Synopsis
Minimal hepatic encephalopathy (MHE) is associated with a high risk of development of overt hepatic encephalopathy, impaired quality of life and driving accidents. The detection of MHE requires specialized testing since it cannot by definition, be diagnosed on standard clinical examination. Psychometric (paper-pencil or computerized or a combination) and neuro-physiological techniques are often used to test for MHE. Paper-pencil psychometric batteries like the Psychometric Hepatic Encephalopathy Score (PHES) have been validated in several countries but do not have US normative values. Computerized tests such as the inhibitory control test (ICT), cognitive drug research system and Scan test have proven useful to diagnose MHE and predict outcomes. The specificity and sensitivity of these tests are similar to the recommended gold standards. Neuro-physiological tests such as the EEG and its interpretations, evoked potentials and Critical Flicker Frequency (CFF) also provide useful information. The diagnosis of MHE is an important issue for clinicians and patients alike and the testing strategies depend on the normative data available, patient comfort and local expertise.
Keywords: minimal hepatic encephalopathy, diagnosis, computerized testing, cognition, inhibitory control test, cognitive drug research system, critical flicker frequency
Introduction
Hepatic encephalopathy consists of a spectrum of neuropsychiatric abnormalities seen in patients with advanced liver disease, and is diagnosed after the exclusion of other known brain disease 1. While overt hepatic encephalopathy (OHE) is often times diagnosed clinically, minimal hepatic encephalopathy (MHE) is more difficult to diagnose and more often requires the use of specialized testing to do so. MHE is regarded as a preclinical stage of OHE 2, and results in a spectrum of cognitive deficits known as SONIC: spectrum of neuro-cognitive impairment in cirrhosis3, particularly in the domains of attention, vigilance, response inhibition, and executive function 4–6,7. This sector of the continuum is being better recognized as having significant impact on quality of life in patients with cirrhosis. It is believed that approximately 60–80% of patients with cirrhosis tested have evidence of cognitive impairment or MHE 8. In addition to the burden on quality of life, patients with evidence of MHE have increased risk for progression to OHE, as well as pose a potential danger to themselves or the community in the operation of heavy equipment and a motor vehicle 4. Not only does this clinical condition affect the individual and those individuals in their immediate vicinity, there is also resource demand on society at large as costs rise to care for patients who ultimately have a high risk of developing OHE 2.
The first challenge to treating these patients is identification and diagnosis. Diagnosis of MHE remains difficult and most cirrhotics are not routinely tested 9, 10,11. The reasoning for this lies in the time, psychological expertise, and financial burdens of copyright constraints of administering the psychometric tests recommended by the Working Group of Hepatic Encephalopathy 1. The Working Group on Hepatic Encephalopathy divided the diagnosis of HE into three categories: A (acute liver failure), B (porto-systemic bypass without liver disease), and C (cirrhosis) 1. Here, we will do a review of the literature as pertaining to group C, cirrhosis from 2001 to 2011. This groups is clinically divided into episodic or persistent HE depending on their chronicity and minimal HE. We will also include any key information outside of this date range included.
Specific testing for cirrhosis and normal mental status
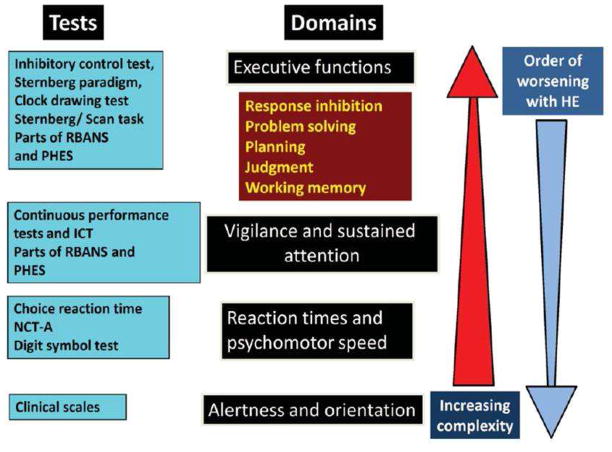
As previously discussed, the Working Group on Hepatic Encephalopathy updated the classification of hepatic encephalopathy, which differentiates the stages of MHE and OHE1. The differentiation between a normal patient and one with subtle neurocognitive changes poses a difficult task, and can only be defined by the presence of specific changes on psychometric testing and attention deficits 5. Attention deficits play a role in a patient’s ability to orient, perform executive functions, and impairs learning and working memory 12. These neurocognitive changes also involve defects in visuo-motor coordination and response inhibition, both of which are important when operating a motor vehicle safely 13–16. The investigation of these problems can only be done by application of neuropsychometric or neuro-physiologic testing, and the current repertoire employs both the use of traditional pen-paper and computerized testing (Figure 1 and Table 1).
Figure 1.
Progression of Severity of Disease and Appropriate Testing Strategies for Each Stage (Reprinted with permission from John Wiley and Sons, Bajaj et al Spectrum of Neurocognitive Impairment in Cirrhosis: Implications for Assessment of Hepatic Encephalopathy; Hepatology 2009 (Reference 3))
Table 1.
