Summary
Endovascular treatment of complex, wide-necked bifurcation cerebral aneurysms is challenging. Intra/extra-aneurysmal stent placement, the “waffle cone” technique, has the advantage of using a single stent to prevent coil herniation without the need to deliver the stent to the efferent vessel. The published data on the use of this technique is limited. We present our initial and follow-up experience with the waffle cone stent-assisted coiling (SAC) of aneurysms to evaluate the durability of the technique. We retrospectively identified ten consecutive patients who underwent SAC of an aneurysm using the waffle cone technique from July 2009 to March 2011. Clinical and angiographic outcomes after initial treatment and follow-up were evaluated.
Raymond Class I or II occlusion of the aneurysm was achieved in all cases with the waffle cone technique. No intraoperative aneurysm rupture was noted. The parent arteries were patent at procedure completion. Clinical follow-up in nine patients (median 12.9 months) revealed no aneurysm rupture. Two patients had a transient embolic ischemic attack at 18 hours and three months after treatment, respectively. Catheter angiography or MRA at six-month follow-up demonstrated persistent occlusions of aneurysms in seven out of eight patients. Another patient had stable aneurysm occlusion at three-month follow-up study. Our experience in the small series suggests the waffle cone technique could be performed on complex, wide-necked aneurysms with relative safety, and it allowed satisfactory occlusions of the aneurysms at six months in most cases.
Key words: waffle cone technique, wide-necked aneurysm, stent-assisted, coiling, endovascular
Introduction
Coiling of intracranial aneurysms is a useful alternative to surgical clipping. However, complex wide-necked bifurcation aneurysms present a difficult challenge to neurointerventionalists because of their anatomic features. Several authors have reported their success in the treatment of these complex, wide-necked aneurysms by using the Y-configured dual stent-assisted coiling (SAC), the X-configured dual SAC, the double microcatheter technique, and balloon remodeling technique. Stent placement with proximal stent edge in the afferent vessel and distal edge in the body of the aneurysm (intra/extra-aneurysmal placement or “waffle cone” technique) was first reported in the successful treatment of eight cases in 2006. However, there is little information regarding medium and long-term outcomes in patients so treated. Here, we present our initial experience and intermediate term clinical outcomes using the waffle-cone technique.
Methods
Patient Selection
The medical records of ten consecutive patients admitted to the Neurosurgery Department of University of Iowa Hospitals and Clinics from July 2009 to March 2011 who underwent SAC of a complex wide-necked bifurcation aneurysm using the waffle cone technique were reviewed. Three patients suffered from ruptured aneurysms (one patient with Hunt and Hess (HH) grade 2 subarachnoid hemorrhage (SAH), another one with HH grade 3 SAH and the third one with HH grade 4 SAH), six had unruptured aneurysms and one had a recurrence after clipping. All patients or their legal power of attorneys elected endovascular treatment for aneurysms.
Aneurysm Morphology
Of the ten wide-necked bifurcation aneurysms, six were located at the anterior communicating artery (AcomA), three were at the middle cerebral artery (MCA) bifurcation, and one was at the basilar artery (BA) terminus. The aneurysms ranged in size from 5 to 13 mm (largest dimension measured by digital subtraction angiography). Aneurysm size was ≤ 6 mm in five aneurysms, 7-10 mm in one, and ≥ 10 mm in four. Aneurysms were assessed as having a wide neck if the neck dimension was > 4 mm or the neck-to-doom ratio ≥ 2. Efferent arteries were incorporated into the aneurysm sac with a sharply angulated course in all cases. This anatomic configuration was judged to pose a formidable technical challenge and unacceptable risks of complication with conventional SAC technique.
