Abstract
Purpose
There is little evidence to support immediate weight bearing after uncemented total hip arthroplasty (THA).
Methods
Thirty-seven patients with unilateral osteoarthritis of the hip received a press-fit cup. Cup stability was assessed with radiostereometry (RSA) over five years. Patients were randomised to immediate full weight bearing, or partial weight bearing for three months.
Results
At five years, we found no difference in micromotion as assessed with radiostereometry. Numerically, there was more proximal translation and increased inclination with immediate weight bearing, but these values barely exceeded the precision limit for the method. Pooled data for the two groups revealed translations of 0.1-0.3 mm and rotations of 0.2-0.3° over the five year follow-up period.
Conclusions
We found no adverse effects of immediate weight bearing after THA in relation to stability of these press-fit cups. Early mobilisation might have other advantages.
Introduction
The regime for postoperative rehabilitation after uncemented total hip arthroplasty (THA) has shifted from partial weight bearing for six–12 weeks towards immediate full weight bearing. Immediate weight bearing may in theory be beneficial regarding rehabilitation time and minimising bone mineral loss due to disuse but may jeopardise initial stability and prevent safe bone ingrowth. Previous controlled studies show no adverse effects of immediate weight bearing as assessed with radiographs [1], radiographs and scintigraphy [2] or radiostereometric analysis (RSA) [3]. Few studies, however, have used a randomised protocol to examine the effect of rehabilitation [3, 4] and, to our knowledge, only Thien et al. [3] have investigated acetabular cup stability in relation to the postoperative weight-bearing regime. Our primary aim was to compare immediate postoperative with partial weight bearing for three months after uncemented THA in relation to the effect on the primary outcome parameters: proximal migration and change in inclination of acetabular press-fit cups. A secondary aim was to analyse the pattern of cup micromotion over the five year follow-up period.
Materials and methods
Forty-three patients who gave informed consent were enrolled between 2000 and 2003 in this randomised controlled trial (RCT). The local ethics committee approved of the study (Ups 99242). Inclusion criteria were unilateral radiographically verified osteoarthritis of the hip (OAH), age between 25 and 65 years and weight <110 kg. Exclusion criteria were patients receiving steroids or other medication known to affect bone metabolism. malignancy, previous hip surgery, body mass index (BMI) >35 and residence outside the Uppsala municipality. Patients were randomised either to immediate postoperative (I group) or to partial weight bearing (P group) for three months. Patients in the P group were instructed to bear weight partially, approximately 15 kg, for three months. To evaluate compliance, weight bearing was assessed with the F-scan system (Tekscan™ Inc, MA, USA) before surgery and one week and three, six, 12 and 24 months after surgery, as previously described [5]. Patient characteristics of gender, age, weight, height, and BMD were similar in both groups. Z-scores for BMD at the femoral neck (FN) and total hip (TH) were above (or just below) zero, indicating normal BMD for age (Table 1).
Table 1.
