Abstract
Purpose
This retrospective review follows 31 tibial nonunions to compare union at the docking site using closed versus open strategies. In this cohort of patients, all but five were infected nonunions.
Methods
Thirteen patients initially treated with single compression were compared with 18 patients treated by open revision of the docking site. In the single compression group, an average of 6.5 cm of bone was resected and index lengthening was 2.04. In the open revision group, a mean of 9.4 cm was resected and the index lengthening was 1.73.
Results
Consolidation at the docking site occurred in all subjects in both groups. There was no statistical difference between the two groups. Conclusive evidence of superiority of one modality of treatment over the other cannot be drawn from our data.
Conclusions
The simple compression procedure requires less invasive surgery and is probably less demanding and more cost-effective in short transports.
Introduction
Wide resection of bone is frequently required during Ilizarov transport techniques [1, 2, 16, 21], leaving the surgeon facing a difficult problem. The remaining gap reduces progressively during transport, but in the interim, the repair process is shifted from a normal biological fracture response to a process in which a fibrocartilaginous tissue caps the bone, mimicking nonunion. The traditional Ilizarov approach consisted of simple compression of these tissues after bone transport was complete, and this was eventually associated with periods of distraction to stimulate osteogenesis [3, 9, 12, 22, 23]. More recently, however, some groups have expressed concern about the healing potential of this technique, proposing osteotomy of the docking ends and removal of the interposing tissue as a solution [6, 13, 19, 21]. With this technique, a biological environment more like fracture healing is restored and consolidation is considered more predictable. Clinical experience comparing closed and open docking site procedures are limited in the literature [14, 15], and definitive evidence of the superiority of one method over the other is lacking. We compared short-term outcomes of open and closed docking site procedures between two matched patient cohorts to assess the impact of the procedure on consolidation and whether this was related to open or closed techniques. In addition, we compared these groups and whether compression-distraction time was correlated with consolidation and consolidation time.
Material and methods
This retrospective study compares docking site strategies in 31 tibial nonunions. These patients were treated with bifocal and trifocal techniques by two experienced surgeons (G.L. and F.S.) at a Level I trauma centre in the period between 1999 and 2009. The patient groups were comparable regarding age and gender distribution, and the hybrid advanced technique [5, 10, 17, 20] was used in all cases. Group A consisted of 13 patients (ten male, three female) with a mean age of 46.3 years (range 21–75 years) treated between January 1999 and December 2004 (Table 1). In this group of subjects, the docking site was compressed after bone transport was complete, without removal of the interposed tissue (Fig. 1). The rate of compression during the procedure was 0.25 mm twice a week for three months. No acute procedures were used. Previous procedures in these patients included: axial external fixation (6), intramedullary nailing (4), bifocal Ilizarov (1), open reduction and internal fixation (ORIF) (2), local debridement (4), plastic surgery (1) and ileopopliteal bypass (1). One patient had temporary external fixation followed by intramedullary nailing, and one had ileopopliteal bypass followed by intramedullary nailing and then plating. Local infection was present in nine of the 13 cases. The conventional Ilizarov frame (Plustek, Assago, Italy) was used in ten cases, the Taylor Spatial Frame (Smith and Nephew, Memphis, TN, USA) was used in two and the TrueLok frame (Orthofix, McKinney, TX, USA) in the other one. The technique of bifocal transport was used 