Procedures
All aneurysms were treated under general anesthesia using a transfemoral approach. Ruptured aneurysms were treated within 24 hours of admission. The Neuroform3® stent (Boston Scientific, Fremont, California, USA) was used in nine cases and the Enterprise stent (Cordis Endovascular, Warren, New Jersey, USA) was used in one. The diameter of stents was determined based on assessment of the size of the aneurysm neck and the diameter of the proximal parent artery. Each stent was deployed with the proximal edge in the parent artery, and the distal edge in the proximal fundus of the aneurysm, which created a waffle-cone configuration. A 6F Envoy MPD catheter (Cordis, Miami Lakes, FL, USA) was used as a guiding catheter. For Neuroform stent placement, a Renegade Hi-Flo microcatheter, (Boston Scientific, Fremont, CA,USA) was positioned with its tip in aneurysm using a 0.014” microguidewire. The stent was transferred to the microcatheter and deployed using a pusher comprised of the stabilizer catheter and a Transend 14 microguidewire (Boston Scientific, Fremont, CA,USA). The Enterprise stent was placed using a Prowler Select Plus microcatheter (Cordis Endovascular, Warren, NJ, USA). Flaring of the intra-aneurysmal portion of the stent resulted in covering of the origins of incorporated efferent arteries in all cases. After successful stenting, a SL-10 microcatheter (Boston Scientific, Fremont, CA,USA) was advanced into the aneurysm through the stent lumen for coiling. Aneurysm occlusions were graded with the Raymond classification: Class I, complete occlusion; Class II, neck remnant; and Class III, residual aneurysm.
Anticoagulation and Antiplatelet Management
Patients with unruptured aneurysms were given aspirin (81 mg daily) and clopidogrel (75 mg daily) for at least three days before the procedure and received systemic heparinization after the sheath placement, with activated clotting time was maintained at two to three times above the baseline value. Heparin was withheld in patients with ruptured aneurysms until the aneurysm was secured, at which time heparin and clopidogrel 600 mg per orogastric tube were administered. After the procedure, all patients continued on aspirin (81 mg daily) and clopidogrel (75 mg daily) for six weeks. Clopidogrel was then discontinued and aspirin was increased to 325 mg daily indefinitely.
Clinical and Angiographic Follow-up
Clinical evaluation consisting of physical examination and modified Rankin scale assessment (mRS, mRS 0-1 was defined as excellent outcomes; mRS 2 good, mRS 3 to 4, poor, and mRS 5 death) was performed at discharge and patients were advised to return for outpatient reassessment at six weeks, six months and 12 months after the treatment and yearly thereafter. Catheter cerebral angiography was advised at six months to access the status of the treated aneurysm. The angiographic results were interpreted by using the Raymond classification. Patients who could not tolerate catheter angiography had MR angiography as follow-up studies.
Results
The characteristics of ten patients including demographics, morphologic features of the aneurysms are summarized in Table 1. The endovascular treatment including stent selection, initial and follow-up outcomes and complications are summarized in Table 2.
Table 1.
Summary of clinical features of ten patients with complex wide-necked aneurysms.
| Patient No. |
Age, y/ (Sex) |
Presentation | HH Grading |
mRS at admission |
Aneurysm Characteristics | |
|---|---|---|---|---|---|---|
| Location | Maximum Diameter (mm) |
|||||
| 1 | 55 (M) | Ruptured | 3 | 1 | AcomA | 12 |
| 2 | 73 (F) | Unruptured | 0 | 0 | AcomA | 6 |
| 3 | 62(F) | Ruptured | 2 | 1 | MCA bifurcation, left | 11 |
| 4 | 50 (M) | Unruptured | 0 | 0 | AcomA | 12 |
| 5 | 65 (F) | Recurrence | 0 | 0 | MCA bifurcation, right | 5 |
| 6 | 62 (M) | Ruptured | 4 | 4 | AcomA | 13 |
| 7 | 48 (F) | Unruptured | 0 | 0 | BA Terminus | 6 |
| 8 | 68 (M) | Unruptured | 0 | 0 | AcomA | 9 |
| 9 | 75 (M) | Unruptured | 0 | 0 | AcomA | 6 |
| 10 | 66 (M) | Unruptured | 0 | 0 | MCA bifurcation, left | 9 |
| HH Hunt and Hess; mRS modified ranking scale; AcomA Anterior communication artery; MCA middle cerebral artery; BA basilar artery | ||||||
Table 2.