Patient characteristics; mean (standard deviation)
| All | I group | P group | P value* | |
|---|---|---|---|---|
| No. of patients | 30 | 13 | 17 | |
| Sex, M/F | 14/16 | 6/7 | 8/9 | |
| Cups, I/A (M) | 14/16 | 6 (3)/7 (3) | 8 (3)/9 (5) | |
| Age, years | 54 (10) | 53 (12) | 54 (8) | 0.8 |
| Weight, kg | 79 (14) | 80 (14) | 79 (14) | 0.9 |
| Height, cm | 171 (9) | 172 (9) | 170 (9) | 0.6 |
| BMD FNa, g/cm2 | 1.02 (0.1) | 1.01 (0.1) | 1.03 (0.1) | 0.8 |
| Z-score FNa | 0.6 (1.2) | 0.5 (1.2) | 0.6 (1.2) | 0.8 |
| BMD THa, g/cm2 | 1.0 (0.1) | 1.0 (0.1) | 1.0 (0.1) | 0.8 |
| Z-score THa | −0.1 (1.2) | 0.0 (1.0) | −0.1 (1.2) | 0.8 |
I group immediate weight bearing, P group partial weight bearing. I/A Interop/Allofit cup, BMD FN bone mineral density femoral neck, Z-score standard deviation from an age- and gender-matched reference, TH total hip,
a26 patients with dual-energy X-ray absorptiometry scans (12 I group/14 P group)
* P value t test between I and P groups
Three of the 43 patients had a contralateral THA within five years and were excluded in accordance with the study protocol (not strictly unilateral OAH). One patient was intra-operatively converted to a cemented femoral stem and was not included. All patients received the CLS hip stem (Centerpulse, now Zimmer Co, Warsaw, IN, USA) with a 28-mm cobalt–chrome head. The original study included the use of the uncemented Interop acetabular cup (Centerpulse, now Zimmer) with a hemispherical porous shell with sealed screw holes, but manufacturing problems with oil-contaminated shells led to withdrawal of this product from the market [6]. Thus, only 15 Interop acetabular cups were inserted. The Allofit acetabular cup without screw holes (Centerpulse, now Zimmer) was used for the remaining 24 patients. The cup is designed as a hemispherical porous shell with sealed screw holes with a roughened cancellised titanium back surface. The Allofit cup has a grit-blasted titanium surface without screw holes and a sealed centring hole. Both press-fit cups were combined with a polyethylene hooded insert. Five experienced surgeons performed the operations in a standardised way in accordance with the manufacturer’s manual, using an anterolateral approach with the patient in the lateral position.
Radiostereometry
The RSA procedure has been widely used for studying implant stability [7, 8]. Cups were marked with five to eight tantalum markers at the outer rim of the polyethylene hooded insert. In addition, the titanium shells were marked pre-operatively with one tantalum marker on the central button at the bottom (Fig. 1). RSA baseline examinations were performed within five to seven days after surgery. Follow-up examinations were done after one and three months and one, two and five years. A specially trained radiology research nurse performed all examinations. Examinations with a scatter corresponding to a condition number (CN) of < 155 [at three months, median CN 33 (range 27–91)] and a stability corresponding to ME (mean error of rigid body fitting) < 0.3 mm [at three months, median ME 0.137 (range 0.058–0.276)] were included for analysis. The precision of our RSA measurements in this study setup was based on 33 duplicate cup examinations (Table 2). Cup micromotion was measured as translations of the centre of the rigid body along three axes and as rotations around these three axes. We used UmRSA Analysis 6.0 (RSA Biomedical, Umeå, Sweden) for measurements and calculations.
Fig. 1.
The Interop cup with sealed screw holes and a central button marked with a tantalum marker (right)
Table 2.
Acetabular cup micromotion precision
| Type of motion | |
|---|---|
| Translation (mm) | |
| Medial/lateral | 0.27 |
| Proximal/distal | 0.23 |
| Anterior/posterior | 0.34 |
| Rotation (°) | |
| Anterior/posterior tilt | 0.87 |
| Ante-/retroversion | 1.17 |
| Inclination | 0.54 |
95% prediction interval about zero for significant motions based on 33 duplicate examinations
DXA
The study protocol included pre-operative BMD measurements, grams per square metre of pressure unit (g/cm2), with dual-energy X-ray absorptiometry (DXA) (DPX-L, Lunar Co, Madison, WI, USA) of the proximal femur bilaterally. Three regions of interest (ROI)—FN, trochanteric region (TR) and TH—were analysed. Results are also presented as Z-scores, i.e. standard deviations (SD) from an age- and gender-matched reference population of Caucasians, National Health and Nutrition Examination Survey (NHANES) III [9]. This allowed a rough estimate of bone quality of the affected hips [10]. The long-term precision error for a lumbar spine phantom expressed as the percent coefficient of variation (%CV) was <1% during the study period.
