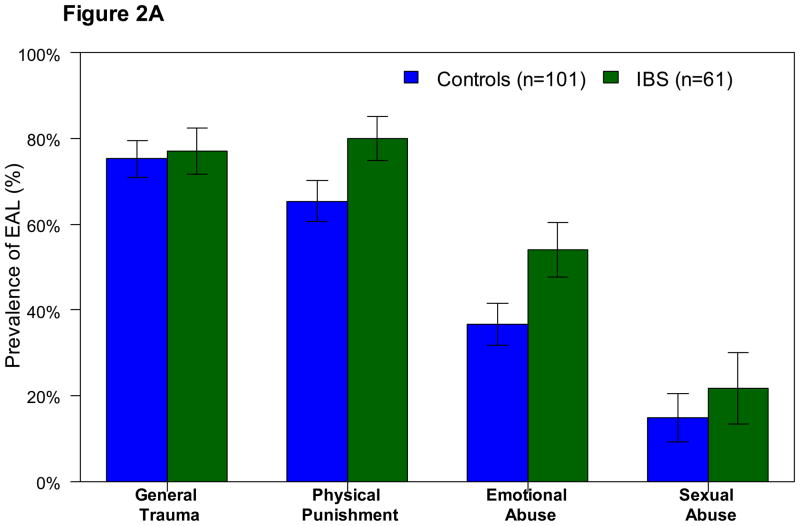
Among men, the prevalence of EAL within the four domains (Figure 2A, Supplement Table C) and ETI-SF total and domain scores (Supplement Table B) were not significantly different between IBS and HCs after correcting for multiple comparisons. Only one of the 27 items (“Were you often ignored or made to feel that you didn’t count?”) was reported by significantly more IBS men than healthy men (39.3 vs. 15.8%, p<0.001). After accounting for demographic variables, this difference was no longer significant.
Figure 2.
The prevalence of the four subcategories of EAL based on the ETI-SF questionnaire in the male (2A) and female (2B) IBS patients and controls are shown. In the male subjects (2A), EALs were not different between IBS patients and controls after controlling for multiple comparisons. In the female subjects (2B), all four types of EAL were significantly more prevalent in IBS patients vs. controls (*p<0.001).
In women, the prevalence of general trauma (78.9 vs. 58.5%, p<0.001), physical punishment (55.6 vs. 44.3%, p=0.01), emotional abuse (55.2 vs. 24%, p<0.001), and sexual abuse (33.6 vs. 18.9%, p<0.001) were significantly higher in IBS patients vs. HCs even after adjusting for demographic variables (Figure 2B, Supplemental Table D). Similar results were obtained with respect to ETI-SF scores (Supplemental Table B). IBS women reported 13 EAL items significantly more often healthy women (p’s <0.001).
Impact of psychological and non-GI symptoms
Each individual psychological variable was evaluated for its relationship with IBS while controlling for demographics. As expected, HAD scores for symptoms of anxiety and depression, PHQ-12 score, trait anxiety, and VSI score had significantly positive associations with IBS (all p’s<0.001, Supplementary Table E) with the strongest association for PHQ-12 (OR=1.73). Psychological variables and ETI-SF scores were highly correlated but we wanted to measure the independent contribution of each to the presence of IBS. We modeled the relationship between the psychological variables and EAL with IBS controlling for demographic variables. The variance explained by demographics alone was increased from 0.109 to 0.298 when psychological variables (HAD anxiety, HAD depression, trait anxiety) were added. When ETI-SF scores were added to the model, the variance further increased to 0.304 (p=0.04). Similarly, the variance explained by demographics alone increased from 0.109 to 0.149 when ETI-SF scores were added and further increased when the psychological variables were included (p<0.01). There was no significant relationship between ETI-SF and IBS when controlling for somatic symptoms (PHQ-12) and GI symptom anxiety (VSI). Thus, while EAL and psychological variables are interrelated, they have some independent association with IBS.
DISCUSSION
The main findings of the current study were: 1) IBS patients had a significantly greater prevalence of EALs, including general trauma, and physical, emotional and sexual abuse compared to HCs, 2) These differences were mainly seen within the women, 3) Of the EAL domains measured, emotional abuse was the strongest predictor of having IBS, 4) The strength of the relationship between EALs and IBS was reduced after controlling for the presence of psychological and other non-GI symptoms. Each of these points will be addressed below.
Association of EAL and IBS
General trauma and emotional, physical and sexual abuse were reported significantly more often by patients than HCs. With respect to individual items, these events included witnessing violence, mental illness in the family, emotional abuse, and being forced to touch intimate parts of a person’s body or have genital sex. The prevalence of specific types of abuse is similar to previously reported prevalence numbers in IBS patients, including the prevalence of a history of sexual abuse15 and the prevalence of disturbances in the child-caregiver relationship.16 Our study found that 47% of IBS patients experienced divorce, separation, or death of parents (vs. 36% in HCs, p=0.004) and 18% had parents or primary caregivers with alcoholism or drug abuse (vs. 13% in HCs, p=0.06). Additionally, 35% of patients in our study stated that their parents or caretakers often failed to understand them or their needs compared to 14% of HCs (p<0.001).