Characteristics of methods used to diagnose MHE (Reprinted with permission from John Wiley and Sons, Bajaj et al Spectrum of Neurocognitive Impairment in Cirrhosis: Implications for Assessment of Hepatic Encephalopathy; Hepatology 2009 (Reference 3))
| Test | Domains tested | US Norms | Copyright | Specialized expertise (Psychology/Neurology) needed | Time for administration interpretation | Specific comments |
|---|---|---|---|---|---|---|
| Paper-pencil psychometric tests | ||||||
| NCT-A (number connection test-A) | Psychomotor speed | + | No | No | 30–120 second | Poor specificity |
| NCT-B (number connection test-B) | Psychomotor speed, set shifting, divided attention | − | Yes | Yes | 1–3 minutes | More specific than NCT-A but is not patho-gnomonic for any disorder |
| BDT (Block Design test) | Visuo-spatial reasoning, praxis, psychomotor speed | + | Yes | Yes | 10–20 minutes | It can be used for dementia testing as well. |
| DST (Digit Symbol test) | Psychomotor speed, attention | + | Yes | Yes | 2 minutes | Tends to be very sensitive and is an early indicator. |
| LTT (Line tracing test) | Psychomotor speed, visuo-spatial | − | Yes | No | 10 minutes | Outcomes are errors and time; tests a balance between speed and accuracy |
| SDT (Serial Dotting test) | Psychomotor speed | − | Yes | No | 1–4 minutes | Only tests psychomotor speed |
| RBANS (Repeatable Battery for Assessment of Neuro-psychological Status) | Verbal/visual/working memory, visuospatial, language & psychomotor speed | + | Yes | Yes | 35 minutes | Has been primarily studied in dementia and brain injury, current trials with HE are underway |
| Computerized Psychometric Tests | ||||||
| ICT | Response inhibition, working memory, vigilance, attention | Limited norms | Yes | No | 15 minutes | Need highly functional patients, Familiarity with computers may be needed |
| CDRS | Attention, episodic and working memory | − | Yes | No | 15–20 minutes | |
| Sternberg paradigm or Scan test | Working memory, vigilance, attention | − | Yes | No | 10–15 minutes | |
| Neuro-physiological Tests | ||||||
| EEG MDF and spectral index | Generalized brain activity | Local norms | No | Yes | Different ranges | Can be performed in comatose patients |
| Visual Evoked potentials | Interval between visual stimulus and activity | Local norms | No | Yes | Different ranges | Highly variable and poor overall results |
| Brainstem auditory evoked potentials | Response in the cortex after auditory click stimuli. | Local norms | No | Yes | Different ranges | Inconsistent response with HE testing/prognostication |
| P300 cognitive evoked potentials | An infrequent stimulus embedded in irrelevant stimuli is studied. | Local norms | No | Yes | Different ranges | Good diagnostic potential but requires patient cooperation |
| CFF | Visual discrimination and general arousal | − | No | No | 10 minutes | Need highly functional patients |
NCT-A/B: number connection tests A/B, DST: digit symbol test, BDT: Block Design Test, SDT: Serial dotting test, LTT: line tracing test, ICT: inhibitory control test, CDR: Cognitive Disease Research, RBANS: repeatable battery for assessment of neuropsychological status, EEG: electroencephalogram, MDF: mean dominant frequency, CFF: critical flicker fusion frequency. NCT-A, NCT-B, DST, LTT and SDT are parts of the psychometric hepatic encephalopathy score (PHES). Expense for each test depends on local availability, the need for copyrighted test materials and computers. Up-front costs may be minimal if these tests are used often.
Paper and Pencil Psychometric tests for MHE
Psychometric hepatic encephalopathy score (PHES)
Several batteries for the diagnosis of HE have been studied, and center around detection of deficits in attention and processing speed 17. They identify impairments in visuo-spatial function, attention, response time and inhibition, and are sensitive to the changes associated with MHE. The Psychometric Hepatic Encephalopathy Score (PHES) was specifically designed to detect changes associated with MHE, and comprises of five different tests. The number connection test-A (NCT-A), number connection test-B (NCT-B), digit symbol test (DST), line tracing test, and the serial dotting test all comprise the PHES. Each of the different exams tests for deficits in different areas; NCT-A and B evaluate concentration, mental tracking, and visuo-motor speed. NCT-B does this with greater complexity. The digit symbol test evaluates psychomotor and visuo-motor speed, while the line tracing test examines visuo-motor and visuo-spatial skills with attention given to speed and accuracy. Lastly, the serial dotting test is a test of psychomotor speed. Each test is scored on a scale of 1 to −3 according to standard deviation. Score ranges are between +6 and −18, with the determining value for pathology at −4 points. This score has a sensitivity of 96% and Specificity of 100%, with validation in several different countries such as Germany, Italy, and Spain 5, 18, 19. This test has not yet been validated in the United States 1. If the entire PHES is unable to be completed, the Working Group on Hepatic Encephalopathy has recommended a combination of two of the following four tests: NCT-A, NCT-B, digit symbol test, or block design test. The recommendation is that impairment in at least two of these tests two standard deviations beyond age-matched controls of same education indicates dysfunction 1. The disadvantages of the PHES is that it is time consuming, not widely available in the United States, a poor test in memory, and often times difficult to interpret. As an advantage, it is the current gold standard endorsed by the Working Party at the 1998 World Congress of Gastroenterology.