11 times (antegrade in ten, retrograde in one) and trifocal transport was used in the other two patients (antegrade in one, converging in one). The amount of bone resected was an average of 6.5 cm (range 3.0–16.0 cm). Fibular osteotomy was performed in nine patients. Group B consisted of 18 patients (15 male, three female) with a mean age of 37.7 years (range 19–79 years) treated between January 2005 and March 2009 (Table 1). In this group of subjects, the docking site procedure included a routine “refreshing” of the bone ends. This refreshing procedure consisted of resection of the bone ends at the terminus of travel, with partial disassembly of the frame to allow surgical access. The skin incision at the site was made in a standard Z-plasty technique to provide good exposure of the ends of the bones as well as allowing easy skin closure. The rate of compression during the procedure was 0.25 mm twice a week for three months. Previous procedures in these patients included: axial external fixation (14), intramedullary nailing (1), ORIF (6), local debridement and vacuum-assisted closure (VAC) therapy (14) and plastic surgery (8). Plastic surgery consisted of skin graft (5), soleus flap (2), and latissimus dorsi and serratus anterior transfer (1). Local infection was present in 14 of the 18 cases. The Taylor Spatial Frame (Smith and Nephew, Memphis, TN, USA) was used in 15 cases (Fig. 2) and the Sheffield External Fixator (Orthofix, McKinney, TX, USA) was used in the other three. The technique of bifocal transport was used seven times (antegrade in all) and trifocal transport was used in the other 11 patients (antegrade in four, retrograde in four, converging in three). Autologous bone grafting was performed in 17 of the 18 patients. In three patients a platelet gel was also added (and in two of these associated fibrin glue was used). The amount of bone resected was an average of 9.4 cm (range 4.5–17.5 cm). Fibular osteotomy was performed in 15 patients. Tendo-Achilles lengthening was performed in five patients and soft tissue transport was used four times. In both groups, bony and functional results were classified according to the Association for the Study and Application of the Method of Ilizarov (ASAMI) bony and functional scores as proposed by Paley. The final phases of docking site ossification was stimulated by gradually destabilising the fixator; with circular frame the nuts on the connecting rods were released in a sequence, one or two rods at a time at weekly intervals. The consolidation time was calculated with the empirical formula: external fixation time (days) − 10 (days before starting distraction) − compression-distraction (bone transport) time (days). When the docking site healed and the regenerate bone had formed a complete cortex on three sides the frame was removed safely.
Table 1.
Details of the 31 patients who were treated with bone transport and grading of results according to the criteria of ASAMI
| Case | Gender, age (years) | Nonunion site | Ex. fix. type | Treatment strategy | Bone transport (cm) | Compression-distraction time (weeks) | Groupa | EFT (days) | Index lengthening (months/cm) | ASAMI outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bony result | Functional result | ||||||||||
| 1 | M, 21 | Distal third | ILZ | BFCC-DO | 6.0 | 10 | A | 224 | 1.23 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 2 | M, 27 | Distal third | ILZ | BFCC-DO | 6.5 | 12 | A | 371 | 1.90 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 3 | M, 24 | Distal third | ILZ | BFCC-DO | 4.0 | 7 | A | 203 | 1.69 | Poor | Poor |
| Antegrade transport | Refracture at the DS level 318 days after frame removal due to recurrence of sepsis | Treated with second BFCC-DO (refer to case 4) | |||||||||
| 4 | M, 25 | Distal third | ILZ | BFCC-DO | 5.0 | 10 | A | 189 | 1.26 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 5 | F, 32 | Diaphyseal | ILZ | BFCC-DO | 5.0 | 12 | A | 266 | 1.77 | Good | Good |
| Antegrade transport | |||||||||||
