Abstract
Repeated transmission of animal influenza viruses to humans has prompted investigation of the viral, host, and environmental factors responsible for transmission via aerosols or respiratory droplets. How do we determine – out of thousands of influenza virus isolates collected in animal surveillance studies each year – which viruses have the potential to become “airborne”, and hence pose a pandemic threat? Here, using knowledge from pandemic, zoonotic and epidemic viruses, we postulate that the minimal requirements for efficient transmission of an animal influenza virus between humans are: efficient virus attachment to (upper) respiratory tissues, replication to high titers in these tissues, and release and aerosolization of single virus particles. Investigating “airborne” transmission of influenza viruses is key to understand – and predict – influenza pandemics.
Introduction
The virus or virus subtype that will cause the next influenza pandemic is a highly debated topic in the field. Some believe that only influenza virus subtypes H1, H2, and H3 can cause pandemics in humans, and therefore – beyond isolated cases of zoonotic infections – we should not worry about virus subtypes such as H5N1, H7N7 or H9N2 for human health. Many believe that swine viruses, rather than avian viruses, are more likely to cause the next pandemic. However, beyond the fact that there will be future pandemics, there is little known in terms of the viral origin, subtype, and virulence of the next pandemic. One other assumption can be made: the virus will be transmissible via small particle aerosols (typically <5μm) or large respiratory droplets (typically >5μm), shortened hereafter as airborne transmissible.
Influenza A viruses are constantly undergoing genetic and phenotypic changes during their circulation in avian and mammalian species. Our knowledge of viral traits necessary for host switching and virulence has increased significantly over the last decade. However, what exactly determines airborne transmission of influenza viruses in humans has remained largely unknown. Only when we fully understand the viral (genetic and phenotypic), host, and environmental factors that drive airborne transmission can we start to make predictions about which influenza viruses may cause future influenza pandemics.
Past pandemics
Four major pandemics have been recognized for which viral genome sequence data is available. While it was initially proposed that the 1918 H1N1 Spanish influenza pandemic was caused by a wholly avian virus that adapted to humans [1], recent evidence suggests that some of its genes were derived from mammalian viruses circulating as early as 1911 [2*]. The 1957 H2N2 Asian influenza pandemic resulted from the reassortment of avian HA, NA, and PB1 virus genes with the then circulating seasonal human H1N1 influenza virus [3]. The H3N2 Hong Kong influenza pandemic of 1968 was also a product of reassortment between avian and human virus genes; HA and PB1 genes of the H2N2 virus were replaced by those of an avian H3 virus [3]. In 2009, an H1N1 influenza virus of swine origin caused the first pandemic of the 21st century [4]. The gene constellation of this virus showed clear evidence of multiple reassortment events that had presumably occurred in pigs over a period of years [5] (Figure 1). The role of swine as a mixing vessel for the generation of reassortant influenza A viruses with pandemic potential is generally accepted, yet still underestimated (reviewed in [6]). However, it should be noted that reassortment can conceivably take place in avian or human hosts; for pandemics prior to 2009, there is no evidence that reassortment events occurred in pigs. Regardless of the identity of the mixing vessel it is important to emphasize that most, if not all, recent influenza pandemics were caused by reassortant viruses. The expansion in surveillance efforts in pigs in response to the 2009 pandemic will most likely reveal many more reassortant viruses that may or may not have the potential to infect and spread in humans. But how, out of thousands of animal influenza viruses from surveillance studies, can we select the ones we should prepare for as potential causes of new pandemics?
Figure 1. Reassortment and adaptation events of pandemic influenza A viruses.