Rather than performing the entire PHES, Riggio et al 20 performed a logistical regression analysis by first incorporating the scores of the 5 tests included in the PHES, and subsequently eliminating stepwise those variables that could be removed without impairing regression called the “ Simplified psychometric hepatic encephalopathy score (SPHES)”. The logistic analysis in this study showed that a model containing only the digit symbol test (DST), the serial dotting test (SDT), and the line tracing test (LLT) was similar to that containing the whole set of tests 20. This is important in simplifying a test that is already highly regarded for being able to diagnose MHE. However SPHES includes the LTT, which is the test that requires the longest to score and there is controversy as to how to interpret its two outcomes; time and errors. The use of the SPHES decreased the time required for MHE screening but since the NCT-A and B only require a maximum of 3 minutes, the practical utility of this reduction is not certain.
Repeatable battery for assessment of neurological status (RBANS)
Another paper and pencil test recently recommended for use in diagnosis of MHE is the repeated battery for the assessment of neuropsychological status (RBANS). The International Society for the Study of Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) has recommended that this test, originally designed to diagnose neurocognitive disorders such as dementia, traumatic brain injury, stroke, multiple sclerosis, and bipolar disorder, be an alternative to PHES 21. The RBANS has not been formally compared to the PHES, and has been the alternative in the US. It has been used in several studies in the US as an effective tool for screening for MHE 22, 23, however has not been formally compared to the PHES head to head. The test itself is divided in cortical and sub-cortical domains, and HE patients perform worse on the sub-cortical components 21. While both of these exams are able to provide information in detecting the diagnosis of MHE, both require a psychologist to order, administer and interpret in the US. Therefore a movement towards computerized testing has the potential to expedite both administration and interpretation of MHE and HE.
Computerized Psychometric Tests
Paper and pencil tests rely heavily on the motor function and involve multiple cognitive functions for their completion. Efforts to overcome this issue have employed the use of reaction time 24–26 which may take advantage of computerized testing and simple button pushing on the part of the patient. Reduced peripheral motor skills have the potential for complicating the interpretation of cognitive function, which is the goal of these tests. Computerized testing would simplify motor response, and may give information about other aspects of cognitive ability like reaction time. The following are available computerized tests for diagnosis of hepatic encephalopathy.
Choice tests and Sternberg Paradigm
Amodio et al used a series of three computerized tests known as the Scan, Choice 1 and Choice 2 tests in a group of 94 cirrhotic patients. They then followed the patients for overall survival and compared these tests to the NCT-A. The Scan test is based on the Sternberg paradigm in which the mean reaction times and the percentage of errors to recognize whether there is at least a common number in pairs of numbers digit (“1” or “3”) in pairs of numbers displayed on the computer screen. The test was performed by displaying a series of 72 random, sorted pairs of numbers for 3 seconds on the screen. The Choice test 1 and 2 differed on difficulty of the task; Choice 1 measures the mean reaction times and the percentage of errors when pressing the same digit (comprised between 1 and 4) on the keyboard, which was displayed for 3 seconds. Choice 2 measured the reaction times as well as the percentage errors when a reverse sequence of what was displayed on the screen was displayed. They used a weighted reaction time (Rt) as their outcomes. The team found that NCT-A, Choice 2 and Scan test were related to the severity of liver disease which was not affected by disease etiology. Importantly they found that overall survival was associated with alteration in Scan test (Hazard ratio 2.4) and the Choice 2 (Hazard ratio 2.8) along with the Child Class 27. This test however needs to be validated in other populations.
Inhibitory Control Test
As mentioned earlier, the computerized psychometric tests have been developed in the last 6 years, and have the opportunity to change the face of how MHE is diagnosed. The Inhibitory Control Test (ICT) is a computerized test of attention and response inhibition that has been used to characaterize attention deficit disorder, schizophrenia, and traumatic brain injury 6, 28–30. ICT measures response to lures, targets, and reaction times to provide objective measurement of separate but complementary aspects of impairment in MHE. The lure response is an act of commission, signifying a defect in response inhibition 31. Response inhibition is an essential aspect of executive function, which allows a subject to inhibit an incorrect response 7, 32. Impairment of response inhibition is responsible for potentiating wrong decisions in psychometric testing and in everyday life, and the ICT has been able to also quantify these errors in MHE 4, 33. The ICT also measures target detection rate, and errors in not detecting targets are considered errors of omission. These errors are considered primary errors of attention. Errors of omission are commonly associated with diminished processing speed and impairment of visuomotor function 28. Both outcomes provide information about separate but complementary aspects of impairment in MHE.