Summary of stent choices, immediate and follow-up outcomes after treatment, and complications.
| Patient No |
Stent diameter/ length, mm |
Immediate resultsa |
Immediate complications |
mRS at discharge |
Angiographic follow-up |
Clinic follow-up | ||
|---|---|---|---|---|---|---|---|---|
| Interval m, modality |
Follow-up resultsa |
Late neurological complications |
Interval m, mRS at latest follow-up |
|||||
| 1 | NF 3.5/15 |
I | 1 | 6 m, DSA |
I | None | 12 m, 1 | |
| 2 | NF 4.0/15 |
I | 0 | 8 m, MRA |
Stable | None | 12 m, 0 | |
| 3 | NF 4.0/20 |
I | TIA from transient MCA thrombosis at 18 h after treatment |
1 | 5 m, DSA |
II | None | 12 m, 0 |
| 4 | NF 3.5/15 |
II | 0 | 6 m, DSA |
II | None | 15 m, 0 | |
| 5 | NF 4.0/15 |
I | 0 | 6 m, DSA |
I | None | 15 m, 0 | |
| 6 | NF 3.5/20 |
I | NA | NA | NA | NA | NA | |
| 7 | EP 4.5/22 | II | 0 | 6 m, DSA |
III | None | 14 m, 0 | |
| 8 | NF 3.5/15 |
II | 0 | 6 m, MRA |
Stable | None | 10 m, 0 | |
| 9 | NF 4.0/20 |
I | 0 | 8 m, MRA |
Stable | None | 10 m, 0 | |
| 10 | NF 3.5/15 |
I | 0 | 3 m, MRA |
Stable | Minor stroke 0at 3 m |
6 m, 0 | |
|
a Embolization results were classified using the Raymond classification system: class I, complete occlusion; class II, residual neck; class III, residual sac. NF Neuroform stent; EP Enterprise stent; TIA transient ischemic attack; MCA middle cerebral artery; mRS modified ranking scale; DSA digital subtraction angiography; MRA magnetic resonance angiography of the head; m months; NA not applicable. | ||||||||
Clinical Outcomes
Clinical evaluation was performed in all patients before hospital discharge. No aneurysm perforation from intra-aneurysmal stent placement or coiling occurred. In one patient with HH grade 4 SAH, care was withdrawn after successful aneurysm coiling. Another patient who had HH grade 2 SAH from ruptured left MCA aneurysm developed thrombosis in left MCA branch arteries 18 hours after the coiling. She had transient right hemiparesis and aphasia, which were completely resolved by the next day, and her mRS was 0 at discharge. A third patient who had HH grade 3 SAH had an uneventful hospital course, and the mRS was 1 at discharge. The other seven patients who had elective coiling had no periprocedural complications and were neurologically intact at discharge. Median length of clinical follow-up for the surviving nine patients was 12 months (range, 6-15 months). No rebleeding occurred during that period. One patient with a history of polycystic kidney disease (PCKD) and renal failure had transient right hemiparesis at three months after the left MCA aneurysm treatment. MRI of the brain showed acute left MCA embolic stroke. Both MRA and CTA of the head showed the stent was patent. He was switched to clopidogrel for better stent protection.
Stent Deployment and Angiographic Results
Diameter and length of stents are summarized in the Table 2. Immediately after coil embolization, seven aneurysms had Raymond Class I occlusion, and three had Class II occlusion.