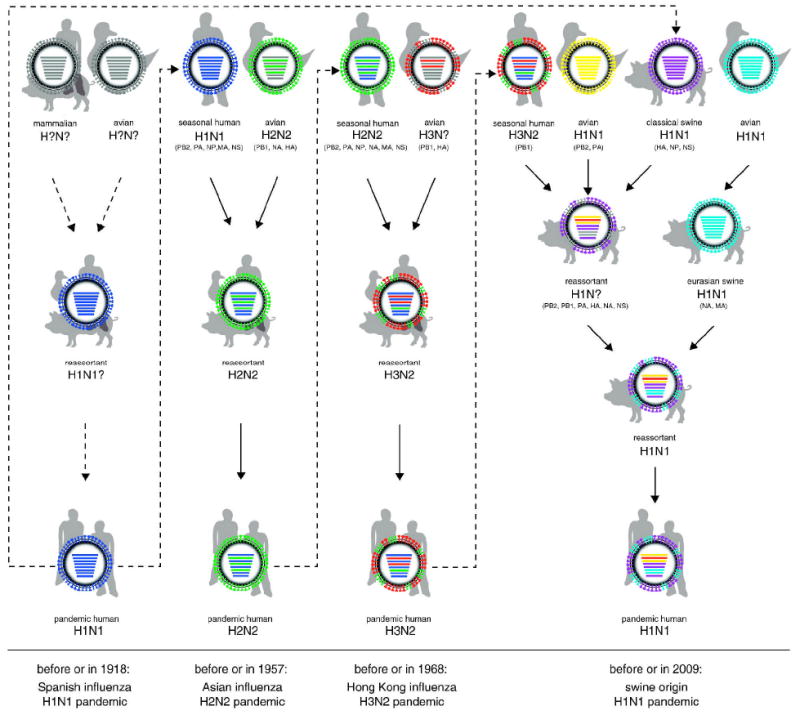
For the 1918 H1N1 “Spanish influenza” pandemic, evidence for two mutually exclusive scenarios has been presented: the gradual adaptation of avian genes to the human host and a reassortment event between avian and mammalian viruses. After 1918, the H1N1 virus caused seasonal epidemics until 1957, when the H2N2 influenza A virus emerged upon reassortment between the seasonal H1N1 and an avian H2N2 virus, introducing the avian HA, NA, and PB1 genes. This H2N2 virus circulated in humans until 1968, when reassortment of the H2N2 with an avian H3 virus resulted in exchange of the H3 HA and PB1 genes to yield a new pandemic virus of subtype H3N2. The 2009 H1N1 pandemic contained the NA and M genes of the Eurasian swine lineage, and the other genes of a “triple reassortant” swine influenza virus that earlier acquired its genes upon reassortment between human, avian, and (classical) swine viruses. Grey colour in virus particles indicates uncertainty of viral gene segment origin or lack of data. Dotted arrows indicate uncertain scenarios and solid arrows indicate events that are supported by scientific evidence. Dashed arrows represent pandemic viruses circulating in following influenza seasons.
Viral determinants of transmission
Retrospective analysis of pandemic H1 (1918), H2 and H3 viruses has revealed that only one to two mutations in the HA receptor binding site are required to confer binding preference for virus receptors on cells of the upper respiratory tract (URT) of humans, α2,6-linked sialic acids (SAs) [7]. Partially borrowing from this knowledge, several mutations in the HA protein, including Q222L, G224S, E186D, K189R, S223N and N182K (H5 numbering), have been shown to change and/or increase receptor binding of avian H9N2 and H5N1 viruses to human URT tissues [8-12] with changes like Q226L (H3 numbering) improving replication and transmission of H9 viruses [13]. However, to date, none of the “designer” H5N1 viruses carrying these mutations have resulted in airborne transmission [11,14]. Efficient H5 transmission may thus require more subtle differences in receptor preference than simple α2,3 (the receptor for avian viruses) versus α2,6 SA linkage specificity.
Previous research has also pointed to key changes in the polymerase proteins that increase virus replication efficiency at 33°C, the accepted temperature for efficient replication in the mammalian URT [15*-16]. These changes at positions 627, 701 and 591 of PB2 have also been shown to support transmission of multiple subtypes in mammalian models [17-19*]. A decrease in association of the PB2 and NP proteins in mammalian cells is thought to be the mechanism behind the increase in replication efficiency [20].
PA and NP genes have also been associated with viral host restriction but the key amino acids have yet to be identified. Even fewer experiments have looked at the roles of NA, M and NS proteins in determining host range and transmission. It is likely that virus tropism, efficiency in replication, amount of virus shed, and the duration of shedding are important factors for transmission efficiency. A longer duration of virus shedding at high titer may be hypothesized to increase the chance for the virus to reach susceptible host(s) and therefore increase transmission events [21**].
Airborne transmission; size does matter
Human-to-human transmission of influenza viruses can occur through contact, direct or indirect, and/or respiratory droplets (large droplets and aerosols). Opinions differ on the importance of each mode of transmission (reviewed in [22-23]). The role of each has been well studied in mammalian models, focusing on the ferret and guinea pig (reviewed in [24*] and Table 1). Efficient aerosolization of viral particles is however crucial for a virus with transmission efficiency and pandemic potential. There is no exact particle size cut-off at which transmission changes from exclusively large droplet to aerosol. However it is generally accepted that for infectious particles with a diameter of 5μm or less, transmission occurs through aerosols. Large aerosol droplets do not remain suspended in air and typically travel < 1m before settling on the mucosa of close contacts or environmental surfaces. In contrast, smaller particles, < 5μm, have a slow settling velocity and can thus travel further than large droplets [25]. Humans exhale droplets of widely varying size and quantity [26] and the generation of aerosol particles by coughing or sneezing has been well documented, with the majority of particles expelled during breathing and sneezing measured at < 1μm [27-28]. Evidence to support the role of aerosols in influenza transmission include the prolonged persistence of infectivity in aerosolized influenza at low humidity [29-30], transmission to volunteers by aerosols reproducing the disease at doses much less than required by intranasal infections [31] and the abolishment of transmission when virus aerosolization is blocked with UV treatment of upper room air [22].