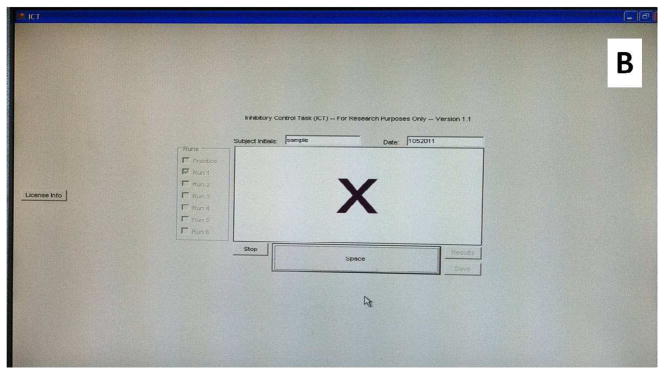
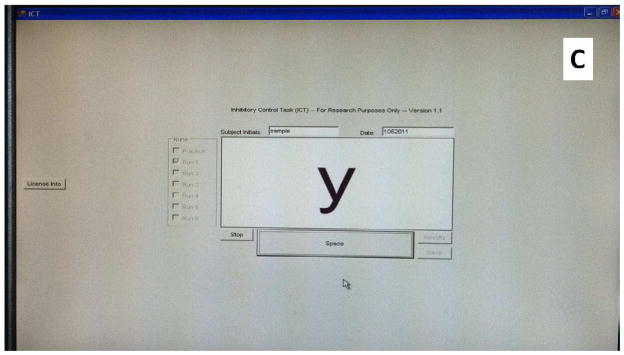
The test consists of the presentation of several letters at 500-ms intervals, with the letters X and Y interspersed. The subject is instructed to respond to every X and Y during the initial part of the training program. This establishes the prepotent response. In the latter part of the training run, the subject is instructed only to respond when X and Y are alternating (targets) and to inhibit from responding when the X and Y are not alternating (lures) (Figures 2A, B and C). Typically, 6 test runs are completed by the patient, lasting two minutes, with a total of 40 lures, 212 targets, and 1728 random letters in between. At the test conclusion, the lure and target response rates, lures, and target reaction time are automatically calculated. Good psychometric testing will depict lower lure response, higher target response, and shorter lure and target reaction times.
Figure 2.
The inhibitory control test
2A: Picture of a subject taking the ICT on a computer screen
2B: The appearance of the letter “X” on the computer screen during ICT
2C: The appearance of the letter “Y” on the computer screen during ICT
The ICT has been used in two US centers and results are also available from two Italian Centers. The results from the US were based on analysis of >200 patients with varying degree of cirrhosis and HE compared to healthy, age and education-matched controls. The initial testing was performed using the NCT-A, DST and BDT as gold standards. Using just the ICT lures in the US population, there was good sensitivity and specificity for diagnosis of MHE. There was a significantly lower target response and higher lure and target reaction times in MHE patients compared to others, but they did not add to the differentiation between the groups. The same group found that ICT lures were equivalent to the standard battery in predicting development of overt HE. ICT has also been externally validated when applied to those patients who have received the transvenous intrahepatic portosystemic shunt (TIPS) procedure and those treated with probiotic therapy and rifaximin 4,34. There is correlation with worsened response to lures in patients status-post TIPS procedure, and improved lure response in patients treated with probiotic therapy 4. Both of these observations are important as we see that change in disease status changes test findings.
ICT is a computerized instrument with automated analysis. Therefore inter- /intraobserver reliability is not important. Studies conducted thus far have shown a high correlation of ICT lures and targets between administrations, indicating good test-retest reliability 4, 33. Studies have shown that the ICT is correlated with driving impairment on a simulator as well as with actual traffic accidents on a retrospective and prospective analysis 14, 16. Both of these findings suggest that ICT may be useful in not only the clinical setting for diagnostic purposes, but also in the trial setting. The experience of the Italian investigators was different with ICT since their population was significantly more advanced clinically and had a lower educational background and exposure to computers 35. They concluded that a weighted lures (lures divided by the square of target accuracy) was a better differentiator of MHE in their patient population. Like Bajaj et al, they also did not find any difference in ICT outcomes between alcoholic and non-alcoholic etiology. The utility of ICT may be due to the difficulty of resource availability for the other psychometric tests, like PHES in the US. A modified version of the ICT is available for use and may be administered on a personal computer available for free download at www.hecme.tv. Also an advantage is that ICT administration can be taught to an untrained, MA-level provider in approximately 30 minutes 4, as opposed to the necessary use of a trained psychologist for administration of more traditional tests. Both the resources of time and personnel have tremendous implications on cost and logistical plausibility of being to obtain the diagnosis of MHE in the clinical setting, and properly address the needs of the patient. In addition, because ICT involves recognizing specific letters, it can potentially be administered to non-English-speaking subjects with minimal modifications.
Cognitive Drug Research (CDR) computerized assessment system
This system was developed by Cognitive Drug Research Ltd (CDR), (Goring-on-Thames, United Kingdom), and is a battery of five psychometric subsets that test attention power, attention continuity, speed of memory, and quality of episodic and working memory 36. Over 50 parallel forms of each task, the CDR system has been used to cognitive function in clinical trials 37, as well as neuropsychiatric conditions in patients with cirrhosis 38. In 2008, a comparison was done between the utility of the CDR computerized assessment battery and the PHES for measuring cognitive function in the cirrhotic patients being evaluated for liver transplantation or elective insertion or follow-up of a TIPS. The test is administered on a computer and requires a yes/no response, requiring no prior computer experience from patients. The results of that study reflected that there was improvement after liver transplantation and worsening after the nitrogen challenge, status-post TIPS procedure 36. The CDR is simple to administer, requiring less than thirty minutes, however it does require a practice session in advance. This test is currently available in the United Kingdom. With reliable correlation with the PHES 36, good test-retest reliability, and high sensitivity in impaired populations 39, the CDR is a good candidate as a diagnostic tool for MHE.