| 6 | M, 45 | Distal third | ILZ | BFCC-DO | 6.0 | 10 | A | 476 | 2.64 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 7 | F, 58 | Diaphyseal | ILZ | BFCC-DO | 4.0 | 9 | A | 315 | 2.62 | Poor | Poor |
| Antegrade transport | DS consolidation | ||||||||||
| Regenerate nonunion | |||||||||||
| 8 | M, 69 | Diaphyseal | IlZ | TFCC-DO | 6.5 | 10 | A | 385 | 1.97 | Excellent | Good |
| Converging transport | |||||||||||
| 9 | M, 66 | Pilon | ILZ | BFCC-DO | 4.5 | 8 | A | 245 | 1.81 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 10 | M, 71 | Diaphyseal | TSF | BFCC-DO | 3.0 | 7 | A | 365 | 4.0 | Excellent | Good |
| Antegrade transport | |||||||||||
| 11 | F, 75 | Diaphyseal | TSF | BFCC-DO | 4.8 | 11 | A | 300 | 2.08 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 12 | M, 51 | Proximal | ILZ | BFCC-DO | 16.0 | 45 | A | 833 | 1.73 | Good | Good |
| Retrograde transport | |||||||||||
| 13 | M, 38 | Distal third | TLK | TFCC-DO | 13.5 | 30 | A | 770 | 1.85 | Excellent | Good |
| Antegrade transport | |||||||||||
| 14 | M, 32 | Proximal | TSF | TFCC-DO | 8.5 | 12 | B | 390 | 1.52 | Excellent | Excellent |
| Retrograde transport then lengthening (after docking site) | |||||||||||
| 15 | M, 38 | Diaphyseal | TSF | TFCC-DO | 10.3 | 11 | B | 330 | 1.06 | Excellent | Excellent |
| Converging transport | |||||||||||
| 16 | M, 38 | Proximal | TSF | TFCC-DO | 9.5 | 13 | B | 365 | 1.28 | Excellent | Good |
| Retrograde transport | |||||||||||
| 17 | M, 79 | Diaphyseal | TSF | BFCC-DO | 7 | 21 | B | 540 | 2.57 | Good | Fair |
| Antegrade transport | |||||||||||
| 18 | M, 19 | Diaphyseal | TSF | BFCC-DO | 6.8 | 13 | B | 365 | 1.76 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 19 | F, 22 | Diaphyseal | TSF | BFCC-DO | 10 | 24 | B | 600 | 2 | Excellent | Good |
| Antegrade transport | |||||||||||
| 20 | F, 50 | Diaphyseal | TSF | BFCC-DO | 5.6 | 14 | B | 570 | 3.39 | Good | Excellent |
| Antegrade transport | |||||||||||
| 21 | M, 27 | Pilon | TSF | TFCC-DO | 8 | 17 | B | 358 | 1.49 | Excellent | Good |
| Antegrade transport | |||||||||||
| 22 | M, 32 | Diaphyseal | TSF | TFCC-DO | 12 | 16 | B | 378 | 1.05 | Excellent | Excellent |
| Retrograde transport | |||||||||||
| 23 | F, 38 | Diaphyseal | TSF | TFCC-DO | 10 | 16 | B | 455 | 1.51 | Excellent | Good |
| Antegrade transport | |||||||||||
| 24 | M, 34 | Diaphyseal | TSF | TFCC-DO | 10.5 | 17 | B | 420 | 1.33 | Good | Excellent |
| Antegrade transport | |||||||||||
| 25 | M, 39 | Diaphyseal | SHF | TFCC-DO | 17.5 | 17 | B | 540 | 1.21 | Excellent | Excellent |
| Converging transport | |||||||||||
| 26 | M, 40 | Pilon | SHF | BFCC-DO | 10.5 | 43 | B | 870 | 2.77 | Good | Fair |
| Antegrade transport | |||||||||||
| 27 | M, 67 | Pilon | SHF | BFCC-DO | 4.5 | 9 | B | 260 | 1.93 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 28 | M, 22 | Diaphyseal | TSF | BFCC-DO | 7 | 12 | B | 330 | 1.6 | Good | Good |
| Antegrade transport | |||||||||||
| 29 | M, 40 | Proximal | TSF | TFCC-DO | 13 | 26 | B | 510 | 1.37 | Excellent | Good |
| Retrograde transport | |||||||||||
| 30 | M, 41 | Diaphyseal | TSF | TFCC-DO | 8 | 14 | B | 390 | 1.75 | Excellent | Excellent |
| Antegrade transport | |||||||||||
| 31 | M, 21 | Diaphyseal | TSF | TFCC-DO | 11 | 19 | B | 530 | 1.6 | Excellent | Excellent |
| Converging transport | |||||||||||
Ex. fix. external fixator, EFT external fixation time, ILZ Ilizarov, BFCC-DO bifocal combined compression-distraction osteosynthesis, TFCC-DO trifocal combined compression-distraction osteosynthesis, DS docking site, TSF Taylor Spatial Frame, TLK TrueLok, SHF Sheffield
aGroup A patients who were treated with single compression of the docking site; group B patients who were treated with open revision of the docking site
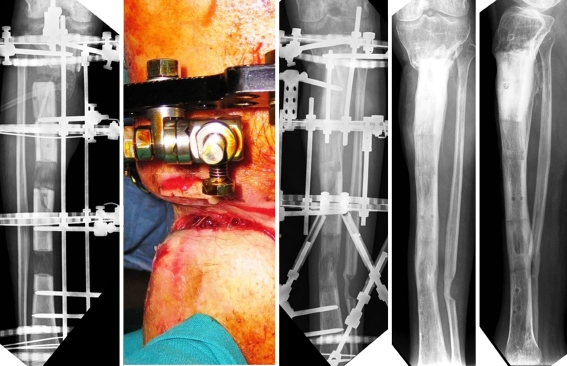
Fig. 1.
Case 13, group A: a 38-year-old man with a trifocal antegrade tibial bone transport. From left to right, images show radiograph 4 months after application of the TrueLok device demonstrating good double bone lengthening alignment, radiograph centred on the site of the un-united docking site, clinical outcome and final radiographs
Fig. 2.