Table 1.
Mammalian Models for Influenza Transmission
| Model/Species | Virus Subtype | Transmissiona | Reference | |
|---|---|---|---|---|
| Mouse (MF-1/CFW)1 | H1N1 | Seasonal | A1 | [47-50] |
| H2N2 | Seasonal | A1 | [49] | |
| Pandemic | A1 | [49] | ||
| Mouse (Balb/C) | H1N1 | Seasonal | None | [38] |
| Pandemic | None | [38] | ||
| H3N2 | Pandemic | None | [38] | |
| H5N1 | HPAI | None | [38] | |
|
| ||||
| Ferret | H1N1 | Seasonal | A | [51-52] |
| Pandemic | A | [53-56] | ||
| H3N2 | Seasonal | A | [13-14,57] | |
| Pandemic | ||||
| H1/H3 | Oseltamivir resistant | D/None | [58-60] | |
| H2N2 | Pandemic | D/A | [61] | |
| H5N1 | HPAI | D2/None | [11,14,37] | |
| H7N7 | HPAI | D | [62] | |
| H7N2 | D/None | [62] | ||
| H7N3 | D/None | [62-63] | ||
| H9N2 | D/A | [13,42] | ||
|
| ||||
| Guinea Pigs | H1N1 | Seasonal | D2/A2 | [38,64-65] |
| Pandemic | D/A | [66] | ||
| H3N2 | Seasonal | D/A | [38,64-65] | |
| H1/H3 | Oseltamivir resistant | D | [67] | |
| H5N1 | HPAI | D2/None | [15,66] | |
| H1 | Swine | A2/None | [17,65] | |
| H3N2 | Swine | None | [65] | |
| H9N2 | None | [65] | ||
|
| ||||
| Hamsters | H1N1 | Seasonal | D2 | [68] |
| H3N2 | Seasonal | D | [68] | |
A = airborne transmission, D = direct contact transmission, None = no transmission direct or airborne
Transmission may have been due to differences in mouse strain and/or husbandry techniques (bacterial co-infections were likely to play a role in the 1960s studies)
Partial transmission found
H1N1, the next pandemic
The continuing spread of highly pathogenic avian influenza (HPAI) H5N1 viruses in poultry and the consistent, albeit infrequent, transmission to humans with high mortality rates [32-33] has kept H5N1 a top candidate on the list of potential future pandemics. It has been suggested that human-to-human transmission between family members in close contact has occurred [34-36] however, sustained human-to-human transmission has not been confirmed. It is this lack of human-to-human transmission that has prevented extensive infection, and therefore prevented an H5N1 pandemic.
The inefficient airborne transmission of HPAI H5N1 virus has been confirmed in several mammalian models including ferrets, mice and guinea pigs (Table 1). Numerous studies with wild type H5N1 viruses, reassortants between H5N1 and human viruses, H5N1 viruses adapted by repeated passage, and “designer” H5N1 viruses with mutations known to increase virus binding and/or replication have failed to yield airborne H5 viruses, showing direct contact transmission at best [14,17,37-39]. This highlights the complexity of the mechanism(s) of influenza virus transmissibility and confirms that H5N1 viruses require further adaptation to become a pandemic threat.
Along with H5N1, H9N2 viruses have become enzootic in poultry in large parts of Eurasia [40]. These H9N2 viruses increasingly display human-like receptor specificity [10,13] and have occasionally transmitted to humans and pigs [41-42] with most human cases likely going unreported due to the relatively mild symptoms associated with infection. In the laboratory, H9N2 viruses have been shown to transmit to direct contact ferrets with no prior adaptation or mutations [13] and compared to H5N1 virus, were easily adapted after reassortment in a human H3N2 backbone to become airborne in the ferret model [43]. Recent work indicates that reassortment of an H9N2 virus, within the backbone of the pandemic 2009 H1N1 virus, supports aerosol transmission in the ferret without any further adaptation [44*]. Therefore, currently circulating avian H9N2 viruses are able to create a potentially pandemic virus when provided the opportunity for reassortment with a human-adapted virus.
Virus design; why and how do influenza viruses become airborne?
