Abstract
Purpose
The aim of this study was to evaluate, in a meta-analysis, the clinical effectiveness of operative treatment for acute Achilles tendon rupture (AATR) compared with nonoperative treatment.
Methods
We systematically searched six electronic databases (Medline, Embase, Clinical Ovid, BIOSIS and Cochrane registry of controlled clinical trials) to identify randomised controlled trials (RCTs) in which operative treatment was compared with nonoperative treatment for AATR from 1980 to 2011. Trial quality was assessed using the modified Jadad scale. The data was using fixed-effects and random-effects models with mean differences and risk ratios for continuous and dichotomous variables, respectively.
Results
Ten RCTs with a total of 894 patients were screened. The results showed that operative was superior to nonoperative treatment regarding lower risk of re-rupture (P = 0.002) and shorter time for sick leave (P = 0.009) but inferior to nonoperative treatment regarding complication risks (P = 0.004). No significant difference was identified between the two methods regarding the number of patients who successfully returned to pre-injury sports (P = 0.30). Subgroup analyses revealed significant differences in relation to scar adhesion (P < 0.00001), superficial infection (P = 0.05), and sensibility disturbance (P = 0.0003). However, no significant differences were found between the two interventions in relation to deep infection (P = 0.22), deep vein thrombosis (DVT) (P = 0.14), and extreme Achilles tendon lengthening (P = 0.31). Little consensus was obtained in the functional recovery from current trials as a result of an inconsistent assessment system.
Conclusions
Compared with conservative treatment, operative treatment can effectively reduce the risk of re-rupture but increase the probability of complications. The increased complication risk may be associated with open repair surgery. However, no sufficient evidence is available from current studies to support the belief that operation may lead to better functional recovery.
Introduction
The Achilles tendon is the largest and strongest tendon in the human body, but it is also the most frequently ruptured [1, 2]. According to a recent report in Finland [3], the incidence of acute Achilles tendon ruptures increased from 8.3/105 in 1987 to 14.8/105 in 1999 and was thought to be increasing. Achilles tendon ruptures occur most frequently in the age groups of 30–39 and 40–49 years old in men and women [4], with a male predominance [5]. On average, women with a tendon rupture tend to be 2–3 years older than men with ruptures [3, 4]. Many studies report that acute Achilles tendon rupture (AATR) mostly occurs during sports activities [6–10], especially in racket games, football and handball [6, 7, 10, 11]. The mechanism of injury includes a sudden pushing off from the weight-bearing forefoot with the knee in extension, unexpected ankle dorsiflexion and violent dorsiflexion of a plantar-flexed foot [12]. As to aetiology, many possible factors have been proposed [14], such as poor tendon vascularity and tendon degeneration [14, 15], gastrocnemius-soleus dysfunction [14], adverse effects of some drugs (e.g. corticosteroids [16, 17], fluoroquinolones [18, 19]) and exercise-induced hyperthermia [20, 21].
AATR can be managed by both operative and nonoperative strategies. It is generally accepted that operation should be performed for athletes, young and fit patients and that conservative treatment may be suitable for the elderly [22, 23]. However, controversy remains with regard to optimal treatment for AATR. The main reason for this controversy is that both operative and nonoperative treatments have pros and cons. Previous randomised controlled trials (RCTs) [6, 7, 24] concluded that operative treatment could reduce the risk of re-rupture but might also lead to a high rate of postoperative complications, which affect quality of life. Conversely, conservative treatments are thought to be advantageous in that there is a lower rate of complications, but their disadvantage is a higher incidence of re-rupture. Three meta-analyses confirmed the above hypotheses [25–27]. However, these meta-analyses were based on a small sample size and insufficient analyses. The need remains for strong evidence based on the latest high-quality RCTs to test the above conclusions.
The aim of our meta-analysis was to determine the advantages and disadvantages of operative versus nonoperative AATR treatment by comparing clinical outcomes reported in all available related RCTs. We believe this meta-analysis will yield stronger evidence for clinical treatment of AATR.
Methods
Study design and search strategy
All published RCTs comparing operative with nonoperative intervention for AATR were searched for by two authors (NJ, AFC) independently. Databases used for searching were Medline, Embase, Clinical, Ovid, BIOSIS and Cochrane registry of controlled clinical trials. The eligible time was from 1980 to 1September 2011. Publication language was limited to English. Key words used for search were as follows: acute Achilles tendon rupture, acute tendocalcaneus rupture, operation, nonoperation, surgery, conservative treatment, randomised controlled trials and randomisation.