Exclusions
Thirty-nine patients were thus eligible for assessment according to the study protocol: two of these were excluded, one (Allofit cup) died of pulmonary embolism three months postoperatively and one received an unmarked Interop cup. Seven of the remaining 37 patients (all with Allofit cups, one of whom underwent a stem revision after 1.5 years because of aseptic loosening) were excluded from analyses because of inadequate visualisation of tantalum markers or poor marker stability. Thus, 30 patients (Table 1) remained for analysis with RSA. One patient, randomised to the P group, had an Interop cup revision within 20 months because of loosening. This patient remained in the study for the first year after the initial surgery. At the five year follow-up, one additional patient had died, and one patient had moved and did not attend the follow-up. Thus, 27 patients (one after 7.5 years; no migration between two year and 7.5-year examination) completed the five year follow-up. Not all patients could be analysed at all time points because of either a too high CN or a too high ME (Table 3). Twenty-six of the 30 patients underwent preoperative DXA on the operated hip.
Table 3.
Micromotion of the 30 press-fit cups from baseline at one week to one and three months, and to one, two and five years. Immediate versus partial weight bearing (WB)
| one month | three months | one year | two years | five years | |
|---|---|---|---|---|---|
| Number (I/P)a | (12/16) | (13/16) | (12/14) | (11/11) | (9/11) |
| Translation (mm) | |||||
| Medial (+)/lateral (−) | |||||
| Immediate WB | 0.04 (0.4) | 0.06 (0.5) | −0.2 (0.6) | −0.05 (0.8) | −0.07 (0.6) |
| Partial WB | 0.2 (0.5) | 0.1 (0.7) | 0.3 (0.8) | 0.3 (0.9) | 0.2 (0.5) |
| Proximal (+)/distal (−) | |||||
| Immediate WB | 0.2 (0.5) | 0.4 (0.4) | 0.4 (0.5) | 0.5 (0.6) | 0.5 (0.6) |
| Partial WB | 0.1 (0.2) | 0.1 (0.7) | 0.5 (1.1) | 0.09 (0.2) | 0.09 (0.4) |
| Anterior (+)/ posterior (−) | |||||
| Immediate WB | 0.1 (0.3) | −0.07 (0.5) | 0.1 (0.4) | 0.02 (0.3) | 0.05 (0.4) |
| Partial WB | −0.03 (0.3) | 0.01 (0.3) | 0.2 (0.8) | 0.2 (0.3) | 0.04 (0.6) |
| Rotation (°) | |||||
| Anterior (+)/posterior (−) tilt | |||||
| Immediate WB | −0.07 (0.8) | −0.08 (1.3) | −0.3 (1.1) | −0.2 (1.2) | −0.09 (1.0) |
| Partial WB | 0.1 (0.4) | 1.8 (7.9) | −0.3 (1.5) | 0.07 (0.5) | 0.5 (0.9) |
| Anteversion (+)/retroversion (−) | |||||
| Immediate WB | −0.3 (0.8) | −0.3 (1.2) | −0.08 (1.0) | −0.2 (1.3) | −0.3 (1.3) |
| Partial WB | −0.3 (0.6) | −1.4 (5.9) | 0.3 (1.7) | 0.1 (0.6) | −0.4 (1.6) |
| Decreased (+)/increased (−) inclination | |||||
| Immediate WB | −0.4 (0.8) | −0.5 (0.9) | −0.8 (1.4) | −0.8 (1.7) | −1.0 (1.4) |
| Partial WB | 0.3 (1.1)b | 0.6 (2.8) | −0.4 (2.8) | 0.6 (1.7)b | 0.2 (1.1) |
Values are mean (standard deviation)
I/P immediate postoperative and partial weight-bearing groups
aExclusions because of mean error >0.3, b p < 0.05 Mann–Whitney U test
Statistics
Values of micromotion are given as mean (SD). RSA values were not normally distributed, and thus the Mann–Whitney U test was used for group comparisons. Statistical analysis was performed with Statistica 8.0 (StatSoft, Inc, Tulsa, USA). Differences were considered significant when p < 0.05. Before the original study, a power analysis was made to estimate the sample size required to detect a difference of 0.2 mm in CLS stem subsidence, and groups of 20 patients were found to be sufficient. The actual power for this part of the study was calculated to 0.52 to detect a change in proximal migration and 0.06 to detect a change in cup inclination at three months. The final protocol included two types of press-fit cups by reason of factors out of our control. Although the sample size was limited, an additional comparison of long-term stability was made between Interop and Allofit cups without considering the postoperative weight-bearing regime.