Case 16, group B: trifocal retrograde tibial bone transport of a 38-year-old man with a Taylor Spatial Frame. From left to right, images show anteroposterior radiograph and clinical soft tissue invagination made at the time of docking site, radiograph after refreshing procedure and final radiographs
Statistical methods
Descriptive statistics were used for the numerical data of the two groups. Inferential statistics including unpaired Student’s t test and chi-square test were used to compare the numerical and categorical data in the two groups respectively. A P value of 0.05 was used as the level of significance. All statistical analysis was done using SPSS program version 10 (SPSS Inc., Chicago, IL, USA).
Results
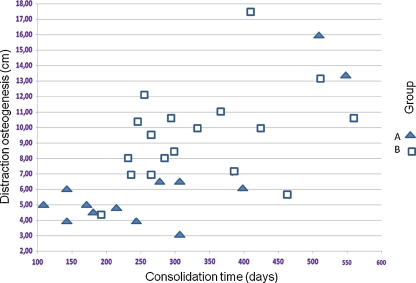
In both groups all the docking sites consolidated. Consolidation time varied from 109 to 559 days, with a mean of 302 days (Fig. 3). Group A: the mean consolidation time was 272 days (range 109–550 days). Anterior bow of the proximal regenerate occurred in one patient, and this was corrected during a second bifocal treatment for septic refracture of a previously consolidated docking site. During treatment, one patient had an ileopopliteal prosthetic bypass for septic occlusion of a previous ileopopliteal bypass. This patient also experienced necrosis of the anterior portion of the proximal regenerate and contiguous soft tissues, with exposure of the regenerate itself, which was treated by cessation of lengthening and local debridement, eventually healing, with posterior consolidation of the regenerate. The distance of bone transport was an average of 6.5 cm (range 3.0–16 cm). The mean compression-distraction time was 13.9 weeks (range 7–45 weeks). The mean external fixation time was 380.2 days (range 189–833 days). The mean lengthening index was 2.04 months/cm (range 1.2–4.0 months/cm). Bony results were excellent in nine cases, good in two and poor in two. The two results classified as poor were as follows. The first was a case of refracture at the docking site 318 days after frame removal due to recurrence of sepsis. The second poor outcome was a case of nonunion of the regenerate in an immunosuppressed patient who was a heavy smoker. The patient otherwise had consolidation of the docking site. Septic refracture at the docking site was treated with a second bifocal treatment with simple compression at the docking site, with excellent bony and functional results. Functional results overall were excellent in six patients, good in five and poor in two. The patient with a septic refracture of the docking site eventually had an excellent bony and functional result, so ultimately only one patient, in effect, had a poor bony and functional result. Group B: the mean consolidation time was 323 days (range 187–559 days). Soft tissue interposition at the docking site was seen three times before surgical docking [11, 18, 24] (Fig. 2), and a false aneurism of the peroneal artery was seen after one of the surgical docking site procedures (this was treated by embolisation). The distance of bone transport was an average of 9.4 cm (range 4.5–17.5 cm). The mean compression-distraction time was 17.4 weeks (range 9–43 weeks). The mean external fixation time was 455.6 days (range 260–870 days). The mean lengthening index was 1.73 months/cm (range 1.1–3.4 months/cm). After frame removal, regenerate bending was observed in four patients. In three the angulation was less than 5° and was left untreated. However, in one patient, bending measured 8° with a skin ulcer, and a second circular frame was applied for correction and removed after three months. One patient had a fracture of the regenerate after frame removal and was treated with plating. Final bony results were excellent in 13 of 18 cases and good in five of 18 cases. Functional results were quoted as excellent in ten patients, good in six and fair in two. Table 2 and Table 3 show the statistical analysis between the two groups; there was no statistical difference between the two groups.
Fig. 3.
Correlation between the distraction osteogenesis (cm) and consolidation time (days) in the selected groups
Table 2.