Inclusion and exclusion criteria
Only RCTs that compared operative with nonoperative methods for AATR were taken into consideration. We excluded retrospective studies, cohort studies and clinical controlled studies. Studies without effective reporting of primary results and those with inadequate data for meta-analysis were also excluded. Eligibility criteria were adult patients with a definite diagnosis (e.g. a positive Thompson squeeze test [28], presence of a palpable gap, loss of plantar flexion strength), intervention initiated within 14 days after injury and written informed consent. Exclusion criteria were re-ruptures, open injury, combination with fractures of foot or ankle, additional ipsilateral injury, neurological or vascular damage requiring medications recognised to affect tendon healing, physical or mental problems that might affect recovery and operative contraindications.
Study identification
Two reviewers (BWW, FD) independently screened titles of all articles obtained. The Abstract of any study that was potentially relevant to the topic was reviewed; the full text was obtained if inadequate information was acquired from the Abstract. A third reviewer (BY) was consulted for the final decision if any disagreement on eligibility existed between the first two reviewers.
Data extraction
Two reviewers participated in the extraction of effective data from all eligible RCTs. One reviewer (NJ) extracted all effective data onto a table prepared in advance; a second reviewer (BWW) verified data for accuracy. Disagreement was resolved by discussion, and a third reviewer’s opinion was asked for when necessary. The effective data collected from all trials contained data available for meta-analyses as well as general information regarding studies and participants (study location, number of cases in each group, sex ratio, etc).
Methodological assessment
The study methodological assessment was conducted using the modified Jadad scale [29]. This is an eight-item scale designed to assess randomisation, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse effects and statistical analysis (Table 1). The score for each article could range from 0 (lowest quality) to 8 (highest quality). Scores of 4–8 denote good to excellent quality and 0–3 poor to low quality. Critical appraisal was conducted by one viewer (FD) and was verified by another (AFC).
Table 1.
Modified Jadad Scale with eight items
| Items assessed | Response | Score |
|---|---|---|
| Was the study described as randomised? | Yes | +1 |
| No | 0 | |
| Was the method of randomisation appropriate? | Yes | +1 |
| No | −1 | |
| Not described | 0 | |
| Was the study described as blinded?a | Yes | +1 |
| No | 0 | |
| Was the method of blinding appropriate? | Yes | +1 |
| No | −1 | |
| Not described | 0 | |
| Was there a description of withdrawals and dropouts? | Yes | +1 |
| No | 0 | |
| Was there a clear description of the inclusion/exclusion criteria? | Yes | +1 |
| No | 0 | |
| Was the method used to assess adverse effects described? | Yes | +1 |
| No | 0 | |
| Was the method of statistical analysis described? | Yes | +1 |
| No | 0 |
aDouble-blind randomised controlled trials 1 score; single-blind RCTs 0.5 score
Outcomes for meta-analysis
Primary outcomes consisted of incidences of re-rupture and complications other than re-rupture. Secondary outcomes included the number of patients who recovered to pre-injury sports, mean time for sick leave (period from injury to return to pre-injury work or sports), results for subgroup meta-analyses (scar adhesion, superficial infection et al.).
Statistical analysis
The primary analysis was to compare outcomes between operative and nonoperative management of AATR from all RCTs included. Next, a secondary sensitivity analysis, which compared outcomes from high Jadad score RCTs (≥4 points) only, with those from all RCTs analysed was designed to ensure low Jadad score RCTs (<4 points) did not bias the primary analysis. Statistical heterogeneity was evaluated using I2 statistics, complying with Quality of Reporting of Meta-Analyses (QUOROM) guidelines [30], which describe the percentage of total variation across studies that is due to heterogeneity rather than chance. I2 can be readily calculated from basic results obtained from a typical meta-analysis as, I2 = 100% × (Q–df)/Q, where Q is Cochrane’s heterogeneity statistic and df is the degrees of freedom [31]. Substantial heterogeneity exists when I2 >50%. For outcomes when P>0.05, a fixed-effects model was used; a random-effects model was adopted for P≤0.05. Dichotomous data are presented as relative risk (RR) and continuous variables as mean difference (MD), both with 95% confidence intervals (CI). To determine whether significant differences would exist in specific complications between the two interventions investigated, subgroup analyses were carried out by sorting the same specific complications reported in enrolled RCTs. The meta-analysis was performed by RevMan 5.1 software (Cochrane Collaboration, Oxford, UK) for outcome measures. A P value of ≤0.05 was considered statistically significant.
Results
Identification of relevant literature
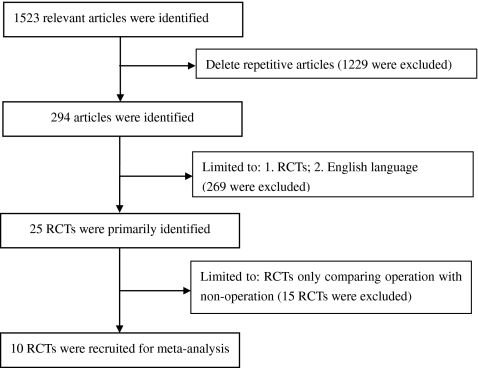
The literature-retrieving strategy and results are shown in Fig. 1. Ten published RCTs [6–8, 10, 24, 32–36] with a total of 894 patients met all inclusion criteria. Information on general characteristics of studies and participants are listed in Table 2.
