Abstract
Purpose
Revision internal fixation for femoral-neck nonunion is a challenging procedure. Treatment options are osteotomy, osteosynthesis using various implants and grafting techniques (muscle pedicle, vascularised or nonvascularised fibular graft) or arthroplasty. The objective of this article is to report the outcome of revision internal fixation using an angle blade plate and autogenous fibular graft in symptomatic aseptic femoral-neck nonunion.
Methods
Twenty-two patients who had been treated previously with cannulated screws or dynamic hip screw for femoral-neck fracture and progressed to nonunion were treated with revision internal fixation using an angle blade plate and autogenous nonvascularised fibular graft. Mean patient age was 38 (range 21–52) years, with average duration between injury and revision surgery 11.2m (range 8–16 months).
Results
Other than one nonunion, we achieved union in all patients (21 patients, 91%) after an average period of 4.4 months. The functional outcome after 3.2 years as per scoring system given by Nagi et al.. showed excellent results in four, good in ten, fair in six and poor in two patients. Patients with poor results included one with nonunion and other with avascular necrosis with collapse of the femoral head. Average limb shortening was 1.5 cm, and mean femoral-neck-shaft angle was 116°. There was no instance of fibular graft fracture, slippage or implant cut-through.
Conclusion
Angle blade plate provides rigid stability and offloads any shearing force over the fibular graft when used for revision internal fixation in aseptic femoral-neck nonunion. Thus, the fibular graft only serves the purpose of osteogenesis and stimulates the surrounding host cells to promote healing at the nonunion site. We recommend the angle blade plate and autogenous fibular graft as a viable option for hip-joint salvage in revision internal fixation of aseptic femoral-neck nonunion.
Introduction
Despite advances in surgical techniques and internal fixation devices, femoral-neck fracture remains an unsolved problem. The reported incidence of nonunion after internal fixation of femoral-neck fracture is about 10–30% [1–3]. Broadly, two types of treatment can be offered following nonunion: joint salvage or prosthetic replacement (hemiarthroplasty or total hip arthroplasty). Whereas arthroplasty gives immediate results and is technically easier than hip-conservation procedures, it is not ideal for younger patients [1]. Various hip-salvage techniques, such as, muscle–pedicle bone grafting, vascularised bone grafting, valgus osteotomy, McMurray displacement osteotomy, fibular grafting and fixation with cancellous screws have been documented with variable results. Nevertheless, there is no standard guideline for choosing one over another for a particular fracture.
Originally, fibular osteosynthesis in femoral-neck nonunion was proposed by Nagi et al. from our institute. The technique involved nonvascular fibular graft with a cannulated cancellous screw [4]. Other studies report using two to three screws as supplemental fixation with a fibular graft [5–9]. Union rates with this technique in two different studies were 69% and 95% [4, 5]. We have evolved the method used for fixation with fibular bone grafting. Neglected fractures or nonunion are often associated with osteopaenia, resorption and avascular necrosis (AVN). Screw-thread purchase in osteopenic bone of the femoral head, further weakened by the previous surgery, does not appear to be substantial. In these cases, stability is largely dependent upon the fibular graft gaining a hold in the femoral head. We propose that a fixed-angle device would offer greater biomechanical stability and provide a better biological environment to fibular graft for union and graft integration. This study evaluated the outcome of revision internal fixation using an angle blade plate and autogenous nonvascular fibular graft in aseptic femoral-neck nonunion.