Angiographic Follow-up
Angiographic and clinical follow-up was available in all nine patients surviving to hospital discharge. Five had follow-up with catheter cerebral angiography at a median of six months (range, 5-6 months). Four aneurysms remained radiographically occluded. One aneurysm had recurrence that required re-treatment. Stents were widely patent in five patients. Mild asymptomatic proximal Neuroform in-stent restenosis was noted in one patient. Another three patients had a follow-up MRA of the head with contrast enhancement between six and eight months after the treatment. All three aneurysms were well secured.
One patient with PKCD had a three-month MRA of the head without contrast enhancement showing the aneurysm was grossly secured.
Illustrative Cases
Patient 1
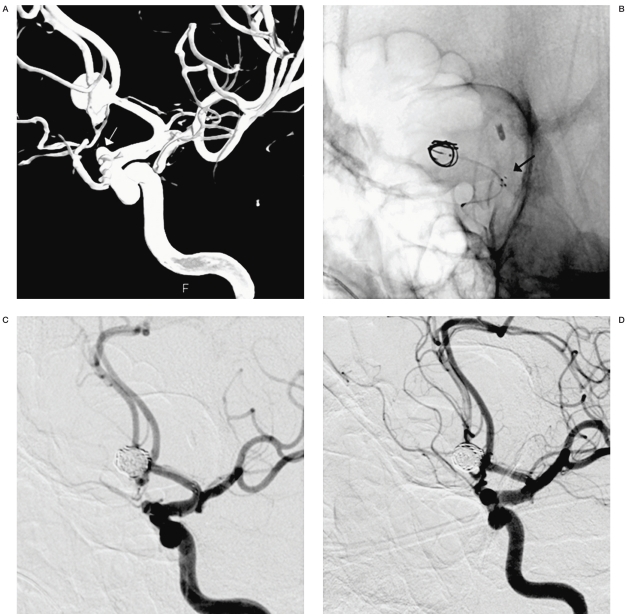
A 55-year-old man presented with a HH grade 3 SAH from a ruptured 12 mm wide neck AcomA aneurysm with incorporation of bilateral A2 segments. The right A1 was hypoplastic. The left A2 segment had an acute angulated course (Figure 1A). A Neuroform3® stent (4 × 15 mm) was deployed with distal edge inside the sac covering both A2 origins and proximal edge in the left A1 (Figure 1B).
The aneurysm was then embolized with Raymond class I occlusion (Figure 1C). The patient recovered well and was discharged home with mild paresthesia (mRS1).
Angiography at six-month follow-up showed the aneurysm remained occluded, and the stent widely patent.
Figure 1.
A) Dynamic DSA demonstrates a wide- necked AcomA aneurysm. A white arrow indicates a small left supraclinoid ICA aneurysm. B) A native view demonstrates the proximal end of the stent is in the left A1 segment (arrow) and the distal end is masked by the coil mass. C) DSA magnified view shows the aneurysm has Raymond Class I occlusion. Bilateral A2 segments were widely patent. D) DSA magnified view demonstrates the aneurysm has persistent complete occlusion at 6 months.