Fig. 1.
Eligibility selection
Table 2.
General information on randomised controlled trials (RCTs) included
| Source, year, country | Cases (O/N) |
Sex ratio (M/F) |
Mean age (O/N) (year) |
Injury side (L/R) |
Follow-up (year) |
Jadad scores |
|---|---|---|---|---|---|---|
| Nistor et al. [6], 1981, Sweden | 45/60 | 96/11 | 41a | 58/48 | 2.5b | 2 |
| Cetti et al. [7], 1993, Denmark | 56/55 | 92/19 | 37.2/37.8 | 65/46 | 1.0 | 4 |
| Schroeder et al. [32], 1997, Germany | 13/15 | NM | 44/38 | NM | 0.67c | 3 |
| Moller et al. [24], 2001, Sweden | 59/53 | 99/13 | 39.6/38.5 | 64/48 | 2.0 | 6 |
| Costa et al. [33], 2006, England | 48/48 | 72/23 | 42/53 | 54/40 | 1.0 | 4 |
| Twaddle et al. [36], 2007, New Zealand | 20/22 | 28/14 | 41.8/40.3 | 22/20 | 1.0 | 5 |
| Metz et al. [8], 2008, Netherlands | 42/41 | 66/17 | 40/41 | 49/34 | 1.0 | 6 |
| Nilsson-Helander et al.[34], 2010, Sweden | 49/48 | 79/18 | 40.9/41.2 | 47/50 | 1.0 | 5 |
| Willits et al.[35], 2010, Canada | 72/72 | 118/26 | 39.7/41.1 | NM | 2.0 | 5 |
| Keating et al.[10], 2011, England | 39/41 | 60/20 | 41.2/39.5 | NM | 1.0 | 5 |
O/N operative group/nonoperative group, L/R left side/right side, NM not mentioned
a41 total average age, b2.5 mean follow-up, range 1–5 years, c0.67 mean follow-up, range 0.5–1 year
Methodological quality assessment
Total RCT scores are shown in Table 2, indicating that most studies achieved high quality by the current rating system. Eight designs scored ≥4, but the main problem reflected in nearly all studies was the nonuse of blinding method, which might bring about a certain degree of detection bias. The two studies [6, 32] that scored <4 had inappropriate randomisation, and there was no detailed information on withdrawals and dropouts in one report [32]
Meta-analyses
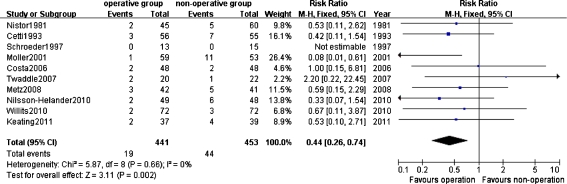
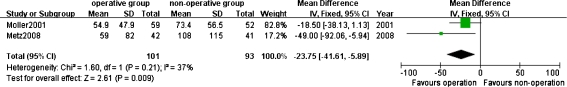
As revealed in Fig. 2, 19 of 441 patients (4.31%) in the operative group had re-ruptures after treatment compared with 44 of 453 patients (9.71%) in the nonoperative group, with a significant difference between the two groups [RR 0.44, 95% CI (0.26–0.74), P = 0.002,]. Nonetheless, Fig. 3 shows that patients managed with surgery had a higher complication rate than those managed with conservative treatment [26.60% (112/421) vs. 7.19% (31/431)] [RR 4.07, 95% CI (1.56–10.67), P = 0.004]. Also, mean time for sick leave following operative treatment was shorter than following nonoperative treatment [MD – 23.75, 95% CI (–41.61 to – 5.89), P = 0.009, Fig. 4]. No statistically significant difference was found between the two methods in the number of patients who resumed pre-injury sports [RR1.16, 95% CI (0.88–1.53), P = 0.30, Fig. 5].
Fig. 2.
Incidence of rerupture after operative and nonoperative treatments
Fig. 3.
Incidence of complications after operative and nonoperative treatments
Fig. 4.
Mean time for sick leave in operative and nonoperative groups
Fig. 5.