ImPACT Assessment System
In a study published only in abstract form, Tsushima et al used the ImPACT (Immediate Post-concussion Assessment and Cognitive Testing), a brief, validated, web-based, computerized module that is validated for concussion 40. It is a 6-module neuropsychological test battery resulting in 4 composite scores [Verbal Memory (VrbM), Visual Memory (VisM), Visual Motor Speed (VMS) and Reaction Time (RT)] with a normative group. They compared ninety cirrhotic patients with 131 controls and found that the ImPACT scores were significantly correlated with a standard battery (NCT-A/B and DST). They also found an association between ImPACT scores and quality of life. However, published studies on ImPACT in MHE and validation in other centers are awaited before this can be used freely.
Electrophysiological assessment
Electroencephalogram
Neurophysiologic testing may be offered for the diagnosis of HE with the assistance of a neurologist and specialized staff, as well as dedicated equipment. This testing provides objective information on metabolic function, electrolyte homeostasis, as well as the effect of drugs and toxins on the brain. This exam is free of educational and cultural confounders when compared to psychometric examinations as previously mentioned. In 1957, Parsons-Smith et al 41 first noted slowing of the EEG rhythms in 40% of patients with cirrhosis, as well as EEG changes and HE severity. Further advances in EEG and the utilization of spectral EEG analysis have allowed for more accurate measurements in abnormalities present in cirrhosis 18, 42, 43. The use of the Short Epoch Dominanat Activity Clustering Algorithm (SEDECA) has subsequently provided a means for spatially mapping these deficits 44. Recently a lot of work has been done to better define the neurophysiologic profile of patients with cirrhosis, specifically with regards to examination of the usefulness of the EEG in routine work-up of patients with cirrhosis. It has been shown that there seems to be associations between severity of liver disease and HE and alterations in EEG 45.
Studies have shown that patients with cirrhosis have a reduced mean dominant frequency, higher theta relative power and lower beta relative power when compared to controls in the parietal regions. The power of the spectral bands was similar in patients and controls over the frontal EEG regions 45. As the degree of cirrhosis increased, there was associated slowing of the EEG rhythms, particularly in the parietal regions, and patients with a history of overt HE had an increase in negative changes in EEG readings compared to those without overt HE. At the conclusion of this study, prognosis and mortality were evaluated in light of changes on EEG, and the EEG may provide valuable prognostic information both about survival and the risk or overt HE 45.
With the proper equipment and supervising personnel, the EEG may provide additional information with regards to neurophysiology during cirrhosis and HE. One thing to consider is that EEG examines only cortical activity, which lacks the sub-cortical activity exam done with psychometric batteries such as the PSE-syndrome test 18. Psychometric batteries have shown to often be more sensitive than the neurophysiologic testing, however there may be promise in measuring evoked potentials with EEG. Evoked potentials are the measurements of the time between a given stimulus (visual, somatosensory, and auditory) and the brain’s ability to sense it. These potentials are divided into both cortial and sub-cortical components, which would be helpful in narrowing the gap between psychometric and physiologic testing 18. Visual evoked potentials have been found to only be useful in detecting of early HE stages 46, however auditory responses to stimuli, measured as the auditory P300, has good diagnostic potential and can be used when available. The visual P300 is not recommended due to inconsistent results 47.
Critical flicker frequency (CFF)
Due to the lack of availability of the aforementioned neuropsychometric and physiologic tests due to a myriad of issues (copyrights, equipment, proper personnel to administer them), recent studies have been performed examining tests that might be applied in the clinical setting by clinicians other than psychologists and/or neurologists. The critical flicker frequency (CFF) measures function at the level of the cortex, and has direct correlation with psychometric tests 48. This test employs the theory that the pathogenesis of HE is comprised of low-grade astrocyte swelling 49, disrupting neuronal communication. This same process occurs in glial cells of the retina 50, 51. The thought is that retinal gliopathy could serve as a marker of cerebral gliopathy occurring in HE, and has been investigated in patients with low grade HE.
The test is conducted by introducing a flickering light to the patient with a portable device, and the patient indicates the minimum frequency at which the light is still perceived as flickering and not fused. The frequency of the flickering is increased from 25 Hz and the patient determines the fusion-frequency threshold. The reverse is also done, where the frequency of the light flickering is started at 60 Hz and the patient determines when the fused flickering light switches to being non-fused. The levels of 38–39 Hz could differentiate between HE and no HE, but is less sensitive in differentiating MHE from HE. Results have been robust in both Spain and India 52. This test is simple to administer, and may be deployed without the supervision or interpretation of a psychologist or neurologist. The test can be performed in a short period of time, and aside from the equipment, is not costly to perform. The CFF, however, has not been validated for use in the US population.