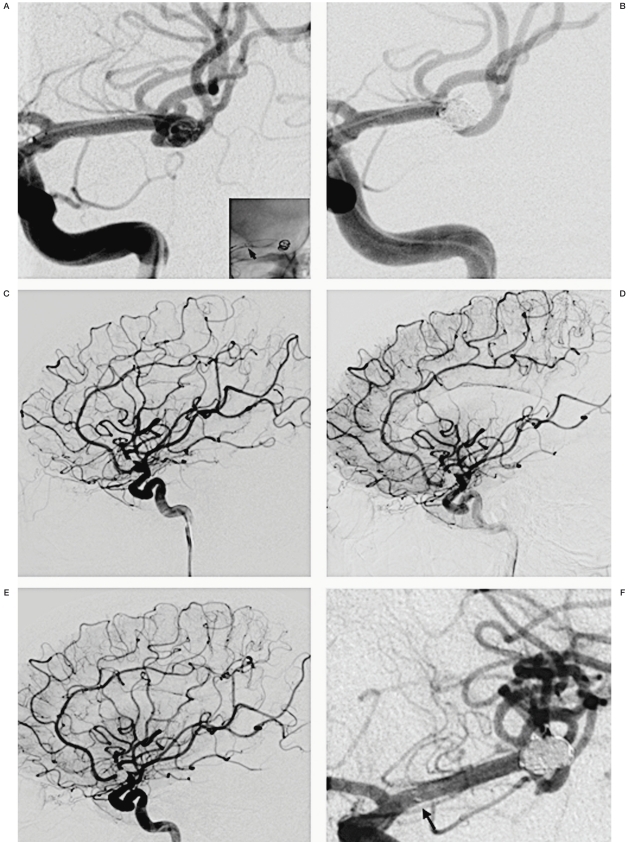
Patient 3
A 62-year-old woman with a history of chronic myelogenous leukemia (CML) presented with a HH grade 2 SAH from a ruptured 11 mm wide-necked MCA aneurysm. The efferent arteries were incorporated into the aneurysm neck with acute curves, rendering the anatomy difficult for Y-stenting or balloon remodeling. A Neuroform3® stent (4 × 20 mm) was deployed with its distal end inside the aneurysm covering both efferent artery origins (Figure 2A). The aneurysm had a Raymond Class I occlusion (Figure 2B) and no evident initial thromboembolic occlusion or in-stent platelet aggregation (Figure 2C). But the patient developed right side hemiparesis and aphasia 18 hours after the treatment. An emergent cerebral angiography revealed thrombosis in the superior division of the left MCA with delayed transit time in central cortical branch and posterior parietal branch arteries (Figure 2D). The stent in the left M1 was widely patent. As the patient's deficits were resolving, she was only treated with systemic infusion of Tirofiban. A follow-up angiography next day showed complete resolution of the thrombosis and normal transit time in the left MCA (Figure 2E). The patient was neurologically intact (mRS 0) at discharge (SAH day 11). An angiography at six-month follow-up showed left MCA aneurysm remained occluded, and the stent widely patent (Figure 2F).
Figure 2.
A) DSA magnified view demonstrates a wide-necked bilobular left MCA bifurcation aneurysm. A native view in the right lower corner shows the proximal end of the stent (a smaller arrow). B) DSA magnified view demonstrates Raymond Class I occlusion of the aneurysm. C) DSA lateral view demonstrates normal fillings of left MCA immediately after the procedure. D) DSA lateral view demonstrates delayed fillings at left central cortical branch and posterior parietal branch arteries at 18 hrs after the treatment. E) DSA lateral view demonstrates complete recanalization and normalized transit time of those branch arteries next day. F) DSA magnified view demonstrates persistent occlusion of the aneurysm and the widely patent stent at 6 months. Arrow indicates the proximal end of the stent.
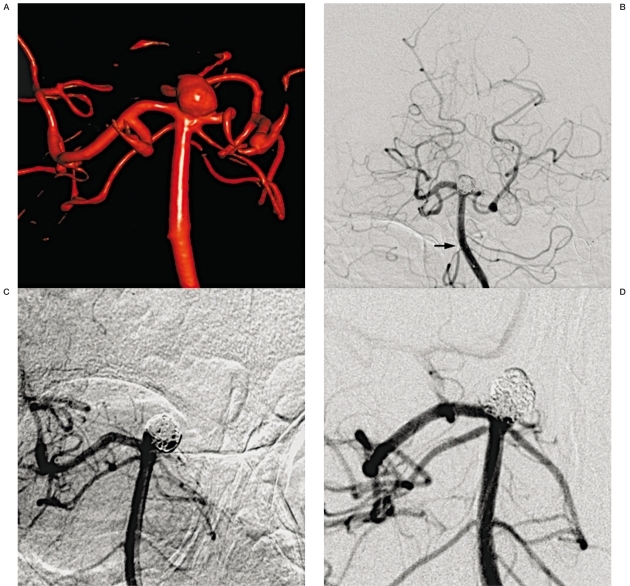
Patient 7
A 48-year-old woman presented with an unruptured 6 mm basilar terminus wide-necked aneurysm with incorporation of bilateral posterior cerebral arteries (PCA) into the neck of the aneurysm. Left P1 segment had a sharp-curved course, which made it impossible for distal access for stenting or balloon remodeling in the left PCA (Figure 3A). An Enterprise stent (4.5 × 22 mm) stent was placed with its distal end inside the sac and proximal end in the basilar artery. The aneurysm had a Raymond Class II occlusion (Figure 3B). An angiography at six-month follow-up showed significant recurrence (Figure 3C), which was successfully re-treated with coiling (Figure 3D).