Results
Cup micromotion with the two weight-bearing regimes
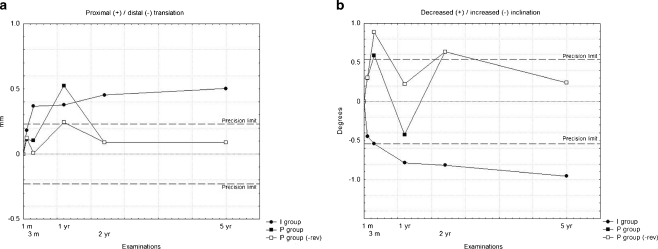
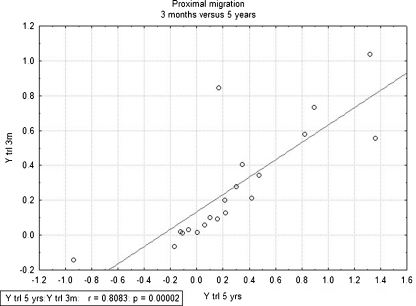
We found no differences in proximal migration at any time point between the two weight-bearing regimes (Fig 2a). There is a high correlation between proximal migration at three months and at five years (Fig. 3). The change in mean cup inclination differed statistically at one month and two years (Fig. 2b) between groups. Mean values at one month were within the precision limit. At two years, cup inclination had increased by 0.8° in the I group and decreased by 0.6° in the P group. At five years, we found no differences between groups (Table 3).
Fig. 2.
a Mean proximal/distal migration, and b mean change in inclination between immediate (I) and partial (P) weight-bearing groups. The P group is also displayed without the patient with the revised Interop cup
Fig. 3.
Correlation between proximal migration at 3 months (y axis) and proximal migration at 5 years (x axis)
The only micromotions that exceeded the precision limit were an increase in inclination and in proximal translation in the I group. Most of this change in inclination occurred during the first year and for proximal translation during the first three months. There was no statistically significant change in inclination or proximal migration over time between groups. Humps in the graphs in the inclination and proximal migration in the P group (Fig. 2a and b) at one year are to some extent explained by the patient who underwent revision because of the loose cup at 20 months. Furthermore, there was no difference between groups for the other translations or rotations measured.
Cup micromotion
We found no difference in micromotion between the Interop and the Allofit cup. At five years, compared with one week postoperatively, all press-fit cups (20 analysed) pooled together, irrespective of postoperative weight bearing regime, displayed a mean micromotion of 0.05 (0.6) mm in the medial, 0.3 (0.5) mm in the proximal and 0.1 (0.5) mm in the anterior direction. There was a mean anterior tilt of 0.2 (0.9)°, a mean retroversion of 0.3 (1.4)° and a mean increase in inclination of 0.3 (1.4)°.
Discussion
In this randomised controlled trial with five years of follow-up, we found no adverse effect of immediate postoperative weight bearing on the stability of the studied press-fit cups as assessed with RSA. The minimal micromotion of these cups had no clinical implication. RSA is the gold standard for noninvasive assessment of implant stability and has been widely used for THA implant stability assessment [7]. RSA detection of early micromotion can predict future aseptic implant loosening [11]. However, acetabular cup stability has not been studied as much as that of femoral stems. One reason for this may be the difficulty in visualising the markers in metal-backed cups and in periprosthetic pelvic bone. New software tools will offer an improvement in cup measurements [12].