The major challenges for influenza virus transmission research going forward are the types of studies needed to elucidate mechanisms for transmission. In our opinion, the focus should be on “gain of function” approaches rather than “loss of function”. For the purpose of virus transmission studies, loss of function experiments are like destroying a car engine; remove any crucial part and the engine will stop running. In analogy, mutating a transmissible virus so it no longer transmits is a pointless exercise, giving us none to little mechanistic information; there are a thousand ways to accomplish that. Gain of function experiments mimic tuning the car’s engine; only one or a few parts need tuning but the key is determining which part(s) out of the possible thousand they are. To investigate which viral parts need “a tune up” before it becomes transmissible, at least two options are available, and both should be followed. First, we could “replay” the evolutionary events leading to the pandemic viruses of e.g. 1957 and 1968. Which genetic changes in the avian-origin viral genes made these reassortant viruses airborne? Such experiments are now ongoing in several laboratories. Secondly, we can hypothesize, based on accumulated data, which viral characteristics would facilitate airborne transmission. Below, we discuss several of these features that we believe are important for influenza to become airborne. We postulate that the minimal requirements for airborne influenza viruses are 1) Attachment to and replication in appropriate cells of the URT; 2) High virus yields in the URT; 3) Virus shedding as single particles.
Attachment and Replication
Viruses with binding preference for α2,3 SAs can infect and replicate in human lungs and can lead to severe clinical symptoms and even death, yet these viruses are limited in their ability to infect the URT and subsequently transmit via aerosols (Figure 2A). Thus far, all transmissible viruses bind to α2,6 SAs and are capable of attaching to, replicating in, and transmitting from the URT (Figure 2B). However, the gross receptor binding profile alone does not guarantee transmission. Therefore, efficient transmission may require more subtle differences in receptor preference than α2,3 or α2,6 SA linkage only. Glycan arrays and other assays for virus attachment may facilitate investigation of these subtle differences in binding specificity, but identification of the critical influenza virus receptors on the cells of the URT and LRT is needed to facilitate future research on host and tissue specificity as well as transmission.
Figure 2. Proposed minimal requirements for influenza viruses to become airborne.
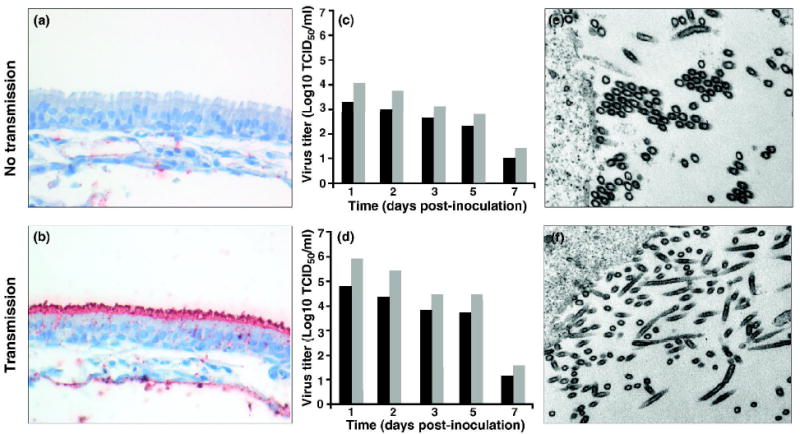
Figures represent theoretical virus subtypes with non-transmissible (virus 1) and transmissible (virus 2) phenotypes, unpublished data. Virus attachment to ferret URT is visualized with FITC-labelled viruses. (A) Shows no attachment of virus 1 to URT whereas (B) shows red staining indicative for attachment of virus 2 to the ferret URT. Virus yield in the URT of ferrets (intranasal infection) is shown for virus 1 (C) and virus 2 (D), with grey bars representing virus shedding from nose swabs and black bars from throat swabs. Electron microscopy of viruses budding from human 293T cells. (E) Shows viral aggregates released in clusters of spherical particles of virus 1 while (F) shows single virus 2 particles being released from the infected cell as both spherical and filamentous virions.
High virus yields in the URT
When the extent of virus replication of airborne viruses is low for example, after vaccination with seasonal live attenuated viruses, transmission generally does not occur [45*-46] (Fig 2C). To date, all pandemic viruses have established efficient and productive infections in the URT (Fig 2D). The mechanism necessary for URT tropism has been linked to affinity for α2,6-SAs and adaptive mutations supporting replication at ~33°C, which optimizes molecular interactions between viral proteins and cellular host factors [16-19]. High levels of virus replication in the URT may ensure that large amounts of progeny virus are released into aerosols from the nose and mouth upon sneezing, coughing, or breathing.
Virus shedding as single particles
Low NA activity can result in inefficient cleavage of SAs and as a consequence, inefficient release and aggregation of virus particles resulting in little to no successive rounds of replication (Figure 2E). The substrate specificity and activity of NA and HA must be in some balance with respect to receptor binding and cleavage in order to maximize the yield of progeny shedding as single virus particles that are efficiently transmitted (Figure 2F). In addition to HA, the NA’s role in virus transmission warrants further investigation.