Possible neurobiological mechanisms underlying the observed association between EALs and IBS have been identified in animal models and in humans linking early life psychosocial exposures with long-lasting changes in gene expression.6, 27 For example, exposure to perinatal stress (i.e. maternal separation) predisposes adult rats to develop stress-induced visceral hypersensitivity, enhanced defecation, intestinal mucosal dysfunction, increased hypothalamic-pituitary-adrenal (HPA) axis responses and anxiety-like behavior.28–31 Studies in adult IBS patients have shown stress-induced alterations in gastrointestinal motility, visceral sensitivity, autonomic tone and HPA axis responses.32 Previous studies on the role of mother offspring interactions on adult stress responsiveness had demonstrated a link between specific maternal behaviors (licking and grooming) and epigenetic alterations at the glucocorticoid receptor (GR) gene locus in the adult offspring.33 Homologous findings of GR methylation have been demonstrated in humans by analysing autopsy specimens from suicide victims with a history of childhood abuse.34 Consistent with alterations in the HPA axis regulation, we recently demonstrated that EALs was associated with increased cortisol response to a visceral stressor in both IBS and controls and the return to basal levels correlated with IBS symptom severity.35, 36
Impact of gender on EALs in IBS
Group differences in EALs were primarily observed in women. The lack of differences within men may be due to the smaller sample size relative to the women and/or the variations in the prevalence of the EAL domains in the overall population. While abuse has been studied predominantly in women,6, 14, 18 a survey conducted in equal numbers of men and women also found that abuse was reported more often by women (41%) than men (11%).14 These differences may be due to the fact that our subjects were mainly recruited from advertisement and not randomly sampled from the community and were more diverse in race and ethnicity. Our study suggests that a history of EALs increases the vulnerability to develop IBS in women, but larger studies with more men are needed to evaluate the relationship in men. Interestingly, the association of EALs and elevated cortisol response to a visceral stressor was seen mainly in men and not in women.35, 36
Impact of psychological and somatic symptoms on EAL and IBS
Controlling for psychological and somatic symptoms weakened the association of ETI-SF scores with IBS, although EAL still had some independent association with IBS. These findings suggest that factors associated with the presence of non-GI symptoms mediate the relationship between EALs and IBS. Previous studies, which measured EALs in a managed-care patient population, found a graded response to early adversity with higher scores related to increased somatic and psychiatric comorbidity, as well as organic diseases such as chronic obstructive pulmonary disease.6, 7 Others have speculated that individuals with a history of EALs have a heightened awareness of bodily sensations, and a tendency to amplify these perceptions.10, 37–41
An association between abuse and somatic symptoms has been reported in FGID patients. Van Oudenhove and colleagues42 found that somatization (e.g., the presence of several somatic symptoms) mediated the effect of sexual and physical abuse on HRQOL in functional dyspepsia. Creed et al.10 demonstrated that the level of somatization in IBS patients was associated with symptom severity, HRQOL and history of sexual abuse. These findings suggest that trauma and abuse is associated with an increased vulnerability for multiple somatic symptoms and syndromes, and that the association is not unique to the symptom complex of IBS.
Studies have shown that patients with an abuse history tend to utilize healthcare and have greater symptom reporting compared to those without this history.14, 15 However, treating providers infrequently inquire about EALs. In Drossman’s study,15 only 17% of providers knew of their patients’ abuse history. This information is an integral part of a patient’s presentation and should be inquired by the health care provider when appropriate.14, 15 Treatment addressing EALs and psychological symptoms can potentially improve symptoms and reduce healthcare utilization. While studies have not directly evaluated the impact of EALs on treatment response in IBS, they have been conducted in other conditions. For example, depressed patients with EALs experienced greater efficacy with psychotherapy with or without an antidepressant when compared to the antidepressant alone.43 However, in patients with depression without a history of childhood abuse, a combination of an antidepressant and psychotherapy was superior to either one alone.43
Limitations of the present study include the possibility of recall bias given our focus on childhood traumatic events. Additionally, the ETI-SF questionnaire includes events of abuse, major losses and other types of trauma but does not allow distinction between the types of trauma. It has also been validated in PTSD, but not in IBS.
In summary, various types of EALs are more prevalent in IBS compared to HCs, particularly among women with IBS and are associated with a greater prevalence of psychological and somatic symptoms. Addressing EALs and associated psychological symptoms in IBS patients is important and may help guide management approaches in an effort to reduce symptoms and healthcare utilization and improve overall well-being.