Methods
We retrospectively studied 22 patients with nonunion of the femoral neck who were operated upon with autologous nonvascular fibular bone graft and revision osteosynthesis with a 130° angle blade plate in all patients. Clinical and radiological data were retrieved from our trauma registry, and patients who completed at least one year of follow-up were included. There were 15 men and seven women, with a mean age at the time of surgery of 38 (range 21–52) years. The mechanism of initial injury was motor vehicle accident in 19 and a fall in three. The initial procedure was closed reduction and internal fixation with cannulated cancellous screws in 16 patients and dynamic hip screw in six. Nonunion was defined as no evidence of healing on anteroposterior and lateral radiographs at six months following surgery. All patients had pain on weightbearing. Preoperatively a bone scan was carried out in all patients to rule out AVN. C-reactive protein (CRP) and erythrocyte sedimentation rates (ESR) were obtained in all cases to rule out infection. One additional cannulated screw was inserted if space was available for the fixation. Mean time between revision surgery and injury was 11.2 (eight to16) months. In situ fixation of the fracture site was carried out in cases where the gap between fracture fragments was greater than two millimetres on radiographs. In six cases, open reduction at the fracture site using the Watson–Jones approach was carried out, and in these cases, iliac-crest-bone graft was used to pack the fracture site. The fibula was harvested from the middle third using a lateral incision. An appropriately sized tract was drilled over the guide wire under image guidance for the fibular graft. This was followed by fixation using a 130° angle blade plate. Postoperatively, patients were mobilised nonweight bearing immediately after surgery. Partial weightbearing was started after six weeks, and full weightbearing was restricted until there were signs of radiological union, following which patients were called every six months for clinical and radiological evaluation. The average duration of follow-up was 3.2 (range 1–5) years. Patients were followed up clinically for pain while weightbearing, ability to perform straight-leg raise, leg-length discrepancy and hip range of motion. Radiographically, they were assessed for evidence of union on anteroposterior and lateral views and development of avascular changes. Functional evaluation was done using the criteria used by Nagi et al. (Table 1) [4].
Table 1.
Nagi et al.’s scoring system for outcome evaluation in femoral-neck fracture fixation
| Grade | Pain | Shortening (cm) | Hip movements | Walking ability | Avascular necrosis (AVN) | Nonunion | Coxa vara (°) |
|---|---|---|---|---|---|---|---|
| Excellent | None | <1 | Full | Full | No | None | None |
| Good | None | 1–2 | Rotation/flexion restricted by 15° | Full | No or healed | None | <10 |
| Fair | Intermittent | 2–3 | Rotation <50%; flexion 90°y | 1 km without aid | AVN; no segmental collapse | None | 10–20 |
| Poor | Constant | >3 | Marked reduction | None without aid | AVN with collapse | Present | >20 |
Results
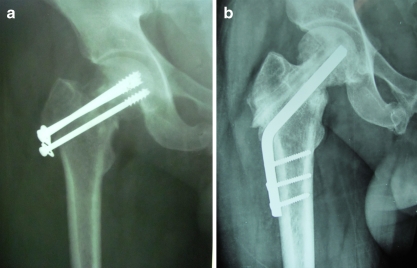
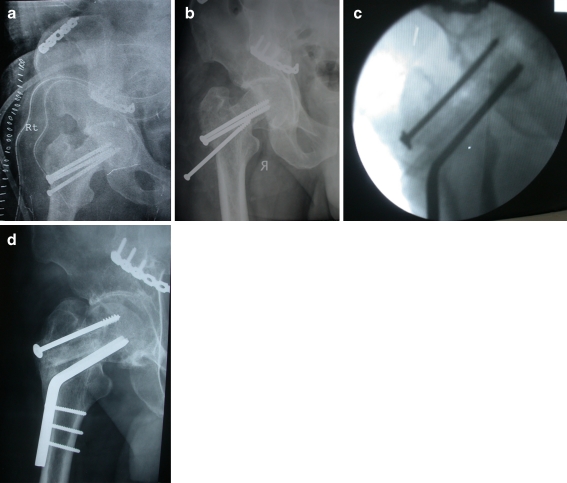
Radiographically, union was seen in 21 patients (Figs. 1 and 2), none of whom had pain on weightbearing or straight-leg raising. Mean time between revision surgery and union was 4.4 (3.6–6) months.
Fig. 1.
a Radiograph showing nonunion 8 months after femoral-neck fracture fixation with cannulated screws in a 35-year-old man; b 4.2 months after revision osteosynthesis with fibular graft and angle blade plate, radiograph shows complete union
Fig 2.
a Cannulated screw fixation in a femoral-neck fracture; b nonunion with screw backout was evident from X-ray after 9 months; c screws were removed, revision surgery with fibular autograft and angle blade plate was performed, implant and graft positions were checked under image intensifier; d 4.5 years after refixation with angle blade plate and fibular graft, the fracture has completely united with graft incorporation
Five patients had evidence of AVN on preoperative bone scan. Follow-up radiographs in all patients demonstrated union. Only one patient progressed to femoral-head collapse. Evidence of revascularisation was seen in the four other cases with maintenance of femoral-head sphericity on follow-up radiographs. Mean neck-shaft angle at follow-up was 116° (124–111° ). Mean leg-length difference was 1.5 cm. There was no instance of fibular graft fracture or slippage or implant cut-through. After a mean of 3.2 years, using the criteria of Nagi et al. [4], excellent results were seen in four, good in ten, fair in six and poor in two patients. Patients with poor results included one with nonunion and other with AVN with collapse of the femoral head. Both patients required total hip replacement (Table 2).
