Abstract
The side-effects of many drugs manifest in the oral mucosa. The anti-malarial agent chloroquine diphosphate, which is also used to treat immunological, dermatological, and rheumatological disorders, usually causes pigmentary changes in the oral mucosa. This report presents a case of palate pigmentation related to the prolonged use of chloroquine diphosphate caused by the deposition of drug metabolites in the mucosa. Healthcare professionals must be aware of these drugs and their adverse effects in order to make the correct diagnosis, decide on the optimal treatment for the condition, or refer the patient to an appropriate specialist.
Keywords: Pigmentary changes, Oral mucosa, Anti-malarials
History
A 64-year-old woman with dark skin tone was referred to us for evaluation of a dark stain on the roof of mouth that had appeared around 3 months before presentation without any painful symptoms. The patient had arterial hypertension and rheumatoid arthritis among other systemic diseases, and she was using a pacemaker. She reported the use of the following medicines: prednisone, methotrexate, meloxicam, aspirin (100 mg) and chloroquine phosphate (200 mg/day, started approximately 15 years prior).
Clinical Examination
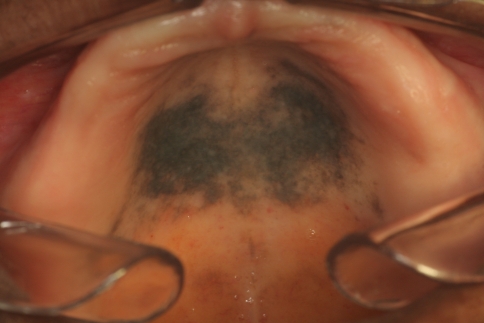
On intraoral examination, a 4 cm darkly pigmented diffuse lesion with irregular borders was seen on the hard palate (Fig. 1). Other small dark areas and pigmented spots were seen on the dorsal tongue and left lower gingival border. Four years before presentation, the patient’s upper removable total prosthesis had been replaced; at that time, no color changes were noted in the palatal mucosa. On extraoral examination, pigmentation was not seen in the nails or in the ocular conjunctiva.
Fig. 1.
Intraoral examination revealed a large 4 cm area of black to gray pigmentation with irregular borders involving the hard palate
Diagnosis
On the basis of the clinical findings, the following differential diagnoses were raised: medical hyperpigmentation, Addison’s disease, vitamin B12 deficiency, and melanoma. The results of extensive blood testing excluded the possibility of Addison’s disease and vitamin B12 deficiency. Given the history of long-term chloroquine use, the top clinical working diagnosis was drug-induced oral pigmentation caused by chloroquine phosphate. To confirm this, and rule out the possibility of melanoma, a surgical evaluation was requested and the patient then underwent an incisional biopsy (Fig. 2). Histologic examination revealed a subepithelial deposition of tiny spherical brown-black structures scattered between collagen fibers and within macrophages. The overlying epithelium was unremarkable and there was no evidence of melanoma. These findings confirmed the diagnosis of drug-induced oral pigmentation caused by chloroquine phosphate (Fig. 3). When asked about changes in vision, the patient mentioned experiencing blurred vision and was referred for ophthalmologic evaluation, which included monocular visual-field testing, specular microscopy, retinography, computed angiography, computed tomography (CT), and optical coherence tomography (OCT). This work-up revealed that the patient had 90% irreversible vision loss.
Fig. 2.
Gross photograph of the tissue removed from the hard palate by incisional biopsy for histopathologic analysis showing marked discoloration
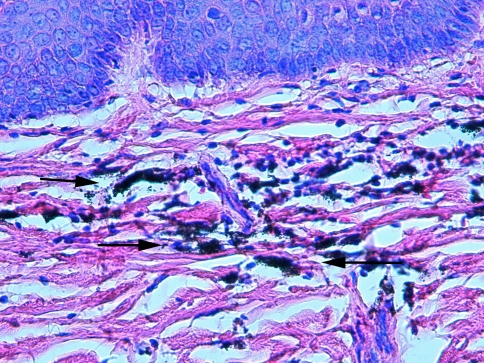
Fig. 3.
The basophilic granules are chloroquine metabolites deposited in the mucosal tissue of the hard palate (arrows) (hematoxylin-eosin, ×400)
Discussion
The oral mucosa is a common site at which the adverse effects of drugs manifest. The most common clinical changes due to adverse drug reactions include inflammatory reactions in the mucosa, non-specific ulcers, gingival hyperplasia, xerostomia, and pigmentation [1]. Anti-malarial agents, such as chloroquine diphosphate and hydroxychloroquine sulfate, are administered for the treatment of several dermatologic and rheumatologic disorders, and they are known to cause hyperpigmentation of the oral mucosa [1–4]. Systemic administration of these drugs for a prolonged period is responsible for the appearance of multifocal hyperpigmentation, which is reversible once the medication is discontinued. Oral pigmentation secondary to drug therapy can be attributed to the stimulation of melanin production by melanocytes and/or the deposition of metabolic products of the drugs in the tissues [3, 5].