Acknowledgments
Grant support: Supported by NIH grant P50 DK64539
Abbreviations
- IBS
irritable bowel syndrome
- HCs
healthy controls
- EALs
early adverse life events
- HAD
Hospital Anxiety and Depression scale
- STAI
State-Trait Anxiety Inventory
- PHQ
Personal Health Questionnaire
Footnotes
Disclosures: No conflicts of interest exist for all authors
Authors’ roles:
KB: acquisition of data, drafting of manuscript
WS: analysis and interpretation of data, drafting of the manuscript
EV: study concept and design; interpretation of data; drafting of the manuscript
APP: supervision of statistical analysis, interpretation of data, critical review of the manuscript
BDN: critical review of the manuscript for important intellectual content
EAM: critical review of the manuscript for important intellectual content, study funding
LC: study concept and design, acquisition of data, interpretation of data, drafting and critical review of the manuscript, study funding
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chitkara DK, van Tilburg MA, Blois-Martin N, et al. Early life risk factors that contribute to irritable bowel syndrome in adults: a systematic review. Am J Gastroenterol. 2008;103:765–74. doi: 10.1111/j.1572-0241.2007.01722.x. quiz 775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heim C, Newport DJ, Heit S, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–7. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- 3.Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–39. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- 4.Bremner JD, Bolus R, Mayer EA. Psychometric properties of the Early Trauma Inventory-Self Report. J Nerv Ment Dis. 2007;195:211–8. doi: 10.1097/01.nmd.0000243824.84651.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282:1652–8. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 6.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anda RF, Brown DW, Dube SR, et al. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med. 2008;34:396–403. doi: 10.1016/j.amepre.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anda RF, Brown DW, Felitti VJ, et al. Adverse childhood experiences and prescription drug use in a cohort study of adult HMO patients. BMC Public Health. 2008;8:198. doi: 10.1186/1471-2458-8-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anda R. The health and social impact of growing up with adverse childhood experiences: The human and economic costs of the status quo. 2008. [Google Scholar]
- 10.Creed F, Tomenson B, Guthrie E, et al. The relationship between somatisation and outcome in patients with severe irritable bowel syndrome. J Psychosom Res. 2008;64:613–20. doi: 10.1016/j.jpsychores.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 11.Mayer EA, Naliboff BD, Chang L, et al. V. Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol. 2001;280:G519–24. doi: 10.1152/ajpgi.2001.280.4.G519. [DOI] [PubMed] [Google Scholar]
- 12.Anand KJ, Runeson B, Jacobson B. Gastric suction at birth associated with long-term risk for functional intestinal disorders in later life. J Pediatr. 2004;144:449–54. doi: 10.1016/j.jpeds.2003.12.035. [DOI] [PubMed] [Google Scholar]
- 13.Bengtson MB, Ronning T, Vatn MH, et al. Irritable bowel syndrome in twins: genes and environment. Gut. 2006;55:1754–9. doi: 10.1136/gut.2006.097287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Talley NJ, Fett SL, Zinsmeister AR, et al. Gastrointestinal tract symptoms and self-reported abuse: a population-based study. Gastroenterology. 1994;107:1040–9. doi: 10.1016/0016-5085(94)90228-3. [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–33. doi: 10.7326/0003-4819-113-11-828. [DOI] [PubMed] [Google Scholar]
- 16.Hislop IG. Childhood deprivation: an antecedent of the irritable bowel syndrome. Med J Aust. 1979;1:372–4. doi: 10.5694/j.1326-5377.1979.tb126963.x. [DOI] [PubMed] [Google Scholar]
- 17.Biggs AM, Aziz Q, Tomenson B, et al. Effect of childhood adversity on health related quality of life in patients with upper abdominal or chest pain. Gut. 2004;53:180–6. doi: 10.1136/gut.2003.020974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drossman DA, Li Z, Leserman J, et al. Health status by gastrointestinal diagnosis and abuse history. Gastroenterology. 1996;110:999–1007. doi: 10.1053/gast.1996.v110.pm8613034. [DOI] [PubMed] [Google Scholar]
- 19.Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees. Prevalence, demographics, and clinical correlates. Dig Dis Sci. 1993;38:1581–9. doi: 10.1007/BF01303163. [DOI] [PubMed] [Google Scholar]
- 20.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(Suppl 2):II43–7. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brun R, Kuo B. Functional dyspepsia. Therapeutic advances in gastroenterology. 2010;3:145–64. doi: 10.1177/1756283X10362639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spiegel BM, Harris LA, Lucak SL, et al. Measuring IBS patient reported outcomes with a single item numeric rating scale: Results from the PROOF cohort. Gastroenterology. 2008;134(Suppl 1):A-467. [Google Scholar]