Summary
The diagnosis of MHE remains an important challenge that needs to be faced in order to evaluate the epidemic of cirrhotic patients with this condition. These subtle changes in cognition require specialized testing and therefore expertise in this field is necessary to evaluate MHE in the clinical arena. There are several psychometric and neurophysiologic tests available to diagnose MHE but there is currently no consensus regarding their use. The challenge for the future is to develop methods that properly evaluate cognitive function in hepatic encephalopathy as a continuum as part of the spectrum of neuro-cognitive impairment in cirrhosis (SONIC) 3 in order to expedite diagnosis for determining outcome and administering proper treatment in a timely fashion.
Footnotes
Relationships: Dr Kappus has nothing to disclose. Dr Bajaj has received grant funding from Salix Pharmaceuticals and Ocera Therapeutics.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ferenci P, et al. Hepatic encephalopathy--definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology. 2002;35:716–721. doi: 10.1053/jhep.2002.31250. [DOI] [PubMed] [Google Scholar]
- 2.Poordad FF. Review article: the burden of hepatic encephalopathy. Aliment Pharmacol Ther. 2007;25 (Suppl 1):3–9. doi: 10.1111/j.1746-6342.2006.03215.x. [DOI] [PubMed] [Google Scholar]
- 3.Bajaj JS, Wade JB, Sanyal AJ. Spectrum of neurocognitive impairment in cirrhosis: Implications for the assessment of hepatic encephalopathy. Hepatology. 2009;50:2014–2021. doi: 10.1002/hep.23216. [DOI] [PubMed] [Google Scholar]
- 4.Bajaj JS, et al. Inhibitory control test for the diagnosis of minimal hepatic encephalopathy. Gastroenterology. 2008;135:1591–1600.e1. doi: 10.1053/j.gastro.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Weissenborn K, Ennen JC, Schomerus H, Ruckert N, Hecker H. Neuropsychological characterization of hepatic encephalopathy. J Hepatol. 2001;34:768–773. doi: 10.1016/s0168-8278(01)00026-5. [DOI] [PubMed] [Google Scholar]
- 6.Ford JM, et al. Acquiring and inhibiting prepotent responses in schizophrenia: event-related brain potentials and functional magnetic resonance imaging. Arch Gen Psychiatry. 2004;61:119–129. doi: 10.1001/archpsyc.61.2.119. [DOI] [PubMed] [Google Scholar]
- 7.Schiff S, et al. Impairment of response inhibition precedes motor alteration in the early stage of liver cirrhosis: a behavioral and electrophysiological study. Metab Brain Dis. 2005;20:381–392. doi: 10.1007/s11011-005-7922-4. [DOI] [PubMed] [Google Scholar]
- 8.Ortiz M, Jacas C, Cordoba J. Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol. 2005;42 (Suppl):S45–53. doi: 10.1016/j.jhep.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 9.Saxena N, et al. Electrophysiological and neuropsychological tests for the diagnosis of subclinical hepatic encephalopathy and prediction of overt encephalopathy. Liver. 2002;22:190–197. doi: 10.1034/j.1600-0676.2002.01431.x. [DOI] [PubMed] [Google Scholar]
- 10.Vergara-Gomez M, Flavia-Olivella M, Gil-Prades M, Dalmau-Obrador B, Cordoba-Cardona J. Diagnosis and treatment of hepatic encephalopathy in Spain: results of a survey of hepatologists. Gastroenterol Hepatol. 2006;29:1–6. doi: 10.1157/13083245. [DOI] [PubMed] [Google Scholar]
- 11.Bajaj JS, Etemadian A, Hafeezullah M, Saeian K. Testing for minimal hepatic encephalopathy in the United States: An AASLD survey. Hepatology. 2007;45:833–834. doi: 10.1002/hep.21515. [DOI] [PubMed] [Google Scholar]
- 12.Amodio P, et al. Attention dysfunction in cirrhotic patients: an inquiry on the role of executive control, attention orienting and focusing. Metab Brain Dis. 2005;20:115–127. doi: 10.1007/s11011-005-4149-3. [DOI] [PubMed] [Google Scholar]
- 13.Bajaj JS. Minimal hepatic encephalopathy matters in daily life. World J Gastroenterol. 2008;14:3609–3615. doi: 10.3748/wjg.14.3609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bajaj JS, Hafeezullah M, Hoffmann RG, Saeian K. Minimal hepatic encephalopathy: a vehicle for accidents and traffic violations. Am J Gastroenterol. 2007;102:1903–1909. doi: 10.1111/j.1572-0241.2007.01424.x. [DOI] [PubMed] [Google Scholar]
- 15.Bajaj JS, et al. Navigation skill impairment: Another dimension of the driving difficulties in minimal hepatic encephalopathy. Hepatology. 2008;47:596–604. doi: 10.1002/hep.22032. [DOI] [PubMed] [Google Scholar]