Postoperative rehabilitation and weight bearing
Compliance with the prescribed partial weight bearing was measured at visits to the physiotherapist (PT). Patients in the P group loaded approximately 30 kg at one week and three months, which was more than the instructed 15 kg, but similar to that used in the only other RCT comparing weight-bearing regimes [3]. On the other hand, patients in the I group loaded the operated leg significantly more as early as one week after surgery, i.e. 39 kg, and at three months, the average load was more than twice that in the P group (70 vs 31.7 kg) [5]. The difficulty in complying to prescribed weight bearing is well documented [13, 14]. Some studies have used auditory devices placed in insoles for at-home feedback [2, 3]. Keeping this in mind, we also set up an intensive rehabilitation programme supervised by our PT for the I group to secure differences in hip loading. The P group received a short written rehabilitation programme. As a consequence, the P group put less weight on the operated leg, at least at the visit to the PT, and performed less intensive muscle training. In a recently published systematic review of the literature of postoperative weight bearing after THA with an uncemented femoral stem, moderate to strong evidence was obtained that immediate unrestricted weight bearing had no adverse effects regarding subsidence [15].
Cup stability
We are aware of only one other RCT in which the effect of weight bearing on cup stability has been studied with RSA. Thien et al. found no adverse effect of immediate weight bearing on the stability of an uncemented hydroxyapatite-coated (HA) press-fit (ABG) cup in 43 patients followed up for 1 year [3]. The auditory feedback device for partial weight bearing was set to 30 kg; the same load, in fact, as was used by our patients. Despite a considerably shorter follow-up and differences in press-fit shell coatings, micromotion was of approximately the same magnitude as in our study.
However, most RSA studies of acetabular implant stability have not taken the postoperative weight-bearing regime into consideration [16, 17]. With pooled data from our two study groups, a comparison with such studies could be of some value. In an RCT of 87 hips followed up for five years, the value of additional screws or pegs for press-fit cups (Reflection) with HA coating was assessed with RSA and was not shown to be of any benefit [16]. Translations of the press-fit cups, with six weeks of recommended postoperative partial weight bearing, were of the same magnitude as in our study, whereas our cups had slightly larger numerical rotations. Thanner et al. found no difference in cup micromotion in 64 hydroxyapatite- and tricalcium phosphate-coated Trilogy cups with eight weeks of partial weight bearing with and without supplementary screw fixation; median translations were <0.2 mm and rotations <0.2° at two years [17]. Patients in the two above-mentioned studies were similar in age to our patients, but there was no data on BMD. These findings support the idea that initial stability is good for press-fit cups, with six to eight weeks of postoperative partial weight bearing, or at least indicate that screws do not add to the stability.
Our study has some limitations. Owing to factors out of our control we were forced to change to an alternative uncemented cup for the latter part of the study. However, both Interop and Allofit press-fit cups have titanium surfaces. Interop cups in this study did not belong to the contaminated batch [6] with early failures. As both were press-fit cups with titanium surfaces it is tempting to generalise the results to different press-fit titanium cups.
Our study has certain strengths. It was designed as a randomised clinical trial, which is often recommended but not so frequently performed in THA studies. The follow-up period was considerable and longer than in most RSA studies. Selected patients were of a typical age for patients receiving uncemented THA and had strictly unilateral OAH. In an attempt to check for bone quality, quantitative BMD measurements in the affected hips were performed with DXA, and the results were found to be normal for patients’ ages.
To conclude, in this RCT with five years of follow-up, we found no adverse effects of immediate weight bearing combined with an intensive rehabilitation programme on the stability of the uncemented press-fit cups used in the study. Whether this result can be extrapolated to all uncemented cups needs to be further investigated.
Acknowledgments
This study could not have been performed without the strenuous work of our late colleague Dr. Håkan Ström. We are grateful to Monika Gelotte, RN, for skilful DXA measurements. Zimmer Inc. sponsored the study financially. They had no influence on study design, data collection or manuscript preparation.