Figure 3.
A) Dynamic DSA demonstrates a wide necked BA terminus aneurysm. B) DSA anteroposterior view demonstrates a Raymond Class II occlusion of the aneurysm. An arrow indicates an Enterprise stent proximal end in the BA. C) DSA magnified view demonstrates recurrence at 6 months. D) DSA magnified view demonstrates successful complete occlusion after coiling retreatment.
Discussion
Stent-assisted coiling has been increasingly utilized for endovascular treatment of intracranial aneurysms with the development of intracranial self-expanding stents. However, complex wide-necked bifurcation aneurysms continue to be technically challenging. Recently, Horowitz et al. presented their series using the waffle cone technique in successful treatment of eight wide-necked bifurcation aneurysms. The anatomic features of those aneurysms did not allow the Neuroform stent to cover the neck either in a straight or Y-configuration fashion. This technique represents an important novel approach for SAC. However, the risks of this technique and the likelihood of aneurysm recurrence are unclear. Thus, we performed a retrospective review of ten consecutive cases treated with the waffle cone technique at our institution with assessment of intermediate term outcomes. Six of eight aneurysms in the Horowitz series and three of four aneurysms in the Huang series had Raymond Class I occlusion. Consistent with their results, our series showed satisfactory occlusions of aneurysms can be achieved with the waffle cone technique. However, the degree of occlusion was less optimal in Sychra et al.'s series (Raymond Class II occlusion in all four treated aneurysms) and in the Yang et al.'s series (class III occlusion in a ruptured MCA aneurysm that was the only aneurysm treated with the waffle cone technique). The Neuroform stent was used in the series of Horowitz et al. and Huang et al., while the Solitaire stent was used in Sychra et al.'s and the LEO stent in the Yang et al.'s series. In our series the Neuroform stent was used in nine cases, and the Enterprise stent was used in one which had incomplete occlusion. The causes of the discrepancies are unclear. Distal stent edge flare behavior with intra-aneurysmal deployment and/or ease of microcatheter placement could be factors in any difference in different stent performance. Yang and Ho reported two aneurysms with initial complete occlusions using the waffle cone technique had continued occlusion at six months. Recently, Xu et al. also reported three aneurysms that had complete occlusion with the waffle cone treatment remained occluded at the follow-up study, while another two aneurysms with incomplete occlusions had significant recurrence. In the series of Sychra et al., all six aneurysms had initial incomplete occlusion. Follow-up angiography obtained in four cases showed all four aneurysms had significant recurrence. Hauck et al. reported a major recurrence of a giant ophthalmic aneurysm treated by the waffle cone technique. Initial occlusion of the aneurysm was incomplete. The recurrent case in our series also had incomplete occlusions. These data suggest that the likelihood of long aneurysm obliteration is related to the immediate embolization results, as with conventional stent-assisted coiling. Gordhan reported a modified waffle cone technique treating a complex, MCA bifurcation aneurysm. The intra-aneurysmal stent divided the aneurysm into compartments (external, and internal to the stent). Aneurysm obliteration by coiling was from the external compartment into the internal compartment. Coils interlocked as they were deployed spontaneously from two microcatheters positioned in two different compartments. This modification may improve the degree of aneurysm occlusion by the waffle