Demographics and clinical features of the study population. Comparison between the two groups using the t test
| Parameter | Group | n = 31 | Mean | SD | SEM | t test | P value* |
|---|---|---|---|---|---|---|---|
| Age | Group A | 13 | 46.3 | 19.9 | 5.5 | 1.355 | 0.186 |
| Group B | 18 | 37.7 | 15.4 | 3.6 | |||
| Bone transport distance, cm | Group A | 13 | 6.5 | 3.8 | 1.1 | −2.369 | 0.025 |
| Group B | 18 | 9.4 | 3.0 | 0.7 | |||
| Compression-distraction time, weeks | Group A | 13 | 13.9 | 11.0 | 3.1 | −1.046 | 0.304 |
| Group B | 18 | 17.4 | 7.8 | 1.8 | |||
| External fixator time, days | Group A | 13 | 380.2 | 204.3 | 56.7 | −1.217 | 0.233 |
| Group B | 18 | 455.6 | 141.4 | 33.3 | |||
| Lengthening index | Group A | 13 | 2.04 | 0.72 | 0.19 | 1.284 | 0.209 |
| Group B | 18 | 1.73 | 0.62 | 0.14 |
SD standard deviation, SEM standard error of mean
*P value < 0.05 was considered statistically significant
Table 3.
Comparison between the parametric data of the two groups
| Variable | Group A (n = 13) | Group B (n = 18) | “Z” | P* | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Gender | ||||||
| Male | 10 | 76.9 | 15 | 83.3 | −0.45 | 0.33 |
| Female | 3 | 23.1 | 3 | 16.7 | 0.45 | 0.33 |
| Nonunion site | ||||||
| Proximal third | 1 | 7.7 | 3 | 16.7 | −0.7 | 0.23 |
| Diaphyseal | 3 | 23.1 | 12 | 66.7 | −2.4 | 0.008* |
| Distal third | 8 | 61.5 | 0 | 0 | 3.9 | 0.000* |
| Pilon | 1 | 7.7 | 3 | 16.7 | −0.7 | 0.23 |
| External fixator type | ||||||
| Ilizarov | 11 | 84.6 | 0 | 0 | 4.86 | 0.000* |
| TSF | 2 | 15.4 | 15 | 83.3 | −3.8 | 0.000* |
| Others | 0 | 0 | 3 | 16.7 | −1.55 | 0.06 |
| Treatment type | ||||||
| Bifocal | 11 | 84.6 | 9 | 50.0 | 1.98 | 0.02* |
| Trifocal | 2 | 15.4 | 9 | 50.0 | −1.98 | 0.02* |
| Bony results | ||||||
| Excellent | 9 | 69.2 | 13 | 72.2 | −0.18 | 0.43 |
| Good | 2 | 15.4 | 5 | 27.8 | −0.81 | 0.21 |
| Poor | 2 | 15.4 | 0 | 0 | 1.72 | 0.043* |
| Functional results | ||||||
| Excellent | 6 | 46.2 | 10 | 55.6 | −0.52 | 0.3 |
| Good | 5 | 38.5 | 6 | 33.3 | 0.29 | 0.4 |
| Fair | 0 | 0 | 2 | 0 | −1.7 | 0.043* |
| Poor | 2 | 15.4 | 0 | 11.1 | 1.7 | 0.043* |
*P value < 0.05 was considered statistically significant
Discussion
Consolidation at the docking site occurred in all subjects in both groups, so we did not find evidence of the superiority of one modality of treatment over the other (Fig. 4). The simple compression procedure did not require an additional component of surgery (bone end resection, harvesting of bone graft) and appears less demanding and more cost-effective. Our statistical analysis supports these findings; the data showed no difference between the two groups. Historically, the Ilizarov technique treated segmental defects up to 19 cm with no mention of opening the docking site [12], and the first experiences of many small series using internal transport included closed compression of the contact area until union, with high success rates reported. One series had 100% union in 25 patients after corticotomy, stimulating blood flow, compared with conventional bone grafting [14]. This study can be compared with another where three of 28 patients had refractures that consolidated after corticotomy, compression and reapplication of the apparatus. These authors emphasised the benefit of a technique that did not require bone grafting [2]. Other studies have reported delays in the healing process after docking; in these cases, the authors adopted a protocol of opening the docking site if progression to union was not seen after three months of compression. All of the patients subsequently went on to union [15]. In a recent review of different options for treatment of the docking site, the authors reported that spontaneous union at the docking site after simple compression is actually infrequent and often due to interposed fibrous tissue. These authors did not support their opinions with data from the literature and presented only five cases, three of which evolved into nonunions, leading us to believe that this work is more an expression of the general scepticism of the orthopaedic community toward closed procedures at the docking site [8]. Our data confirm the results of the first reported studies on closed Ilizarov treatment of tibial bone loss [2, 3, 12, 14] evidenced by all patients in group A showing docking site consolidation