Number of patients who successfully resumed pre-injury sports after treatments
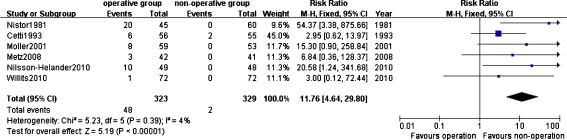
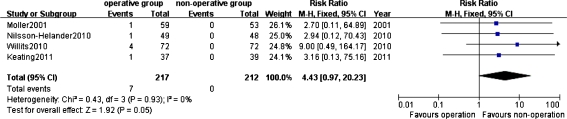
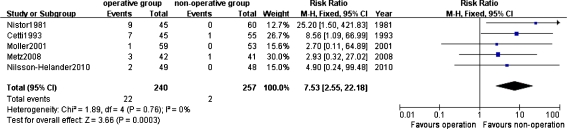
Subgroup meta-analyses were further performed because high heterogeneity (I2 = 78%) existed among studies that were available for the comparison of complications. The operative group showed a significantly higher complication rate than the nonoperative group in terms of scar adhesion [RR11.76, 95% CI (4.64–29.80), P<0.00001, Fig. 6], superficial infection [RR 4.43, 95 % CI (0.97–20.23), P = 0.05, Fig. 7] and sensibility disturbance [RR = 7.53, 95% CI (2.55–22.18), P = 0.0003, Fig. 8]. However, as revealed in Table 3, few significant differences were observed with respect to deep infection [RR 2.07, 95% CI (0.64–6.69), P = 0.22], DVT [RR = 0.37, 95% CI (0.10–1.38), P = 0.14] or extreme Achilles tendon lengthening [RR0.31, 95% CI (0.03–2.97), P = 0.31].
Fig. 6.
Incidence of scar adhesion after operative and nonoperative treatments
Fig. 7.
Incidence of superficial infection after operative and nonoperative treatments
Fig. 8.
Incidence of sensibility disturbance after operative and nonoperative treatments
Table 3.
Complications with no significant differences between the two methods by subgroup analyses
| Complications | Studies included | ||||
|---|---|---|---|---|---|
| Number | Patients | I2 | RR (95% CI) | P values | |
| Deep infection | 5 [6, 7, 10, 34, 35] | 533 | 0% | 2.07 (0.64, 6.69) | 0.22 |
| DVT | 5 [8, 10, 24, 33, 35] | 511 | 0% | 0.37 (0.10, 1.38) | 0.14 |
| Extreme tendon lengthening | 2 [7, 24] | 223 | 0% | 0.31 (0.03, 2.97) | 0.31 |
RR risk ratio, CI confidence interval, DVT deep vein thrombosis
Functional assessment
No meta-analysis on functional recovery was carried out because different assessment systems had been used in the studies and few effective data could be extracted and pooled. Outcomes and conclusions concerning functional recovery varied. Nistor et al. [6] reported that more operatively treated patients had difficulty wearing shoes and felt stiffness in the ankle. This is in disagreement with Cetti et al. [7], who stated that 1 year after injury, operatively treated patients had a significantly reduced severity of calf atrophy, better ankle movement and fewer complaints. Outcomes of visual analogue score recorded by Moller et al. [24] showed that the operative group had higher mean scores than the nonoperative group at 2-year follow-up. Nilsson-Helander et al. [34] found that operatively treated patients had better results in some muscle-function tests at the 6-month evaluation and in heel-rise work at 12-month evaluation. However, Moller et al. [24] indicated that operative and nonoperative treatments produced equally good results if complications were avoided. Outcomes from Keating et al. [10] revealed no convincing benefits from surgery, which was consistent with findings by Willits et al. [35]. Therefore, no consensus was reached in functional recovery based on the current studies.
Sensitivity analysis
Sensitivity analysis was performed by excluding low-quality studies (Jadad score <4). RRs, 95% CIs and P values for incidences of rerupture and complications, scar adhesion, sensibility disturbance and deep infection were still similar to results before exclusion of low-quality studies (Table 4). This indicates that low-score RCTs had no bias on results of our meta-analyses.
Table 4.
Results of sensitivity analysis
| Outcomes | All eligible RCTs included | Only high-score RCTs included | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Patients | I2 | RR (95% CI) | P values | Number | Patients | I2 | RR (95% CI) | P values | |
| Re-rupture | 10 | 894 | 0% | 0.44 (0.26, 0.74) | 0.002 | 8 | 761 | 0% | 0.43 (0.25, 0.74) | 0.002 |
| Complications | 9 | 852 | 78% | 4.07 (1.56,10.67) | 0.004 | 7 | 719 | 75% | 3.07 (1.17, 8.06) | 0.02 |
| Scar adhesion | 6 | 652 | 4% | 11.76 (4.64, 29.80) | <0.00001 | 5 | 547 | 0% | 7.24 (2.58, 20.34) | 0.0002 |
| Sensibility disturbance | 5 | 497 | 0% | 7.53 (2.55, 22.18) | 0.0003 | 4 | 392 | 0% | 4.95 (1.47, 16.64) | 0.01 |
| Deep infection | 5 | 533 | 0% | 2.07 (0.64, 6.69) | 0.22 | 4 | 428 | 0% | 4.02 (0.87, 18.67) | 0.08 |
RCT randomised controlled trial, RR relative risk, CI confidence interval
Discussion
Results of our meta-analyses that included a greater number of latest RCTs available once again confirmed that in AATR treatment, operation can effectively reduce the risk of re-rupture but is unlikely to avoid a high complication rate. This is in accordance with the conclusion proposed by Khan et al. [25, 26] Our meta-analyses, however, offered new findings. Our subgroup analyses found scar adhesion, superficial infection and sensibility disturbance are significantly associated with open repair surgery. Secondly, surgically treated patients may have shorter mean sick leave time than those treated nonoperatively. In other words, operation can lead to a faster recovery in time, though disagreements exist in specific functional outcomes.