cone technique. Compared to the Y-configuration stenting, the waffle cone technique involves a shorter total length of stented artery and no stent-in-stent overlap. These characteristics may reduce the risk of stent thrombosis. In the prior published case series, there was no stent-related thrombosis during the periprocedural period, and no ischemic clinical events during the reported follow-up. In our series, the afferent and efferent arteries were patent at the conclusion of the treatment in all patients. In the surviving nine patients, one patient had one minor ischemic event that could be related to stenting. Left MCA transient thrombosis in another patient was more likely due to hypercoagulable state from SAH and leukemia than the waffle cone technique. There were several drawbacks of the waffle cone technique. First, it is possible that stent may rupture the aneurysm if it jumps during positioning and deployment. There has been no reported ruptured case from the waffle cone treatment. Huang et al. suggested the waffle cone treatment could only be used in the aneurysms larger than 4 mm. In our series, the smallest treated aneurysms were 5 mm. Second, the waffle cone technique may divert the flow into the aneurysm thus possibly predisposing higher chance of aneurysm recurrences, especially when occlusion was not complete. However, there is no long-term follow-up study to access this possibility. Our report was the first series having intermediate follow-up results to evaluate this technique. Our initial experience suggests the durability of this technique in treatment of challenging wide-necked bifurcation aneurysms evident by that the majority of aneurysms treated with this method remained obliterated at six months. We will continue to monitor those aneurysms in a longer term. Third, the efferent arteries may be jailed by the stent. This could make it difficult to convert into a conventional stent assisted coiling in the future. In our series, we treated recurrent basilar aneurysm with recoiling without a need for additional stent. Our current study has limitations due to the fact that it is a retrospective study with a small number of aneurysms treated with this technique, and it lacks long-term follow-up results.
Conclusion
Our study showed the waffle cone technique to be a safe, effective alternative tool for stent-assisted coiling of complex, wide-necked bifurcation aneurysms whose anatomic features are unfavorable for conventional stent-assisted coiling.
The completeness of aneurysm occlusion with initial treatment may be important for persistent obliteration.
However, more cases with long-term follow-up results are needed to evaluate the durability of this technique
References
- 1.Leung CH, Poon WS, Yu LM. The ISAT trial. Lancet. 2003;361:430–431. doi: 10.1016/s0140-6736(03)12405-1. author reply 432. [DOI] [PubMed] [Google Scholar]
- 2.Wiebers DO, Whisnant JP, Huston J, 3rd, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–110 . doi: 10.1016/s0140-6736(03)13860-3. [DOI] [PubMed] [Google Scholar]
- 3.Biondi A, Janardhan V, Katz JM, et al. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery. 2007;61:460–468. doi: 10.1227/01.NEU.0000290890.62201.A9. discussion 468-469. [DOI] [PubMed] [Google Scholar]
- 4.Horowitz M, Levy E, Sauvageau E, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked- bifurcation aneurysms: eight cases using the waffle cone technique. Neurosurgery. 2006;58(4) Suppl 2:ONS-258–262. doi: 10.1227/01.NEU.0000204713.24945.D2. discussion ONS-262. [DOI] [PubMed] [Google Scholar]
- 5.Kai Y, Hamada J, Morioka M, et al. Double microcatheter technique for endovascular coiling of wide-neck aneurysms using a new guiding device for the transcarotid approach: technical note. Neuroradiology. 2005;47:73–77. doi: 10.1007/s00234-004-1277-0. [DOI] [PubMed] [Google Scholar]