without further procedures. We believe that some technical details contributed to the success of the subsequent compression. First, the debridement during the initial surgery was very thorough, extending to viable, bleeding bone on both sides, but avoiding any periosteal stripping of the bone ends. In addition, the bony resection was made in a plane strictly perpendicular to the long axis of the tibia, taking great care to perfectly align the bone ends during compression. It is our conviction that the presence of devitalised or poorly vascularised bone at the docking site and poor contact between bone ends secondary to inappropriate resection or malalignment during compression are important factors that can facilitate a nonunion. One argument in favour of open procedures states that by the end of travel, the bone ends are covered with a fibrocartilaginous cap which will impede healing. However, simple compression of a cartilaginous tissue can stimulate endochondral ossification, similar to the process of bone formation that occurs in growing bones (and is also present in fracture repair along with intramembranous ossification [4]. In most studies of open docking site procedures, there has been no analysis of the removed fibrocartilaginous material. To our knowledge, the only histological study of this material was in an animal model, confirming the presence of both intramembranous and endochondral ossification [7]. In one of our cases, local sepsis did not resolve, in spite of consolidation, and a refracture occurred after ten months. In this case, an open docking site procedure could had resolved the infection, and this is perhaps the main, if not only, indication for an open procedure. We also acknowledge that open procedures performed in group B resulted in consolidation in all cases. The increased external fixator time in group B (455 versus 380 days in group A) was related more to the amount of bone transport (9.9 cm in group B versus 5.9 cm in group A) than to any other factors. In addition, index lengthening appears to be superior in group A (2.1 versus 1.8 in group B), but this difference is largely due to a higher number of trifocal procedures in group B (11/18 versus 2/13 in group A) rather than a shorter consolidation time after the open docking site procedure. In addition, it is important to note that a decision on frame removal has been largely dependent on consolidation of the lengthened bone. Two other biases evident in our study are the shorter bone transport of the closed procedures of group A as well as the absence of cases of soft tissue invagination in group A. With these limitations, it is difficult to make definitive conclusions regarding the superiority of one approach over another. However, we believe that our study is the first to compare closed and open docking site procedures, and it does show that both are able to adequately achieve consolidation. Our results with closed procedures have confirmed the earliest experiences using Ilizarov bone transport techniques, questioning the need for opening and refreshing bone ends, especially in shorter transports.
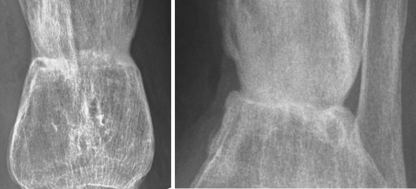
Fig. 4.
This patient is the same 38-year-old man from Fig. 1. Follow-up anteroposterior and lateral radiographs show good consolidation of the docking site
Acknowledgments
We thank Rasha Shaker, MD, for great care in providing excellent statistic revision of the paper.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
This study was approved by the Ethics Review Boards of Sant’Anna, Menaggio and Niguarda Hospitals, Italy.
References
- 1.Bumbasirević M, Tomić S, Lesić A, et al. War-related infected tibial nonunion with bone and soft-tissue loss treated with bone transport using the Ilizarov method. Arch Orthop Trauma Surg. 2010;130:739–749. doi: 10.1007/s00402-009-1014-6. [DOI] [PubMed] [Google Scholar]
- 2.Cattaneo R, Catagni MA, Johnson EE. The treatment of infected nonunions and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop Relat Res. 1992;280:143–152. [PubMed] [Google Scholar]
- 3.Dendrinos GK, Kontos S, Lyritsis E. Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am. 1995;77(6):835–846. doi: 10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Einhorn TA. The cell and molecular biology of fracture healing. Clin Orthop Relat Res. 1998;355:S7–S21. doi: 10.1097/00003086-199810001-00003. [DOI] [PubMed] [Google Scholar]