Table 2.
Demographic profiles, surgical details, complications and outcome of patients treated with autogenous nonvascularised fibular graft and angle blade plate
| Serial no | Age (years) | Interval between injury and revision (months) | Original surgery | Avascular necrosis (preoperative) | Nagi score | Comments/ complications | Time to union (months) | Limb shortening (cm) |
|---|---|---|---|---|---|---|---|---|
| 1 | 22/M | 11.4 | Cannulated screw fixation | Excellent | 5.2 | 1.5 | ||
| 2 | 43/M | 12 | Cannulated screw fixation | Yes | Good | No evidence of AVN | 3.6 | 1.8 |
| 3 | 25/F | 8.5 | Dynamic hip screw | Good | 4 | 1.6 | ||
| 4 | 30/M | 13 | Dynamic hip screw | Fair | 3.6 | 2.2 | ||
| 5 | 21/M | 12.5 | Cannulated screw fixation | Yes | Excellent | No evidence of AVN | 4.1 | 1.0 |
| 6 | 38/M | 8.5 | Dynamic hip screw | Yes | Poor | AVN with head collapse | 3.8 | 2.0 |
| 7 | 35/M | 8 | Cannulated screws fixation | Good | 4.2 | 0.8 | ||
| 8 | 29/F | 9 | Cannulated screw fixation | Good | 5.4 | 1.4 | ||
| 9 | 49/M | 14.8 | Dynamic hip screw | Excellent | 6 | 1.8 | ||
| 10 | 42/F | 12 | Cannulated screw fixation | Fair | 4.9 | 2.0 | ||
| 11 | 26/F | 15 | Cannulated screw fixation | Yes | Fair | No evidence of AVN | 5.3 | 1.2 |
| 12 | 29/M | 8.5 | Cannulated screw fixation | Good | 5 | 1.6 | ||
| 13 | 35/M | 9 | Cannulated screw fixation | Good | 4.4 | 2.2 | ||
| 14 | 28/M | 10.6 | Cannulated screw fixation | Good | 3.8 | 1.4 | ||
| 15 | 52/M | 15.4 | Dynamic hip screw | Fair | 4.2 | 1.6 | ||
| 16 | 27/M | 9 | Cannulated screw fixation | Excellent | 5.2 | 1.0 | ||
| 17 | 45/M | 8 | Cannulated screw fixation | Yes | Good | No evidence of AVN | 4.8 | 1.2 |
| 18 | 38/M | 12 | Dynamic hip screw | Good | 4 | 1.4 | ||
| 19 | 29/F | 9 | Cannulated screw fixation | Fair | 3.8 | 1.4 | ||
| 20 | 38/F | 15.5 | Cannulated screw fixation | Fair | 4 | 1.2 | ||
| 21 | 47/F | 16 | Cannulated screw fixation | Good | 4 | 2.0 | ||
| 22 | 50/M | 8 | Cannulated screw fixation | Poor | Nonunion | - | 2.5 |
AVN avascular necrosis
Following fibular graft harvest, transient loss of extensor hallucis longus power was seen in three patients, all of whom had recovered at follow-up. No sensory deficit was seen in any patient.
Discussion
The major causes of nonunion and AVN after femoral-neck fracture can be attributed to a combination of unfavourable biomechanical and vascular conditions caused by the fracture itself, poor reduction and inadequate internal fixation. Varus malreduction is the main risk factor for nonunion [5, 10, 11]. It is therefore advocated to proceed with open reduction if there is difficulty in obtaining closed reduction. Cannulated cancellous screws are the most commonly used hardware for internal fixation of these fractures and also during revision surgery using fibular grafting. Osteotomy has been used with better outcomes in femoral-neck nonunions (AVN in 6–17% and nonunion rates 0–15%), but functional results are mediocre because of the frequency of a persistent painful limp due to mechanical changes at the femoral neck [12–16]. Limb shortening and decreased range of motion are common after osteotomy, probably because of increased pressures on the femoral head, leading to degenerative disease or osteonecrosis. Again, there are potential risks for nonunion at the osteotomy site, although this has not been commonly reported in the literature. Osteotomy converts the vertical fracture line to the horizontal compressive force and thus creates better hip biomechanics for fracture healing. However, in view of the described morbidities, it may not be justified in cases where nonunion is not associated with significant varus deformity at the fracture site [4, 5]. The primary issue in these situations is biology at the fracture site and stability of internal fixation. This is addressed by fibular grafting and stable internal fixation. This avoids addition of another procedure, with its added complications such as nonunion at the osteotomy site and increased risk of AVN [15]. It has been suggested that valgus osteotomy should be preferred for cases in which shortening is significant (>1.5 cm), as this helps improve limb length [15, 16]. In our experience, most of these patients are those with a significant gap at the fracture site and varus collapse. These cases benefit most from open reduction and valgus osteotomy with or without fibular grafting. Higher Pauwels-type fractures have a greater chance of failure and varus collapse [12, 17]. It has been suggested that such fracture nonunions are best treated by valgus osteotomy to improve biomechanics at the fracture site [12].