- 6.Sani S, Lopes DK. Treatment of a middle cerebral artery bifurcation aneurysm using a double neuroform stent “Y” configuration and coil embolization: technical case report. Neurosurgery. 2005;57(Suppl 1):E209. doi: 10.1227/01.neu.0000163684.75204.cd. discussion E209. [DOI] [PubMed] [Google Scholar]
- 7.Stahl K, Augenstein J, Schulman CI, et al. Assessing the impact of teaching patient safety principles to medical students during surgical clerkships. J Surg Res. 2011;170:e29–e40. doi: 10.1016/j.jss.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 8.Thorell WE, Chow MM, Woo HH, et al. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery. 2005;56:1035–1040. discussion 1040. [PubMed] [Google Scholar]
- 9.Raymond J, Guilbert F, Weill A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–1403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 10.Akpek S, Arat A, Morsi H, et al. Self-expandable stent-assisted coiling of wide-necked intracranial aneurysms: a single-center experience. Am J Neuroradiol. 2005;26:1223–1231. [PMC free article] [PubMed] [Google Scholar]
- 11.Benitez RP, Silva MT, Klem J, et al. Endovascular occlusion of wide-necked aneurysms with a new intracranial microstent (Neuroform) and detachable coils. Neurosurgery. 2004;54:1359–1367. doi: 10.1227/01.neu.0000124484.87635.cd. discussion 1368. [DOI] [PubMed] [Google Scholar]
- 12.Fiorella D, Albuquerque FC, Deshmukh VR, et al. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3-6-mo) follow-up. Neurosurgery. 2005;56:1191–1201. doi: 10.1227/01.neu.0000159645.86823.af. discussion 1201-1202. [DOI] [PubMed] [Google Scholar]
- 13.Higashida RT, Halbach VV, Dowd CF, et al. Initial clinical experience with a new self-expanding nitinol stent for the treatment of intracranial cerebral aneurysms: the Cordis Enterprise stent. Am J Neuroradiol. 2005;26:1751–1756. [PMC free article] [PubMed] [Google Scholar]
- 14.Huang Q, Xu Y, Hong B, et al. Stent-assisted embolization of wide-neck anterior communicating artery aneurysms: review of 21 consecutive cases. Am J Neuroradiol. 2009;30:1502–1506. doi: 10.3174/ajnr.A1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sychra V, Klisch J, Werner M, et al. Waffle-cone technique with Solitaire AB Remodeling Device: endovascular treatment of highly selected complex cerebral aneurysms. Neuroradiology. 2011;53:961–972. doi: 10.1007/s00234-010-0766-6. [DOI] [PubMed] [Google Scholar]
- 16.Yang P, Liu J, Huang Q, et al. Endovascular treatment of wide-neck middle cerebral artery aneurysms with stents: a review of 16 cases. Am J Neuroradiol. 2010;31:940–946. doi: 10.3174/ajnr.A1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang TH, Wong HF, Yang MS, et al. “Waffle cone” technique for intra/extra-aneurysmal stent placement for the treatment of complex and wide-necked bifurcation aneurysm. Interv Neuroradiol. 2008;14 Suppl 2:49–52. doi: 10.1177/15910199080140S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu F, Qin X, Tian Y, et al. Endovascular treatment of complex intracranial aneurysms using intra/extra-aneurysmal stent. Acta Neurochir (Wien) 2011;153:923–930. doi: 10.1007/s00701-010-0934-9. [DOI] [PubMed] [Google Scholar]
- 19.Hauck EF, Natarajan SK, Hopkins LN, et al. Salvage Neuroform stent-assisted coiling for recurrent giant aneurysm after waffle-cone treatment. J NeuroIntervent Surg. 2011;3:27–29. doi: 10.1136/jnis.2010.002931. [DOI] [PubMed] [Google Scholar]
- 20.Gordhan AD. Intraaneurysmal neuroform stent implantation with compartmental dual microcatheter coil embolization: technical case report. J Neuroimaging. 2010;20:277–279. doi: 10.1111/j.1552-6569.2009.00423.x. [DOI] [PubMed] [Google Scholar]