Pathologic changes in the oral mucosa can be associated with several drugs [1–5]. These adverse reactions depend on the drug and its pharmacodynamics and pharmacokinetics, as well as any individual variability in drug metabolism [6]. Pigmentary changes in the oral mucosa are caused by many medications, including anti-malarial drugs (chloroquine phosphate, hydroxychloroquine, quinidine, and quinacrine), tranquilizers (chlorpromazine), chemotherapeutics (doxorubicin, busulfan, and cyclophosphamide), anti-retroviral agents (zidovudine, AZT, and ketoconazole), antibiotics (minocycline), and laxatives (phenolphthalein) [1]. In the current case, oral mucosal hyperpigmentation was caused by chloroquine phosphate, which the patient had been using for rheumatoid arthritis treatment for approximately 15 years.
Chloroquine phosphate and hydroxychloroquine sulfate have been used since the Second World War as anti-malarial agents. Furthermore, because of their immunosuppressive and anti-inflammatory actions, they came into widespread use for treating systemic and discoid lupus erythematosus, rheumatoid arthritis, cutaneous porphyria, solar hives, and other dermatological conditions [3, 5]. Although these drugs yield good therapeutic results, there are significant concerns regarding the ocular toxicity of these drugs, particularly chloroquine. Chronic use of these drugs can result in retinal degeneration [2, 7, 8] that can persist even after the medication has been discontinued [5, 9]. The two most important irreversible ocular side effects of chloroquine are retinotoxicity and corneal deposits [8, 9]. The patient in the current case had 90% loss of vision due to the deposition of chloroquine in the pigmented retinal tissues. The daily dose of the drug seems to determine the development of ocular disease, and it should be established depending on the patient’s weight; in the case of chloroquine, it should not exceed 4 mg kg−1 day−1 [5].
Unlike the ocular effects, the pigmentary changes caused by chloroquine are reversible once the dose is reduced or the drug is discontinued. These changes can appear in the upper lip, the oral mucosa, and the hard palate, the latter being the site at which the prevalence is highest [9]. The hyperpigmented areas can be of several different sizes, and are normally diffuse, macular lesions with well-defined edges. In terms of color variations, they can be brown, black, or gray [3]. The characteristics of the lesion found in our patient are consistent with those described above. Although the pigmentary lesions caused by drugs can sometimes be esthetically unpleasant, they do not require treatment, since they usually disappear once the drug is discontinued [1].
A dental surgeon must be aware of the many adverse reactions and side effects from medications that can compromise the oral tissues in order to identify them and treat them, as well as prevent them whenever possible [6]. Important factors to consider in the differential diagnosis include the site and color of the lesion, changes in pigmentation over time, family medical history, and medication use including duration [3]. Patients who develop intraoral signs and symptoms attributable to adverse drug reactions should seek assistance from healthcare professionals, who must be able to recognize such signs and symptoms, be aware of the commonly involved medicines, and establish a clear relationship between the drug and the oral side effects [3]. Even though the patient in this case sought assistance relatively late, her condition was correctly diagnosed because of good anamnesis. She was quickly referred for specialized evaluation, thereby preventing worse damage, which would have been total vision loss. In summary, pigmentary alterations in the oral mucosa caused by the use of medications, particularly anti-malarial drugs, should be included as part of the clinical differential diagnosis of hyperpigmentation of the oral mucosa.
References
- 1.Porter SR, Scully C. Adverse drug reactions in the mouth. Clin Dermatol. 2000;18:525–532. doi: 10.1016/S0738-081X(00)00143-7. [DOI] [PubMed] [Google Scholar]
- 2.Arana LA, Arana J, Hasimoto AR, et al. Tomografia de coerência óptica na avaliação da camada de fibras nervosas peripapilar nos usuários de cloroquina. Arq Bras Oftalmol. 2010;73:28–32. doi: 10.1590/S0004-27492010000100005. [DOI] [PubMed] [Google Scholar]
- 3.Kleinegger CL, Hammond HL, Finkelstein MW. Oral mucosal hyperpigmentation secondary to antimalarial drug therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:189–194. doi: 10.1067/moe.2000.106340. [DOI] [PubMed] [Google Scholar]
- 4.Martin TJM, Sharp I. Oral mucosal pigmentation secondary to treatment with mepacrine, with sparing of the denture bearing área. Br J Oral Maxillofac Surg. 2004;42:351–353. doi: 10.1016/j.bjoms.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 5.Gouveia EB, Morales MAS, Gouveia GB, et al. Toxicidade ocular por derivados da 4-aminoquinolona. Arq Bras Oftalmol. 2007;70:1046–1051. doi: 10.1590/S0004-27492007000600033. [DOI] [PubMed] [Google Scholar]
- 6.Seymour RA, Rudralingham M. Oral and dental adverse drug reactions. Periodontology. 2000;2008(46):9–26. doi: 10.1111/j.1600-0757.2008.00226.x. [DOI] [PubMed] [Google Scholar]
- 7.Lacava AC. Complicações oculares da terapêutica com a cloroquina e derivados. Arq Bras Oftalmol. 2010;73:384–389. doi: 10.1590/S0004-27492010000400019. [DOI] [PubMed] [Google Scholar]
- 8.Rodrigues LD, Shinjo SK, Oyamada MK, et al. Métodos diagnósticos para retinopatia induzida pelo difosfato de cloroquina nos portadores de lúpus eritematoso sistêmico. Arq Bras Oftalmol. 2009;72:313–320. doi: 10.1590/S0004-27492009000300007. [DOI] [PubMed] [Google Scholar]
- 9.Lerman MA, Karimbux N, Guze KA, et al. Pigmentation of the hard palate. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:8–12. doi: 10.1016/j.tripleo.2008.07.022. [DOI] [PubMed] [Google Scholar]