An important concern in revision surgery is the quality of bone that is available for secure fixation. The femoral head in a nonunion femoral-neck fracture is compromised by osteoporosis secondary to disuse and bone deficiency inside the femoral head due to previous hardware. This greatly impairs the strength of fixation in the femoral head. We often found it difficult to obtain good purchase of the cannulated cancellous screws while fixing femoral-neck nonunions. Poor fixation delays mobilisation, and the patient must be nonweightbearing for a longer period. These screws depend upon threads fixation in the bone of femoral head. On the contrary, the angle blade plate, owing to its rectangular shape, better resists torsional and shearing forces. With a larger volume of bone coming in contact with the blade surfaces, angle blade plates are ideal implants where bone quality is compromised. Angle blade plates have been used for proximal femoral osteotomies in paediatric and adult patients, and for fixation of some unstable subtrochanteric or pertrochanteric fractures. There is no report regarding this implant in revision surgery for femoral-neck fractures without valgus osteotomy.
Nagi et al. [4] used a single cancellous screw along with the fibular graft for supplemental fixation [4]. They found this implant unstable and relied on postoperative hip spica. Various other authors used two to three cancellous screws for supplemental fixation. They all relied on the fibular graft for primary stable fixation and believed that the cancellous screws provided additional stability. This arrangement exerts great shear forces on the graft, which in our opinion would hamper the biological environment for graft uptake. The angle blade plate offloads the graft of the shearing forces, which now only serve the function of osteogenesis. Considerable forces acting on the grafts can be determined from the instances of fibular graft fractures or slippage while using screws. Fracture of the fibular graft was seen in four patients in the series by Nagi et al. [4]. There was no instance of fibular fracture in any of our patients. Though Nagi et al.. achieved 95% union rate in their study, similar results were not replicated in other studies, even when more than one screw was used for stability [5]. Elgafy et al. achieved fusion rates of 69.2% by using screws and autogenous fibular graft [5]. We agree that angle blade placement in the femur and neck is technically demanding, and utmost care must be taken to place it in its optimal position, preferably in the inferomedial quadrant of the femoral head, to avoid implant cut-through. A dynamic hip screw cannot take the place of an angle blade plate, as it enhances the risk of AVN due to reaming and also does not provide rotational stability. As an indirect effect of this, force may be exerted over the fibular graft. Angle blade plate, with or without supplementary screws, provides rigid stability to the femoral-neck nonunion and allows the fibula to perform the sole purpose of osteogenesis. By stimulating the native host cells, fibular autograft promotes union at the fracture site at a faster rate. This is evident in our study, as mean fracture union duration was only 4.4 months, which is less than most previous studies [5, 6].
Although the vascularised fibula appears to be a more biological graft, it is technically more difficult and needs greater expertise, which may not be available in many centres. Union rates >90% can be seen with free vascularised fibular grafting [6–8]. Jun et al. achieved union in 92.3% (24 of 26) cases in 5.3 months [6]. The success rate in our series was 91%, which is almost equivalent to that reported using vascularised fibular graft. The advantage of using vascularised graft in union rates and time to union is not apparent in the literature.
The presence of avascular changes on preoperative investigations is not a contraindication for revision internal fixation, as a majority of these changes have been shown to resolve in favour of revascularisation as union occurs. Of four patients with avascular changes in our series, three had healed at follow-up. Follow-up radiographs showed that the fibular graft begins the union process at the graft periphery, and the centre is the last to integrate. This is probably due to the more vascular environment available in the ends of the graft compared with the fracture site, which is relatively avascular.