References
- 1.Markmiller M, Weiss T, Kreuz P, Ruter A, Konrad G. Partial weightbearing is not necessary after cementless total hip arthroplasty: a two-year prospective randomized study on 100 patients. Int Orthop. 2011;35(8):1139–1143. doi: 10.1007/s00264-010-1089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boden H, Adolphson P. No adverse effects of early weight bearing after uncemented total hip arthroplasty: a randomized study of 20 patients. Acta Orthop Scand. 2004;75(1):21–29. doi: 10.1080/00016470410001708040. [DOI] [PubMed] [Google Scholar]
- 3.Thien TM, Ahnfelt L, Eriksson M, Stromberg C, Karrholm J. Immediate weight bearing after uncemented total hip arthroplasty with an anteverted stem: a prospective randomized comparison using radiostereometry. Acta Orthop. 2007;78(6):730–738. doi: 10.1080/17453670710014491. [DOI] [PubMed] [Google Scholar]
- 4.Ström H, Nilsson O, Milbrink J, Mallmin H, Larsson S. The effect of early weight bearing on migration pattern of the uncemented CLS stem in total hip arthroplasty. J Arthroplasty. 2007;22(8):1122–1129. doi: 10.1016/j.arth.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 5.Ström H, Huss K, Larsson S. Unrestricted weight bearing and intensive physiotherapy after uncemented total hip arthroplasty. Scand J Surg. 2006;95(1):55–60. doi: 10.1177/145749690609500111. [DOI] [PubMed] [Google Scholar]
- 6.Blumenfeld TJ, Bargar WL. Early aseptic loosening of a modern acetabular component secondary to a change in manufacturing. J Arthroplasty. 2006;21(5):689–695. doi: 10.1016/j.arth.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Kärrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses. Review of methodology and clinical results. Clin Orthop Relat Res. 1997;344:94–110. [PubMed] [Google Scholar]
- 8.Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Thesis, University of Lund, Lund, Sweden 1974. Reprinted. Acta Orthop Scand Suppl. 1989;232:1–51. [PubMed] [Google Scholar]
- 9.Looker AC, Orwoll ES, Johnston CC, Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP. Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res. 1997;12(11):1761–1768. doi: 10.1359/jbmr.1997.12.11.1761. [DOI] [PubMed] [Google Scholar]
- 10.Wolf O, Ström H, Milbrink J, Larsson S, Mallmin H. Differences in hip bone mineral density may explain the hip fracture pattern in osteoarthritic hips. Acta Orthop. 2009;80(3):308–313. doi: 10.3109/17453670903039528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kärrholm J, Borssen B, Lowenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br. 1994;76(6):912–917. [PubMed] [Google Scholar]
- 12.Baad-Hansen T, Kold S, Kaptein BL, Soballe K. High-precision measurements of cementless acetabular components using model-based RSA: an experimental study. Acta Orthop. 2007;78(4):463–469. doi: 10.1080/17453670710014095. [DOI] [PubMed] [Google Scholar]
- 13.Hurkmans HL, Bussmann JB, Selles RW, Benda E, Stam HJ, Verhaar JA. The difference between actual and prescribed weight bearing of total hip patients with a trochanteric osteotomy: long-term vertical force measurements inside and outside the hospital. Arch Phys Med Rehabil. 2007;88(2):200–206. doi: 10.1016/j.apmr.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Tveit M, Karrholm J. Low effectiveness of prescribed partial weight bearing. Continuous recording of vertical loads using a new pressure-sensitive insole. J Rehabil Med. 2001;33(1):42–46. doi: 10.1080/165019701300006533. [DOI] [PubMed] [Google Scholar]
- 15.Hol AM, Grinsven S, Lucas C, Susante JL, Loon CJ. Partial versus unrestricted weight bearing after an uncemented femoral stem in total hip arthroplasty: recommendation of a concise rehabilitation protocol from a systematic review of the literature. Arch Orthop Trauma Surg. 2010;130(4):547–555. doi: 10.1007/s00402-009-1017-3. [DOI] [PubMed] [Google Scholar]
- 16.Rohrl SM, Nivbrant B, Strom H, Nilsson KG. Effect of augmented cup fixation on stability, wear, and osteolysis: a 5-year follow-up of total hip arthroplasty with RSA. J Arthroplasty. 2004;19(8):962–971. doi: 10.1016/j.arth.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 17.Thanner J, Karrholm J, Herberts P, Malchau H. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation: a randomized study of 64 hips. J Arthroplasty. 2000;15(4):405–412. doi: 10.1054/arth.2000.2963. [DOI] [PubMed] [Google Scholar]