Unknowns
There are many unknowns when it comes to airborne transmission. The above factors are only a starting point for research. More work is needed to elucidate the relative contribution of human influenza virus transmission via contact, (large) respiratory droplets, and aerosols. With respect to airborne routes, how much does sneezing and coughing add to transmission in comparison to breathing alone? How representative are the available animal models (guinea pigs, ferrets) for transmission in humans? Guinea pigs generally do not sneeze upon influenza virus infection yet transmit viruses via the airborne route and some viruses are not transmitted between ferrets despite frequent sneezing of the animals [24]. Neither of these results provides definitive proof for a role of coughing and sneezing in transmission. Other important questions are whether airborne viruses come from one or many cell types, whether virus shape is important for transmission or virus stability and whether key changes that drive transmission of one viral subtype are applicable to every other viral subtype. Research and attention should be focused on answering these questions regarding the mechanisms involved in airborne transmission. It is crucial to sustain the current funding, energy and collaboration in order to answer these key questions, which may in the future, be able to inform approaches to prioritizing risk from other emerging viruses.
Acknowledgments
The authors thank Debby van Riel for providing Figure 2 A and B. The research of the authors is sponsored under contract HHSN266200700010C from National Institutes of Health/National Institute of Allergy and Infectious Diseases (NIH/NIAID). M.G. is a Marie Curie fellow and funded under contract PIEF-GA-2009-237505
References
- 1.Taubenberger JK, Morens DM. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2*.Smith GJ, Bahl J, Vijaykrishna D, Zhang J, Poon LL, Chen H, Webster RG, Peiris JS, Guan Y. Dating the emergence of pandemic influenza viruses. Proc Natl Acad Sci U S A. 2009;106:11709–11712. doi: 10.1073/pnas.0904991106. The authors estimate the evolutionary history and date of introduction to humans of the 20th century pandemic viruses. This is this study indicates that H1N1 influenza was circulating in mammals as early as 1911 and that the 1918 pandemic resulted from reassortment and not a recent avian introduction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scholtissek C, Rohde W, Von Hoyningen V, Rott R. On the origin of the human influenza virus subtypes H2N2 and H3N2. Virology. 1978;87:13–20. doi: 10.1016/0042-6822(78)90153-8. [DOI] [PubMed] [Google Scholar]
- 4.Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325:197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith GJ, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, Ma SK, Cheung CL, Raghwani J, Bhatt S, et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature. 2009;459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 6.Ma W, Kahn RE, Richt JA. The pig as a mixing vessel for influenza viruses: Human and veterinary implications. J Mol Genet Med. 2008;3:158–166. [PMC free article] [PubMed] [Google Scholar]
- 7.Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol. 2000;74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 9.Stevens J, Blixt O, Chen LM, Donis RO, Paulson JC, Wilson IA. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J Mol Biol. 2008;381:1382–1394. doi: 10.1016/j.jmb.2008.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matrosovich MN, Krauss S, Webster RG. H9N2 influenza A viruses from poultry in Asia have human virus-like receptor specificity. Virology. 2001;281:156–162. doi: 10.1006/viro.2000.0799. [DOI] [PubMed] [Google Scholar]
- 11.Maines TR, Chen LM, Van Hoeven N, Tumpey TM, Blixt O, Belser JA, Gustin KM, Pearce MB, Pappas C, Stevens J, et al. Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology. 2011;413:139–147. doi: 10.1016/j.virol.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chutinimitkul S, van Riel D, Munster VJ, van den Brand JM, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA, de Wit E. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J Virol. 2010;84:6825–6833. doi: 10.1128/JVI.02737-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wan H, Sorrell EM, Song H, Hossain MJ, Ramirez-Nieto G, Monne I, Stevens J, Cattoli G, Capua I, Chen LM, et al. Replication and transmission of H9N2 influenza viruses in ferrets: evaluation of pandemic potential. PLoS One. 2008;3:e2923. doi: 10.1371/journal.pone.0002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maines TR, Chen LM, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcon A, Nguyen TH, Maile Q, Sedyaningsih ER, et al. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc Natl Acad Sci U S A. 2006;103:12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15*.Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, et al. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 2009;5:e1000709. doi: 10.1371/journal.ppat.1000709. The authors investigate the basis for H5N1 transmission using guinea pigs as a mammalian model to study multiple H5N1 avian influenza viruses. They found two viruses were transmitted through direct contact due to amino acid changes: At position 701 of PB2 asparagine (Asn) and at position 160 of HA (Thr160Ala), resulting in the loss of glycosylation at 158-160. These amino acids changes in PB2 and HA could serve as important molecular markers for assessing the pandemic potential of H5N1 field isolates. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamada S, Hatta M, Staker BL, Watanabe S, Imai M, Shinya K, Sakai-Tagawa Y, Ito M, Ozawa M, Watanabe T, et al. Biological and structural characterization of a host-adapting amino acid in influenza virus. PLoS Pathog. 2010;6 doi: 10.1371/journal.ppat.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 2009;5:e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Hoeven N, Pappas C, Belser JA, Maines TR, Zeng H, Garcia-Sastre A, Sasisekharan R, Katz JM, Tumpey TM. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc Natl Acad Sci U S A. 2009;106:3366–3371. doi: 10.1073/pnas.0813172106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19*.Mehle A, Doudna JA. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc Natl Acad Sci U S A. 2009;106:21312–21316. doi: 10.1073/pnas.0911915106. The authors discuss changes in the influenza polymerase complex that can overcome species-specific barriers to infection. In addition to the glutamic acid to lysine change at 627 of PB2, two additional pathways have been identified where influenza can evolve to enhance replication in humans. The first is by second-site suppressor mutations in PB2 that improve polymerase activity, the second by introduction of a human PA subunit into an avian polymerase. Both overcome restriction in human cells. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehle A, Doudna JA. An inhibitory activity in human cells restricts the function of an avian-like influenza virus polymerase. Cell Host Microbe. 2008;4:111–122. doi: 10.1016/j.chom.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21**.Gustin KM, Belser JA, Wadford DA, Pearce MB, Katz JM, Tumpey TM, Maines TR. Influenza virus aerosol exposure and analytical system for ferrets. Proc Natl Acad Sci U S A. 2011 doi: 10.1073/pnas.1100768108. The authors indicate that aerosol inoculation of ferrets mimics natural influenza infection better than intranasal infection, typically used in influenza studies in ferrets. They compare virus deposition, infectivity, virulence, and transmissibility in ferrets inoculated intranasally or by aerosols. They also show that viable virus is measurable in droplets and droplet nuclei exhaled by infected ferrets. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface. 2009;6(Suppl 6):S783–790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brankston G, Gitterman L, Hirji Z, Lemieux C, Gardam M. Transmission of influenza A in human beings. Lancet Infect Dis. 2007;7:257–265. doi: 10.1016/S1473-3099(07)70029-4. [DOI] [PubMed] [Google Scholar]
- 24*.Bouvier NM, Lowen AC. Animal Models for Influenza Virus Pathogenesis and Transmission. Viruses. 2010;2:1530–1563. doi: 10.3390/v20801530. The authors review all known mammalian models for influenza transmission and pathogenesis. They highlight pros and cons for each model and perform a literature review on studies performed in each model. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hinds W. Wiley. 2 1999. Aerosol Technology, Properties, Behavior, and Measurement of Airborne Particles. [Google Scholar]
- 26.Edwards DA, Man JC, Brand P, Katstra JP, Sommerer K, Stone HA, Nardell E, Scheuch G. Inhaling to mitigate exhaled bioaerosols. Proc Natl Acad Sci U S A. 2004;101:17383–17388. doi: 10.1073/pnas.0408159101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fabian P, McDevitt JJ, DeHaan WH, Fung RO, Cowling BJ, Chan KH, Leung GM, Milton DK. Influenza virus in human exhaled breath: an observational study. PLoS One. 2008;3:e2691. doi: 10.1371/journal.pone.0002691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindsley WG, Blachere FM, Thewlis RE, Vishnu A, Davis KA, Cao G, Palmer JE, Clark KE, Fisher MA, Khakoo R, et al. Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS One. 5:e15100. doi: 10.1371/journal.pone.0015100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lowen AC, Palese P. Influenza virus transmission: basic science and implications for the use of antiviral drugs during a pandemic. Infect Disord Drug Targets. 2007;7:318–328. doi: 10.2174/187152607783018736. [DOI] [PubMed] [Google Scholar]
- 30.Steel J, Palese P, Lowen AC. Transmission of a 2009 pandemic influenza virus shows a sensitivity to temperature and humidity similar to that of an H3N2 seasonal strain. J Virol. 2011;85:1400–1402. doi: 10.1128/JVI.02186-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alford RH, Kasel JA, Gerone PJ, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med. 1966;122:800–804. doi: 10.3181/00379727-122-31255. [DOI] [PubMed] [Google Scholar]
- 32.Confirmed Human Cases of Avian Influenza A(H5N1) on World Wide Web. URL: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2011_05_13/en/index.html.