Limitations of the study were the retrospective design, small number patients and absence of a control group. However, it seems that the angle blade plate with or without a supplementary cannulated screw provides rigid stability in femoral-neck nonunion, and the fibular graft augments the biological healing process at a faster pace with less chance of failure. This technique offers more reliable fixation with early mobilisation.
Acknowledgement
None.
Source of support/funding
None.
References
- 1.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68:236–242. doi: 10.1097/TA.0b013e3181c428ce. [DOI] [PubMed] [Google Scholar]
- 3.Mathews V, Cabanela ME. Femoral neck nonunion treatment. Clin Orthop Relat Res. 2004;419:57–64. doi: 10.1097/00003086-200402000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Nagi ON, Dhillon MS, Goni VG. Open reduction, internal fixation and fibular autografting for neglected fracture of the femoral neck. J Bone Joint Surg Br. 1998;80:798–804. doi: 10.1302/0301-620X.80B5.8703. [DOI] [PubMed] [Google Scholar]
- 5.Elgafy H, Ebraheim NA, Bach HG. Revision internal fixation and nonvascular fibular graft for femoral neck nonunion. J Trauma. 2011;70:169–173. doi: 10.1097/TA.0b013e3181e5108b. [DOI] [PubMed] [Google Scholar]
- 6.Jun X, Chang-Qing Z, Kai-Gang Z, Hong-Shuai L, Jia-Gen S. Modified free vascularized fibular grafting for the treatment of femoral neck nonunion. J Orthop Trauma. 2010;24:230–235. doi: 10.1097/BOT.0b013e3181be3ec3. [DOI] [PubMed] [Google Scholar]
- 7.Azam MQ, Iraqi A, Sherwani M, Sabir AB, Abbas M, Asif N. Free fibular strut graft in neglected femoral neck fractures in adult. Indian J Orthop. 2009;43(1):62–66. doi: 10.4103/0019-5413.45325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angelini M, McKee MD, Waddell JP, Haidukewych G, Schemitsch EH. Salvage of failed hip fracture fixation. J Orthop Trauma. 2009;23(6):471–478. doi: 10.1097/BOT.0b013e3181acfc8c. [DOI] [PubMed] [Google Scholar]
- 9.Haidukewych GJ. Salvage of failed treatment of femoral neck fractures. Instr Course Lect. 2009;58:83–90. [PubMed] [Google Scholar]
- 10.Jackson M, Learmonth ID. The treatment of nonunion after intracapsular fracture of the proximal femur. Clin Orthop Relat Res. 2002;399:119–128. doi: 10.1097/00003086-200206000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Chua D, Jaglal SB, Schatzker J. Predictors of early failure of fixation in the treatment of displaced subcapital hip fractures. J Orthop Trauma. 1998;12:230–234. doi: 10.1097/00005131-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Raaymakers EL, Marti RK. Nonunion of the femoral neck: possibilities and limitations of the various treatment modalities. Indian J Orthop. 2008;42(1):13–21. doi: 10.4103/0019-5413.38575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ballmer FT, Ballmer PM, Baumgaertel F, Ganz R, Mast JW. Pauwels osteotomy for nonunions of the femoral neck. Orthop Clin North Am. 1990;21:759–767. [PubMed] [Google Scholar]
- 14.Said GZ, Farouk O, Said HG. Valgus intertrochanteric osteotomy with single-angled 130° plate fixation for fractures and non-unions of the femoral neck. Int Orthop. 2010;34(8):1291–1295. doi: 10.1007/s00264-009-0885-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu CC, Shih CH, Chen WJ, Tai CL. Treatment of femoral neck nonunions with a sliding compression screw: Comparison with and without subtrochanteric valgus osteotomy. J Trauma. 1999;46:312–317. doi: 10.1097/00005373-199902000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Min BW, Bae KC, Kang CH, Song KS, Kim SY, Won YY. Valgus intertrochanteric osteotomy for non-union of femoral neck fracture. Injury. 2006;37:786–790. doi: 10.1016/j.injury.2006.02.045. [DOI] [PubMed] [Google Scholar]
- 17.Liporace F, Gaines R, Collinge C, Haidukewych GJ. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J Bone Joint Surg Am. 2008;90(8):1654–1659. doi: 10.2106/JBJS.G.01353. [DOI] [PubMed] [Google Scholar]