- 23.Zigmond ASSR. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 24.Kvaal K, Ulstein I, Nordhus IH, et al. The Spielberger State-Trait Anxiety Inventory (STAI): the state scale in detecting mental disorders in geriatric patients. International journal of geriatric psychiatry. 2005;20:629–34. doi: 10.1002/gps.1330. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The PHQ-15: Validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Medicine. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Labus JS, Bolus R, Chang L, et al. The Visceral Sensitivity Index: development and validation of a gastrointestinal symptom-specific anxiety scale. Alimentary pharmacology & therapeutics. 2004;20:89–97. doi: 10.1111/j.1365-2036.2004.02007.x. [DOI] [PubMed] [Google Scholar]
- 27.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American journal of preventive medicine. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 28.Coutinho SV, Plotsky PM, Sablad M, et al. Neonatal maternal separation alters stress-induced responses to viscerosomatic nociceptive stimuli in rat. Am J Physiol Gastrointest Liver Physiol. 2002;282:G307–16. doi: 10.1152/ajpgi.00240.2001. [DOI] [PubMed] [Google Scholar]
- 29.Gareau MG, Jury J, Yang PC, et al. Neonatal maternal separation causes colonic dysfunction in rat pups including impaired host resistance. Pediatric research. 2006;59:83–8. doi: 10.1203/01.pdr.0000190577.62426.45. [DOI] [PubMed] [Google Scholar]
- 30.Gareau MG, Jury J, Perdue MH. Neonatal maternal separation of rat pups results in abnormal cholinergic regulation of epithelial permeability. American journal of physiology Gastrointestinal and liver physiology. 2007;293:G198–203. doi: 10.1152/ajpgi.00392.2006. [DOI] [PubMed] [Google Scholar]
- 31.Ladd CO, Owens MJ, Nemeroff CB. Persistent changes in corticotropin-releasing factor neuronal systems induced by maternal deprivation. Endocrinology. 1996;137:1212–8. doi: 10.1210/endo.137.4.8625891. [DOI] [PubMed] [Google Scholar]
- 32.Chang L, Sundaresh S, Elliott J, et al. Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis in irritable bowel syndrome. Neurogastroenterol Motil. 2009;21:149–59. doi: 10.1111/j.1365-2982.2008.01171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McGowan PO, Meaney MJ, Szyf M. Diet and the epigenetic (re)programming of phenotypic differences in behavior. Brain Research. 2008;1237:12–24. doi: 10.1016/j.brainres.2008.07.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McGowan PO, Sasaki A, D'Alessio AC, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nature neuroscience. 2009;12:342–8. doi: 10.1038/nn.2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Videlock EJ, Adeyemo M, Licudine A, et al. Childhood trauma is associated with hypothalamic–pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterology. 2009;137:1954–62. doi: 10.1053/j.gastro.2009.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chang L, Toner BB, Fukudo S, et al. Gender, age, society, culture, and the patient's perspective in the functional gastrointestinal disorders. Gastroenterology. 2006;130:1435–1446. doi: 10.1053/j.gastro.2005.09.071. [DOI] [PubMed] [Google Scholar]
- 37.Leserman J, Drossman DA, Li Z, et al. Sexual and physical abuse history in gastroenterology practice: how types of abuse impact health status. Psychosomatic medicine. 1996;58:4–15. doi: 10.1097/00006842-199601000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Leserman J, Li Z, Drossman DA, et al. Selected symptoms associated with sexual and physical abuse history among female patients with gastrointestinal disorders: the impact on subsequent health care visits. Psychological medicine. 1998;28:417–25. doi: 10.1017/s0033291797006508. [DOI] [PubMed] [Google Scholar]
- 39.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130:910–21. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 40.Salmon P, Skaife K, Rhodes J. Abuse, dissociation, and somatization in irritable bowel syndrome: towards an explanatory model. J Behav Med. 2003;26:1–18. doi: 10.1023/a:1021718304633. [DOI] [PubMed] [Google Scholar]
- 41.Hunt MGMM, Moshier S. Catastrophizing the Consequences of Gastrointestinal Symptoms in Irritable Bowel Syndrome. Journal of Cognitive Psychotherapy. 2009;23:160–173. [Google Scholar]
- 42.Van Oudenhove L, Vandenberghe J, Vos R, et al. Risk factors for impaired health-related quality of life in functional dyspepsia. Aliment Pharmacol Ther. 2011;33:261–74. doi: 10.1111/j.1365-2036.2010.04510.x. [DOI] [PubMed] [Google Scholar]
- 43.Nemeroff CB, Heim CM, Thase ME, et al. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proc Natl Acad Sci U S A. 2003;100:14293–6. doi: 10.1073/pnas.2336126100. [DOI] [PMC free article] [PubMed] [Google Scholar]