- 16.Bajaj JS, et al. Minimal hepatic encephalopathy is associated with motor vehicle crashes: the reality beyond the driving test. Hepatology. 2009;50:1175–1183. doi: 10.1002/hep.23128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ortiz M. Development of a clinical hepatic encephalopathy staging scale. [DOI] [PubMed] [Google Scholar]
- 18.Amodio P, et al. Detection of minimal hepatic encephalopathy: normalization and optimization of the Psychometric Hepatic Encephalopathy Score. A neuropsychological and quantified EEG study. J Hepatol. 2008;49:346–353. doi: 10.1016/j.jhep.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 19.Romero-Gomez M, et al. Value of the critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology. 2007;45:879–885. doi: 10.1002/hep.21586. [DOI] [PubMed] [Google Scholar]
- 20.Riggio O, et al. A simplified psychometric evaluation for the diagnosis of minimal hepatic encephalopathy. Clin Gastroenterol Hepatol. 2011;9:613–6.e1. doi: 10.1016/j.cgh.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 21.Sotil EU, Gottstein J, Ayala E, Randolph C, Blei AT. Impact of preoperative overt hepatic encephalopathy on neurocognitive function after liver transplantation. Liver Transpl. 2009;15:184–192. doi: 10.1002/lt.21593. [DOI] [PubMed] [Google Scholar]
- 22.Sorrell JH, Zolnikov BJ, Sharma A, Jinnai I. Cognitive impairment in people diagnosed with end-stage liver disease evaluated for liver transplantation. Psychiatry Clin Neurosci. 2006;60:174–181. doi: 10.1111/j.1440-1819.2006.01483.x. [DOI] [PubMed] [Google Scholar]
- 23.Meyer T, Eshelman A, Abouljoud M. Neuropsychological changes in a large sample of liver transplant candidates. Transplant Proc. 2006;38:3559–3560. doi: 10.1016/j.transproceed.2006.10.050. [DOI] [PubMed] [Google Scholar]
- 24.Douglass A, Al Mardini H, Record C. Amino acid challenge in patients with cirrhosis: a model for the assessment of treatments for hepatic encephalopathy. J Hepatol. 2001;34:658–664. doi: 10.1016/s0168-8278(01)00004-6. [DOI] [PubMed] [Google Scholar]
- 25.Oppong KN, Al-Mardini H, Thick M, Record CO. Oral glutamine challenge in cirrhotics pre- and post-liver transplantation: a psychometric and analyzed EEG study. Hepatology. 1997;26:870–876. doi: 10.1002/hep.510260411. [DOI] [PubMed] [Google Scholar]
- 26.Rees CJ, Oppong K, Al Mardini H, Hudson M, Record CO. Effect of L-ornithine-L-aspartate on patients with and without TIPS undergoing glutamine challenge: a double blind, placebo controlled trial. Gut. 2000;47:571–574. doi: 10.1136/gut.47.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amodio P, et al. Clinical features and survivial of cirrhotic patients with subclinical cognitive alterations detected by the number connection test and computerized psychometric tests. Hepatology. 1999;29:1662–1667. doi: 10.1002/hep.510290619. [DOI] [PubMed] [Google Scholar]
- 28.Garavan H, Ross TJ, Stein EA. Right hemispheric dominance of inhibitory control: an event-related functional MRI study. Proc Natl Acad Sci U S A. 1999;96:8301–8306. doi: 10.1073/pnas.96.14.8301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konrad K, Gauggel S, Manz A, Scholl M. Inhibitory control in children with traumatic brain injury (TBI) and children with attention deficit/hyperactivity disorder (ADHD) Brain Inj. 2000;14:859–875. doi: 10.1080/026990500445691. [DOI] [PubMed] [Google Scholar]
- 30.Pliszka SR, Liotti M, Woldorff MG. Inhibitory control in children with attention-deficit/hyperactivity disorder: event-related potentials identify the processing component and timing of an impaired right-frontal response-inhibition mechanism. Biol Psychiatry. 2000;48:238–246. doi: 10.1016/s0006-3223(00)00890-8. [DOI] [PubMed] [Google Scholar]
- 31.Ballard JC. Assessing attention: comparison of response-inhibition and traditional continuous performance tests. J Clin Exp Neuropsychol. 2001;23:331–350. doi: 10.1076/jcen.23.3.331.1188. [DOI] [PubMed] [Google Scholar]
- 32.Walker AJ, Shores EA, Trollor JN, Lee T, Sachdev PS. Neuropsychological functioning of adults with attention deficit hyperactivity disorder. J Clin Exp Neuropsychol. 2000;22:115–124. doi: 10.1076/1380-3395(200002)22:1;1-8;FT115. [DOI] [PubMed] [Google Scholar]
- 33.Bajaj JS, et al. Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol. 2007;102:754–760. doi: 10.1111/j.1572-0241.2007.01048.x. [DOI] [PubMed] [Google Scholar]