- 5.Elbatrawy Y, Fayed M. Deformity correction with an external fixator: ease of use and accuracy? Orthopedics. 2009;32:82. [PubMed] [Google Scholar]
- 6.El-Alfy B, El-Mowafi H, El-Moghazy N. Distraction osteogenesis in management of composite bone and soft tissue defects. Int Orthop. 2010;34(1):115–118. doi: 10.1007/s00264-008-0574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia FL, Picado CH, Garcia SB. Histology of the regenerate and docking site in bone transport. Arch Orthop Trauma Surg. 2009;129(4):549–558. doi: 10.1007/s00402-008-0587-9. [DOI] [PubMed] [Google Scholar]
- 8.Giotakis N, Narayan B, Nayagam S. Distraction osteogenesis and nonunion of the docking site: is there an ideal treatment option? Injury. 2007;38(Suppl 1):S100–S107. doi: 10.1016/j.injury.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Green SA. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop Relat Res. 1994;301:111–117. [PubMed] [Google Scholar]
- 10.Guerreschi F, Azzam W, Camagni M, et al. Tetrafocal bone transport of the tibia with circular external fixation: a case report. J Bone Joint Surg Am. 2010;92:190–195. doi: 10.2106/JBJS.H.01109. [DOI] [PubMed] [Google Scholar]
- 11.Hutson JJ, Jr, Dayicioglu D, Oeltjen JC, et al. The treatment of Gustilo grade IIIB tibia fractures with application of antibiotic spacer, flap, and sequential distraction osteogenesis. Ann Plast Surg. 2010;64:541–552. doi: 10.1097/SAP.0b013e3181cf9fb5. [DOI] [PubMed] [Google Scholar]
- 12.Ilizarov GA, Ledyaev VI. The replacement of long tubular bone defects by lengthening distraction osteotomy of one of the fragments. Clin Orthop Relat Res. 1992;280:7–10. [PubMed] [Google Scholar]
- 13.Lovisetti G, Sala F, Thabet AM, et al. Osteocutaneous thermal necrosis of the leg salvaged by TSF/Ilizarov reconstruction. Report of 7 patients. Int Orthop. 2011;35(1):121–126. doi: 10.1007/s00264-010-0952-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paley D, Catagni MA, Argnani F, et al. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146–165. [PubMed] [Google Scholar]
- 15.Paley D, Maar DC. Ilizarov bone transport treatment for tibial defects. J Orthop Trauma. 2000;14(2):76–85. doi: 10.1097/00005131-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Rozbruch SR, Pugsley JS, Fragomen T, et al. Repair of tibial nonunions and bone defects with the Taylor Spatial Frame. J Orthop Trauma. 2008;22:88–95. doi: 10.1097/BOT.0b013e318162ab49. [DOI] [PubMed] [Google Scholar]
- 17.Rozbruch RS, Weitzman AM, Watson JT, et al. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma. 2006;20:197–205. doi: 10.1097/00005131-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Sabharwal S, Green S, McCarthy J, et al. What’s new in limb lengthening and deformity correction. J Bone Joint Surg Am. 2011;93:213–221. doi: 10.2106/JBJS.J.01420. [DOI] [PubMed] [Google Scholar]
- 19.Sala F, Marinoni E, Castelli F, et al. Endoscopic approach for docking site bone grafting in Taylor Spatial Frame during bone transport. Injury Extra. 2009;40:175–177. doi: 10.1016/j.injury.2009.05.032. [DOI] [Google Scholar]
- 20.Sala F, Talamonti T, Agus MA. Tetrafocal leg reconstruction using combined Ilizarov/TSF technique. Musculoskelet Surg. 2011 doi: 10.1007/s12306-011-0116-9. [DOI] [PubMed] [Google Scholar]
- 21.Sala F, Thabet AM, Castelli F, et al. Bone transport for postinfectious segmental tibial bone defects with a combined Ilizarov/Taylor spatial frame technique. J Orthop Trauma. 2011;25(3):162–168. doi: 10.1097/BOT.0b013e3181e5e160. [DOI] [PubMed] [Google Scholar]
- 22.Saleh M, Rees A. Bifocal surgery for deformity and bone loss after lower-limb fractures. Comparison of bone-transport and compression-distraction methods. J Bone Joint Surg Br. 1995;77(3):429–434. [PubMed] [Google Scholar]
- 23.Song HR, Cho SH, Koo KH, et al. Tibial bone defects treated by internal bone transport using the Ilizarov method. Int Orthop. 1998;22:293–297. doi: 10.1007/s002640050263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uzel AP, Lemonne F, Casoli V. Tibial segmental bone defect reconstruction by Ilizarov type bone transport in an induced membrane. Orthop Traumatol Surg Res. 2010;96:194–198. doi: 10.1016/j.otsr.2009.10.017. [DOI] [PubMed] [Google Scholar]