- 33.Van Kerkhove MD, Mumford E, Mounts AW, Bresee J, Ly S, Bridges CB, Otte J. Highly pathogenic avian influenza (H5N1): pathways of exposure at the animal-human interface, a systematic review. PLoS One. 2011;6:e14582. doi: 10.1371/journal.pone.0014582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ungchusak K, Auewarakul P, Dowell SF, Kitphati R, Auwanit W, Puthavathana P, Uiprasertkul M, Boonnak K, Pittayawonganon C, Cox NJ, et al. Probable person-to-person transmission of avian influenza A (H5N1) N Engl J Med. 2005;352:333–340. doi: 10.1056/NEJMoa044021. [DOI] [PubMed] [Google Scholar]
- 35.Wang H, Feng Z, Shu Y, Yu H, Zhou L, Zu R, Huai Y, Dong J, Bao C, Wen L, et al. Probable limited person-to-person transmission of highly pathogenic avian influenza A (H5N1) virus in China. Lancet. 2008;371:1427–1434. doi: 10.1016/S0140-6736(08)60493-6. [DOI] [PubMed] [Google Scholar]
- 36.Kandun IN, Wibisono H, Sedyaningsih ER, Yusharmen, Hadisoedarsuno W, Purba W, Santoso H, Septiawati C, Tresnaningsih E, Heriyanto B, et al. Three Indonesian clusters of H5N1 virus infection in 2005. N Engl J Med. 2006;355:2186–2194. doi: 10.1056/NEJMoa060930. [DOI] [PubMed] [Google Scholar]
- 37.Jackson S, Van Hoeven N, Chen LM, Maines TR, Cox NJ, Katz JM, Donis RO. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. J Virol. 2009;83:8131–8140. doi: 10.1128/JVI.00534-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yen HL, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, et al. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J Virol. 2007;81:6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lowen AC, Mubareka S, Tumpey TM, Garcia-Sastre A, Palese P. The guinea pig as a transmission model for human influenza viruses. Proc Natl Acad Sci U S A. 2006;103:9988–9992. doi: 10.1073/pnas.0604157103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maines TR, Szretter KJ, Perrone L, Belser JA, Bright RA, Zeng H, Tumpey TM, Katz JM. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunol Rev. 2008;225:68–84. doi: 10.1111/j.1600-065X.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- 41.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. Human infection with influenza H9N2. Lancet. 1999;354:916–917. doi: 10.1016/s0140-6736(99)03311-5. [DOI] [PubMed] [Google Scholar]
- 42.Peiris JS, Guan Y, Markwell D, Ghose P, Webster RG, Shortridge KF. Cocirculation of avian H9N2 and contemporary “human” H3N2 influenza A viruses in pigs in southeastern China: potential for genetic reassortment? J Virol. 2001;75:9679–9686. doi: 10.1128/JVI.75.20.9679-9686.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sorrell EM, Wan H, Araya Y, Song H, Perez DR. Minimal molecular constraints for respiratory droplet transmission of an avian-human H9N2 influenza A virus. Proc Natl Acad Sci U S A. 2009;106:7565–7570. doi: 10.1073/pnas.0900877106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44*.Kimble B, Sorrell E, Shao H, Martin P, Perez DR. Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model. Proc Natl Acad Sci U S A. 2011 doi: 10.1073/pnas.1108058108. in press. The authors show that given the internal genes from the 2009 H1N1 pandemic, avian H9N2 influenza can readily replicate and transmit via aerosol droplets in the ferret model. Thus, given the environment to support reassortment, this avian H9N2 virus can support aerosol transmission without any additional adaptation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45*.Lowen AC, Steel J, Mubareka S, Carnero E, Garcia-Sastre A, Palese P. Blocking interhost transmission of influenza virus by vaccination in the guinea pig model. J Virol. 2009;83:2803–2818. doi: 10.1128/JVI.02424-08. The authors reviewed the efficacy of vaccination in blocking transmission of influenza viruses between guinea pigs. Three modes of immunization were compared: natural infection, inactivated virus, and live attenuated virus. The ability of each immunization method to block transmission of a homologous a heterologous subtype influenza was tested. They found that previous infection through a natural route provided sterilizing immunity against both homologous and heterologous challenges whereas vaccination with an inactivated virus did not. Vaccination with a live attenuated virus was more efficacious than with inactivated virus, resulting in sterilizing immunity against homologous challenge and full protection against the transmission of the homologous and heterologous viruses to naïve contacts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pearce MB, Belser JA, Houser KV, Katz JM, Tumpey TM. Efficacy of seasonal live attenuated influenza vaccine against virus replication and transmission of a pandemic 2009 H1N1 virus in ferrets. Vaccine. 2011;29:2887–2894. doi: 10.1016/j.vaccine.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 47.Schulman JL. Experimental transmission of influenza virus infection in mice. IV. Relationship of transmissibility of different strains of virus and recovery of airborne virus in the environment of infector mice. J Exp Med. 1967;125:479–488. doi: 10.1084/jem.125.3.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schulman JL. Experimental transmission of influenza virus infection in mice. 3. Differing effects of immunity induced by infection and by inactivated influenza virus vaccine on transmission of infection. J Exp Med. 1967;125:467–478. doi: 10.1084/jem.125.3.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schulman JL. The use of an animal model to study transmission of influenza virus infection. Am J Public Health Nations Health. 1968;58:2092–2096. doi: 10.2105/ajph.58.11.2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schulman JL. Effects of immunity on transmission of influenza: experimental studies. Prog Med Virol. 1970;12:128–160. [PubMed] [Google Scholar]