- 34.Bajaj JS, et al. Rifaximin improves driving simulator performance in a randomized trial of patients with minimal hepatic encephalopathy. Gastroenterology. 2011;140:478–487.e1. doi: 10.1053/j.gastro.2010.08.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Amodio P, et al. Improving the inhibitory control task to detect minimal hepatic encephalopathy. Gastroenterology. 2010;139:510–8. 518.e1–2. doi: 10.1053/j.gastro.2010.04.057. [DOI] [PubMed] [Google Scholar]
- 36.Mardini H, Saxby BK, Record CO. Computerized psychometric testing in minimal encephalopathy and modulation by nitrogen challenge and liver transplant. Gastroenterology. 2008;135:1582–1590. doi: 10.1053/j.gastro.2008.06.043. [DOI] [PubMed] [Google Scholar]
- 37.McKeith I, et al. Efficacy of rivastigmine in dementia with Lewy bodies: a randomised, double-blind, placebo-controlled international study. Lancet. 2000;356:2031–2036. doi: 10.1016/S0140-6736(00)03399-7. [DOI] [PubMed] [Google Scholar]
- 38.Forton DM, et al. Hepatitis C and cognitive impairment in a cohort of patients with mild liver disease. Hepatology. 2002;35:433–439. doi: 10.1053/jhep.2002.30688. [DOI] [PubMed] [Google Scholar]
- 39.Wesnes KA, et al. Effects of rivastigmine on cognitive function in dementia with lewy bodies: a randomised placebo-controlled international study using the cognitive drug research computerised assessment system. Dement Geriatr Cogn Disord. 2002;13:183–192. doi: 10.1159/000048651. [DOI] [PubMed] [Google Scholar]
- 40.Tsushima M, Tsushima W, Tsushima V, Lim N, Madrigal E, Jackson C, Mendler M. A case control study of ImPACT: a brief and effective web-based neuropsychological assessment battery to diagnose minimal hepatic encephalopathy (mhe) Journal of hepatology. 2010 doi: 10.1007/s10620-013-2668-z. [DOI] [PubMed] [Google Scholar]
- 41.Parsons-Smith BG, Summerskill WH, Dawson AM, Sherlock S. The electroencephalograph in liver disease. Lancet. 1957;273:867–871. doi: 10.1016/s0140-6736(57)90005-3. [DOI] [PubMed] [Google Scholar]
- 42.Quero JC, Hartmann IJ, Meulstee J, Hop WC, Schalm SW. The diagnosis of subclinical hepatic encephalopathy in patients with cirrhosis using neuropsychological tests and automated electroencephalogram analysis. Hepatology. 1996;24:556–560. doi: 10.1002/hep.510240316. [DOI] [PubMed] [Google Scholar]
- 43.Van der Rijt CC, Schalm SW, De Groot GH, De Vlieger M. Objective measurement of hepatic encephalopathy by means of automated EEG analysis. Electroencephalogr Clin Neurophysiol. 1984;57:423–426. doi: 10.1016/0013-4694(84)90071-3. [DOI] [PubMed] [Google Scholar]
- 44.Montagnese S, Jackson C, Morgan MY. Spatio-temporal decomposition of the electroencephalogram in patients with cirrhosis. J Hepatol. 2007;46:447–458. doi: 10.1016/j.jhep.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 45.Marchetti P, et al. Electroencephalography Alterations in Patients with Cirrhosis. Gastroenterology. 2011 doi: 10.1053/j.gastro.2011.06.085. [DOI] [PubMed] [Google Scholar]
- 46.Amodio P, et al. Prevalence and prognostic value of quantified electroencephalogram (EEG) alterations in cirrhotic patients. J Hepatol. 2001;35:37–45. doi: 10.1016/s0168-8278(01)00129-5. [DOI] [PubMed] [Google Scholar]
- 47.Montagnese S, Amodio P, Morgan MY. Methods for diagnosing hepatic encephalopathy in patients with cirrhosis: a multidimensional approach. Metab Brain Dis. 2004;19:281–312. doi: 10.1023/b:mebr.0000043977.11113.2a. [DOI] [PubMed] [Google Scholar]
- 48.Kircheis G, Wettstein M, Timmermann L, Schnitzler A, Haussinger D. Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology. 2002;35:357–366. doi: 10.1053/jhep.2002.30957. [DOI] [PubMed] [Google Scholar]
- 49.Haussinger D, Kircheis G, Fischer R, Schliess F, vom Dahl S. Hepatic encephalopathy in chronic liver disease: a clinical manifestation of astrocyte swelling and low-grade cerebral edema? J Hepatol. 2000;32:1035–1038. doi: 10.1016/s0168-8278(00)80110-5. [DOI] [PubMed] [Google Scholar]
- 50.Eckstein AK, et al. Hepatic retinopathia. Changes in retinal function. Vision Res. 1997;37:1699–1706. doi: 10.1016/s0042-6989(96)00318-5. [DOI] [PubMed] [Google Scholar]
- 51.Reichenbach A, Fuchs U, Kasper M, el-Hifnawi E, Eckstein AK. Hepatic retinopathy: morphological features of retinal glial (Muller) cells accompanying hepatic failure. Acta Neuropathol. 1995;90:273–281. doi: 10.1007/BF00296511. [DOI] [PubMed] [Google Scholar]
- 52.Sharma P, Sharma BC, Puri V, Sarin SK. Critical flicker frequency: diagnostic tool for minimal hepatic encephalopathy. J Hepatol. 2007;47:67–73. doi: 10.1016/j.jhep.2007.02.022. [DOI] [PubMed] [Google Scholar]