Some basic epidemiological information can be derived from Table 2. First, it is noticeable that men accounted for 81.52% of all AATR patients. Male dominance (4.41:1) may indicate that those who participate in activities with higher violence are mostly men. Second, most AATR patients were in their 30s–40s. This suggests that the middle-aged population should be given more advice on violent activities because their Achilles tendons are no longer as strong as they were in adolescence. Third, the left side is more prone to AATR than the right side (359 vs. 286) (according to seven RCTs). This interesting fact may be due to habitual foot usage in human beings.
Besides our present meta-analysis, most current relevant researches indicates that nonoperatively treated AATR patients tend to have a higher re-rupture rate. This statistically significant difference can be explained by two factors: First, after healing without surgical suture, the once-ruptured Achilles tendons do not bear the intensity of pre-injury activities well. The usual immobilisation period of 6–8 weeks in nonoperative treatment seems insufficient to allow tendon recovery. Twaddle et al. [36], however, had an opposite finding: that re-rupture rate was lower in the nonoperative group. They explained that this might be a consequence of early functional rehabilitation. This disagreement may imply an important role of different therapy strategies, such as early functional rehabilitation, in nonoperative treatment. Whether or not different therapy strategies can make a difference needs further clinical trials.
We confirmed a higher complication rate in operated AATR patients than in those undergoing conservative treatment (26.60% vs 7.19%). On the other hand, we found a relatively high heterogeneity (I2 = 78%) among the RCTs included. A random-effects model and subgroup analyses were therefore designed to reduce potential biases because we believe the complication rate could not be regarded as one entity. There were different complications, which might cause differences. As a result, subgroup analyses revealed significant differences between the two treatment types in regard to scar adhesion, superficial infection and sensibility disturbance, but not in deep infection, DVT or extreme tendon lengthening. It is interesting that one RCT in this study [6] reported that patients undergoing conservative treatment had more deep infections than operatively treated patients (2 vs 0). As this RCT study had more than a half weight (51.8%) in the deep infection subgroup analysis, another meta-analysis seemed necessary. However, this RCT was just excluded because of its low Jadad score regarding sensitivity analysis for bias, the result of which indicated that there was still no statistically significant difference in the incidence of deep infection [RR4.02, 95% CI (0.87–18.67), P = 0.08].
In disagreement with our second finding, two studies [8, 24] suggested that the nonoperative group did not have longer sick leave. We did not include these two studies because they failed to present the results in means and SDs for meta-analysis. In addition, the studies reported different findings in the time of sick leave. One [6] indicated that the nonoperative group had obviously shorter sick leave, whereas the other [7] indicated there was no significant difference in this respect. Therefore, more RCTs are needed to certify this conclusion.
We believe that the conclusions reached in this meta-analysis comparing operative and nonoperative AATR treatment may be changed if conventional therapies are improved. For example, we found an association between open repair surgery and wound problems. This association, however, is likely to be changed by improved techniques for open surgery. Recently, percutaneous repair techniques have been adopted as new operative procedures that attempt to reduce complications caused by open surgery and has exhibited good efficacy. An up-to-date systematic review performed by Khan et al. [25], along with several most recent studies [37–42], indicate that compared with open repair, percutaneous repair results in a lower complication rate. Moreover, Maffulli et al. [43, 44] proved that percutaneous repair of Achilles tendon was not only available for diabetic patients but also suitable for patients >65 years. Furthermore, Kosanovic et al. [45] showed that percutaneous repair was effective in treating chronic Achilles tendon rupture. In a recent meta-analysis, McMahon et al. [46] concluded that percutaneous minimally invasive surgery had a significantly reduced risk of superficial wound infection and a three times larger number of patients with good to excellent results compared with conventional open repair. Gigante et al. [47], in a RCT, found that percutaneous repair surgery had significantly shorter operating time than did open repair surgery (P<0.01).