- 51.Smith W, A C, Laidlaw PP. A virus obtained from influenza patients. Lancet. 1933;2:66–68. [Google Scholar]
- 52.Francis T, Magill TP. Immunological Studies with the Virus of Influenza. J Exp Med. 1935;62:505–516. doi: 10.1084/jem.62.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maines TR, Jayaraman A, Belser JA, Wadford DA, Pappas C, Zeng H, Gustin KM, Pearce MB, Viswanathan K, Shriver ZH, et al. Transmission and pathogenesis of swine-origin 2009 A(H1N1) influenza viruses in ferrets and mice. Science. 2009;325:484–487. doi: 10.1126/science.1177238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Munster VJ, de Wit E, van den Brand JM, Herfst S, Schrauwen EJ, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, et al. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perez DR, Sorrell E, Angel M, Ye J, Hickman D, Pena L, Ramirez-Nieto G, Kimble B, Araya Y. Fitness of pandemic H1N1 and seasonal influenza A viruses during co-infection: evidence of competitive advantage of pandemic H1N1 influenza versus seasonal influenza. PLoS Curr. 2009;1:RRN1011. doi: 10.1371/currents.RRN1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 57.Herlocher ML, Elias S, Truscon R, Harrison S, Mindell D, Simon C, Monto AS. Ferrets as a transmission model for influenza: sequence changes in HA1 of type A (H3N2) virus. J Infect Dis. 2001;184:542–546. doi: 10.1086/322801. [DOI] [PubMed] [Google Scholar]
- 58.Herlocher ML, Carr J, Ives J, Elias S, Truscon R, Roberts N, Monto AS. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 2002;54:99–111. doi: 10.1016/s0166-3542(01)00214-5. [DOI] [PubMed] [Google Scholar]
- 59.Herlocher ML, Truscon R, Elias S, Yen HL, Roberts NA, Ohmit SE, Monto AS. Influenza viruses resistant to the antiviral drug oseltamivir: transmission studies in ferrets. J Infect Dis. 2004;190:1627–1630. doi: 10.1086/424572. [DOI] [PubMed] [Google Scholar]
- 60.Yen HL, Herlocher LM, Hoffmann E, Matrosovich MN, Monto AS, Webster RG, Govorkova EA. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob Agents Chemother. 2005;49:4075–4084. doi: 10.1128/AAC.49.10.4075-4084.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pappas C, Viswanathan K, Chandrasekaran A, Raman R, Katz JM, Sasisekharan R, Tumpey TM. Receptor specificity and transmission of H2N2 subtype viruses isolated from the pandemic of 1957. PLoS One. 2010;5:e11158. doi: 10.1371/journal.pone.0011158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Belser JA, Blixt O, Chen LM, Pappas C, Maines TR, Van Hoeven N, Donis R, Busch J, McBride R, Paulson JC, et al. Contemporary North American influenza H7 viruses possess human receptor specificity: Implications for virus transmissibility. Proc Natl Acad Sci U S A. 2008;105:7558–7563. doi: 10.1073/pnas.0801259105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song H, Wan H, Araya Y, Perez DR. Partial direct contact transmission in ferrets of a mallard H7N3 influenza virus with typical avian-like receptor specificity. Virol J. 2009;6:126. doi: 10.1186/1743-422X-6-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mubareka S, Lowen AC, Steel J, Coates AL, Garcia-Sastre A, Palese P. Transmission of Influenza Virus via Aerosols and Fomites in the Guinea Pig Model. J Infect Dis. 2009 doi: 10.1086/597073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sun Y, Bi Y, Pu J, Hu Y, Wang J, Gao H, Liu L, Xu Q, Tan Y, Liu M, et al. Guinea pig model for evaluating the potential public health risk of swine and avian influenza viruses. PLoS One. 2010;5:e15537. doi: 10.1371/journal.pone.0015537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Steel J, Staeheli P, Mubareka S, Garcia-Sastre A, Palese P, Lowen AC. Transmission of pandemic H1N1 influenza virus and impact of prior exposure to seasonal strains or interferon treatment. J Virol. 2010;84:21–26. doi: 10.1128/JVI.01732-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bouvier NM, Lowen AC, Palese P. Oseltamivir-resistant influenza A viruses are transmitted efficiently among guinea pigs by direct contact but not by aerosol. J Virol. 2008;82:10052–10058. doi: 10.1128/JVI.01226-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ali MJ, Teh CZ, Jennings R, Potter CW. Transmissibility of influenza viruses in hamsters. Arch Virol. 1982;72:187–197. doi: 10.1007/BF01348964. [DOI] [PubMed] [Google Scholar]