Likewise, technical progresses are ongoing in conservative AATR treatment, with improved outcomes. According to a latest study by Wallace et al. [48], patients undergoing nonoperative functional management had a similar or even lower rate of re-rupture than operatively treated ones, regardless of presentation time (acute presentation or delayed presentation after more than 2 weeks). Similarly, Hufner et al. [49] emphasised the decisive advantages and better results of conservative functional therapy.
High heterogeneity among the relevant RCTs we analysed may be a limitation to our meta-analysis. Of the ten RCTs, only five reported the number of patients who successfully returned to pre-injury sports and found no significant difference between the two-methods. But a high heterogeneity (I2 = 70%) existed among these studies, probably because the levels and intensities of pre-injury sports had not been clearly specified. This high heterogeneity can definitely compromise the credibility of the findings and prevent further specific subgroup analyses. Unfortunately, in outcomes assessment for AATR management, we still lack uniform, specific end points or criteria, especially regarding functional recovery. RCTs without uniform, specific end points or criteria can hardly produce high-quality meta-analysis.
The lack of adequate RCTs and consistent functional assessment system are the main weakness of studies on AATR. It is worth mentioning that Metz et al. [50] first proposed an appropriate RCT design in 2007. On the basis of their proposal, we suggest an “ultimate” RCT on the topic at hand, which should include the following necessary elements: correct methods of randomisation and blinding, inclusion and exclusion criteria clearly defined, appropriate statistical methods and an ample sample size (at least 36 participants each group). It should contain main outcome measures of three categories: evaluation scales, daily activity assessment and post treatment complications. Evaluation scales should include the most frequently used and validated scales or scores, such as American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot scale, Achilles Tendon Total Rupture Score (ATRS), visual analogue Scale (VAS) etc. The daily activity assessment system should be composed of two sections: physical functional measures with specific items (e.g. mean range of ankle movement, strength of plantar flexion and dorsiflexion and side-to-side difference in calf circumference) and social functional measures with specific items (e.g. mean time for sick leave, recovery to pre-injury foot-related activities and residual pain). We suggest that the pre-injury foot-related activities should be further specified as daily activity level, recreational sports level and competitive sports level. Complications should be reported in detail as much as possible. With respect to follow-up, we suggest that, if possible, participants be reviewed and followed at 6 weeks, 3 months, 6 months, 1 year and 2 years. With adequate specific data from RCTs, we believe in-depth comparison and classification can be conducted in a meta-analysis to provide more convincing evidence for precise assessment of operative and nonoperative treatment of AATR.
Conclusions
In summary, our meta-analyses confirmed that operative AATR treatment can effectively reduce the risk of re-rupture but may also lead to more complications related to open surgery. On the other hand, nonoperative AATR treatment may have a low risk of complications but a high risk of re-rupture. The meta-analyses failed to validate an insignificant difference in functional recovery between the two methods. Based on current evidence, we find it difficult to determine whether one is superior to the other. We believe that major technical improvements in either operative or nonoperative treatment will change their advantages and disadvantages. We hope there will be more multicentre, large-scale RCTs comparing AATR therapeutic strategies with high methodological quality and consistent assessment systems or specific measures, particularly for post treatment functional recovery.
Acknowledgments
The authors thank Professor Allen P. Liang for revision and editing of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Ames PR, Longo UG, Denaro V, Maffulli N. Achilles tendon problems: not just an orthopaedic issue. Disabil Rehabil. 2008;30:1646–1650. doi: 10.1080/09638280701785882. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS. Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med. 1999;9:157–160. doi: 10.1097/00042752-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Nyyssonen T, Luthje P, Kroger H. The increasing incidence and difference in sex distribution of Achilles tendon rupture in Finland in 1987–1999. Scand J Surg. 2008;97:272–275. doi: 10.1177/145749690809700312. [DOI] [PubMed] [Google Scholar]
- 4.Suchak AA, Bostick G, Reid D, Blitz S, Jomha N. The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int. 2005;26:932–936. doi: 10.1177/107110070502601106. [DOI] [PubMed] [Google Scholar]
- 5.Hattrup SJ, Johnson KA. A review of ruptures of the Achilles tendon. Foot Ankle. 1985;6:34–38. doi: 10.1177/107110078500600107. [DOI] [PubMed] [Google Scholar]
- 6.Nistor L. Surgical and non-surgical treatment of Achilles Tendon rupture. A prospective randomized study. J Bone Joint Surg Am. 1981;63:394–399. [PubMed] [Google Scholar]
- 7.Cetti R, Christensen SE, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. doi: 10.1177/036354659302100606. [DOI] [PubMed] [Google Scholar]
- 8.Metz R, Verleisdonk EJ, Heijden GJ, Clevers GJ, Hammacher ER, Verhofstad MH, Werken C. Acute Achilles tendon rupture: minimally invasive surgery versus nonoperative treatment with immediate full weightbearing–a randomized controlled trial. Am J Sports Med. 2008;36:1688–1694. doi: 10.1177/0363546508319312. [DOI] [PubMed] [Google Scholar]
- 9.Thompson J, Baravarian B. Acute and chronic Achilles tendon ruptures in athletes. Clin Podiatr Med Surg. 2011;28:117–135. doi: 10.1016/j.cpm.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 10.Keating JF, Will EM. Operative versus non-operative treatment of acute rupture of tendo Achillis: A PROSPECTIVE RANDOMISED EVALUATION OF FUNCTIONAL OUTCOME. J Bone Joint Surg Br. 2011;93:1071–1078. doi: 10.1302/0301-620X.93B8.25998. [DOI] [PubMed] [Google Scholar]
- 11.Gwynne-Jones DP, Sims M, Handcock D. Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int. 2011;32:337–343. doi: 10.3113/FAI.2011.0337. [DOI] [PubMed] [Google Scholar]
- 12.Arner O, Lindholm A. Subcutaneous rupture of the Achilles tendon; a study of 92 cases. Acta Chir Scand Suppl. 1959;116:1–51. [PubMed] [Google Scholar]
- 13.Longo UG, Ronga M, Maffulli N (2009) Acute ruptures of the achilles tendon. Sports Med Arthrosc 17:127–138 [DOI] [PubMed]
- 14.Maffulli N. Achilles tendon rupture. Br J Sports Med. 1995;29:279–280. doi: 10.1136/bjsm.29.4.279-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams JG. Achilles tendon lesions in sport. Sports Med. 1993;16:216–220. doi: 10.2165/00007256-199316030-00006. [DOI] [PubMed] [Google Scholar]
- 16.McQuillan R, Gregan P. Tendon rupture as a complication of corticosteroid therapy. Palliat Med. 2005;19:352–353. doi: 10.1177/026921630501900412. [DOI] [PubMed] [Google Scholar]
- 17.Kao NL, Moy JN, Richmond GW. Achilles tendon rupture: an underrated complication of corticosteroid treatment. Thorax. 1992;47:484. doi: 10.1136/thx.47.6.484-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seeger JD, West WA, Fife D, Noel GJ, Johnson LN, Walker AM. Achilles tendon rupture and its association with fluoroquinolone antibiotics and other potential risk factors in a managed care population. Pharmacoepidemiol Drug Saf. 2006;15:784–792. doi: 10.1002/pds.1214. [DOI] [PubMed] [Google Scholar]
- 19.Linden PD, Sturkenboom MC, Herings RM, Leufkens HG, Stricker BH. Fluoroquinolones and risk of Achilles tendon disorders: case–control study. BMJ. 2002;324:1306–1307. doi: 10.1136/bmj.324.7349.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wilson AM, Goodship AE. Exercise-induced hyperthermia as a possible mechanism for tendon degeneration. J Biomech. 1994;27:899–905. doi: 10.1016/0021-9290(94)90262-3. [DOI] [PubMed] [Google Scholar]
- 21.Birch HL, Wilson AM, Goodship AE. The effect of exercise-induced localised hyperthermia on tendon cell survival. J Exp Biol. 1997;200:1703–1708. doi: 10.1242/jeb.200.11.1703. [DOI] [PubMed] [Google Scholar]
- 22.Raisbeck CC. Rupture of the Achilles tendon. J Bone Joint Surg Am. 2000;82-A:1804–1805. doi: 10.2106/00004623-200012000-00016. [DOI] [PubMed] [Google Scholar]
- 23.Martinelli B (2000) Rupture of the Achilles tendon. J Bone Joint Surg Am 82-A:1804 [DOI] [PubMed]
- 24.Moller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83:843–848. doi: 10.1302/0301-620X.83B6.11676. [DOI] [PubMed] [Google Scholar]
- 25.Khan RJ, Carey SR (2010) Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev:D3674 [DOI] [PubMed]
- 26.Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202–2210. doi: 10.2106/JBJS.D.03049. [DOI] [PubMed] [Google Scholar]
- 27.Bhandari M, Guyatt GH, Siddiqui F, Morrow F, Busse J, Leighton RK, Sprague S, Schemitsch EH (2002) Treatment of acute Achilles tendon ruptures: a systematic overview and metaanalysis. Clin Orthop Relat Res:190–200 [DOI] [PubMed]
- 28.Thompson TC, Doherty JH. Spontaneous rupture of tendon of Achilles: a new clinical diagnostic test. J Trauma. 1962;2:126–129. doi: 10.1097/00005373-196203000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord. 2001;12:232–236. doi: 10.1159/000051263. [DOI] [PubMed] [Google Scholar]
- 30.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schroeder D, Lehmann M, Steinbrueck K (1997) Treatment of acute achilles tendon ruptures: open vs. percutaneous repair vs. conservative treatment. A prospective randomized study. Orthopaedic Transactions 21:1228
- 33.Costa ML, MacMillan K, Halliday D, Chester R, Shepstone L, Robinson AH, Donell ST. Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg Br. 2006;88:69–77. doi: 10.1302/0301-620X.88B1.16549. [DOI] [PubMed] [Google Scholar]
- 34.Nilsson-Helander K, Silbernagel KG, Thomee R, Faxen E, Olsson N, Eriksson BI, Karlsson J. Acute achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38:2186–2193. doi: 10.1177/0363546510376052. [DOI] [PubMed] [Google Scholar]
- 35.Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, Kean CO, Kirkley A. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:2767–2775. doi: 10.2106/JBJS.I.01401. [DOI] [PubMed] [Google Scholar]
- 36.Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med. 2007;35:2033–2038. doi: 10.1177/0363546507307503. [DOI] [PubMed] [Google Scholar]
- 37.Valente M, Crucil M, Alecci V, Frezza G (2011) Minimally invasive repair of acute Achilles tendon ruptures with Achillon device. Musculoskelet Surg [DOI] [PubMed]
- 38.Henriquez H, Munoz R, Carcuro G, Bastias C (2011) Is Percutaneous Repair Better Than Open Repair in Acute Achilles Tendon Rupture? Clin Orthop Relat Res [DOI] [PMC free article] [PubMed]
- 39.Tenenbaum S, Dreiangel N, Segal A, Herman A, Israeli A, Chechik A. The percutaneous surgical approach for repairing acute Achilles tendon rupture: a comprehensive outcome assessment. J Am Podiatr Med Assoc. 2010;100:270–275. doi: 10.7547/1000270. [DOI] [PubMed] [Google Scholar]
- 40.Rouvillain JL, Navarre T, Labrada-Blanco O, Garron E, Daoud W. Percutaneous suture of acute Achilles tendon rupture. A study of 60 cases. Acta Orthop Belg. 2010;76:237–242. [PubMed] [Google Scholar]
- 41.Sirovy M, Carda M. Open vs. percutaneous suture repair of the subcutaneous Achilles tendon rupture. Rozhl Chir. 2007;86:594–599. [PubMed] [Google Scholar]
- 42.Elliot RR, Calder JD. Percutaneous and mini-open repair of acute Achilles tendon rupture. Foot Ankle Clin. 2007;12:573–582. doi: 10.1016/j.fcl.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 43.Maffulli N, Longo UG, Ronga M, Khanna A, Denaro V. Favorable outcome of percutaneous repair of achilles tendon ruptures in the elderly. Clin Orthop Relat Res. 2010;468:1039–1046. doi: 10.1007/s11999-009-0944-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maffulli N, Longo UG, Maffulli GD, Khanna A, Denaro V. Achilles tendon ruptures in diabetic patients. Arch Orthop Trauma Surg. 2011;131:33–38. doi: 10.1007/s00402-010-1097-0. [DOI] [PubMed] [Google Scholar]
- 45.Kosanovic M, Brilej D. Chronic rupture of Achilles tendon: is the percutaneous suture technique effective? Arch Orthop Trauma Surg. 2008;128:211–216. doi: 10.1007/s00402-007-0514-5. [DOI] [PubMed] [Google Scholar]
- 46.McMahon SE, Smith TO, Hing CB. A meta-analysis of randomised controlled trials comparing conventional to minimally invasive approaches for repair of an Achilles tendon rupture. Foot Ankle Surg. 2011;17:211–217. doi: 10.1016/j.fas.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 47.Gigante A, Moschini A, Verdenelli A, Del TM, Ulisse S, Palma L. Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2008;16:204–209. doi: 10.1007/s00167-007-0448-z. [DOI] [PubMed] [Google Scholar]
- 48.Wallace RG, Heyes GJ, Michael AL. The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture. J Bone Joint Surg Br. 2011;93:1362–1366. doi: 10.1302/0301-620X.93B10.26187. [DOI] [PubMed] [Google Scholar]
- 49.Hufner T, Gaulke R, Imrecke J, Krettek C, Stubig T. Conservative functional treatment of Achilles tendon ruptures. Unfallchirurg. 2010;113(699–702):704. doi: 10.1007/s00113-010-1833-5. [DOI] [PubMed] [Google Scholar]
- 50.Metz R, Kerkhoffs GM, Verleisdonk EJ, Heijden GJ. Acute Achilles tendon rupture: minimally invasive surgery versus non operative treatment, with immediate full weight bearing. Design of a randomized controlled trial. BMC Musculoskelet Disord. 2007;8:108. doi: 10.1186/1471-2474-8-108. [DOI] [PMC free article] [PubMed] [Google Scholar]